Volume 13, Issue 3 (2021)
Iran J War Public Health 2021, 13(3): 185-188 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2021/08/22 | Accepted: 2021/08/25 | Published: 2021/11/8
Received: 2021/08/22 | Accepted: 2021/08/25 | Published: 2021/11/8
How to cite this article
Kadhim T, Abdulilah H. Eosinopenia; a Predictor of Non-Respiratory COVID-19. Iran J War Public Health 2021; 13 (3) :185-188
URL: http://ijwph.ir/article-1-998-en.html
URL: http://ijwph.ir/article-1-998-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Authors
T. Kadhim *1, H. Abdulilah1
1- Department of Internal Medicine, College of Medicine, University of Basrah, Basrah, Iraq
Full-Text (HTML) (1185 Views)
Introduction
December 2019 was the first appearance of a novel virus named SARS-COV-2 that causes severe acute respiratory distress syndrome in many thousands of Wuhan China; after that, it spread worldwide [1]; three months later, the WHO proclaimed it as a pandemic [2]. The spectrum of COVID-19 morbidity ranges from a flu-like illness to life-threatening pneumonia that culminates in severe acute respiratory distress syndrome, disseminated intravascular coagulopathy (DIC), or respiratory failure [3]. The infection is spreading worldwide, causing severe outbreaks, and in 2020 it became the third leading cause of death in the United States [4]. The complex pathophysiology of the virus Infectivity needs angiotensin-converting enzyme inhibiter (ACEI) receptors to trigger its cytopathic effect [5]; these receptors are scattered in the lungs, gastrointestinal system, heart, blood vessels, and blood cells like lymphocytes [6].
Hematological complications are common, including lymphopenia, leucopenia, thrombocytopenia & DIC [7]. Lymphopenia is often predicting a severe infection with poor outcomes [8].
The common cause of COVID 19 is deterioration to acute severe respiratory distress syndrome due to an uncontrolled inflammatory response termed cytokine storm [9]. Eosinophils are differentiated from hematopoietic progenitors cells in bone morrow, controlled by IL, 3, 4, 5 & other cytokines; they stay eight days in bone morrow to mature [10]; they reside mainly in the respiratory system, gastrointestinal system, and the skin and may survive 1-2 weeks if apoptosis prevented by cytokines [11]. Eosinophils are mostly a tissue leukocyte [12]; the tissue life span of eosinophil ranging from 2-5 days, & cytokines may increase their survival [13].
.Eosinophils constitute 1-6% of whole WBC [14] but increase in allergic and parasitic infections they have a potential role in inflammatory response at the level of innate and adaptive immunity; they modulate the immune response by production of inflammatory cytokines. Eosinophils can be recruited by dangerous signals released by viral, bacterial & parasitic infections. They have been shown to act as coordinators to regulate various immune cells, including lymphocytes & immune homeostasis [15]. C-reactive protein is liver protein elevated in widespread inflammatory reactions started after 6-8 hours reaching the peak after 48 hours the level decrease once the inflammatory reaction recovered [16].
This study aimed to investigate eosinopenia in non-respiratory COVID-19 patients.
Materials and Methods
This experimental study was carried out on COVID-19 patients who had the positive PCR (Polymerase Chain Reaction) test in an outpatient clinic in Al-Feiha Teaching Hospital in Basrah, Iraq. One hundred four patients were selected from June to November 2020.
The study was approved by the research ethics committee in the college of medicine, university of Basrah. Each patient had ascertained whether respiratory or non-respiratory illnesses and from each patient, a sample of blood was withdrawn for evaluation of blood counts and estimation of the inflammatory marker C-reactive protein. Screening for oxygen saturation was done by fingertip pulse oximeter (Model: AB-88, Lot: 200620 RoHS, China). Respiratory symptoms included anosmia, running, congested nose, sore throat, cough, sputum production, dyspnea, wheeze, or hemoptysis are obtained from history and clinical examination [17]. Each blood sample was examined for the counts of all cellular elements including total White Blood Cells, Lymphocytes, Basophil, Eosinophil, Neutrophil, Monocytes, Platelets & Red Blood Cells, along with other hematological indices including Hemoglobin level, Hematocrit, Mean Corpuscular Volume, Mean Corpuscular Hemoglobin concentration, Mean corpuscular Hemoglobin using Automated Hematology Analyser XP series 2018/08 Kobe 601-0073 (Sysmex corporation Japan). Eosinopenia was defined as an eosinophil count less than 0.04×103/µL [18]. C-reactive protein is considered elevated when leveling >10mg/L [19] and it was measured by Cobas Integra 400 Plus (Roche, Germany). Oxygen saturation is considered low when <95% [20]. Elevated body temperature is defined as >37.2°C in the morning or body temperature >37.7°C in the evening [21]. SARS-COV-2 RNA was detected by reverse transcription-polymerase chain reaction (BIO-RAD, model No. CFX96 Optics module, 2021/03 Singapore) using a nasopharyngeal swab.
The Chi-square statistical test in SPSS 20 software was used for data analysis.
Findings
A total of 104 patients with COVID 19 were included. Thirty-eight patients were male, and 66 patients were female (M:F ratio was 1:1.7). The mean±SD age was 41.6±13.0 with a range of 17-70 years. Respiratory COVID-19 cases were 54 patients, while 50 patients were non-respiratory COVID-19. Fever documented in 47 patients. Oxygen saturation declined in 41 patients. C-reactive protein was elevated in 99 patients. Platelets were normal in 76 patients.
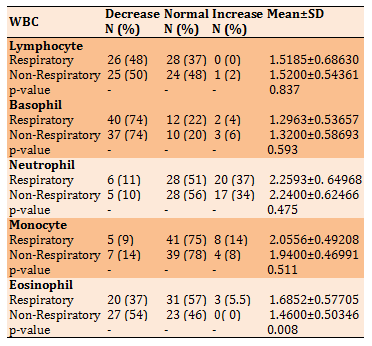
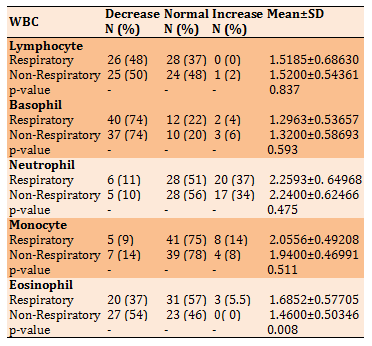
Total white blood cell count reduced in 17 patients and increased in 30 patients while normal in 57 patients (Table 1). Lymphocytosis was detected only in one patient (2%) with non-respiratory COVID-19. Monocytopenia was observed in 12 (24%) patients that five patients (9%) were respiratory COVID-19 and seven patients (14%) were non-respiratory COVID-19. Eosinopenia observed in 47 patients (45.1%); 20 patients (19%) were respiratory COVID-19 and 27 patients (26%) were non-respiratory COVID-19.
Table 1) Result of WBC counts in patients with the COVID-19
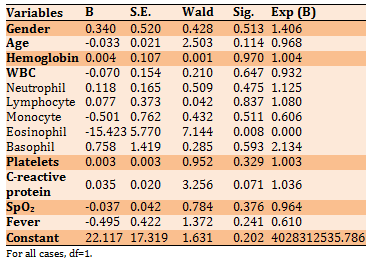
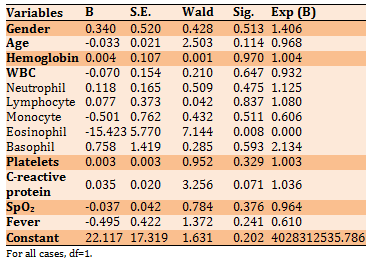
Logistic regression analysis indicated that eosinopenia is a significant independent predictor of non-respiratory COVID-19 infection (p<0.05; Table 2).
Table 2) Results of logistic regression analysis to predict the type of COVID-19 (respiratory versus non-respiratory)
Discussion
In this study, the reduction of eosinophil count is a strong predictor of non-respiratory infection COVID-19; our findings in this regard meet with several studies, among them is Fraisse et al. who reported that eosinopenia is accompanied by early and severe COVID-19 infection, and they also found that recovery from eosinophilia when to appear in an intensive care unit (ICU) patients, indicates a better prognosis [17].
A comparable result was observed by Tanni et al., where they found that persistent eosinopenia indicates a low recovery rate [18]. Similarly, other studies reported that eosinophilic patients had a high transfer rate to ICU [19]. Likewise, a recent Chinese study showed that patients with COVID-19 tend to have eosinopenia, which correlates to disease severity [20]. Another Chinese study concluded that eosinopenia is common in severe respiratory COVID-19, especially those with significant CT scan findings, yet the reduction of eosinophil is interestingly seen in the early days of illness [21]. Against that, a Taiwan study published in February 2021 showed that severe eosinopenia is observed more in patients with non-chest CT, finding COVID-19 [22]. Upon reviewing these notes, we conclude that eosinopenia is the sensitive index for the severity of COVID-19 infection & we assume that eosinopenia appears earlier & clearer even in asymptomatic or non-ordinary presentation & possibly all non-respiratory COVID-19 are sooner or later transformed to established pneumonic or other respiratory COVID-19. Another possible explanation for eosinopenia in non-respiratory COVID-19 is that eosinophils might have been targeted by the virulent virus in their shorter life span in circulation (8-18 hours), especially in the earlier or asymptomatic course. However, the roles of osteopenia in COVID-19 require further studies. Including the evaluations of other potential causes of eosinopenia like the use of corticosteroids or others [23].
Conclusion
Eosinopenia is a simple and reliable marker, helping in the early identification of COVID-19 suspected patients, especially those with non-respiratory manifestations.
Acknowledgments: We acknowledge the contribution of Omran S. Habeeb, professor of Basrah University, to review the paper's final draft.
Ethical Permissions: The ethical approval was dated June 29, 2021, at No. 272/24 by the College of Medicine, University of Basrah.
Conflicts of Interests: -
Authors' Contribution: Kadhim T. (First Author), Introduction Writer/Methodologist/Main Researcher/Statistical Analyst/Discussion Writer (50%); Abdulilah H. (Second Author), Introduction Writer/Methodologist/Assistant Researcher/Statistical Analyst/Discussion Writer (50%).
Funding/Support: This was personal.
December 2019 was the first appearance of a novel virus named SARS-COV-2 that causes severe acute respiratory distress syndrome in many thousands of Wuhan China; after that, it spread worldwide [1]; three months later, the WHO proclaimed it as a pandemic [2]. The spectrum of COVID-19 morbidity ranges from a flu-like illness to life-threatening pneumonia that culminates in severe acute respiratory distress syndrome, disseminated intravascular coagulopathy (DIC), or respiratory failure [3]. The infection is spreading worldwide, causing severe outbreaks, and in 2020 it became the third leading cause of death in the United States [4]. The complex pathophysiology of the virus Infectivity needs angiotensin-converting enzyme inhibiter (ACEI) receptors to trigger its cytopathic effect [5]; these receptors are scattered in the lungs, gastrointestinal system, heart, blood vessels, and blood cells like lymphocytes [6].
Hematological complications are common, including lymphopenia, leucopenia, thrombocytopenia & DIC [7]. Lymphopenia is often predicting a severe infection with poor outcomes [8].
The common cause of COVID 19 is deterioration to acute severe respiratory distress syndrome due to an uncontrolled inflammatory response termed cytokine storm [9]. Eosinophils are differentiated from hematopoietic progenitors cells in bone morrow, controlled by IL, 3, 4, 5 & other cytokines; they stay eight days in bone morrow to mature [10]; they reside mainly in the respiratory system, gastrointestinal system, and the skin and may survive 1-2 weeks if apoptosis prevented by cytokines [11]. Eosinophils are mostly a tissue leukocyte [12]; the tissue life span of eosinophil ranging from 2-5 days, & cytokines may increase their survival [13].
.Eosinophils constitute 1-6% of whole WBC [14] but increase in allergic and parasitic infections they have a potential role in inflammatory response at the level of innate and adaptive immunity; they modulate the immune response by production of inflammatory cytokines. Eosinophils can be recruited by dangerous signals released by viral, bacterial & parasitic infections. They have been shown to act as coordinators to regulate various immune cells, including lymphocytes & immune homeostasis [15]. C-reactive protein is liver protein elevated in widespread inflammatory reactions started after 6-8 hours reaching the peak after 48 hours the level decrease once the inflammatory reaction recovered [16].
This study aimed to investigate eosinopenia in non-respiratory COVID-19 patients.
Materials and Methods
This experimental study was carried out on COVID-19 patients who had the positive PCR (Polymerase Chain Reaction) test in an outpatient clinic in Al-Feiha Teaching Hospital in Basrah, Iraq. One hundred four patients were selected from June to November 2020.
The study was approved by the research ethics committee in the college of medicine, university of Basrah. Each patient had ascertained whether respiratory or non-respiratory illnesses and from each patient, a sample of blood was withdrawn for evaluation of blood counts and estimation of the inflammatory marker C-reactive protein. Screening for oxygen saturation was done by fingertip pulse oximeter (Model: AB-88, Lot: 200620 RoHS, China). Respiratory symptoms included anosmia, running, congested nose, sore throat, cough, sputum production, dyspnea, wheeze, or hemoptysis are obtained from history and clinical examination [17]. Each blood sample was examined for the counts of all cellular elements including total White Blood Cells, Lymphocytes, Basophil, Eosinophil, Neutrophil, Monocytes, Platelets & Red Blood Cells, along with other hematological indices including Hemoglobin level, Hematocrit, Mean Corpuscular Volume, Mean Corpuscular Hemoglobin concentration, Mean corpuscular Hemoglobin using Automated Hematology Analyser XP series 2018/08 Kobe 601-0073 (Sysmex corporation Japan). Eosinopenia was defined as an eosinophil count less than 0.04×103/µL [18]. C-reactive protein is considered elevated when leveling >10mg/L [19] and it was measured by Cobas Integra 400 Plus (Roche, Germany). Oxygen saturation is considered low when <95% [20]. Elevated body temperature is defined as >37.2°C in the morning or body temperature >37.7°C in the evening [21]. SARS-COV-2 RNA was detected by reverse transcription-polymerase chain reaction (BIO-RAD, model No. CFX96 Optics module, 2021/03 Singapore) using a nasopharyngeal swab.
The Chi-square statistical test in SPSS 20 software was used for data analysis.
Findings
A total of 104 patients with COVID 19 were included. Thirty-eight patients were male, and 66 patients were female (M:F ratio was 1:1.7). The mean±SD age was 41.6±13.0 with a range of 17-70 years. Respiratory COVID-19 cases were 54 patients, while 50 patients were non-respiratory COVID-19. Fever documented in 47 patients. Oxygen saturation declined in 41 patients. C-reactive protein was elevated in 99 patients. Platelets were normal in 76 patients.
Total white blood cell count reduced in 17 patients and increased in 30 patients while normal in 57 patients (Table 1). Lymphocytosis was detected only in one patient (2%) with non-respiratory COVID-19. Monocytopenia was observed in 12 (24%) patients that five patients (9%) were respiratory COVID-19 and seven patients (14%) were non-respiratory COVID-19. Eosinopenia observed in 47 patients (45.1%); 20 patients (19%) were respiratory COVID-19 and 27 patients (26%) were non-respiratory COVID-19.
Table 1) Result of WBC counts in patients with the COVID-19
Logistic regression analysis indicated that eosinopenia is a significant independent predictor of non-respiratory COVID-19 infection (p<0.05; Table 2).
Table 2) Results of logistic regression analysis to predict the type of COVID-19 (respiratory versus non-respiratory)
Discussion
In this study, the reduction of eosinophil count is a strong predictor of non-respiratory infection COVID-19; our findings in this regard meet with several studies, among them is Fraisse et al. who reported that eosinopenia is accompanied by early and severe COVID-19 infection, and they also found that recovery from eosinophilia when to appear in an intensive care unit (ICU) patients, indicates a better prognosis [17].
A comparable result was observed by Tanni et al., where they found that persistent eosinopenia indicates a low recovery rate [18]. Similarly, other studies reported that eosinophilic patients had a high transfer rate to ICU [19]. Likewise, a recent Chinese study showed that patients with COVID-19 tend to have eosinopenia, which correlates to disease severity [20]. Another Chinese study concluded that eosinopenia is common in severe respiratory COVID-19, especially those with significant CT scan findings, yet the reduction of eosinophil is interestingly seen in the early days of illness [21]. Against that, a Taiwan study published in February 2021 showed that severe eosinopenia is observed more in patients with non-chest CT, finding COVID-19 [22]. Upon reviewing these notes, we conclude that eosinopenia is the sensitive index for the severity of COVID-19 infection & we assume that eosinopenia appears earlier & clearer even in asymptomatic or non-ordinary presentation & possibly all non-respiratory COVID-19 are sooner or later transformed to established pneumonic or other respiratory COVID-19. Another possible explanation for eosinopenia in non-respiratory COVID-19 is that eosinophils might have been targeted by the virulent virus in their shorter life span in circulation (8-18 hours), especially in the earlier or asymptomatic course. However, the roles of osteopenia in COVID-19 require further studies. Including the evaluations of other potential causes of eosinopenia like the use of corticosteroids or others [23].
Conclusion
Eosinopenia is a simple and reliable marker, helping in the early identification of COVID-19 suspected patients, especially those with non-respiratory manifestations.
Acknowledgments: We acknowledge the contribution of Omran S. Habeeb, professor of Basrah University, to review the paper's final draft.
Ethical Permissions: The ethical approval was dated June 29, 2021, at No. 272/24 by the College of Medicine, University of Basrah.
Conflicts of Interests: -
Authors' Contribution: Kadhim T. (First Author), Introduction Writer/Methodologist/Main Researcher/Statistical Analyst/Discussion Writer (50%); Abdulilah H. (Second Author), Introduction Writer/Methodologist/Assistant Researcher/Statistical Analyst/Discussion Writer (50%).
Funding/Support: This was personal.
Keywords:
References
1. Huanng I, Pranta R. Lymphopenia in sever coronavirus disease - 19 (COVID-19): Systematic review and meta-analysis. J Intensive Care. 2020;8:36. [Link] [DOI:10.1186/s40560-020-00453-4] [PMID] [PMCID]
2. Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91(1):157-60. [Link]
3. De Oliveira Toledo SL, Nogueira LS, Cavalho MDG, Rios DRA, De Barros Penheiro M. COVID-19: Review and hematological impact. Clin Chim Acta. 2020;510:170-6. [Link] [DOI:10.1016/j.cca.2020.07.016] [PMID] [PMCID]
4. Woolf SH, Masters R, Aron L. Effect of COVID-19 pandemic in 2020, on life expectancy across populations in the USA and other high income countries: Simulations of provisional mortality data. BMJ. 2021;373:1343. [Link] [DOI:10.1136/bmj.n1343] [PMID] [PMCID]
5. Ni W, Yang X, Yang D, Bao J, Li R, Xiao Y, et al. Role of angiotensin-converting enzyme 2 (ACE2) in COVID-19. Crit Care. 2020;24(1):422. [Link] [DOI:10.1186/s13054-020-03120-0] [PMID] [PMCID]
6. Geblawi M, Wang K, Viveiros A, Nguyen Q, Zhang JC, Turnur AJ, et al. Angiotensin-converting enzyme 2: SARS-CoV-2 receptor and regulator of the renin-angiotensin system: Celebrating the 20th anniversary of the discovery of ACE2. Circ Res. 2020;126(10):1456-74. [Link] [DOI:10.1161/CIRCRESAHA.120.317015] [PMID] [PMCID]
7. Terpos E, Ntanasis-Stathopoulos I, Elalamy I, Kastritis E, Sergentanis TN, Politou M, et al. Hematological finding and complications of COVID-19. Am J Hematol. 2020;95(7):834-47. [Link] [DOI:10.1002/ajh.25829] [PMID] [PMCID]
8. Tan L, Wang Q, Zang D, Ding J, Huang Q, Tang YQ, et al. lymphopenia predicts disease severity of COVID-19: A descriptive and predictive study. Signal Transduct Target Ther. 2020;5(1):3. [Link] [DOI:10.1038/s41392-020-0159-1] [PMID] [PMCID]
9. Tang Y, Liu J, Zhang D, Xu Z, Ji J, Wen C. Cytokin storm in COVID-19: The current evidence and treatment strategies. Front Immunol. 2020;11:1708. [Link] [DOI:10.3389/fimmu.2020.01708] [PMID] [PMCID]
10. Rachel N. Eosinopphil, eosinophilia, and other disorders [Internet]. Brighton: Medical News Today; 2017 [cited: unknown]. Available from: https://www.medicalnewstoday.com/articles/311601. [Link]
11. Park YM, Bochner BS. Eosinophil survival and apoptosis in health and disease. Allergy Asthma Immunol Res. 2010;2(2):87-101. [Link] [DOI:10.4168/aair.2010.2.2.87] [PMID] [PMCID]
12. Rosenberg H, Phipps S, Foster P. Eosinophil trafficking in allergy and asthma. J Allergy Clin Immunol. 2007;119(6):1303-10. [Link] [DOI:10.1016/j.jaci.2007.03.048] [PMID]
13. Sur S, Adolphson C, Gleich G. Eosinophils: Biochemical and cellular aspects. Saint Louis: Mosby; 1993. [Link]
14. Celli B. Is the blood eosinophil count a useful biomarker in copd? the devil is in the details!. Arch Bronconeumol. 2017;53(8):415-6. [Spanish] [Link] [DOI:10.1016/j.arbres.2017.01.011] [PMID]
15. Long H, Liao W, Wang L, Lu Q. A player and coordinated: The versatile roles of eosinophils in immune system. Transfuse Med Hemother. 2016;43(2):96-108. [Link] [DOI:10.1159/000445215] [PMID] [PMCID]
16. Marnell L, Mold C, Du Clos TW. C-reactive protein: Ligands, receptors and role in inflammation. Clin Immunol. 2005;117(2):104-11. [Link] [DOI:10.1016/j.clim.2005.08.004] [PMID]
17. Fraisse M, Lgre E, Mentec H, Cally R, Plantefve G, Contou D. Eosinophilia in critically ill COVID-19 patients: A French monocentric retrospective study. Crit Care. 2020;24(1):635. [Link] [DOI:10.1186/s13054-020-03361-z] [PMID] [PMCID]
18. Tanni F, Akker E, Zaman MM, Figueroa N, Tharian B, Hupart KH. Eosinopenia and COVID-19. J Am Osteopath Assoc. 2020 Jul:7556. [Link] [DOI:10.7556/jaoa.2020.091] [PMID]
19. Huang J, Zhang Z, Liu S, Gong C, Chen L, Ai G, et al. Absolute eosinophil count predicts intensive care unit transfer among elderly COVID-19 patients from general isolation wards. Front Med. 2020;7:585222. [Link] [DOI:10.3389/fmed.2020.585222] [PMID] [PMCID]
20. Yan B, Yang J, Xie Y, Tang X. Relationship between a blood eosinophil level and COVID-19 mortality. World Allergy Organ J. 2021;14(3):100521. [Link] [DOI:10.1016/j.waojou.2021.100521] [PMID] [PMCID]
21. Xie G, Ding F, Han L, Yin D, Lu H, Zang M. The role of peripheral blood eosinophil counts in COVID-19 patients. Allergy. 2021;76(2):471-82. [Link] [DOI:10.1111/all.14465] [PMID] [PMCID]
22. Outh R, Boutin C, Gueudet P, Suzuki M, Saada M. Eosiopenia <100Ml as a marker of active COVID-19: An observational prospective study. J Microbiol Immunol Infect. 2021;54(1):61-8. [Link] [DOI:10.1016/j.jmii.2020.12.005] [PMID] [PMCID]
23. Khoury P, Stokes K, Gadkari M, Michelle A. Glucocorticosteroid-induce osteopenia in humans can be linked to early transcriptional events. Allergy. 2018;73(10):2076-9. [Link] [DOI:10.1111/all.13497] [PMID] [PMCID]