Volume 16, Issue 1 (2024)
Iran J War Public Health 2024, 16(1): 75-79 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2023/12/27 | Accepted: 2024/04/4 | Published: 2024/04/10
Received: 2023/12/27 | Accepted: 2024/04/4 | Published: 2024/04/10
How to cite this article
Sherhan A. A Comparison of the Effect of Multiple Inhalers Compared to Single Inhalers Salbutamol and Steroid on Patients with Asthma. Iran J War Public Health 2024; 16 (1) :75-79
URL: http://ijwph.ir/article-1-1426-en.html
URL: http://ijwph.ir/article-1-1426-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Authors
A.A. Sherhan *
Department of Medicine, Basrah Medical College, University Basrah, Basrah, Iraq
Full-Text (HTML) (511 Views)
Introduction
Due to its widespread prevalence and the persistent threat it poses to patients' lives, as well as their social and economic well-being, bronchial asthma, especially the chronic persistent form, remains a significant health concern [1]. The incidence of bronchial asthma is on the rise, with an estimated 400 million sufferers worldwide expected by the year 2025 [1, 2]. Factors such as climate changes, dietary habits, humidity, exposure to noxious substances, and indoor and outdoor risk factors may alter the natural history of bronchial asthma, affecting its incidence, prevalence, and prognosis, leading to various morbidity and mortality outcomes [3].
Treatment approaches for bronchial asthma have evolved in response to the complexity of the condition, with modifications to treatment strategies and annual revisions of guidelines to address new therapeutic options [3, 4]. Combination therapy, including double or even triple therapy, has revolutionized treatment, with numerous studies exploring combinations of inhalers and medications, including long-acting bronchodilators and various steroid formulations, either alone or in combination.
Patients are increasingly involved in the decision-making process regarding the choice of inhaler type, preferred route of administration, and methods to enhance communication about treatment options, leading to improved patient compliance, quality of life, and prognosis [5-7]. Combined therapy involving long-acting bronchodilators (e.g., LADA) and long-acting steroids, administered at varying doses, has been recommended for patients with chronic persistent asthma. This approach has been shown to alleviate symptoms, improve quality of life, reduce hospital admissions by decreasing the risk of acute asthma attacks and exacerbations, and minimize the adverse effects associated with short-acting bronchodilators and high-potency steroids [8-10].
The adoption of this type of therapy by primary healthcare centers and general practitioners undoubtedly promotes therapy adherence and dispels the misconceptions held by patients and their relatives about inhaler therapy [11, 12]. However, in the strategy of managing chronic asthma at the community or individual levels, there is still no clear consensus on the use of combination long-acting therapy, and there is a lack of national-level data, especially regarding short- and long-term prognosis and the cost-effectiveness of this approach. If a patient's asthma remains poorly controlled despite regular use of ICS, a thorough review should be conducted to assess adherence, inhaler technique, and ongoing exposure to modifiable aggravating factors [13-15]. While increasing the dose of ICS may benefit some patients, add-on therapy should generally be considered for adults taking 800 μg/day BDP (or equivalent) [16, 17].
The phenomenon of airway remodeling, considered a consequence of chronic asthma, along with age-related difficulties in handling inhaler devices, may affect the optimal response to treatment [18-20].
This study aimed to determine whether this type of inhaler therapy for patients with chronic asthma reduces symptoms, decreases the need for hospital admissions, improves the quality of life, and whether a high-dose combination is superior to a low dose in managing patients.
Materials and Methods
A prospective descriptive cross-sectional study was conducted on 207 patients, with 120 (58.0%) being female and 87 (42.0%) male, aged between 16 and 75 years, with a mean age of 45.59±14.67 years, during the period of 2021-2022 after approval by the scientific research committee at Basra College of Medicine. Patients experiencing acute asthmatic attacks or acute life-threatening asthma were excluded from the study. The inclusion criteria encompassed complaints of shortness of breath, cough, nocturnal shortness of breath, nocturnal cough, and scattered wheezing affecting their quality of life. Demographic data were collected using a separate form distributed to each participant, including age, gender, duration of asthma, diagnosis, treatment modalities, and types of inhalers.
After obtaining oral consent, the sample was divided into two main groups: those using short-acting inhalers and those using long-acting combined inhalers. The second group was further subdivided into two main categories: high-dose combination inhalers and low-dose combination inhalers (high dose: salmeterol/fluticasone 25/250 µg, low dose: salmeterol/fluticasone 25/125 µg). Pulmonary function tests, particularly FEV1/FVC and PEFR, were utilized to compare between the studied groups. The results of these objective parameters, including their means, standard deviations, and the percentage of FEV1/FVC, were considered as cutoff points for determining the beneficial effects obtained by inhaler type and dose.
The collected data were analyzed using SPSS version 22. Variables were calculated according to the study design using independent sample tests, Levene's test for equality of variances, and t-tests for equality of means. A p-value of less than 0.05 was considered statistically significant.
Findings
The mean age of participants was 45.59±14.67 years, ranging from 16 to 75 years, of whom 120 cases (58.0) were female and 87 cases were male (42.0).
Table 1 presents the general characteristics of the studied groups. Regarding confidence of patients regarding short-acting and long-acting and high-dose or low-dose inhalers, 51 (24.6) and 34 (16.4) cases were not confident and confident with short-acting and 34 (16.4) and 88 (42.5) were not confident and confident with long-acting inhalers, respectively (p=0.001). Also, 19 (15.6) and 39 (23.00) cases were not confident and confident with high-dose, and 13 (10.7) and 51 (41.8) cases were not confident and confident with low-dose inhalers, respectively (p=0.17).
Table 1. Demographic criteria and confidence of patients with the treatments, regarding inhaler type and dose

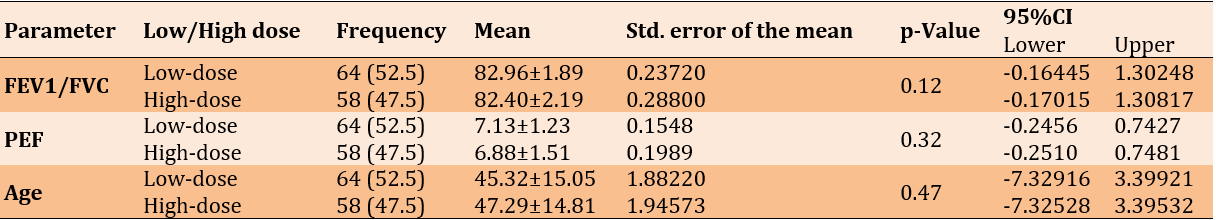
Table 2 illustrates the confidence levels of patients using both types of inhalers, including short-acting and long-acting, as indicated by measurements of FEV1/FVC, PEFR, and the age of patients as a non-modifiable factor in both groups (single or combined inhalers).
Table 2. Mean and frequency of patients’ confidence with both types of inhalers

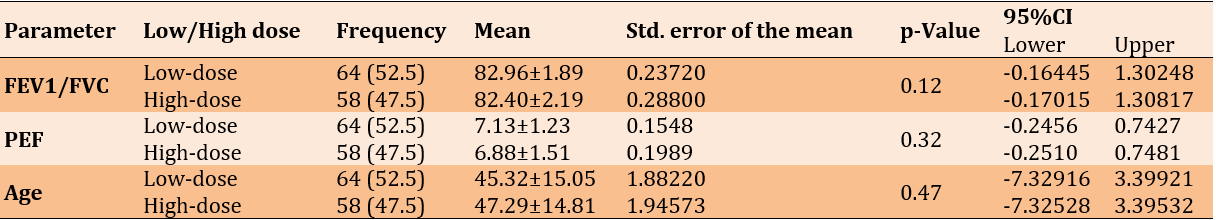
Table 3 displays the confidence levels of patients using both high-dose and low-dose combined inhalers, analyzed by Levene's test for equality of means, reflecting FEV1/FVC, PEFR, and age factors as non-modifiable factors. No significant difference was found between both types.
Table 3. Confidence levels of patients using both high-dose and low-dose combined inhalers
Discussion
This study, which assessed patients' subjective support alongside objective parameters, such as FEV1/LFVC and PEFR, revealed that patients' confidence in therapy was not solely dependent on symptom improvement. Other factors, including technical difficulties experienced with inhaler devices, type of inhalers, induced irritations, frequency of administrations, and potential side effects, also play a significant role. These social factors are considered to encourage patient compliance, leading to increased improvement rates, decreased exacerbations, and reduced hospital admissions. This is notably reflected in the study through the use of combination inhalers compared to single inhalers [3, 10].
In an outpatient study conducted in Bangladesh, highlighting the patient's role in selecting or influencing physicians to choose the most suitable inhaler types, similar results were observed. The addition of LABA components to ICS demonstrated significant improvements in FEV1/FVC parameters, but not in PEFR, in both types [17].
Age, though matched, implies no effects on both types, neither on pulmonary functions nor on the desire and confidence of the users, which is not consistent with many different studies, as the older age group may have difficulty in handling and inhaling properly [21, 22].
In this study, both combined and single inhalers showed parameters reflecting improvement in lung function when used in chronic persistent asthmatic patients using combined inhaled steroids and LABD, and less significantly in patients using single-based therapy such as steroids or LADA. This finding is consistent with multiple studies [12].
Regarding combinations of steroids and LABD inhalers, two main types were studied subjectively and objectively, including high-dose and low-dose. The patients' wishes and choices were secondary to the objective improvement demonstrated by pulmonary function tests, showing no significant difference between both types. Disregarding the patients' wishes may introduce bias, as their ideas about the exact dose of inhaler components could vary. However, pulmonary function tests, being a more solid parameter, did not show significant differences between the types. This is similar to a study by Patel et al. [19]. Even if not consistent with a foreign study, the peculiarity of environmental factors in this area, including wet weather and industrial emissions from oil companies, affects patient factors including confidence in inhalers.
Contrary to other studies, age factors, whether in the young age group or older, do not appear to affect the response to inhalers in this study, whether single-use inhalers or combined inhalers are used. Though theoretically advancing age and longer duration of disease may lead to remodeling phenomena, resulting in decreased response to bronchodilator therapy, patients' desires and confidence through questionnaires answered may be subject to bias. In this study, patients were more confident with combined than single-drug inhalers, with no differences in response between high-dose and low-dose combined inhalers. This is consistent with many meta-analyses studies (Patel 2013) [19]
The current study was restricted due to the limited number of patients and short duration of follow-up.. It is highly recommended that the study be replicated in different areas with extended follow-up durations.
Conclusion
Combined inhaler therapy for patients with chronic persistent asthma is superior to single-drug inhalers, whether as B-agonist drugs or steroids. This occurs for a variety of reasons, including improvements in quality of life, decreased side effects, from common simple side effects to more serious ones, like deaths associated with LADA alone, as well as the use of minimum doses in combined types rather than high doses to decrease side effects and prices for economic reasons, as the disease has chronic sequelae.
Acknowledgments: The authors like to thank all patients for their participation and information, and also all the staff of pulmonary function unit.
Ethical Permission: The study approved by scientific researches committees, Basrah medical college.
Conflicts of Interests: There is no conflicts of interest.
Authors’ Contribution: Aubed Sherhan A (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (100%)
Funding/Support: Nothing is declared by the authors.
Due to its widespread prevalence and the persistent threat it poses to patients' lives, as well as their social and economic well-being, bronchial asthma, especially the chronic persistent form, remains a significant health concern [1]. The incidence of bronchial asthma is on the rise, with an estimated 400 million sufferers worldwide expected by the year 2025 [1, 2]. Factors such as climate changes, dietary habits, humidity, exposure to noxious substances, and indoor and outdoor risk factors may alter the natural history of bronchial asthma, affecting its incidence, prevalence, and prognosis, leading to various morbidity and mortality outcomes [3].
Treatment approaches for bronchial asthma have evolved in response to the complexity of the condition, with modifications to treatment strategies and annual revisions of guidelines to address new therapeutic options [3, 4]. Combination therapy, including double or even triple therapy, has revolutionized treatment, with numerous studies exploring combinations of inhalers and medications, including long-acting bronchodilators and various steroid formulations, either alone or in combination.
Patients are increasingly involved in the decision-making process regarding the choice of inhaler type, preferred route of administration, and methods to enhance communication about treatment options, leading to improved patient compliance, quality of life, and prognosis [5-7]. Combined therapy involving long-acting bronchodilators (e.g., LADA) and long-acting steroids, administered at varying doses, has been recommended for patients with chronic persistent asthma. This approach has been shown to alleviate symptoms, improve quality of life, reduce hospital admissions by decreasing the risk of acute asthma attacks and exacerbations, and minimize the adverse effects associated with short-acting bronchodilators and high-potency steroids [8-10].
The adoption of this type of therapy by primary healthcare centers and general practitioners undoubtedly promotes therapy adherence and dispels the misconceptions held by patients and their relatives about inhaler therapy [11, 12]. However, in the strategy of managing chronic asthma at the community or individual levels, there is still no clear consensus on the use of combination long-acting therapy, and there is a lack of national-level data, especially regarding short- and long-term prognosis and the cost-effectiveness of this approach. If a patient's asthma remains poorly controlled despite regular use of ICS, a thorough review should be conducted to assess adherence, inhaler technique, and ongoing exposure to modifiable aggravating factors [13-15]. While increasing the dose of ICS may benefit some patients, add-on therapy should generally be considered for adults taking 800 μg/day BDP (or equivalent) [16, 17].
The phenomenon of airway remodeling, considered a consequence of chronic asthma, along with age-related difficulties in handling inhaler devices, may affect the optimal response to treatment [18-20].
This study aimed to determine whether this type of inhaler therapy for patients with chronic asthma reduces symptoms, decreases the need for hospital admissions, improves the quality of life, and whether a high-dose combination is superior to a low dose in managing patients.
Materials and Methods
A prospective descriptive cross-sectional study was conducted on 207 patients, with 120 (58.0%) being female and 87 (42.0%) male, aged between 16 and 75 years, with a mean age of 45.59±14.67 years, during the period of 2021-2022 after approval by the scientific research committee at Basra College of Medicine. Patients experiencing acute asthmatic attacks or acute life-threatening asthma were excluded from the study. The inclusion criteria encompassed complaints of shortness of breath, cough, nocturnal shortness of breath, nocturnal cough, and scattered wheezing affecting their quality of life. Demographic data were collected using a separate form distributed to each participant, including age, gender, duration of asthma, diagnosis, treatment modalities, and types of inhalers.
After obtaining oral consent, the sample was divided into two main groups: those using short-acting inhalers and those using long-acting combined inhalers. The second group was further subdivided into two main categories: high-dose combination inhalers and low-dose combination inhalers (high dose: salmeterol/fluticasone 25/250 µg, low dose: salmeterol/fluticasone 25/125 µg). Pulmonary function tests, particularly FEV1/FVC and PEFR, were utilized to compare between the studied groups. The results of these objective parameters, including their means, standard deviations, and the percentage of FEV1/FVC, were considered as cutoff points for determining the beneficial effects obtained by inhaler type and dose.
The collected data were analyzed using SPSS version 22. Variables were calculated according to the study design using independent sample tests, Levene's test for equality of variances, and t-tests for equality of means. A p-value of less than 0.05 was considered statistically significant.
Findings
The mean age of participants was 45.59±14.67 years, ranging from 16 to 75 years, of whom 120 cases (58.0) were female and 87 cases were male (42.0).
Table 1 presents the general characteristics of the studied groups. Regarding confidence of patients regarding short-acting and long-acting and high-dose or low-dose inhalers, 51 (24.6) and 34 (16.4) cases were not confident and confident with short-acting and 34 (16.4) and 88 (42.5) were not confident and confident with long-acting inhalers, respectively (p=0.001). Also, 19 (15.6) and 39 (23.00) cases were not confident and confident with high-dose, and 13 (10.7) and 51 (41.8) cases were not confident and confident with low-dose inhalers, respectively (p=0.17).
Table 1. Demographic criteria and confidence of patients with the treatments, regarding inhaler type and dose

Table 2 illustrates the confidence levels of patients using both types of inhalers, including short-acting and long-acting, as indicated by measurements of FEV1/FVC, PEFR, and the age of patients as a non-modifiable factor in both groups (single or combined inhalers).
Table 2. Mean and frequency of patients’ confidence with both types of inhalers

Table 3 displays the confidence levels of patients using both high-dose and low-dose combined inhalers, analyzed by Levene's test for equality of means, reflecting FEV1/FVC, PEFR, and age factors as non-modifiable factors. No significant difference was found between both types.
Table 3. Confidence levels of patients using both high-dose and low-dose combined inhalers
Discussion
This study, which assessed patients' subjective support alongside objective parameters, such as FEV1/LFVC and PEFR, revealed that patients' confidence in therapy was not solely dependent on symptom improvement. Other factors, including technical difficulties experienced with inhaler devices, type of inhalers, induced irritations, frequency of administrations, and potential side effects, also play a significant role. These social factors are considered to encourage patient compliance, leading to increased improvement rates, decreased exacerbations, and reduced hospital admissions. This is notably reflected in the study through the use of combination inhalers compared to single inhalers [3, 10].
In an outpatient study conducted in Bangladesh, highlighting the patient's role in selecting or influencing physicians to choose the most suitable inhaler types, similar results were observed. The addition of LABA components to ICS demonstrated significant improvements in FEV1/FVC parameters, but not in PEFR, in both types [17].
Age, though matched, implies no effects on both types, neither on pulmonary functions nor on the desire and confidence of the users, which is not consistent with many different studies, as the older age group may have difficulty in handling and inhaling properly [21, 22].
In this study, both combined and single inhalers showed parameters reflecting improvement in lung function when used in chronic persistent asthmatic patients using combined inhaled steroids and LABD, and less significantly in patients using single-based therapy such as steroids or LADA. This finding is consistent with multiple studies [12].
Regarding combinations of steroids and LABD inhalers, two main types were studied subjectively and objectively, including high-dose and low-dose. The patients' wishes and choices were secondary to the objective improvement demonstrated by pulmonary function tests, showing no significant difference between both types. Disregarding the patients' wishes may introduce bias, as their ideas about the exact dose of inhaler components could vary. However, pulmonary function tests, being a more solid parameter, did not show significant differences between the types. This is similar to a study by Patel et al. [19]. Even if not consistent with a foreign study, the peculiarity of environmental factors in this area, including wet weather and industrial emissions from oil companies, affects patient factors including confidence in inhalers.
Contrary to other studies, age factors, whether in the young age group or older, do not appear to affect the response to inhalers in this study, whether single-use inhalers or combined inhalers are used. Though theoretically advancing age and longer duration of disease may lead to remodeling phenomena, resulting in decreased response to bronchodilator therapy, patients' desires and confidence through questionnaires answered may be subject to bias. In this study, patients were more confident with combined than single-drug inhalers, with no differences in response between high-dose and low-dose combined inhalers. This is consistent with many meta-analyses studies (Patel 2013) [19]
The current study was restricted due to the limited number of patients and short duration of follow-up.. It is highly recommended that the study be replicated in different areas with extended follow-up durations.
Conclusion
Combined inhaler therapy for patients with chronic persistent asthma is superior to single-drug inhalers, whether as B-agonist drugs or steroids. This occurs for a variety of reasons, including improvements in quality of life, decreased side effects, from common simple side effects to more serious ones, like deaths associated with LADA alone, as well as the use of minimum doses in combined types rather than high doses to decrease side effects and prices for economic reasons, as the disease has chronic sequelae.
Acknowledgments: The authors like to thank all patients for their participation and information, and also all the staff of pulmonary function unit.
Ethical Permission: The study approved by scientific researches committees, Basrah medical college.
Conflicts of Interests: There is no conflicts of interest.
Authors’ Contribution: Aubed Sherhan A (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (100%)
Funding/Support: Nothing is declared by the authors.
References
1. Bateman ED, Hurd SS, Barnes PJ, Bousquet J, Drazen JM, FitzGerald M, et al. Global strategy for asthma management and prevention: GINA executive summary. Eur Respir J. 2008;31(1):143-78. [Link] [DOI:10.1183/09031936.00138707]
2. Global Initiative for Asthma (GINA). Global burden of asthma report. Fontana: Global Initiative for Asthma; 2009. [Link]
3. Global Initiative for Asthma (GINA). Global strategy for asthma management and prevention. Fontana: Global Initiative for Asthma; 2016. p. 50-63. [Link]
4. Nigro SC, Sobieraj DM. Budesonide/glycopyrrolate/formoterol fumarate co-suspension metered dose inhaler: A triple therapy for the treatment of chronic obstructive pulmonary disease. Ann Pharmacother. 2022;56(5):582-91. [Link] [DOI:10.1177/10600280211038353]
5. Kelly HW, Sternberg AL, Lescher R, Fuhlbrigge AL, Williams P, Zeiger RS, et al. Effect of inhaled glucocorticoids in childhood on adult height. N Engl J Med. 2012;367(10):904-12. [Link] [DOI:10.1056/NEJMoa1203229]
6. Kew KM, Karner C, Mindus SM, Ferrara G. Combination formoterol and budesonide as maintenance and reliever therapy versus combination inhaler maintenance for chronic asthma in adults and children. Cochrane Database Syst Rev. 2013;(12):CD009019. [Link] [DOI:10.1002/14651858.CD009019.pub2]
7. Melani AS. Inhalation therapy training: A priority challenge for the physician. Acta Biomed. 2007;78(3):233-45. [Link]
8. Nair SJ, Daigle KL, DeCuir P, Lapin CD, Schramm CM. The influence of pulmonary function testing on the management of asthma in children. J Pediatr. 2005;147(6):797-801. [Link] [DOI:10.1016/j.jpeds.2005.07.023]
9. Sestini P, Cappiello V, Aliani M, Martucci P, Sena A, Vaghi A, et al. Prescription bias and factors associated with improper use of inhalers. J Aerosol Med. 2006;19(2):127-36. [Link] [DOI:10.1089/jam.2006.19.127]
10. Adams RJ, Smith BJ, Ruffin RE. Patient preference for autonomy in decision making in asthma management. Thorax. 2001;56(2):126-32. [Link] [DOI:10.1136/thorax.56.2.126]
11. Papi A, Haughney J, Virchow JC, Roche N, Palkonen S, Price D. Inhaler devices for asthma: A call for action in a neglected field. Eur Respir J. 2011;37(5):982-5. [Link] [DOI:10.1183/09031936.00150910]
12. Chrystyn H, Price D. Not all asthma inhalers are the same: Factors to consider when prescribing an inhaler. Prim Care Respir J. 2009;18(4):243-9. [Link] [DOI:10.4104/pcrj.2009.00029]
13. Haughney J, Price D, Barnes NC, Virchow C, Roche N, Chrystyn H. Choosing inhaler devices for people with asthma: Current knowledge and research needs. Respir Med. 2010;104(9):1237-45. [Link] [DOI:10.1016/j.rmed.2010.04.012]
14. Haughney J, Price D, Kaplan A, Chrystyn H, Horne R, May N, et al. Achieving asthma control in practice: Understanding the reasons for poor control. Respir Med. 2008;102(12):1681-93. [Link] [DOI:10.1016/j.rmed.2008.08.003]
15. Melani AS, Zanchetta D, Barbato N, Sestini P, Cinti C, Canessa PA, et al. Inhalation technique and variables associated with misuse of conventional metered-dose inhaler and newer dry powder inhaler inexperienced adults. Ann Allergy Asthma Immunol. 2004;93(5):439-46. [Link] [DOI:10.1016/S1081-1206(10)61410-X]
16. Penman ID, Ralston SH, Strachan MWJ, Hobson R, editors. Davidson's principles and practice of medicine. Amsterdam: Elsevier; 2022. p. 669-72. [Link]
17. Rafi MA, Tahmin CI, Tashrik S, Bonna AS, Jannat F, Mily SJ, et al. Adherence to inhalers and associated factors among adult asthma patients: An outpatient-based study in a tertiary hospital of Rajshahi, Bangladesh. Asthma Res Pract. 2022;8(1):1. [Link] [DOI:10.1186/s40733-022-00083-7]
18. Bond K, Coyle D, O'Gorman K, Coyle K, Spooner C, Lemière C, et al. Long-acting beta2-agonist and inhaled corticosteroid combination therapy for adult persistent asthma: Systematic review of clinical outcomes and economic evaluation. Ottawa: Canadian Agency for Drugs and Technologies in Health; 2009. [Link]
19. Patel S, Padh H, Bhavsar C. MANOVA over ANOVA- A better objective in bioequivalence study. IJPSR. 2013;4(5):1874-1881. [Link]
20. Melani AS, Bonavia M, Cilenti V, Cinti C, Lodi M, Martucci P, et al. Inhaler mishandling remains common in real life and is associated with reduced disease control. Respir Med. 2011;105(6):930-8. [Link] [DOI:10.1016/j.rmed.2011.01.005]
21. Mohammed A, Khalaf H, Jamal Kamal B, Ali Kamal M. Prevalence of Asthma control in adult patients in Kirkuk city. Medical Journal of Babylon. 2024;20(1):53-57. [Link] [DOI:10.4103/MJBL.MJBL_363_22]
22. Ho SF, Omahony MS, Steward JA, Breay P, Burr ML. Inhaler technique in the older people in the community. Age Ageing. 2004;33(2):185-8. [Link] [DOI:10.1093/ageing/afh062]
23. Basheti IA, Armour CL, Bosnic-Anticevich SZ, Reddel HK. Evaluation of a novel educational strategy, including inhaler-based reminder labels, to improve asthma inhaler technique. Patient Educ Couns. 2008;72(1):26-33. [Link] [DOI:10.1016/j.pec.2008.01.014]
24. Kim SH, Kwak HJ, Kim TB, Chang YS, Jeong JW, Kim CW, et al. Inappropriate techniques used by internal medicine residents with three kinds of inhalers (a metered dose inhaler, Diskus, and Turbuhaler): Changes after a single teaching session. J Asthma. 2009;46(9):944-50. [Link] [DOI:10.3109/02770900903229701]
25. Chrystyn H, Price D. Not all asthma inhalers are the same: factors to consider when prescribing an inhaler. Prim Care Respir J. 2009;18(4):243-9. [Link] [DOI:10.4104/pcrj.2009.00029]









