Volume 16, Issue 4 (2024)
Iran J War Public Health 2024, 16(4): 369-374 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2024/10/16 | Accepted: 2024/11/27 | Published: 2024/12/5
Received: 2024/10/16 | Accepted: 2024/11/27 | Published: 2024/12/5
How to cite this article
Mohsin T, Hussein G, Hummadi M, Abass H. The Quality of Life of Post-Hernioplasty Inguinodynia Patients in Kut, Iraq. Iran J War Public Health 2024; 16 (4) :369-374
URL: http://ijwph.ir/article-1-1513-en.html
URL: http://ijwph.ir/article-1-1513-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
1- Department of Anesthesia Techniques, Kut University College, Wasit, Iraq
Full-Text (HTML) (446 Views)
Introduction
Inguinal hernia is considered the most common type of abdominal hernia, with approximately 20 million people undergoing surgery for its treatment worldwide each year [1]. This condition is more prevalent among young men and is frequently observed in manual laborers and individuals from lower socioeconomic backgrounds [2]. Several factors contribute to the development of inguinal hernias, including aging, reduced physical activity, smoking, muscle weakness due to previous surgeries [1], connective tissue disorders [3], and increased intra-abdominal pressure. This pressure may arise from chronic coughing, prolonged constipation, or other gastrointestinal issues, leading to hernia formation.
One of the complications reported after inguinal hernia surgery is the occurrence of chronic pain and discomfort in the groin area [4]. Studies estimate that its prevalence varies between 0% and 53%, significantly affecting patients’ quality of life [5]. Some individuals experience persistent pain following surgery, which intensifies with daily activities such as prolonged standing, heavy lifting, or even coughing. This pain may result from inflammatory changes, nerve damage, or the body's reaction to the mesh used in the procedure. In certain cases, patients may feel discomfort long after surgery, leading to mobility restrictions and a decreased ability to perform routine tasks. This highlights the importance of identifying and effectively managing post-surgical complications to prevent long-term patient issues [1, 2].
Chronic groin pain (Inguinodynia) following inguinal hernia repair is a significant, though sometimes underreported [6], concern [7]. Mild transient soreness lasting several days is common following mesh inguinal hernia repair [8]. However, moderate to severe pain persisting for more than three months after inguinal herniorrhaphy should be considered abnormal [9]. Approximately 10% of patients experience increased pain following hernia surgery. This persistent chronic pain is often associated with the use of open inguinal surgical techniques combined with heavyweight mesh, pre-existing severe pain before surgery, and younger age [10]. Prosthetic mesh materials, such as nonabsorbable polypropylene commonly used in hernia repair, have been linked to physiological reactions that lead to discomfort, pain, and heaviness in the groin area [11]. However, introducing lighter mesh materials, such as lightweight Prolene mesh, has significantly reduced post-surgical pain and associated groin symptoms [10].
The principal etiologies of chronic groin pain are classified as neuropathic, stemming from damage to the inguinal nerve(s), or non-neuropathic, linked to mesh or other associated diseases. Chronic groin pain can be incapacitating and may include paresthesia [12, 13], neuralgia [14], hypoesthesia [15], and hyperesthesia [16]. Patients may encounter employment incapacity, limited physical and social engagement, sleep disturbances, and psychological distress [17, 18].
Inguinodynia is generally classified as neuropathic pain or non-neuropathic pain, with the latter being inflammatory or nociceptive [19, 20]. The nerves most impacted during hernioplasty include the ilioinguinal nerve, the vaginal branch of the genitofemoral nerve, and the iliohypogastric nerve. These nerves are designated as border nerves due to their location at the junction of the lower abdomen and the groin [21-23].
Chronic post-hernioplasty pain is defined as pain that endures beyond the typical healing period, lasting a minimum of 3 months, necessitating the exclusion of alternative pain sources, particularly those arising from pre-existing conditions before the surgery [24, 25]. The etiology and mechanisms of chronic pain following hernioplasty are intricate and encompass various pain types: neuropathic, non-neuropathic [26], somatic, and visceral pain. Neuropathic pain (NP) following inguinal hernia repair (IHR) arises from a lesion impacting the somatosensory system [25], particularly due to direct injury to the inguinal nerves. Common sources of discomfort include hernia recurrence, nociceptive issues (tissue inflammation and meshoma) [27], and neuropathic factors (direct nerve injury or perineural scarring) [28]. During hernioplasty, the ilioinguinal nerve, iliohypogastric nerve, and the genital branch of the genitofemoral nerve traversing the surgical field may be subjected to stretching, entrapment, compression, thermal injury [29], or transection. The most frequently observed lesions are compression resulting from sutures, staples [30], mesh-associated fibrosis or meshoma, and transection of susceptible nerves [31]. The entrapped nerve segment may experience venous stasis, intra- and perineural edema, ischemia, and ultimately, fibrosis and scar tissue development [32]. Furthermore, peripheral nerve injuries can result in the development of two varieties of neuromas: Neuroma in continuity, which typically encompasses all levels of nerve injury, ranging from normal to neurotmesis, and end-bulb neuroma, which arises wherever a nerve is entirely severed and lacks opposing neural tissue [7, 33]. Conversely, the interaction between peripheral nerve tissue and polypropylene mesh induces a persistent inflammatory response, axonal dilation, myelin degeneration, endoneurial edema accompanied by thickening of the endoneurium and perineurium [27], separation of myelin layers, and fibrosis, potentially resulting in peripheral neuropathy [24-26].
The health problem came from the nerve injuries that resulted from the resection performed in neurons during the hernioplasty surgery, which led to chronic groin pain from this nerve injury [14, 19].
The general health, mental, and social states of patients following hernioplastic surgery were referred to as post-hernioplasty quality of life. Severe chronic pain after hernia surgery can have profound effects on a patient’s overall well-being. It limits physical activity and negatively impacts professional life by reducing work efficiency and, in some cases, making it impossible for patients to continue their jobs. Additionally, persistent pain can disrupt social interactions, preventing individuals from engaging in recreational activities and social gatherings and even fulfilling family responsibilities. In more severe cases, chronic pain can contribute to psychological distress, including anxiety and depression, further diminishing the patient’s quality of life [1, 34]. Given these challenges, effective pain management strategies following hernia surgery are essential to help patients regain their normal lifestyle and overall functionality.
In many cases, improvement in the patient's pain relief and the ability to restore the body's energetic functions was observed [14, 25]. Thus, this study aimed to assess the impact of post-hernioplasty inguinodynia on quality of life and pain manifestation.
Instrument and Methods
Design & sampling
This case-series study was conducted in the General Surgery Clinics of Alkarama Teaching Hospital in Kut, Iraq, from January 2023 to May 2024. All patients who visited the clinics throughout the time and developed inguinodynia after hernioplasty was considered the study population. One hundred forty-seven patients who accepted the invitation were chosen for the study. The samples shouldn’t have any history of any chronic illnesses.
Tools
The SF-36 quality-of-life assessment scale, as reported and modified by Adke et al. [35], was used to measure and assess the quality-of-life following hernioplasty. Additionally, cases were surveyed regarding vitality, physical functioning, bodily pain, general health perception, and social role functioning. While the general groin pain was measured according to the Copenhagen Hip and Groin Outcome Score (HAGOS), it is a primary outcome measure equally important to quality of life [36]. As well as paresthesia, neuralgia, hypoesthesia, and hyperesthesia were assessed for the symptoms of post-hernioplasty among cases.
Procedure
Following IRB permission from the board of the chosen hospital, all necessary data were gathered, including quality of life information, complete blood count values, and persistent groin pain complaints following hernioplasty. Then, all complete reports were extracted in an Excel sheet to be analyzed using suitable statistical analysis. All data were kept for the researcher without personal data, keeping patients anonymous.
Statistical analysis
SPSS 27 software was used to analyze the collected data. Descriptive statistics (mean, frequencies, percentages, and standard deviations) were obtained with suitable tools. ANOVA and unpaired t-test were used to analyze inferential statistical data.
Findings
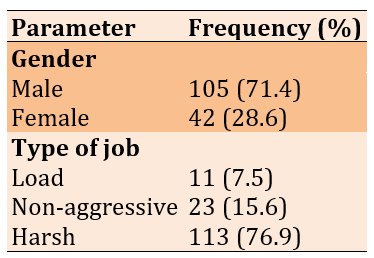
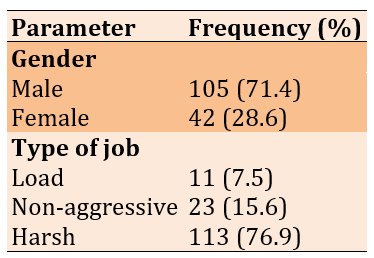
The mean age of the participants was 51.2±1.9 years and the majority were males (71.4%) and had harsh-type jobs (76.9%; Table 1).
Table 1. The frequency of demographic data of the participants
The Hemoglobin mean was 10.6±2.6g/dL, the White Blood Cells mean was 45.0±1.2U/L, PT mean was 11.4±2.3sec, and PTT mean was 12.3±4.1sec.
The most satisfied quality-of-life parameters were vitality (n=213), bodily pain (n=78), physical functioning (n=61), social role functioning (n=31), and general health perception (n=24). Hyperesthesia was the most common symptom of post-hernioplasty (n=112), and paresthesia (n=25), neuralgia (n=11), and hypoesthesia (n=3) were less common.
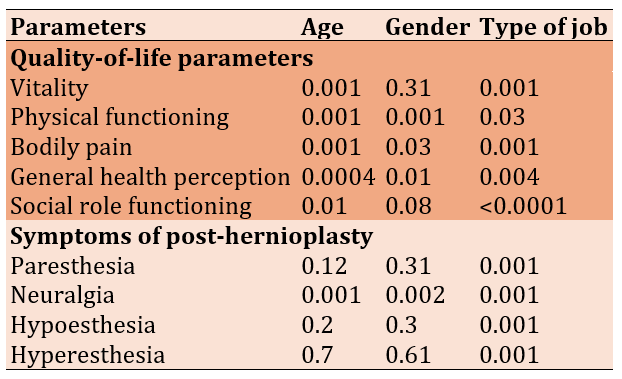
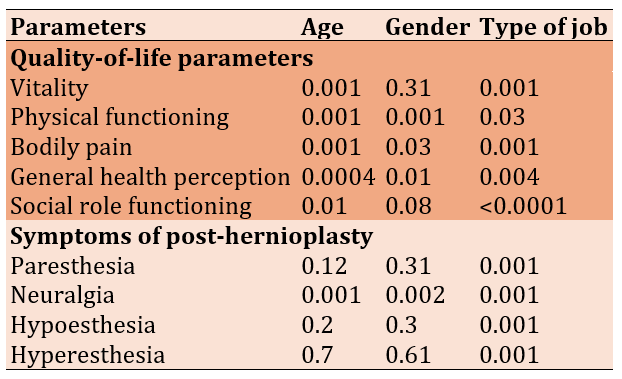
There were significant correlations between age and all quality-of-life parameters, while gender significantly correlated to all quality-of-life parameters except vitality. The type of job was strongly correlated with all quality-of-life parameters. Job type had significant correlations with all symptoms of post-hernioplasty, while gender and age significantly correlated only with neuralgia (Table 2).
Table 2. The correlation of demographic characteristics with quality-of-life parameters and the symptoms of post-hernioplasty (ANOVA)
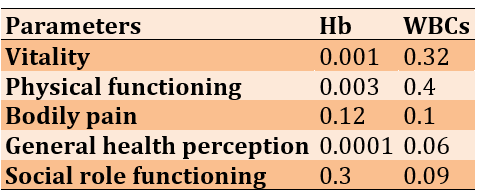
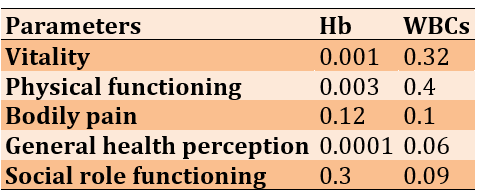
The correlation between quality-of-life parameters and the remarked laboratory markers (Hb and WBCs) showed a significant correlation to only vitality, physical functioning, and general health perception (p<0.01). Meanwhile, WBCs showed no significant correlation with all quality-of-life parameters (Table 3).
Table 3. The laboratory markers' relationship to quality-of-life parameters (t-test)
Discussion
One of the most commonly used surgical procedures for treating inguinal hernia is hernioplasty. This procedure is widely performed due to its effectiveness in repairing the hernia; however, it is not without complications. Patients undergoing hernioplasty may experience a range of post-operative issues that can significantly impact their quality of life. These include persistent pain, limited mobility, and sensory disturbances, which can contribute to discomfort and interfere with daily activities. Additionally, factors such as surgical technique, patient demographics, and occupational demands may play a role in determining post-operative recovery outcomes. Given the potential long-term consequences of post-hernioplasty complications, this study aims to evaluate the quality of life in patients who developed inguinodynia following a hernioplastic procedure. A thorough assessment of their physical, psychological, and occupational challenges can provide valuable insights into the post-surgical experience and guide future improvements in patient care.
The study included 147 randomly selected cases of patients who had previously undergone hernioplasty. Most participants were male (n=105, 71.4%), with a mean age of 51.2±1.9 years. A significant proportion of the participants (n=113, 76.9%) were employed in physically demanding jobs, which may have played a role in the hernia's development and their post-operative recovery. Patients working in harsh environments often engage in repetitive heavy lifting, prolonged standing, or strenuous manual labor, which can exert excessive strain on the abdominal muscles, potentially affecting the durability of the surgical repair and prolonging recovery.
Laboratory analysis was conducted to assess hematological and coagulation parameters among the participants. The mean hemoglobin (Hb) level was recorded at 10.6±2.6 g/dL, while the prothrombin time (PT) averaged 11.4±2.3 seconds, and the partial thromboplastin time (PTT) was 12.3±4.1 seconds. These findings align with the study conducted by Chibata & Daronch, which reported that 49 out of 313 patients (15.65%) who underwent open inguinal hernioplasty exhibited issues related to low hemoglobin levels and altered coagulation markers, particularly PT [7]. Reduced hemoglobin levels in post-hernioplasty patients may indicate intraoperative blood loss, nutritional deficiencies, or chronic disease, negatively impacting wound healing and overall recovery. Additionally, prolonged PT and PTT values may suggest underlying coagulation abnormalities, increasing the risk of post-surgical hematomas or excessive bleeding.
To assess the impact of hernioplasty on patients' quality of life, five main parameters were evaluated. The findings revealed that most participants reported high satisfaction with their surgical outcomes (n=213). However, the lowest satisfaction scores were observed in the general health perception category (n=24). This pattern of responses is consistent with the findings of Iftikhar & Kerawala, who conducted a study on 88 patients and found that a significant proportion experienced a high level of satisfaction with their post-operative quality of life [1]. Similarly, Huang et al. examined 183 patients and reported that most of them exhibited an improved quality of life following hernioplasty [37]. These results underscore the importance of managing patient expectations and implementing post-operative care strategies to enhance general health perception, pain management, and psychological well-being.
A detailed evaluation of post-hernioplasty symptoms was conducted to identify common post-surgical complications. The most frequently reported symptom was hyperesthesia, affecting 112 cases, while only three patients experienced hypoesthesia. These findings agree with the study by Falzone et al., who assessed 266 patients during their initial outpatient follow-up visit and found that all cases exhibited hyperesthesia and neuralgia, specifically involving the ilioinguinal and iliohypogastric nerves [38]. The presence of hyperesthesia and neuralgia suggests that nerve irritation or damage may play a crucial role in the post-operative symptomatology of hernioplasty patients. Given that nerve-related complications are among the most common causes of post-surgical pain, future research should explore surgical techniques that minimize nerve trauma to improve patient outcomes.
Statistical analysis using the ANOVA test demonstrated a significant correlation between age and all quality-of-life parameters (p<0.01). The highest F value was observed for bodily pain (3.41), indicating that older patients were more likely to experience post-operative discomfort. Gender was also significantly correlated with all quality-of-life parameters except vitality (p>0.05). Furthermore, occupational factors were strongly correlated with quality-of-life measures, with general health perception showing the highest F value (4.34). These findings are supported by research conducted by Bona et al. [39] and Moreton & Truter, both of whom reported a strong correlation between patients' quality of life and post-hernioplasty symptoms (p<0.001) [40]. These results emphasize the importance of considering demographic and occupational factors when developing post-operative rehabilitation programs.
A comparative analysis of post-hernioplasty symptoms revealed a significant association between job type and all reported symptoms (p=0.001). Gender and age were specifically associated with neuralgia (p=0.001 and 0.002, respectively). These findings are consistent with research by Pinto et al., who used multivariate hierarchical regression analysis to examine predictors of post-hernioplasty symptoms in 135 patients. Their study identified younger age, strenuous work environments, preoperative anxiety, and chronic pain as significant risk factors for postoperative complications [42]. These findings highlight the need for preoperative counseling and tailored post-operative care strategies to address the specific risks associated with individual patient demographics and occupational conditions.
The relationship between quality-of-life parameters and laboratory markers was also examined. Hemoglobin levels and white blood cell (WBC) counts were significantly correlated with vitality, physical functioning, and general health perception (p<0.01). However, WBC counts did not significantly correlate with any of the quality-of-life parameters. These findings align with research by Bona et al., who reported that physical functioning and general health perception were significantly related to hemoglobin levels, which tend to decline after hernioplasty [39]. This suggests that monitoring and managing hemoglobin levels post-operatively may be beneficial in optimizing recovery and improving overall well-being in patients undergoing hernioplasty.
Further comparisons between surgical techniques indicate that laparoscopic total extraperitoneal (TEP) hernia repair is associated with less early postoperative pain than open mesh fixation techniques. One study found that TEP repair resulted in a more comfortable recovery, with reduced rates of neuralgia and hyperesthesia [41]. Additionally, studies comparing open Lichtenstein repair to laparoscopic TEP repair suggest that while recurrence rates may be similar between the two techniques, laparoscopic repair is associated with a quicker return to daily activities and improved post-operative comfort [1]. These findings suggest that minimally invasive techniques may offer advantages in pain reduction and faster rehabilitation, making them a preferred option in certain patient populations. Despite the overall positive impact of hernioplasty on quality of life, this study underscores the need for continued efforts to minimize post-surgical complications, including chronic pain, and to address potential factors like low hemoglobin levels that may affect overall well-being following hernioplasty.
Conclusion
Patients generally experience a high degree of quality of life after hernioplasty, with a reduction in symptom severity, including chronic pain. However, lower hemoglobin levels are observed in some patients, potentially impacting their general health perception.
Acknowledgments: The authors declared no acknowledgement.
Ethical Permissions: An IRB approval was obtained with number 311ac-A3 from the selected hospital in Kut, Iraq.
Conflicts of Interests: The authors declare no conflict of interests.
Authors' Contribution: Mohsin TS (First Author), Introduction Writer/Methodologist/Main or Assistant Researcher/Discussion Writer/Statistical Analyst (25%); Hussein GH (Second Author), Introduction Writer/Methodologist/ Main or Assistant Researcher/Discussion Writer/Statistical Analyst (25%); Hummadi MM (Third Author), Introduction Writer/Methodologist/ Main or Assistant Researcher/Discussion Writer/Statistical Analyst (25%); Abass HKA (Fourth Author), Introduction Writer/Methodologist/ Main or Assistant Researcher/Discussion Writer/Statistical Analyst (25%)
Funding/Support: The authors declared no funding.
Inguinal hernia is considered the most common type of abdominal hernia, with approximately 20 million people undergoing surgery for its treatment worldwide each year [1]. This condition is more prevalent among young men and is frequently observed in manual laborers and individuals from lower socioeconomic backgrounds [2]. Several factors contribute to the development of inguinal hernias, including aging, reduced physical activity, smoking, muscle weakness due to previous surgeries [1], connective tissue disorders [3], and increased intra-abdominal pressure. This pressure may arise from chronic coughing, prolonged constipation, or other gastrointestinal issues, leading to hernia formation.
One of the complications reported after inguinal hernia surgery is the occurrence of chronic pain and discomfort in the groin area [4]. Studies estimate that its prevalence varies between 0% and 53%, significantly affecting patients’ quality of life [5]. Some individuals experience persistent pain following surgery, which intensifies with daily activities such as prolonged standing, heavy lifting, or even coughing. This pain may result from inflammatory changes, nerve damage, or the body's reaction to the mesh used in the procedure. In certain cases, patients may feel discomfort long after surgery, leading to mobility restrictions and a decreased ability to perform routine tasks. This highlights the importance of identifying and effectively managing post-surgical complications to prevent long-term patient issues [1, 2].
Chronic groin pain (Inguinodynia) following inguinal hernia repair is a significant, though sometimes underreported [6], concern [7]. Mild transient soreness lasting several days is common following mesh inguinal hernia repair [8]. However, moderate to severe pain persisting for more than three months after inguinal herniorrhaphy should be considered abnormal [9]. Approximately 10% of patients experience increased pain following hernia surgery. This persistent chronic pain is often associated with the use of open inguinal surgical techniques combined with heavyweight mesh, pre-existing severe pain before surgery, and younger age [10]. Prosthetic mesh materials, such as nonabsorbable polypropylene commonly used in hernia repair, have been linked to physiological reactions that lead to discomfort, pain, and heaviness in the groin area [11]. However, introducing lighter mesh materials, such as lightweight Prolene mesh, has significantly reduced post-surgical pain and associated groin symptoms [10].
The principal etiologies of chronic groin pain are classified as neuropathic, stemming from damage to the inguinal nerve(s), or non-neuropathic, linked to mesh or other associated diseases. Chronic groin pain can be incapacitating and may include paresthesia [12, 13], neuralgia [14], hypoesthesia [15], and hyperesthesia [16]. Patients may encounter employment incapacity, limited physical and social engagement, sleep disturbances, and psychological distress [17, 18].
Inguinodynia is generally classified as neuropathic pain or non-neuropathic pain, with the latter being inflammatory or nociceptive [19, 20]. The nerves most impacted during hernioplasty include the ilioinguinal nerve, the vaginal branch of the genitofemoral nerve, and the iliohypogastric nerve. These nerves are designated as border nerves due to their location at the junction of the lower abdomen and the groin [21-23].
Chronic post-hernioplasty pain is defined as pain that endures beyond the typical healing period, lasting a minimum of 3 months, necessitating the exclusion of alternative pain sources, particularly those arising from pre-existing conditions before the surgery [24, 25]. The etiology and mechanisms of chronic pain following hernioplasty are intricate and encompass various pain types: neuropathic, non-neuropathic [26], somatic, and visceral pain. Neuropathic pain (NP) following inguinal hernia repair (IHR) arises from a lesion impacting the somatosensory system [25], particularly due to direct injury to the inguinal nerves. Common sources of discomfort include hernia recurrence, nociceptive issues (tissue inflammation and meshoma) [27], and neuropathic factors (direct nerve injury or perineural scarring) [28]. During hernioplasty, the ilioinguinal nerve, iliohypogastric nerve, and the genital branch of the genitofemoral nerve traversing the surgical field may be subjected to stretching, entrapment, compression, thermal injury [29], or transection. The most frequently observed lesions are compression resulting from sutures, staples [30], mesh-associated fibrosis or meshoma, and transection of susceptible nerves [31]. The entrapped nerve segment may experience venous stasis, intra- and perineural edema, ischemia, and ultimately, fibrosis and scar tissue development [32]. Furthermore, peripheral nerve injuries can result in the development of two varieties of neuromas: Neuroma in continuity, which typically encompasses all levels of nerve injury, ranging from normal to neurotmesis, and end-bulb neuroma, which arises wherever a nerve is entirely severed and lacks opposing neural tissue [7, 33]. Conversely, the interaction between peripheral nerve tissue and polypropylene mesh induces a persistent inflammatory response, axonal dilation, myelin degeneration, endoneurial edema accompanied by thickening of the endoneurium and perineurium [27], separation of myelin layers, and fibrosis, potentially resulting in peripheral neuropathy [24-26].
The health problem came from the nerve injuries that resulted from the resection performed in neurons during the hernioplasty surgery, which led to chronic groin pain from this nerve injury [14, 19].
The general health, mental, and social states of patients following hernioplastic surgery were referred to as post-hernioplasty quality of life. Severe chronic pain after hernia surgery can have profound effects on a patient’s overall well-being. It limits physical activity and negatively impacts professional life by reducing work efficiency and, in some cases, making it impossible for patients to continue their jobs. Additionally, persistent pain can disrupt social interactions, preventing individuals from engaging in recreational activities and social gatherings and even fulfilling family responsibilities. In more severe cases, chronic pain can contribute to psychological distress, including anxiety and depression, further diminishing the patient’s quality of life [1, 34]. Given these challenges, effective pain management strategies following hernia surgery are essential to help patients regain their normal lifestyle and overall functionality.
In many cases, improvement in the patient's pain relief and the ability to restore the body's energetic functions was observed [14, 25]. Thus, this study aimed to assess the impact of post-hernioplasty inguinodynia on quality of life and pain manifestation.
Instrument and Methods
Design & sampling
This case-series study was conducted in the General Surgery Clinics of Alkarama Teaching Hospital in Kut, Iraq, from January 2023 to May 2024. All patients who visited the clinics throughout the time and developed inguinodynia after hernioplasty was considered the study population. One hundred forty-seven patients who accepted the invitation were chosen for the study. The samples shouldn’t have any history of any chronic illnesses.
Tools
The SF-36 quality-of-life assessment scale, as reported and modified by Adke et al. [35], was used to measure and assess the quality-of-life following hernioplasty. Additionally, cases were surveyed regarding vitality, physical functioning, bodily pain, general health perception, and social role functioning. While the general groin pain was measured according to the Copenhagen Hip and Groin Outcome Score (HAGOS), it is a primary outcome measure equally important to quality of life [36]. As well as paresthesia, neuralgia, hypoesthesia, and hyperesthesia were assessed for the symptoms of post-hernioplasty among cases.
Procedure
Following IRB permission from the board of the chosen hospital, all necessary data were gathered, including quality of life information, complete blood count values, and persistent groin pain complaints following hernioplasty. Then, all complete reports were extracted in an Excel sheet to be analyzed using suitable statistical analysis. All data were kept for the researcher without personal data, keeping patients anonymous.
Statistical analysis
SPSS 27 software was used to analyze the collected data. Descriptive statistics (mean, frequencies, percentages, and standard deviations) were obtained with suitable tools. ANOVA and unpaired t-test were used to analyze inferential statistical data.
Findings
The mean age of the participants was 51.2±1.9 years and the majority were males (71.4%) and had harsh-type jobs (76.9%; Table 1).
Table 1. The frequency of demographic data of the participants
The Hemoglobin mean was 10.6±2.6g/dL, the White Blood Cells mean was 45.0±1.2U/L, PT mean was 11.4±2.3sec, and PTT mean was 12.3±4.1sec.
The most satisfied quality-of-life parameters were vitality (n=213), bodily pain (n=78), physical functioning (n=61), social role functioning (n=31), and general health perception (n=24). Hyperesthesia was the most common symptom of post-hernioplasty (n=112), and paresthesia (n=25), neuralgia (n=11), and hypoesthesia (n=3) were less common.
There were significant correlations between age and all quality-of-life parameters, while gender significantly correlated to all quality-of-life parameters except vitality. The type of job was strongly correlated with all quality-of-life parameters. Job type had significant correlations with all symptoms of post-hernioplasty, while gender and age significantly correlated only with neuralgia (Table 2).
Table 2. The correlation of demographic characteristics with quality-of-life parameters and the symptoms of post-hernioplasty (ANOVA)
The correlation between quality-of-life parameters and the remarked laboratory markers (Hb and WBCs) showed a significant correlation to only vitality, physical functioning, and general health perception (p<0.01). Meanwhile, WBCs showed no significant correlation with all quality-of-life parameters (Table 3).
Table 3. The laboratory markers' relationship to quality-of-life parameters (t-test)
Discussion
One of the most commonly used surgical procedures for treating inguinal hernia is hernioplasty. This procedure is widely performed due to its effectiveness in repairing the hernia; however, it is not without complications. Patients undergoing hernioplasty may experience a range of post-operative issues that can significantly impact their quality of life. These include persistent pain, limited mobility, and sensory disturbances, which can contribute to discomfort and interfere with daily activities. Additionally, factors such as surgical technique, patient demographics, and occupational demands may play a role in determining post-operative recovery outcomes. Given the potential long-term consequences of post-hernioplasty complications, this study aims to evaluate the quality of life in patients who developed inguinodynia following a hernioplastic procedure. A thorough assessment of their physical, psychological, and occupational challenges can provide valuable insights into the post-surgical experience and guide future improvements in patient care.
The study included 147 randomly selected cases of patients who had previously undergone hernioplasty. Most participants were male (n=105, 71.4%), with a mean age of 51.2±1.9 years. A significant proportion of the participants (n=113, 76.9%) were employed in physically demanding jobs, which may have played a role in the hernia's development and their post-operative recovery. Patients working in harsh environments often engage in repetitive heavy lifting, prolonged standing, or strenuous manual labor, which can exert excessive strain on the abdominal muscles, potentially affecting the durability of the surgical repair and prolonging recovery.
Laboratory analysis was conducted to assess hematological and coagulation parameters among the participants. The mean hemoglobin (Hb) level was recorded at 10.6±2.6 g/dL, while the prothrombin time (PT) averaged 11.4±2.3 seconds, and the partial thromboplastin time (PTT) was 12.3±4.1 seconds. These findings align with the study conducted by Chibata & Daronch, which reported that 49 out of 313 patients (15.65%) who underwent open inguinal hernioplasty exhibited issues related to low hemoglobin levels and altered coagulation markers, particularly PT [7]. Reduced hemoglobin levels in post-hernioplasty patients may indicate intraoperative blood loss, nutritional deficiencies, or chronic disease, negatively impacting wound healing and overall recovery. Additionally, prolonged PT and PTT values may suggest underlying coagulation abnormalities, increasing the risk of post-surgical hematomas or excessive bleeding.
To assess the impact of hernioplasty on patients' quality of life, five main parameters were evaluated. The findings revealed that most participants reported high satisfaction with their surgical outcomes (n=213). However, the lowest satisfaction scores were observed in the general health perception category (n=24). This pattern of responses is consistent with the findings of Iftikhar & Kerawala, who conducted a study on 88 patients and found that a significant proportion experienced a high level of satisfaction with their post-operative quality of life [1]. Similarly, Huang et al. examined 183 patients and reported that most of them exhibited an improved quality of life following hernioplasty [37]. These results underscore the importance of managing patient expectations and implementing post-operative care strategies to enhance general health perception, pain management, and psychological well-being.
A detailed evaluation of post-hernioplasty symptoms was conducted to identify common post-surgical complications. The most frequently reported symptom was hyperesthesia, affecting 112 cases, while only three patients experienced hypoesthesia. These findings agree with the study by Falzone et al., who assessed 266 patients during their initial outpatient follow-up visit and found that all cases exhibited hyperesthesia and neuralgia, specifically involving the ilioinguinal and iliohypogastric nerves [38]. The presence of hyperesthesia and neuralgia suggests that nerve irritation or damage may play a crucial role in the post-operative symptomatology of hernioplasty patients. Given that nerve-related complications are among the most common causes of post-surgical pain, future research should explore surgical techniques that minimize nerve trauma to improve patient outcomes.
Statistical analysis using the ANOVA test demonstrated a significant correlation between age and all quality-of-life parameters (p<0.01). The highest F value was observed for bodily pain (3.41), indicating that older patients were more likely to experience post-operative discomfort. Gender was also significantly correlated with all quality-of-life parameters except vitality (p>0.05). Furthermore, occupational factors were strongly correlated with quality-of-life measures, with general health perception showing the highest F value (4.34). These findings are supported by research conducted by Bona et al. [39] and Moreton & Truter, both of whom reported a strong correlation between patients' quality of life and post-hernioplasty symptoms (p<0.001) [40]. These results emphasize the importance of considering demographic and occupational factors when developing post-operative rehabilitation programs.
A comparative analysis of post-hernioplasty symptoms revealed a significant association between job type and all reported symptoms (p=0.001). Gender and age were specifically associated with neuralgia (p=0.001 and 0.002, respectively). These findings are consistent with research by Pinto et al., who used multivariate hierarchical regression analysis to examine predictors of post-hernioplasty symptoms in 135 patients. Their study identified younger age, strenuous work environments, preoperative anxiety, and chronic pain as significant risk factors for postoperative complications [42]. These findings highlight the need for preoperative counseling and tailored post-operative care strategies to address the specific risks associated with individual patient demographics and occupational conditions.
The relationship between quality-of-life parameters and laboratory markers was also examined. Hemoglobin levels and white blood cell (WBC) counts were significantly correlated with vitality, physical functioning, and general health perception (p<0.01). However, WBC counts did not significantly correlate with any of the quality-of-life parameters. These findings align with research by Bona et al., who reported that physical functioning and general health perception were significantly related to hemoglobin levels, which tend to decline after hernioplasty [39]. This suggests that monitoring and managing hemoglobin levels post-operatively may be beneficial in optimizing recovery and improving overall well-being in patients undergoing hernioplasty.
Further comparisons between surgical techniques indicate that laparoscopic total extraperitoneal (TEP) hernia repair is associated with less early postoperative pain than open mesh fixation techniques. One study found that TEP repair resulted in a more comfortable recovery, with reduced rates of neuralgia and hyperesthesia [41]. Additionally, studies comparing open Lichtenstein repair to laparoscopic TEP repair suggest that while recurrence rates may be similar between the two techniques, laparoscopic repair is associated with a quicker return to daily activities and improved post-operative comfort [1]. These findings suggest that minimally invasive techniques may offer advantages in pain reduction and faster rehabilitation, making them a preferred option in certain patient populations. Despite the overall positive impact of hernioplasty on quality of life, this study underscores the need for continued efforts to minimize post-surgical complications, including chronic pain, and to address potential factors like low hemoglobin levels that may affect overall well-being following hernioplasty.
Conclusion
Patients generally experience a high degree of quality of life after hernioplasty, with a reduction in symptom severity, including chronic pain. However, lower hemoglobin levels are observed in some patients, potentially impacting their general health perception.
Acknowledgments: The authors declared no acknowledgement.
Ethical Permissions: An IRB approval was obtained with number 311ac-A3 from the selected hospital in Kut, Iraq.
Conflicts of Interests: The authors declare no conflict of interests.
Authors' Contribution: Mohsin TS (First Author), Introduction Writer/Methodologist/Main or Assistant Researcher/Discussion Writer/Statistical Analyst (25%); Hussein GH (Second Author), Introduction Writer/Methodologist/ Main or Assistant Researcher/Discussion Writer/Statistical Analyst (25%); Hummadi MM (Third Author), Introduction Writer/Methodologist/ Main or Assistant Researcher/Discussion Writer/Statistical Analyst (25%); Abass HKA (Fourth Author), Introduction Writer/Methodologist/ Main or Assistant Researcher/Discussion Writer/Statistical Analyst (25%)
Funding/Support: The authors declared no funding.
Keywords:
References
1. Iftikhar N, Kerawala AA. Quality of life after inguinal hernia repair. Polish J Surg. 2021;93(3):35-39. [Link] [DOI:10.5604/01.3001.0014.8218]
2. LeBlanc KE, LeBlanc LL, LeBlanc KA. Inguinal hernias: diagnosis and management. Am Fam Physician. 2013;87(12):844-848. [Link]
3. Patti R, Picone E, Aiello P, Sammartano S, Migliore G, Di Vita G. Quality of life in elderly patients after inguinal hernioplasty. BMC Geriatrics. 2009;9:1-1. [Link] [DOI:10.1186/1471-2318-9-S1-A34]
4. Memon GA, Shah SKA. An experience with mesh versus darn repair in inguinal hernias. Pakistan J Med Sci. 2017;33(3):699. [Link] [DOI:10.12669/pjms.333.13257]
5. Poobalan AS, Bruce J, Smith WCS, King PM, Krukowski ZH, Chambers WA. A review of chronic pain after inguinal herniorrhaphy. Clinical J Pain. 2003;19(1):48-54. [Link] [DOI:10.1097/00002508-200301000-00006]
6. Huerta S, Patel PM, Mokdad AA, Chang J. Predictors of inguinodynia, recurrence, and metachronous hernias after inguinal herniorrhaphy in veteran patients. Am J Surg. 2016;212(3):391-8. [Link] [DOI:10.1016/j.amjsurg.2016.01.036]
7. Chibata M, Daronch OT. Assessment of postoperative risk of complications on inguinal hernioplasty and its relation to risk factors. Rev Assoc Med Bras. 2020;66(5):623-9. [Link] [DOI:10.1590/1806-9282.66.5.623]
8. Salah AN, Alwabsi HA. An overview of the antimicrobial activity of some microbial enzymes. Am J Biochem Biotechnol. 2024;20(2):140-50. [Link] [DOI:10.3844/ajbbsp.2024.140.150]
9. Zannoni M, Luzietti E, Viani L, Nisi P, Caramatti C, Sianesi M. Wide resection of inguinal nerves versus simple section to prevent postoperative pain after prosthetic inguinal hernioplasty: Our experience. World J Surg. 2014;38(5):1037-43. [Link] [DOI:10.1007/s00268-013-2363-4]
10. Koju R, Koju RB, Malla B, Dongol Y, Thapa LB. Transabdominal pre-peritoneal mesh repair versus Lichtenstein’ s hernioplasty. J Nepal Health Res Counc. 2017;15(2):135-140. [Link] [DOI:10.3126/jnhrc.v15i2.18202]
11. Poobalan AS, Bruce J, Smith WCS, King PM, Krukowski ZH, Chambers WA. A review of chronic pain after inguinal herniorrhaphy. Clin J pain. 2003;19(1):48-54. [Link] [DOI:10.1097/00002508-200301000-00006]
12. Salah AN, Elleboudy NS, El-Housseiny GS, Yassien MA. Cloning and sequencing of lsaE efflux pump gene from MDR Enterococci and its role in erythromycin resistance. Infect Genet Evol. 2021;94:105010. [Link] [DOI:10.1016/j.meegid.2021.105010]
13. Akim K, Gorretti N, Basimbe F. Inguinodynia and inguinal hernia recurrence amongst Ugandan patients who underwent mesh versus non-mesh inguinal hernia repair. South Sudan Med J. 2020;13(4):136-40. [Link]
14. Nateson AK, Basavanayak SN, Sudarsansrikanth. Study of the Lichtenstein's hernioplasty and its post-operative complications for different types of inguinal hernia. Int Surg J. 2019;6(7):2514-8. [Link] [DOI:10.18203/2349-2902.isj20192984]
15. Salah AN, Al-Otaibi MB, Al-dhmashi ASF, Mariee AA. Infection control practices and approaches in the dentistry field; A review. J Biosci Appl Res. 2024;10(1):42-58. [Link]
16. Hemdan M, Mageed SSA, Abulsoud AI, Faraag AH, Zaki MB, Mansour RM, et al. Approaches based on miRNAs in Behçet's disease: Unveiling pathogenic mechanisms, diagnostic strategies, and therapeutic applications. Life Sci. 2024;354:122950 [Link] [DOI:10.1016/j.lfs.2024.122950]
17. Schwartz JS, Strosberg DS, Renton DB. Chronic groin pain following anterior hernia surgery. In: The SAGES manual of groin pain. Cham: Springer; 2016. p. 211-9. [Link] [DOI:10.1007/978-3-319-21587-7_15]
18. Salah A, El-Housseiny G, Elleboudy N, Yassien M. Antimicrobial stewardship programs: A review. Arch Pharm Sci AIN SHAMS Univ. 2021;5(1):143-57. [Link] [DOI:10.21608/aps.2021.76105.1059]
19. Guttadauro A, Maternini M, Frassani S, De Simone M, Chiarelli M, Macchini D, et al. "All-in-one mesh" hernioplasty: A new procedure for primary inguinal hernia open repair. Asian J Surg. 2018;41(5):473-9. [Link] [DOI:10.1016/j.asjsur.2017.07.003]
20. Narita M, Jikihara S, Hata H, Matsusue R, Yamaguchi T, Otani T, et al. Surgical experience of laparoscopic retroperitoneal triple neurectomy for a patient with chronic neuropathic inguinodynia. Int J Surg Case Rep. 2017;40:80-4. [Link] [DOI:10.1016/j.ijscr.2017.09.012]
21. Mariee AA, Almulafekh M, Almahaid MA, Mohsen W, Esmail WMM, Alfraijat A, et al. The authentic leadership impact on the locus of control of nurses among nurse managers at certain primary healthcare centers. Int J Nov Res Healthc Nurs. 2024;11(1):307-15. [Link]
22. de La Croix H, Montgomery A, Nilsson E, Rogmark P, Sandblom G, Österberg J. Laparoscopic hernia surgery in Sweden 2010 to 2020: Scientifically highlights from the national Swedish Hernia Register. Laparosc Surg. 2021;5:48. [Link] [DOI:10.21037/ls-20-122]
23. Li J. Patient-reported chronic pain after open inguinal hernia repair with lightweight or heavyweight mesh: A prospective, patient-reported outcomes study. J Br Surg. 2020;107(13):e657. [Link] [DOI:10.1002/bjs.11755]
24. Zwaans WA, Verhagen T, Wouters L, Loos MJ, Roumen RM, Scheltinga MR. Groin pain characteristics and recurrence rates: Three-year results of a randomized controlled trial comparing self-gripping Progrip mesh and sutured polypropylene mesh for open inguinal hernia repair. Ann Surg. 2018;267(6):1028-33. [Link] [DOI:10.1097/SLA.0000000000002331]
25. Abdelwahab AE, Elgohary HGH, Hassan HEA, Elbegawy MA. Open inguinal hernia repair comparative study between external oblique aponeurosis flab herniorrhaphy versus Lichtenstein tension free hernioplasty. Benha J Appl Sci. 2022;7(10):7-13. [Link] [DOI:10.21608/bjas.2022.284636]
26. Lee SR, Park JY. Comparison of laparoscopic transabdominal preperitoneal hernioplasty and laparoscopic iliopubic tract repair for Nyhus type II hernia in women. Surg Endosc. 2021;35(12):7260-6. [Link] [DOI:10.1007/s00464-021-08739-w]
27. Shafqatullah SM, Wasim M, Zubair R, Mehmood Z, Khalid F, Khan N, et al. Prophylactic ilio-inguinal neurectomy in open inguinal hernia repair. Pak J Surg. 2019;35(3):209-13. [Link]
28. Chandana G. Comparative study between tapp and open hernioplasty in inguinal hernia repair [dissertation]. Vijayapura: BLDE (Deemed to be University); 2019. [Link]
29. Kulkarni ND, Adhikari G, Jadhav GS. An observational study to compare the outcomes of onlay technique with combined onlay-plug technique of mesh hernioplasty in inguinal hernia. Int Surg J. 2022;9(3):567. [Link] [DOI:10.18203/2349-2902.isj20220396]
30. Iakovlev V, Koch A, Petersen K, Morrison J, Grischkan D, Oprea V, et al. A pathology of mesh and time: Dysejaculation, sexual pain, and orchialgia resulting from polypropylene mesh erosion into the spermatic cord. Ann Surg. 2018;267(3):569-75. [Link] [DOI:10.1097/SLA.0000000000002134]
31. Pradyumna SR. A prospective study comparing the desarda technique versus lichtenstein technique for inguinal hernia treatment [dissertation]. Vijayapura: BLDE (Deemed to be University); 2019. [Link]
32. Campanelli G, Bruni PG, Morlacchi A, Lombardo F, Cavalli M. Primary inguinal hernia: The open repair today pros and cons. Asian J Endosc Surg. 2017;10(3):236-43. [Link] [DOI:10.1111/ases.12394]
33. Pillay Y. A rare case of a concomitant inguinal and obturator hernia and their laparoscopic transabdominal repair: A case report. Int J Abdom Wall Hernia Surg. 2023;6(3):193-6. [Link] [DOI:10.4103/ijawhs.IJAWHS_22_23]
34. Sanderson R, DE-MARCHI DD, Cesário JCB, Sanderson LGD, Zilberstein B. Quality of life using Eurahs-Qol scores after surgical treatment of inguinal hernia: laparoscopic transabdominal preperitoneal (TAPP) and Lichtenstein techniques. Arquivos Brasileiros de Cirurgia Digestiva. 2024;37:e1798. [Link] [DOI:10.1590/0102-672020240005e1798]
35. Adke S, Varrior AR, Minj N. Posthernioplasty inguinodynia. BMJ Case Rep. 2023;16(11):e256739. [Link] [DOI:10.1136/bcr-2023-256739]
36. Thorborg K, Hölmich P, Christensen R, Petersen J, Roos EM. The Copenhagen Hip and Groin Outcome Score (HAGOS): Development and validation according to the COSMIN checklist. Br J Sports Med. 2011;45(6):478-91. [Link] [DOI:10.1136/bjsm.2010.080937]
37. Huang CC, Tai FC, Chou TH, Lien HH, Jeng JY, Ho TF, et al. Quality of life of inguinal hernia patients in Taiwan: The application of the hernia-specific quality of life assessment instrument. PLoS One. 2017;12(8):e0183138. [Link] [DOI:10.1371/journal.pone.0183138]
38. Falzone U, Santonocito C, Zanghì MG, Rinzivillo N, Provenzano D, Sapienza E, et al. Neuropathic inguinal pain: Neurectomy associated with open prosthetic hernioplasty for the prevention of post-operative pain. Annali Italiani Di Chirurgia. 2022;93(4):377-84. [Link]
39. Bona S, Rosati R, Opocher E, Fiore B, Montorsi M, SUPERMESH Study Group. Pain and quality of life after inguinal hernia surgery: a multicenter randomized controlled trial comparing lightweight vs heavyweight mesh (Supermesh Study). Updates Surg. 2018;70(1):77-83 [Link] [DOI:10.1007/s13304-017-0483-3]
40. Moreton ML, Truter A. Evaluation of inguinal hernia repair using post-operative pain and quality of life metrics. Hernia. 2023;27(1):71-6. [Link] [DOI:10.1007/s10029-022-02701-y]
41. Matikainen M, Vironen JH, Silvasti S, Ilves I, Kössi J, Kivivuori A, Paajanen H. A randomized clinical trial comparing early patient-reported pain after open anterior mesh repair versus totally extraperitoneal repair of inguinal hernia. Br J Surg. 2021;108(12):1433-1437. [Link] [DOI:10.1093/bjs/znab354]
42. Pinto PR, Vieira A, Pereira D, Almeida A. Predictors of acute postsurgical pain after inguinal hernioplasty. J Pain. 2017;18(8):947-55. [Link] [DOI:10.1016/j.jpain.2017.03.003]