Volume 17, Issue 1 (2025)
Iran J War Public Health 2025, 17(1): 17-22 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2025/01/10 | Accepted: 2025/02/20 | Published: 2025/02/26
Received: 2025/01/10 | Accepted: 2025/02/20 | Published: 2025/02/26
How to cite this article
Alwatify S, Radhi M. Diabetes Self-Management and its Association with Medication Adherence in Diabetic Patients. Iran J War Public Health 2025; 17 (1) :17-22
URL: http://ijwph.ir/article-1-1560-en.html
URL: http://ijwph.ir/article-1-1560-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Authors
S.S.D. Alwatify1, M.M. Radhi *1
1- Department of Community Health Techniques, College of Health and Medical Techniques, Al-Furat Al-Awsat Technical University, Kufa, Iraq
Full-Text (HTML) (618 Views)
Introduction
Diabetes mellitus (DM) is a continual metabolic ailment characterized by persistent hyperglycemia, which may lead to severe headaches if not well managed [1]. Effective self-management of diabetes, which incorporates blood glucose tracking, nutritional modifications, physical hobbies, and remedy adherence, is critical in preventing headaches and enhancing the affected person's consequences [2]. Despite its importance, many patients fear maintaining ok self-management behaviors, especially in adhering to prescribed medications, which remains a key issue of diabetes care [3].
The interplay between self-management practices and medication adherence has drawn tremendous attention in recent years, as addressing these issues can contribute to higher glycemic management and reduced healthcare charges [4].
Previous studies have continuously highlighted the significance of medication adherence in diabetes management. According to a systematic evaluation, non-adherence to antidiabetic medicines is associated with higher dangers of complications along with cardiovascular disorders, neuropathy, and retinopathy [5]. Furthermore, previous research demonstrated that advanced medication adherence appreciably reduces hospitalization rates and improves the quality of life among diabetic sufferers. However, medicinal medication adherence is influenced by various things, including sufferers’ self-management competencies, health literacy, psychological well-being, and assistance from healthcare carriers [6-8].
Diabetes self-management, encompassing a wide range of day-by-day behaviors, has been identified as a critical determinant of medication adherence. It is suggested that patients with strong self-management capabilities are much more likely to adhere to their prescribed remedy regimens [9]. Similarly, it emphasized the role of self-efficacy in fostering medication adherence among people with type 2 diabetes [10]. These findings align with the theoretical framework of Bandura’s Social Cognitive Theory, which posits that self-efficacy and behavioral self-regulation are crucial to maintaining health-selling behaviors [11]. However, gaps remain in how particular self-management practices directly correlate with medicinal medication adherence across numerous populations and healthcare settings.
The association between diabetes self-management and medicinal medication adherence is similarly complex through socio-demographic and cultural factors. For instance, it highlighted disparities in diabetes self-management behaviors among ethnic minorities, suggesting the need for tailor-made interventions [12]. Moreover, economic constraints and the complexity of remedy regimens were recognized as limitations to adherence [13]. These challenges underscore comprehensive research's need to discover the multidimensional relationship between self-management and medicinal medication adherence, supplying insights into manual healthcare guidelines and patient-focused interventions [14].
In light of these issues, this study aimed to investigate the affiliation between diabetes self-management and medicine adherence among diabetic patients.
Instrument and Methods
Design and sampling
This cross-sectional descriptive study was conducted at Babylon Diabetes and Endocrinology Center/Iraq, from September 2024 to February 2025. The examination uses a comfort sampling method to recruit 328 patients from a goal populace of 2262, based on Cochran’s method for pattern size determination. The method calculates the pattern length for big populations and adjusts it for finite populations [15]. The participants were diabetic patients aged 18 years or older, diagnosed with type 1 or 2 diabetes, and actively receiving treatment at the Babylon Diabetes and Endocrinology Center. Patients with severe cognitive impairment or severe infection were excluded. Participants were approached during their habitual visits to the center, ensuring a diverse representation of patients dealing with diabetes via self-care and prescribed medicine regimens.
Instrument
The use of two established contraptions facilitated the data series. The Diabetes Self-Management Questionnaire (DSMQ) assessed patients’ self-management behaviors, overlaying elements, glucose management, dietary management, bodily hobby, and healthcare usage [16]. The Medication Adherence Report Scale (MARS) assessed adherence to prescribed remedy regimens [17]. Both instruments are extensively recognized for their reliability and validity in diabetes studies. A panel of experts in diabetes care and studies tested the instruments. Reliability was assessed through a pilot study involving 30 diabetic patients. The DSMQ showed a Cronbach’s alpha of 0.85 and the MARS’s alpha of 0.82, indicating strong internal consistency for each instrument.
Procedure
The data collection process spanned three months after obtaining the ethical approval and other required permissions. During this time, participants were provided with questionnaires in an independent interview format. Trained research assistants administered the instruments to reduce response bias and ensure the readability of patient responses. Demographic information, including age, gender, marital status, education level, occupation, monthly income, and duration of diabetes, was also recorded to aid in contextual analysis.
Data analysis
The collected data were entered into SPSS 29 software and analyzed using inferential tests. The Kolmogorov-Smirnov test was used to test for normality. The association between diabetes self-management and treatment adherence was analyzed using Pearson's correlation coefficient. Non-parametric analysis was performed to determine statistical differences based on sociodemographic variables. A significance level of p<0.05 was set for all statistical tests.
Findings
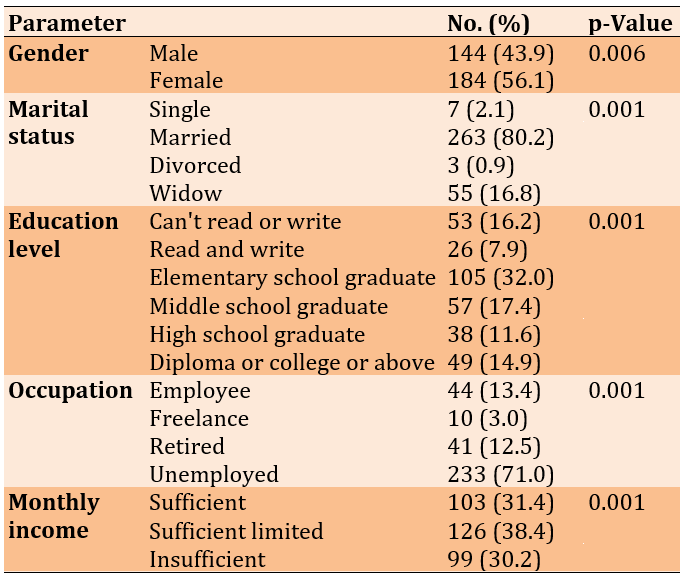
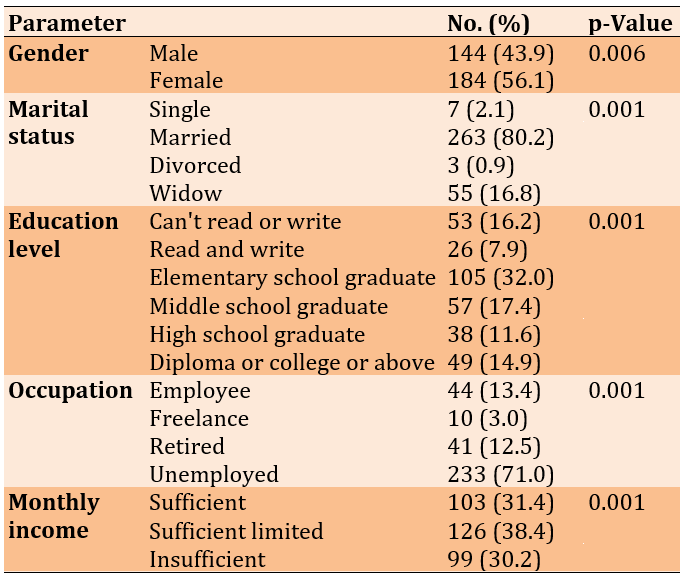
The mean age of the participants was 45.35±9.38 (21-68) years, and the mean duration of DM was 9.62±6.48 (1-28) years. There were statistically significant differences in diabetes self-management between groups of gender (p=0.006), marital status (p=0.001), education level (p=0.001), occupation (p=0.001), and monthly income (p=0.001; Table 1).
Table 1. Frequency of the socio-demographic characteristics of the study samples (n=328) and the comparison of self-management scores according to the demographic parameters
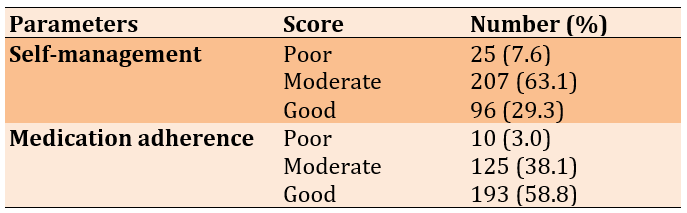
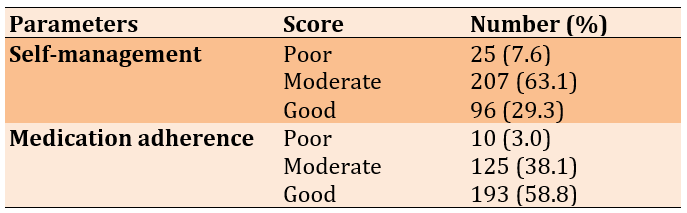
63.1% of diabetic patients expressed moderate diabetic self-management (34.44±5.35). Regarding treatment adherence, 58.8% of diabetic patients exhibited good adherence (25.87±3.36).
Table 2. Overall evaluation of study parameters
There was a positive correlation between diabetes self-management and treatment adherence among diabetic patients (r=0.622; p=0.0001). Also, there was a significant negative correlation between diabetes self-management and age (r=-0.134; p<0.05).
Every increase in diabetes self-management by +4.5691 increases the adherence to treatment by 0.9095 (Figure 1).
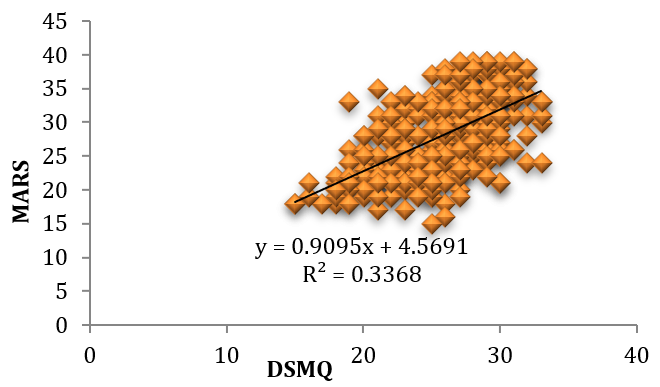
Figure 1. Relationship between DSMQ and MARS
Discussion
This study investigated the affiliation between diabetes self-management and medicine adherence among diabetic patients. The percentage of diabetic self-management is better than the findings in a study carried out in Ethiopia, wherein 84% of diabetic patients tested an insufficient level of self-management. This disparity can be attributed to variations in accessibility and the exceptionality of instructional packages that sell self-management practices to diabetic sufferers. A study in an identical vicinity shows that structured diabetes education packages considerably decorate self-management behaviors among diabetic sufferers [18]. The availability of such programs in our vicinity possibly contributed to the better fees for mild self-management. Conversely, the share of diabetic sufferers in this examination displaying a slight level of self-management is decreased than that stated in Italy, where 79.5% of patients completed this degree [19]. One feasible explanation for this discrepancy is the effect of socioeconomic elements, as highlighted by looking at equal region offers with disabilities, which noted that higher ranges of profits and training are associated with better self-management effects [20]. In comparison, the population in our study may additionally face economic or instructional demanding situations that restrict their potential to adhere to gold-standard self-management practices completely.
The treatment adherence percentage exceeds the results from Kenyatta National Hospital, where only 28.3% of diabetic patients showed correct adherence. The higher adherence rate found in our study could be attributed to strong communication between healthcare providers and patients, and a study from Thailand has also confirmed the role of effective counseling in improving adherence among diabetic patients [21]. In addition, cultural attitudes toward health and treatment compliance in our region may influence adherence behaviors. In contrast, the adherence rate in this study is lower than that documented in Riyadh, Saudi Arabia, where 80.5% of diabetic patients reported good adherence. The difference may also stem from differences in healthcare systems and patient assistance services. For example, a study in the same region reported that comprehensive follow-up and reminders significantly improved adherence rates [22].
The results of this study reveal a significant positive association between diabetes self-management and medication adherence among diabetic patients. This finding suggests that as diabetic patients engage in higher self-management practices, their chances of adhering to prescribed medications also increase. Regression analysis further supports this relationship, suggesting that for each unit increase in diabetes self-management, there may be a corresponding upward push in medication adherence. These findings are consistent with previous research and emphasize the important role of diabetes self-management in promoting adherence to medication regimens. A study conducted in Nekemte, Ethiopia, suggests that self-management behaviors, including tracking blood glucose levels, following dietary advice, and engaging in physical activity, were significantly associated with improved medication adherence among diabetic patients. This confirms that self-management promotes an empowering and habitual experience, which complements patients’ ability to follow prescribed medications [23] properly. In Canada, an observation highlighted the significance of affected persons' schooling and self-management in improving remedy adherence. The researchers observed that diabetic sufferers who participated in dependent self-management programs were substantially more likely to adhere to their medication and lifestyle modifications in comparison to folks who no longer acquired such interventions. The Canadian context specifically emphasized the position of culturally tailored schooling packages in improving self-management behaviors and adherence. These findings together aid the effects of the modern-day. They spotlight the conventional significance of diabetes self-management across numerous healthcare settings. The consistent, high-quality courting among self-management and remedy adherence emphasizes the need for healthcare providers to implement and maintain diabetes training programs that promote self-management talents. Such programs should deal with boundaries to self-management and a lack of expertise, motivation, and access to healthcare assets. Addressing these elements may notably enhance adherence costs, leading to better health consequences for diabetic patients globally [24].
The result implies that as the age of patients increases, their capacity or engagement in self-management behaviors tends to say no. This observation aligns with previous research exploring age-related factors influencing diabetes self-management. Older adults regularly face unique, demanding situations in dealing with diabetes efficiently. According to the Joslin Diabetes Center in Massachusetts, advancing age is related to a decline in bodily, cognitive, and sensory capabilities, which may additionally preclude the ability to perform vital self-care activities, which include monitoring blood glucose ranges, adhering to dietary recommendations, and engaging in normal bodily pastimes [25]. Similarly, a study carried out at Johann Wolfgang Goethe University, Germany, emphasized that older adults might struggle with the complexity of diabetes management due to comorbidities and the weight of polypharmacy, which can compromise their adherence to self-management protocols [26].
The significant difference in diabetes self-management between genders aligns with prior studies highlighting the function of gender-unique behaviors and fitness practices. For instance, a study in the Netherlands pronounced that males frequently demonstrate extra adherence to nutritional regimens and glucose monitoring protocols compared to females doubtlessly because of their better fitness in search of behaviors and engagement in caregiving roles. However, males may display better workout adherence, reflecting differing priorities and way of life alternatives. Understanding these gender-precise dispositions is essential for tailoring interventions to improve self-management consequences [27].
The extensive association between marital popularity and diabetes self-management is regular, with evidence suggesting that marital assistance is essential in handling persistent conditions. Married individuals are regularly found to have higher glycemic management because of their spouses' emotional and practical assistance, as mentioned in an observation performed in South Africa [27]. Conversely, unmarried, widowed, or divorced individuals may face extra challenges in keeping steady self-care exercises, underscoring the significance of incorporating social support mechanisms into diabetes training packages.
The finding that education level notably influences diabetes self-management is supported using preceding research demonstrating that people with better schooling levels are more prepared to recognize and implement complex self-care regimens. The Western Pacific region reported that training improves fitness literacy, enhancing people’s ability to interpret blood glucose readings, adhere to remedy schedules, and make knowledgeable nutritional selections. Targeted educational interventions for people with decreased instructional attainment may want to bridge the gap and enhance self-management practices [28].
Occupation and monthly earnings were additionally substantially related to diabetes self-management, reflecting the socioeconomic determinants of fitness. Higher-income agencies may additionally have higher admission to healthcare assets, nutritious meals, and bodily pastime facilities, as highlighted in North Carolina [29]. In contrast, people with lower incomes or unstable occupations may additionally struggle with monetary barriers, leading to compromised medicine adherence or reliance on less wholesome, cost-effective diets. These findings emphasize the need for guidelines addressing monetary disparities to ensure equitable access to diabetes management sources.
These findings together spotlight the significance of tailoring diabetes self-management applications to cope with demographic disparities. Interventions should consider gender-specific techniques, including marital and social aid, enhancing fitness literacy through centered education, and dealing with monetary obstacles. By adopting a holistic technique informed by those large demographic factors, healthcare vendors can improve diabetes self-management outcomes and decrease the burden of this chronic situation throughout numerous populations. The significant positive association between self-management and adherence highlights the importance of empowering patients through structured, culturally tailored educational programs and enhanced healthcare communication. Addressing socioeconomic disparities, strengthening age- and gender-specific interventions, and integrating social support mechanisms are crucial. Policies targeting health literacy and equitable access to resources are essential to improve diabetes outcomes comprehensively.
Conclusion
There is a moderate level of diabetes management and good adherence to treatment in Babylon province, Iraq, that vary globally due to factors such as access to healthcare, socioeconomic status, and education.
Acknowledgments: We thank the Babylon Diabetes and Endocrinology Center for allowing the research (study ID: Q.1717) and for accepting the final report of this study.
Ethical Permissions: The ethical approval was obtained from the Research Ethics Committee of the College of Health and Medical Techniques/Kufa, Al-Furat Al-Awsat Technical University (No. 217; September 29, 2024).
Conflicts of Interests: There are no conflicts of interest.
Authors' Contribution: Alwatify SSD (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (50%); Radhi MM (Second Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (50%)
Funding/Support: The College of Health and Medical Techniques-Kufa/Al-Furat Al-Awsat Technical University supported the study
Diabetes mellitus (DM) is a continual metabolic ailment characterized by persistent hyperglycemia, which may lead to severe headaches if not well managed [1]. Effective self-management of diabetes, which incorporates blood glucose tracking, nutritional modifications, physical hobbies, and remedy adherence, is critical in preventing headaches and enhancing the affected person's consequences [2]. Despite its importance, many patients fear maintaining ok self-management behaviors, especially in adhering to prescribed medications, which remains a key issue of diabetes care [3].
The interplay between self-management practices and medication adherence has drawn tremendous attention in recent years, as addressing these issues can contribute to higher glycemic management and reduced healthcare charges [4].
Previous studies have continuously highlighted the significance of medication adherence in diabetes management. According to a systematic evaluation, non-adherence to antidiabetic medicines is associated with higher dangers of complications along with cardiovascular disorders, neuropathy, and retinopathy [5]. Furthermore, previous research demonstrated that advanced medication adherence appreciably reduces hospitalization rates and improves the quality of life among diabetic sufferers. However, medicinal medication adherence is influenced by various things, including sufferers’ self-management competencies, health literacy, psychological well-being, and assistance from healthcare carriers [6-8].
Diabetes self-management, encompassing a wide range of day-by-day behaviors, has been identified as a critical determinant of medication adherence. It is suggested that patients with strong self-management capabilities are much more likely to adhere to their prescribed remedy regimens [9]. Similarly, it emphasized the role of self-efficacy in fostering medication adherence among people with type 2 diabetes [10]. These findings align with the theoretical framework of Bandura’s Social Cognitive Theory, which posits that self-efficacy and behavioral self-regulation are crucial to maintaining health-selling behaviors [11]. However, gaps remain in how particular self-management practices directly correlate with medicinal medication adherence across numerous populations and healthcare settings.
The association between diabetes self-management and medicinal medication adherence is similarly complex through socio-demographic and cultural factors. For instance, it highlighted disparities in diabetes self-management behaviors among ethnic minorities, suggesting the need for tailor-made interventions [12]. Moreover, economic constraints and the complexity of remedy regimens were recognized as limitations to adherence [13]. These challenges underscore comprehensive research's need to discover the multidimensional relationship between self-management and medicinal medication adherence, supplying insights into manual healthcare guidelines and patient-focused interventions [14].
In light of these issues, this study aimed to investigate the affiliation between diabetes self-management and medicine adherence among diabetic patients.
Instrument and Methods
Design and sampling
This cross-sectional descriptive study was conducted at Babylon Diabetes and Endocrinology Center/Iraq, from September 2024 to February 2025. The examination uses a comfort sampling method to recruit 328 patients from a goal populace of 2262, based on Cochran’s method for pattern size determination. The method calculates the pattern length for big populations and adjusts it for finite populations [15]. The participants were diabetic patients aged 18 years or older, diagnosed with type 1 or 2 diabetes, and actively receiving treatment at the Babylon Diabetes and Endocrinology Center. Patients with severe cognitive impairment or severe infection were excluded. Participants were approached during their habitual visits to the center, ensuring a diverse representation of patients dealing with diabetes via self-care and prescribed medicine regimens.
Instrument
The use of two established contraptions facilitated the data series. The Diabetes Self-Management Questionnaire (DSMQ) assessed patients’ self-management behaviors, overlaying elements, glucose management, dietary management, bodily hobby, and healthcare usage [16]. The Medication Adherence Report Scale (MARS) assessed adherence to prescribed remedy regimens [17]. Both instruments are extensively recognized for their reliability and validity in diabetes studies. A panel of experts in diabetes care and studies tested the instruments. Reliability was assessed through a pilot study involving 30 diabetic patients. The DSMQ showed a Cronbach’s alpha of 0.85 and the MARS’s alpha of 0.82, indicating strong internal consistency for each instrument.
Procedure
The data collection process spanned three months after obtaining the ethical approval and other required permissions. During this time, participants were provided with questionnaires in an independent interview format. Trained research assistants administered the instruments to reduce response bias and ensure the readability of patient responses. Demographic information, including age, gender, marital status, education level, occupation, monthly income, and duration of diabetes, was also recorded to aid in contextual analysis.
Data analysis
The collected data were entered into SPSS 29 software and analyzed using inferential tests. The Kolmogorov-Smirnov test was used to test for normality. The association between diabetes self-management and treatment adherence was analyzed using Pearson's correlation coefficient. Non-parametric analysis was performed to determine statistical differences based on sociodemographic variables. A significance level of p<0.05 was set for all statistical tests.
Findings
The mean age of the participants was 45.35±9.38 (21-68) years, and the mean duration of DM was 9.62±6.48 (1-28) years. There were statistically significant differences in diabetes self-management between groups of gender (p=0.006), marital status (p=0.001), education level (p=0.001), occupation (p=0.001), and monthly income (p=0.001; Table 1).
Table 1. Frequency of the socio-demographic characteristics of the study samples (n=328) and the comparison of self-management scores according to the demographic parameters
63.1% of diabetic patients expressed moderate diabetic self-management (34.44±5.35). Regarding treatment adherence, 58.8% of diabetic patients exhibited good adherence (25.87±3.36).
Table 2. Overall evaluation of study parameters
There was a positive correlation between diabetes self-management and treatment adherence among diabetic patients (r=0.622; p=0.0001). Also, there was a significant negative correlation between diabetes self-management and age (r=-0.134; p<0.05).
Every increase in diabetes self-management by +4.5691 increases the adherence to treatment by 0.9095 (Figure 1).
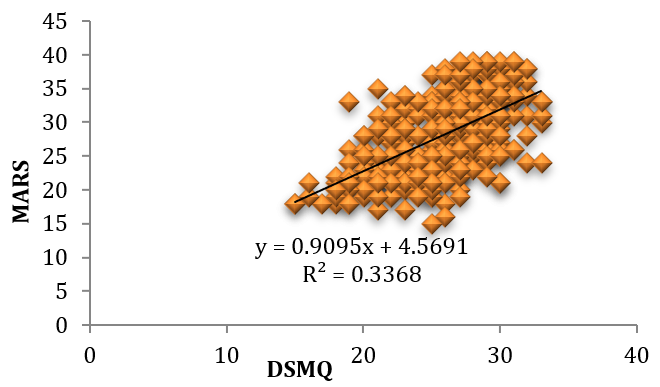
Figure 1. Relationship between DSMQ and MARS
Discussion
This study investigated the affiliation between diabetes self-management and medicine adherence among diabetic patients. The percentage of diabetic self-management is better than the findings in a study carried out in Ethiopia, wherein 84% of diabetic patients tested an insufficient level of self-management. This disparity can be attributed to variations in accessibility and the exceptionality of instructional packages that sell self-management practices to diabetic sufferers. A study in an identical vicinity shows that structured diabetes education packages considerably decorate self-management behaviors among diabetic sufferers [18]. The availability of such programs in our vicinity possibly contributed to the better fees for mild self-management. Conversely, the share of diabetic sufferers in this examination displaying a slight level of self-management is decreased than that stated in Italy, where 79.5% of patients completed this degree [19]. One feasible explanation for this discrepancy is the effect of socioeconomic elements, as highlighted by looking at equal region offers with disabilities, which noted that higher ranges of profits and training are associated with better self-management effects [20]. In comparison, the population in our study may additionally face economic or instructional demanding situations that restrict their potential to adhere to gold-standard self-management practices completely.
The treatment adherence percentage exceeds the results from Kenyatta National Hospital, where only 28.3% of diabetic patients showed correct adherence. The higher adherence rate found in our study could be attributed to strong communication between healthcare providers and patients, and a study from Thailand has also confirmed the role of effective counseling in improving adherence among diabetic patients [21]. In addition, cultural attitudes toward health and treatment compliance in our region may influence adherence behaviors. In contrast, the adherence rate in this study is lower than that documented in Riyadh, Saudi Arabia, where 80.5% of diabetic patients reported good adherence. The difference may also stem from differences in healthcare systems and patient assistance services. For example, a study in the same region reported that comprehensive follow-up and reminders significantly improved adherence rates [22].
The results of this study reveal a significant positive association between diabetes self-management and medication adherence among diabetic patients. This finding suggests that as diabetic patients engage in higher self-management practices, their chances of adhering to prescribed medications also increase. Regression analysis further supports this relationship, suggesting that for each unit increase in diabetes self-management, there may be a corresponding upward push in medication adherence. These findings are consistent with previous research and emphasize the important role of diabetes self-management in promoting adherence to medication regimens. A study conducted in Nekemte, Ethiopia, suggests that self-management behaviors, including tracking blood glucose levels, following dietary advice, and engaging in physical activity, were significantly associated with improved medication adherence among diabetic patients. This confirms that self-management promotes an empowering and habitual experience, which complements patients’ ability to follow prescribed medications [23] properly. In Canada, an observation highlighted the significance of affected persons' schooling and self-management in improving remedy adherence. The researchers observed that diabetic sufferers who participated in dependent self-management programs were substantially more likely to adhere to their medication and lifestyle modifications in comparison to folks who no longer acquired such interventions. The Canadian context specifically emphasized the position of culturally tailored schooling packages in improving self-management behaviors and adherence. These findings together aid the effects of the modern-day. They spotlight the conventional significance of diabetes self-management across numerous healthcare settings. The consistent, high-quality courting among self-management and remedy adherence emphasizes the need for healthcare providers to implement and maintain diabetes training programs that promote self-management talents. Such programs should deal with boundaries to self-management and a lack of expertise, motivation, and access to healthcare assets. Addressing these elements may notably enhance adherence costs, leading to better health consequences for diabetic patients globally [24].
The result implies that as the age of patients increases, their capacity or engagement in self-management behaviors tends to say no. This observation aligns with previous research exploring age-related factors influencing diabetes self-management. Older adults regularly face unique, demanding situations in dealing with diabetes efficiently. According to the Joslin Diabetes Center in Massachusetts, advancing age is related to a decline in bodily, cognitive, and sensory capabilities, which may additionally preclude the ability to perform vital self-care activities, which include monitoring blood glucose ranges, adhering to dietary recommendations, and engaging in normal bodily pastimes [25]. Similarly, a study carried out at Johann Wolfgang Goethe University, Germany, emphasized that older adults might struggle with the complexity of diabetes management due to comorbidities and the weight of polypharmacy, which can compromise their adherence to self-management protocols [26].
The significant difference in diabetes self-management between genders aligns with prior studies highlighting the function of gender-unique behaviors and fitness practices. For instance, a study in the Netherlands pronounced that males frequently demonstrate extra adherence to nutritional regimens and glucose monitoring protocols compared to females doubtlessly because of their better fitness in search of behaviors and engagement in caregiving roles. However, males may display better workout adherence, reflecting differing priorities and way of life alternatives. Understanding these gender-precise dispositions is essential for tailoring interventions to improve self-management consequences [27].
The extensive association between marital popularity and diabetes self-management is regular, with evidence suggesting that marital assistance is essential in handling persistent conditions. Married individuals are regularly found to have higher glycemic management because of their spouses' emotional and practical assistance, as mentioned in an observation performed in South Africa [27]. Conversely, unmarried, widowed, or divorced individuals may face extra challenges in keeping steady self-care exercises, underscoring the significance of incorporating social support mechanisms into diabetes training packages.
The finding that education level notably influences diabetes self-management is supported using preceding research demonstrating that people with better schooling levels are more prepared to recognize and implement complex self-care regimens. The Western Pacific region reported that training improves fitness literacy, enhancing people’s ability to interpret blood glucose readings, adhere to remedy schedules, and make knowledgeable nutritional selections. Targeted educational interventions for people with decreased instructional attainment may want to bridge the gap and enhance self-management practices [28].
Occupation and monthly earnings were additionally substantially related to diabetes self-management, reflecting the socioeconomic determinants of fitness. Higher-income agencies may additionally have higher admission to healthcare assets, nutritious meals, and bodily pastime facilities, as highlighted in North Carolina [29]. In contrast, people with lower incomes or unstable occupations may additionally struggle with monetary barriers, leading to compromised medicine adherence or reliance on less wholesome, cost-effective diets. These findings emphasize the need for guidelines addressing monetary disparities to ensure equitable access to diabetes management sources.
These findings together spotlight the significance of tailoring diabetes self-management applications to cope with demographic disparities. Interventions should consider gender-specific techniques, including marital and social aid, enhancing fitness literacy through centered education, and dealing with monetary obstacles. By adopting a holistic technique informed by those large demographic factors, healthcare vendors can improve diabetes self-management outcomes and decrease the burden of this chronic situation throughout numerous populations. The significant positive association between self-management and adherence highlights the importance of empowering patients through structured, culturally tailored educational programs and enhanced healthcare communication. Addressing socioeconomic disparities, strengthening age- and gender-specific interventions, and integrating social support mechanisms are crucial. Policies targeting health literacy and equitable access to resources are essential to improve diabetes outcomes comprehensively.
Conclusion
There is a moderate level of diabetes management and good adherence to treatment in Babylon province, Iraq, that vary globally due to factors such as access to healthcare, socioeconomic status, and education.
Acknowledgments: We thank the Babylon Diabetes and Endocrinology Center for allowing the research (study ID: Q.1717) and for accepting the final report of this study.
Ethical Permissions: The ethical approval was obtained from the Research Ethics Committee of the College of Health and Medical Techniques/Kufa, Al-Furat Al-Awsat Technical University (No. 217; September 29, 2024).
Conflicts of Interests: There are no conflicts of interest.
Authors' Contribution: Alwatify SSD (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (50%); Radhi MM (Second Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (50%)
Funding/Support: The College of Health and Medical Techniques-Kufa/Al-Furat Al-Awsat Technical University supported the study
Keywords:
References
1. Balaji R, Duraisamy R, Kumar MP. Complications of diabetes mellitus: A review. Drug Invent Today. 2019;12(1):98-103. [Link]
2. Al-Eqabi QAK, Niazy SM, Radhi MM. Effectiveness of digital health interventions in managing glycated hemoglobin: A randomized management led trial. Natl J Community Med. 2024;15(9):747-53. [Link]
3. Radhi MM. Degree of disease acceptance and health-seeking behaviors for type 2 diabetic patients at diabetic center in Hilla City. Medico Leg Update. 2020;20(2):853-8. [Link] [DOI:10.37506/mlu.v20i2.1347]
4. Radhi MM, Zair Balat K. Health literacy and its association with medication adherence in patients with hypertension: A mediating role of social support. Iran Rehabil J. 2024;22(1):117-28. [Link] [DOI:10.32598/irj.22.1.1989.1]
5. Azharuddin M, Adil M, Sharma M, Gyawali B. A systematic review and meta‐analysis of non‐adherence to anti‐diabetic medication: Evidence from low‐and middle‐income countries. Int J Clin Pract. 2021;75(11):e14717. [Link] [DOI:10.1111/ijcp.14717]
6. Radhi MM, Niazy SM, Abed SN. Individual-related factors associated with treatment adherence among hypertensive patients. J Public Health Afr. 2023;14(6):2466. [Link] [DOI:10.4081/jphia.2023.2466]
7. Khazew HR, Faraj RK. Illness acceptance and its relationship to health-behaviors among patients with type 2 diabetes: A mediating role of self-hardiness. Curr Probl Cardiol. 2024;49(8):102606. [Link] [DOI:10.1016/j.cpcardiol.2024.102606]
8. Qassim WJ, Yasir AA, Radhi MM. Assessment of self hardness and its relationship to treatment acceptance for patients with diabetes mellitus at diabetic center in Hilla City/Iraq. J Pharm Sci Res. 2018;10(1):142-5. [Link]
9. Husdal R, Thors Adolfsson E, Leksell J, Nordgren L. Diabetes care provided by national standards can improve patients' self‐management skills: A qualitative study of how people with type 2 diabetes perceive primary diabetes care. Health Expect. 2021;24(3):1000-8. [Link] [DOI:10.1111/hex.13247]
10. Huang YM, Shiyanbola OO, Chan HY. A path model linking health literacy, medication self-efficacy, medication adherence, and glycemic management. Patient Educ Couns. 2018;101(11):1906-13. [Link] [DOI:10.1016/j.pec.2018.06.010]
11. Bandura A. Social foundations of thought and action. Englewood Cliffs: Prentice Hall; 1986. [Link]
12. Xie Z, Liu K, Or C, Chen J, Yan M, Wang H. An examination of the socio-demographic correlates of patient adherence to self-management behaviors and the mediating roles of health attitudes and self-efficacy among patients with coexisting type 2 diabetes and hypertension. BMC Public Health. 2020;20(1):1227. [Link] [DOI:10.1186/s12889-020-09274-4]
13. Radhi MM, Al-Eqabi QA, Hindi NK. Rehabilitation problems of people with motor disabilities at Babylon center for rehabilitation of the disabled. Med J Babylon. 2023;20(4):838-43. [Link] [DOI:10.4103/MJBL.MJBL_674_23]
14. Elywy GJ, Radhi MM, AlEqabi QA. Relationship between social support and self-hardiness among breast cancer women in Nasiriyah, Iraq. J Pak Med Assoc. 2023;73(9):S9-14. [Link] [DOI:10.47391/JPMA.IQ-02]
15. Balat KZ, Laftah SA, Radhi M. The relationship between psychological distress and quality of life among women undergoing mastectomy in Iraq: A descriptive correlational study. Natl J Community Med. 2025;16(1):20-7. [Link] [DOI:10.55489/njcm.160120254716]
16. Schmitt A, Gahr A, Hermanns N, Kulzer B, Huber J, Haak T. The diabetes self-management questionnaire (DSMQ): Development and evaluation of an instrument to assess diabetes self-care activities associated with glycaemic management. Health Qual Life Outcomes. 2013;11:138. [Link] [DOI:10.1186/1477-7525-11-138]
17. Alsous M, Alhalaiqa F, Abu Farha R, Abdel Jalil M, McElnay J, Horne R. Reliability and validity of Arabic translation of Medication Adherence Report Scale (MARS) and Beliefs about Medication Questionnaire (BMQ)-specific for use in children and their parents. PLoS One. 2017;12(2):e0171863. [Link] [DOI:10.1371/journal.pone.0171863]
18. Dedefo MG, Ejeta BM, Wakjira GB, Mekonen GF, Labata BG. Self-care practices regarding diabetes among diabetic patients in West Ethiopia. BMC Res Notes. 2019;12(1):212. [Link] [DOI:10.1186/s13104-019-4258-4]
19. Al-Eqabi QA, Niazy SM, Radhi MM. Amputation-related factors influencing activities of daily living among amputees. Iran J War Public Health. 2024;16(2):123-9. [Link]
20. Malih Radhi M, Juma Elywy G, Al-Eqabi AK. Burdens among wives of disabled people in the light of some social variables. Iran Rehabil J. 2023;21(3):473-84. [Link] [DOI:10.32598/irj.21.3.1765.3]
21. Wungrath J, Autorn N. Effectiveness of Line application and telephone-based counseling to improve medication adherence: A randomized control trial study among uncontrolled type 2 diabetes patients. Health Promot Perspect. 2021;11(4):438-43. [Link] [DOI:10.34172/hpp.2021.55]
22. Alqarni AM, Alrahbeni T, Qarni AA, Qarni HM. Adherence to diabetes medication among diabetic patients in the Bisha governorate of Saudi Arabia-a cross-sectional survey. Patient Prefer Adherence. 2018;13:63-71. [Link] [DOI:10.2147/PPA.S176355]
23. Oluma A, Mosisa G, Abadiga M, Tsegaye R, Habte A, Abdissa E. Predictors of adherence to self-care behavior among patients with diabetes at public hospitals in West Ethiopia. Diabetes Metab Syndr Obes. 2020;13:3277-88. [Link] [DOI:10.2147/DMSO.S266589]
24. Hester KL, Newton J, Rapley T, De Soyza A. Patient information, education and self-management in bronchiectasis: Facilitating improvements to optimise health outcomes. BMC Pulm Med. 2018;18(1):80. [Link] [DOI:10.1186/s12890-018-0633-5]
25. Munshi MN. Continuous glucose monitoring use in older adults for optimal diabetes management. Diabetes Technol Ther. 2023;25(S3):S56-64. [Link] [DOI:10.1089/dia.2023.0111]
26. Muth C, Blom JW, Smith SM, Johnell K, Gonzalez‐Gonzalez AI, Nguyen TS, et al. Evidence supporting the best clinical management of patients with multimorbidity and polypharmacy: A systematic guideline review and expert consensus. J Intern Med. 2019;285(3):272-88. [Link] [DOI:10.1111/joim.12842]
27. Mutyambizi C, Pavlova M, Hongoro C, Groot W. Inequalities and factors associated with adherence to diabetes self-care practices amongst patients at two public hospitals in Gauteng, South Africa. BMC Endocr Disord. 2020;20:15. [Link] [DOI:10.1186/s12902-020-0492-y]
28. Mohamed A, Staite E, Ismail K, Winkley K. A systematic review of diabetes self‐management education interventions for people with type 2 diabetes mellitus in the Asian Western Pacific (AWP) region. Nurs Open. 2019;6(4):1424-37. [Link] [DOI:10.1002/nop2.340]
29. Armstrong S, Wong CA, Perrin E, Page S, Sibley L, Skinner A. Association of physical activity with income, race/ethnicity, and sex among adolescents and young adults in the United States: Findings from the national health and nutrition examination survey, 2007-2016. JAMA Pediatr. 2018;172(8):732-40. [Link] [DOI:10.1001/jamapediatrics.2018.1273]