Volume 17, Issue 3 (2025)
Iran J War Public Health 2025, 17(3): 325-333 |
Back to browse issues page
Article Type:
Subject:
Ethics code: IR.AJAUMS.REC.1402.044
History
Received: 2025/06/14 | Accepted: 2025/07/26 | Published: 2025/07/30
Received: 2025/06/14 | Accepted: 2025/07/26 | Published: 2025/07/30
How to cite this article
Zibasokhan S, Sharififar S, Azizi M, Teimouri F, Azarmi S. Challenges and Promotion Strategies of Temporary Medical Centers in Mass gatherings; A Qualitative Study. Iran J War Public Health 2025; 17 (3) :325-333
URL: http://ijwph.ir/article-1-1660-en.html
URL: http://ijwph.ir/article-1-1660-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
1- Department of Health in Disasters and Emergencies, Faculty of Nursing, Aja University of Medical Sciences, Tehran, Iran
Full-Text (HTML) (5 Views)
Introduction
The Arbaeen pilgrimage is considered one of the largest peaceful human gatherings in the contemporary world [1]. Every year, approximately 17 to 20 million people from different countries participate in this great march [2]. These events pose significant public health challenges related to the well-being of participants and the provision of healthcare services [3].
If a mass gathering is not carefully managed, it can lead to the spread of infectious diseases, threatening global health security and even the political stability of countries [4]. During the Arbaeen pilgrimage, like any other human gathering, the combination of population density and nonobservance of basic hygiene principles has contributed to the increased spread of communicable diseases [5]. Gastrointestinal diseases are also prevalent due to cultural differences in eating habits across countries [6]. Additionally, heatstroke can occur because of the high temperatures in Iraq during the summer season of the pilgrimage [7]. Musculoskeletal disorders may arise from not adhering to basic walking principles, while skin diseases and blisters on the feet can result from wearing inappropriate shoes or walking nonstop without rest [5]. As a result, pilgrims often seek medical care along the pilgrimage route [1]. According to the Iranian Red Crescent Society, during the 2023 Arbaeen pilgrimage, healthcare services were provided to pilgrims at military temporary medical centers (MTMCs) [8].
MTMCs are practical solutions for meeting health and treatment demands in mass gatherings, such as the Arbaeen pilgrimage [9]. MTMCs have key features, such as rapid deployment for urgent medical needs, increased patient care capacity, addressing a variety of medical needs—including first aid, chronic disease management, and physical and mental preventive care—and providing basic medical services, including triage, treatment, and coordination with local healthcare systems and emergency response teams [10, 11]. In addition, considering the long distances and numerous health challenges that pilgrims face, MTMCs play a vital role in ensuring the health and safety of pilgrims [12, 13].
Various quantitative and qualitative studies in countries, such as China, the United States, and Spain have examined the challenges faced by medical centers and temporary hospitals in disasters. Some of the reported challenges included a lack of human resources and equipment, an inability to predict the number of patients, and communication problems. Additionally, there is the difficulty of sending a large number of experienced specialists with relevant clinical records to these centers [14-17]. Another study that examined the challenges of MTMCs during Arbaeen reported a lack of experienced health workers [18]. Overcoming these challenges and improving MTMCs requires a multifaceted approach. According to a study, strategies such as surge capacity management, staff training, and enhanced communication systems are crucial [14].
According to the aforementioned cases and the special importance of holding the Arbaeen pilgrimage in Islamic countries, especially Iran, health issues and facilities should be taken into consideration. Although studies have been conducted in this field, our understanding of the challenges and promotion strategies of MTMCs within our country’s context is still limited. This study was conducted to address the existing research gap, enhance our understanding of the challenges and promotion strategies of MTMCs during the Arbaeen pilgrimage, and provide new information for improving the health and safety of pilgrims.
Participants and Methods
The present qualitative research with a conventional content analysis approach, utilizing Granheim and Lundman’s method for data analysis, was conducted at the military temporary facilities providing health services along the route where the Arbaeen pilgrimage ritual takes place, including clinics, health treatment centers, and sites located in the Ilam and Khuzestan Provinces in Iran in 2024 [19].
The participants were selected using a purpose-based sampling method with maximum diversity. These individuals are better positioned than others to describe the various aspects of the challenges and promotion strategies of MTMCs. Therefore, sampling with maximum diversity [20] was conducted from MTMCs located in Ilam and Khuzestan Provinces in Iran. The participants included executive directors, policymakers, physicians, nurses, health and paraclinical staff in MTMCs, Iranian patients, and other individuals referred to MTMCs during the Arbaeen days (such as patients’ companions), as well as personnel from cooperating and supporting organizations within the health system during the 2024 Arbaeen event. The interviews continued until data saturation was reached, ensuring that no new issues were raised in subsequent interviews. The participants consisted of 15 individuals, including 4 managers, 8 health workers, 1 patient companion, and 2 patients from MTMCs.
Semi-structured interviews based on an interview guide were used to collect information. From the beginning, the purpose of the study was explained to the participants, and after obtaining written consent and observing ethical considerations (such as keeping information confidential and the right of participants to withdraw from the research at any time), the interviews were conducted and recorded with the participants’ consent. Ten interviews were conducted face-to-face, and five were conducted over the phone, each lasting between 30 and 45 minutes. The interviews were conducted individually. The interviews continued until information saturation was achieved, and no new topics were raised in subsequent interviews [21].
At the beginning of the interview, general questions, such as “Can you describe your experience of a day’s work or attending an MTMC?” and “What are the health challenges in MTMCs during the Arbaeen pilgrimage?” were asked, along with “What strategies do you suggest to improve health services in MTMCs during the Arbaeen pilgrimage for the coming years?” The participants were then asked probing questions such as “Can you elaborate on this?” The interviews followed this format. Finally, the participants were asked to express any additional comments they wished to share. The location of the interviews was determined according to the preferences of the participants. Field notes were another method of data collection considered during the data analysis. In this case, the researcher visited several centers and recorded his observations.
The interviews were first transcribed using Microsoft Word software. The transcripts of the interviews were read several times by the researchers for overall understanding. To analyze the data, Granheim and Lundman’s conventional content analysis method was used [19]. During the data collection process, the researchers performed coding analysis and continuous comparisons. Similar codes were grouped into subcategories and then organized into categories based on the similarities and differences among the subcategories.
Findings
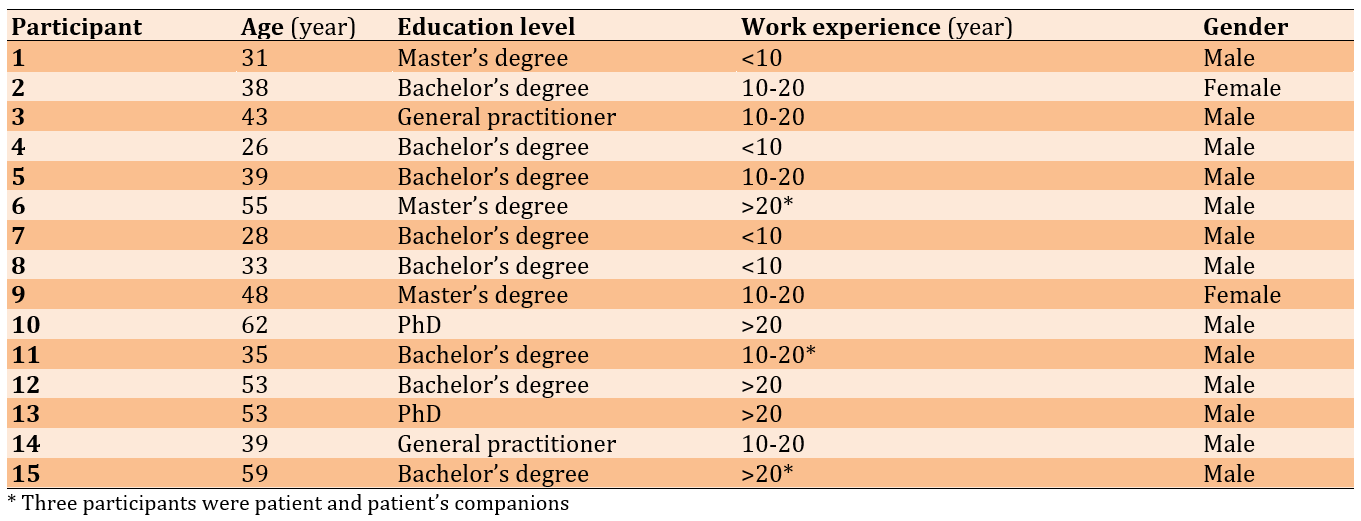
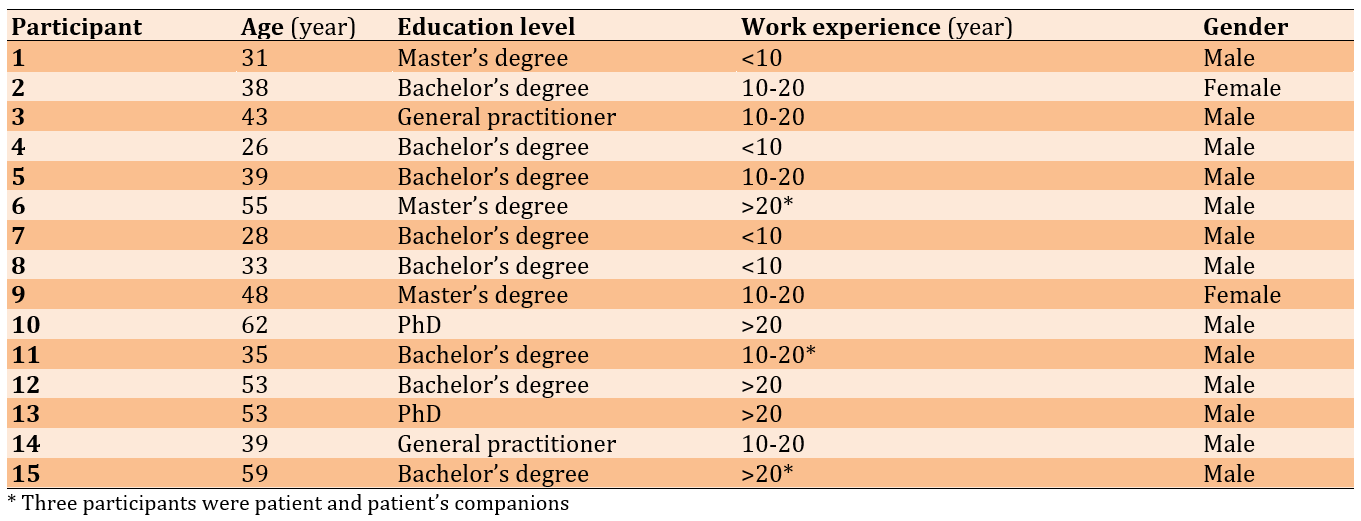
The mean age of the participants was 43 years, and their mean work experience was 14 years (Table 1).
Table 1. Individual characteristics of the participants
The initial codes obtained from the interviews totaled 1,576 codes. After integration through conventional conceptual analysis, these codes were classified into two domains: challenges and promotion strategies. The specific strategies and solutions expressed by the participants for all the existing challenges were categorized and presented.
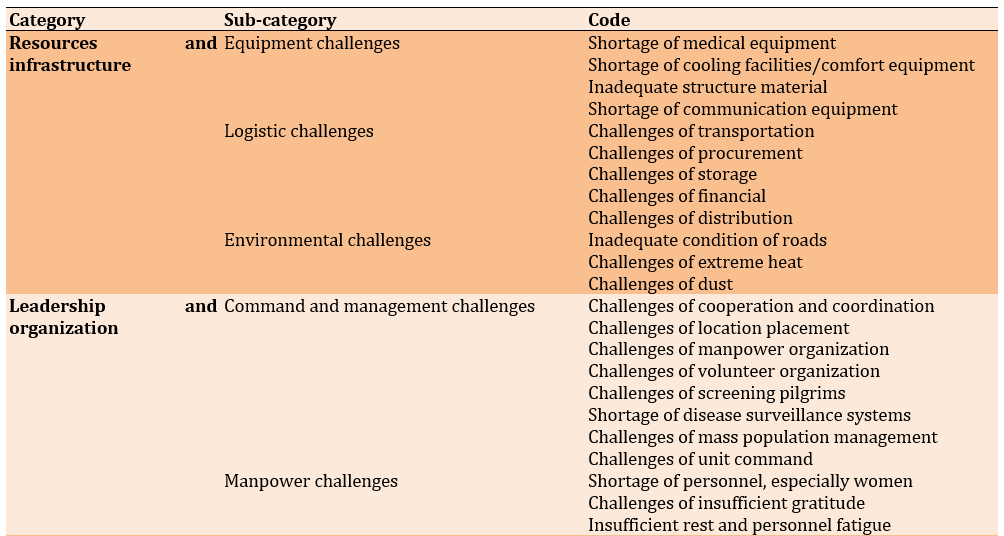
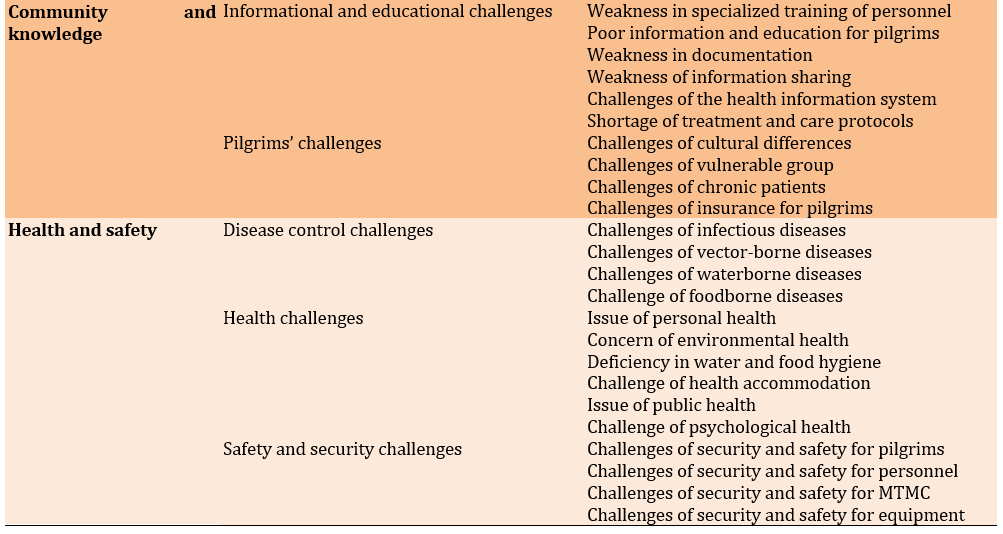
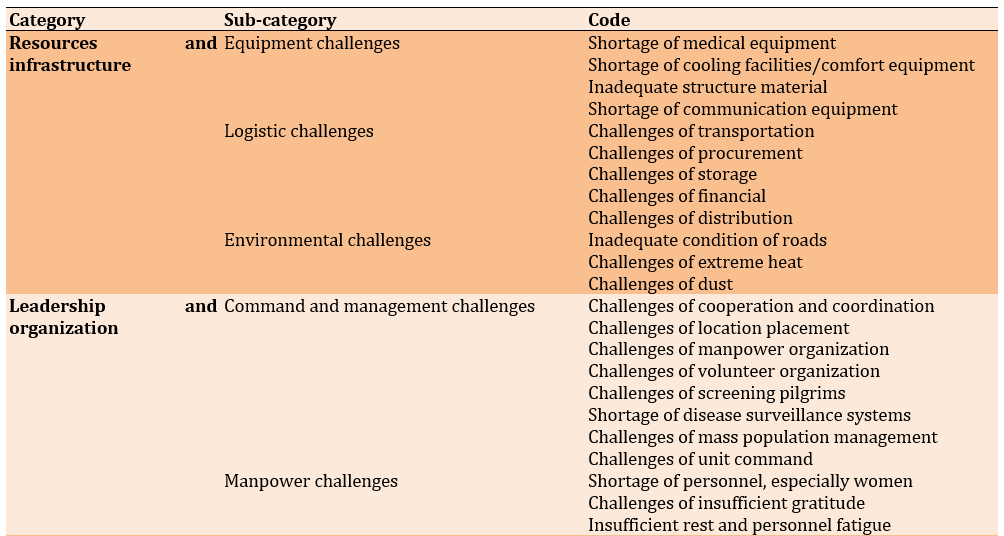
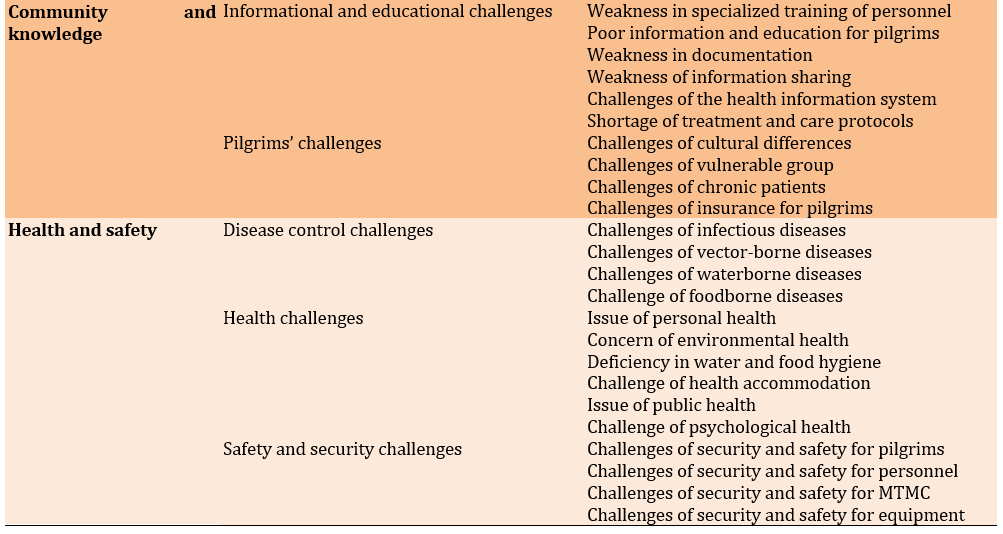
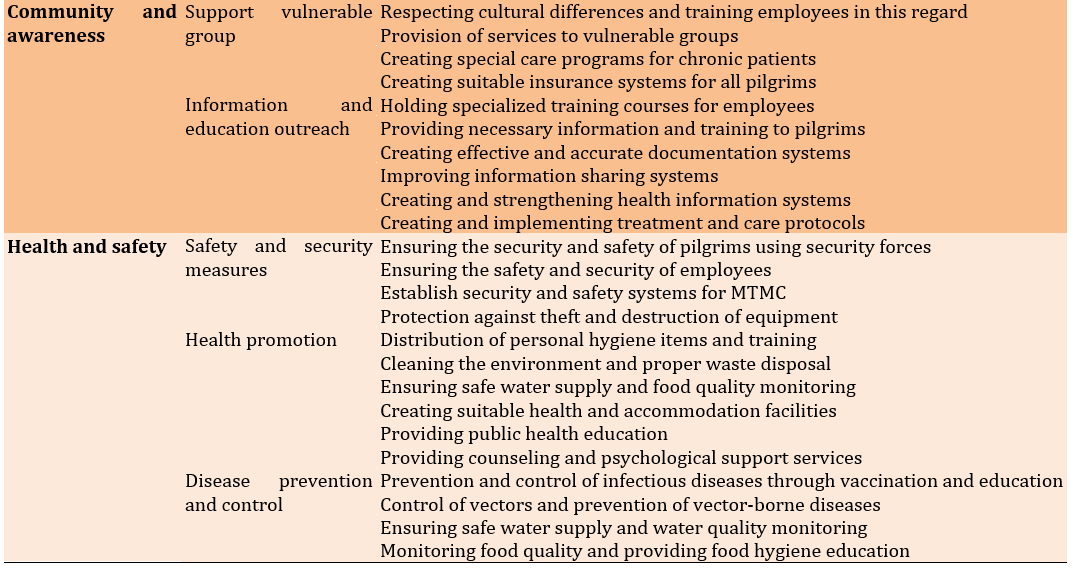
In the challenges domain, there were 4 main categories and 10 subcategories, including resources and infrastructure (equipment challenges, logistical challenges, environmental challenges), leadership and organization (command and management challenges, manpower challenges), community and knowledge (informational and educational challenges, pilgrims’ challenges), and health and safety (disease control challenges, health challenges, safety and security challenges; Table 2).
Table 2. Categories and sub-categories of challenges at military temporary medical centers (MTMCs)
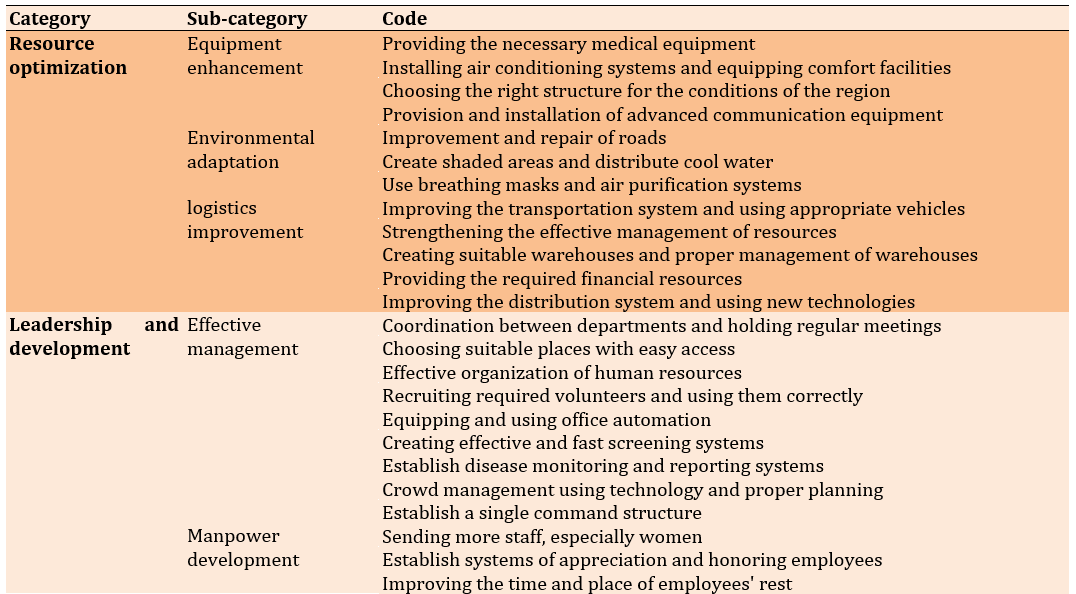
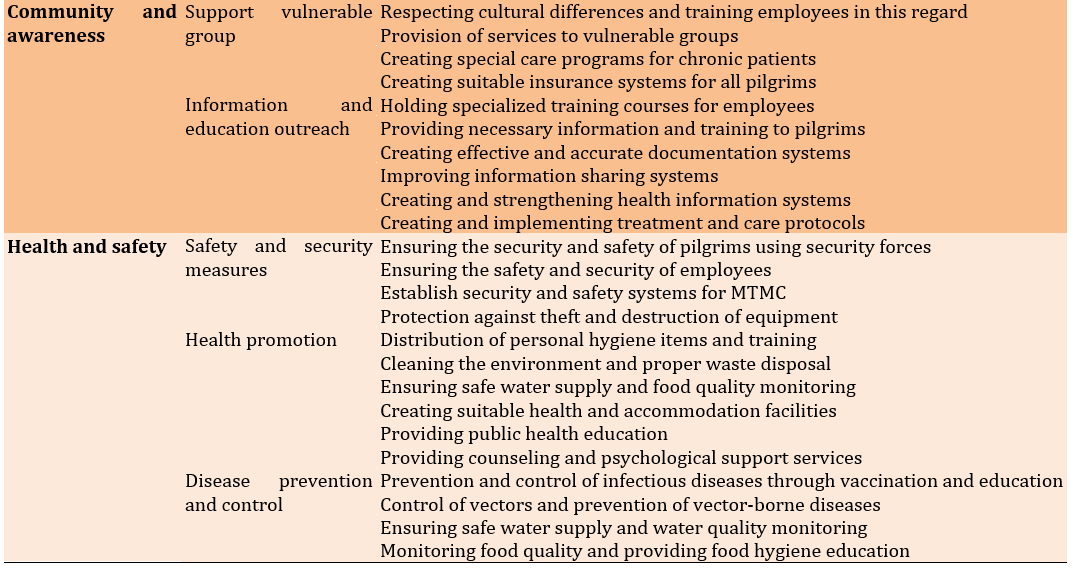
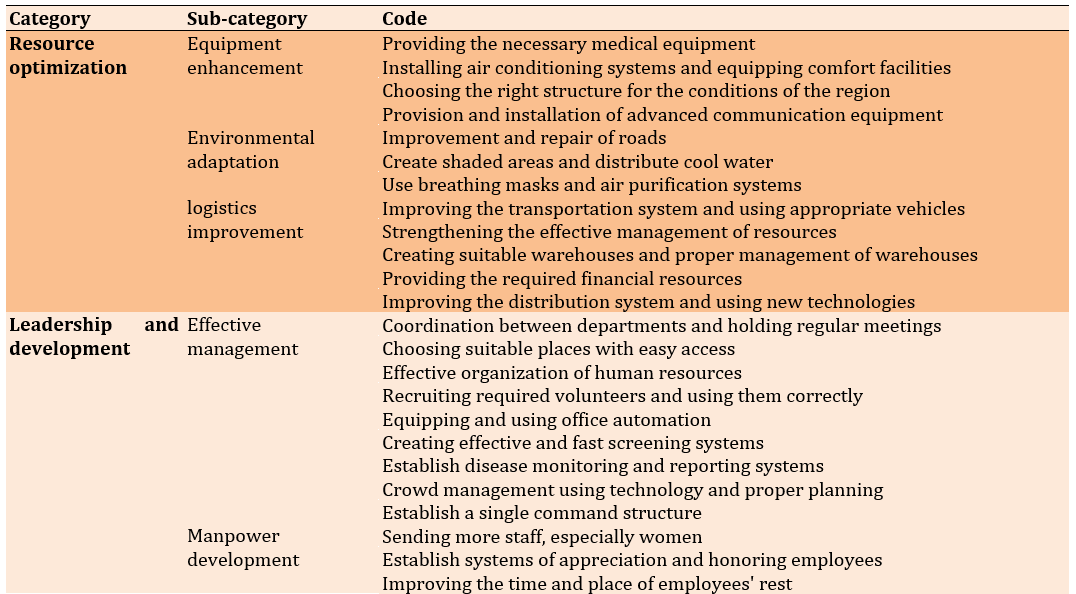
In the promotion strategies domain, there were 4 main categories and 10 subcategories, including resource optimization (equipment enhancement, environmental adaptation, logistics improvement), leadership and development (effective management, manpower development), community and awareness (support for pilgrims, information and education outreach), and health and safety (safety and security measures, health promotion, disease prevention and control; Table 3).
Table 3. Categories and sub-categories of promotion strategies at military temporary medical centers (MTMCs)
Resources and infrastructure
Equipment challenges
MTMCs in the Arbaeen pilgrimage face a shortage of medical, pharmaceutical, and communication equipment. Due to the tent structure of these centers and the heat of the air, a large amount of cooling equipment is needed. Notably, maintenance and repair of equipment in these difficult conditions is also a major challenge.
One of the participants stated, “The temperature in the area where we were over 50 degrees and the air conditioners did not respond to the entire space of the center, it was very difficult to work in those tents.” [Participant 2]
Logistics challenges
Transporting equipment and medicines to remote and scattered areas, managing traffic and procurement, and addressing storage and financial issues are important logistical challenges. Additionally, the distribution of facilities among centers is also very important.
Environmental challenges
Unfavorable weather conditions, dust, heat, and poor access to roads can negatively affect the performance of MTMCs. These conditions can reduce the efficiency of equipment and increase the risk of weather-related diseases.
One of the participants stated, “The roads had terrible conditions, and we could only go back and forth with a series of special cars, and of course, in that weather, the cars sometimes did not even have air conditioners.” [Participant 11]
Leadership and organization
Command and management challenges
Coordination among different treatment teams, management of human resources and volunteers, appropriate placement of centers, creation of a registration and screening system for patients, and quick decision-making in emergency situations are among the challenges of command and management in these centers. A lack of strong management structures can lead to reduced efficiency and increased risks.
Manpower challenges
A lack of specialized and trained manpower, fatigue, and high work pressure are the most important challenges in this field. Additionally, attracting human resources under harsh environmental conditions is difficult and should be recognized.
One of the participants stated, "Before sending the personnel, people who are experienced in the required fields should be selected. Sometimes people come who do not have the experience and special expertise of the existing conditions and cannot provide special help." [Participant 5]
Community and knowledge
Informational and educational challenges
Proper training for employees and pilgrims regarding disease prevention and management methods, the use of medical equipment, and compliance with health guidelines are among the informational and educational challenges. Furthermore, there is a need for efficient information systems to manage data and information.
Pilgrims’ challenges
Pilgrims may constitute a vulnerable group with specific underlying diseases. Additionally, providing medical services to pilgrims from diverse language and cultural backgrounds is also a major challenge.
One of the participants stated, "You can imagine that almost all languages and cultures are different from the clients, and it was truly difficult to communicate properly with them." [Participant 2]
Health and safety
Disease control challenges
A large gathering of pilgrims in one place can lead to the spread of infectious diseases. The management and control of these diseases require detailed planning and interdepartmental cooperation. Additionally, the provision of sufficient equipment and medicines to address the spread of diseases is also highly important.
One of the participants stated, "There was not much supervision over the cooking and distribution of food, and sometimes you go to the food distribution centers and there is a lot of garbage with flies and mosquitoes." [Participant 10]
Health challenges
The large gathering of pilgrims in one location, along with the lack of sanitary facilities, safe drinking water, and poor environmental hygiene, can lead to numerous physical and mental health problems.
One of the participants stated, "Because most of the processions served food in disposable containers, there was a lot of garbage around the pilgrims' accommodations and routes, and some pilgrims did not expect this situation at all and were very worried about their health." [Participant 8]
Security and safety challenges
Ensuring the safety of pilgrims and employees against various threats, including terrorist attacks and natural disasters, is crucial. Additionally, the safety of equipment and buildings should also be considered.
Resource optimization
Equipment enhancement
Upgrading and improving equipment, as well as modifying the design and structure of MTMCs, play an important role in enhancing the quality of medical services provided to pilgrims. By using advanced and up-to-date medical, welfare, and communication equipment, patients can be treated more effectively, and problems can be prevented.
Environmental adaptation
Adapting MTMCs to the environmental conditions of the Arbaeen pilgrimage, including temperature, humidity, and weather conditions, is of great importance. By adjusting equipment and facilities to these conditions, we can ensure the optimal performance of treatment centers and provide better services to pilgrims.
One of the participants stated: "Almost all roads and trails are dirt, so due to the high dust, tents should be equipped with air purifiers." [Participant 11]
Logistics improvement
Improvement of logistics services in MTMCs, including the timely transfer and distribution of needed items and proper storage, plays a significant role in increasing the efficiency and effectiveness of these centers. With proper resource management and careful planning, we can avoid shortages and logistical issues.
One of the participants stated: "Many times, with planning and distribution management, we can prevent wasted costs and shortages." [Participant 3]
Leadership and development
Effective management
Improving command and management through the establishment of efficient management structures and necessary training for staff can enhance the coordination and efficiency of these centers. With proper management and timely decision-making, we can prevent problems and miscoordination.
Manpower development
Allocating manpower in the appropriate numbers and paying attention to work and rest schedules greatly helps to improve the services provided.
One of the participants stated: "A sufficient number of personnel, especially women, can help a lot." [Participant 9]
Community and awareness
Information and education outreach
Enhancing the skills of staff through specialized training can significantly improve the quality of healthcare services in MTMCs during the Arbaeen pilgrimage. By boosting staff capabilities, we can deliver more effective and higher-quality services.
One of the participants stated: "Personnel should be trained according to the existing conditions before being sent, and great care should be taken in selecting efficient personnel." [Participant 3]
Support pilgrims
In MTMCs during the Arbaeen pilgrimage, it is crucial to adapt healthcare services to accommodate the diverse cultural backgrounds of pilgrims. This includes understanding and respecting different cultural practices and beliefs to provide effective care. Additionally, managing chronic diseases such as diabetes and hypertension is essential, as these conditions can be exacerbated by the physical demands of the pilgrimage.
Health and safety
Disease prevention and control
Paying attention to the quality of water and food, as well as the vectors in the region, along with providing care and prevention methods such as vaccination, greatly helps to control epidemics.
Health promotion
Providing health consultations and distributing hygiene materials such as masks and sanitizers can help reduce the burden of illnesses and health issues during the Arbaeen pilgrimage.
One of the participants stated: "For the paths, a bunch of people are needed to collect the garbage and give the necessary training to the pilgrims." [Participant 8]
Safety and security measures
Improving security and safety in MTMCs through the establishment of appropriate infrastructure and the implementation of safety protocols can help reduce risks and adverse incidents. By creating a safe and secure environment, we can protect the health and well-being of pilgrims.
One of the participants stated: "Safety and security should be given a lot of attention by the officials and specialized teams should be sent for this work" [Participant 10]
The promotion strategies presented included resource optimization, effective management, and tailored health and safety measures. These strategies provide actionable recommendations for policymakers and planners to enhance the efficiency and effectiveness of MTMCs during mass gatherings.
Discussion
This study aimed to examine the challenges faced by military temporary medical centers and identify solutions to overcome these challenges. The results highlight the existence of ten subcategories that express the challenges in MTMCs. Several studies, both inside and outside the country, have investigated the issue of health and the challenges of providing health services in mass gatherings. There is a high prevalence of infectious diseases, such as those observed during the Hajj and Arbaeen pilgrimage, in mass gatherings [22-24]. Infectious diseases are the most common health threat associated with mass gatherings [2, 4]. Viral respiratory infections are a significant public health concern that can cause serious illness, especially in vulnerable populations [25].
The needs and challenges of providing health services in MTMCs during the Arbaeen pilgrimage ceremony vary each year and depend on the season in which the ceremony is held [4]. Those planning mass gatherings should also consider the seasonality of some common conditions, such as flu-like symptoms, which may be more likely to occur in relatively colder months, and cases of diarrhea and food poisoning, which may be more common in warmer months [24]. According to a study by Al-Ansari et al. from Australia in 2021, one out of every five participants in the Arbaeen ceremony has a cough, and one out of eight experiences diarrhea. These results highlight the need for governments, religious authorities, and participants in Arbaeen to plan and implement preventive measures to prevent the spread of more serious infections. Such measures can include health initiatives, health education, health equipment, and proper management of water and sewage resources [26].
Access to health centers can affect the occurrence of infectious diseases in large communities [11]. Soltani et al.'s study on the challenges of health services during the Arbaeen ceremony reveals that the Iraqi health system faces many difficulties during the Arbaeen pilgrimage. These challenges are compounded by the infrastructural deficiencies in the Iraqi health system, the lack of detailed planning, and the ignorance of the participants. To address these challenges and minimize problems, the authorities of the Iraqi health system should cooperate with organizations from other countries participating in the Arbaeen pilgrimage to foster collaboration and provide health and treatment equipment and facilities. Additionally, multiorganizational comprehensive planning and internal and external coordination before the Arbaeen pilgrimage, along with the education of pilgrims, are two key factors that can help ensure better organization of the ceremonies [12].
Additionally, during the days of Arbaeen, the control of contagious diseases is very challenging due to the low readiness of health systems, lack of equipment, inappropriate weather conditions [4], high population density [2, 4, 11], an unresilient health infrastructure, limited control of infectious diseases, and a low understanding of health risk factors among participants [2]. This is consistent with the challenges identified in the present study.
In another study, Kheradmand et al. identified nine main categories as required factors: trauma system, disease care system, health issues, education and health promotion, coordination and command of health cooperation within the health system, information management and communication, response planning, support and resource management, and safety and security [27]. These findings are consistent with our results.
Even with advanced equipment and adequate resources for disease prevention and control, the public health system can be under severe pressure. Facilities can influence the occurrence of infectious diseases in mass gatherings. Therefore, planners should pay attention to these factors during preparation. To prevent infectious diseases and their consequences, comprehensive planning, rapid diagnosis, and effective management are necessary [4]. Additionally, it is essential to have equipment, facilities, and specialized personnel available at the site of health service provision, based on needs assessments and studies [11].
In the review study by Moulaei et al., the most frequent challenges identified include the spread of infectious diseases, poor management of the health system in Iraq regarding the collection and disposal of waste, an increase in the incidence of walking injuries among pilgrims (such as burns, fractures, lacerations, wounds, and blisters), and insufficient knowledge about personal and public health. The most important facilitators to address these challenges are specialized training for pilgrims, focused on vital procedures, extensive coordination among stakeholders (such as Health Ministries and Organizations), and the implementation of an agile syndromic system for rapid monitoring and identification of infectious diseases. These factors have also been identified in the findings of this study [13].
Additionally, Mohammadinia et al. reviewed the condition of outpatients during the Arbaeen pilgrimage as a cross-sectional study in temporary clinics and health stations, where pilgrims required nursing, midwifery, and medical services provided by general and specialist doctors along the route from Najaf to Karbala, Iraq. The most common chief complaints reported by patients include 21% for musculoskeletal problems, 20% for foot blisters, and 20% for skin lesions, indicating the need for more organized services, especially in emergency health care, as well as the necessity of paying increasing attention to the health history of the pilgrims who participated in this ceremony [28]. Furthermore, various studies have emphasized the importance of psychological preparation and the provision of psychological solutions [29, 30].
Limitations of this research include the lack of cooperation from some managers and employees, as well as the unavailability of certain individuals. These challenges often create difficulties in collecting comprehensive data. However, by clearly explaining the research objectives and emphasizing the necessity of coordination within the research team, many of these issues were mitigated.
Our results highlight the undeniable need for MTMCs during the Arbaeen pilgrimage, which significantly impacts the health system’s capacity. However, this necessity also brings substantial challenges in delivering healthcare services. Our study not only addresses all previously identified challenges but also brings attention to several new issues, such as environmental conditions (heat waves, dust, etc.), cultural differences, and personnel adaptation considerations. Solutions such as proper planning, resource allocation, addressing infrastructural gaps, improving coordination, and fostering a spirit of volunteerism can enhance the resilience and adaptability of these centers. Ultimately, the strategies and solutions proposed by the participants aim to improve the health of millions of pilgrims by categorizing and presenting specific approaches to tackle all existing challenges.
Conclusion
The main challenges faced by military temporary medical centers are resources and infrastructure, leadership and organization, community and knowledge, and health and safety, while the promotion strategies encompasses resource optimization, leadership and development, community awareness, and health and safety.
Acknowledgments: We are grateful to all those who assisted us during this study.
Ethical Permissions: This study is in accordance with the Declaration of Helsinki and has been approved as a research project by the Ethics Committee of Aja University of Medical Sciences (Code: IR.AJAUMS.REC.1402.044). The participants provided written and verbal informed consent before the interviews, along with explanations of the study’s objectives and methods. They were assured that the recorded interviews would be deleted after the study concluded and that their personal information would remain confidential. Additionally, they were informed that they could withdraw from the study at any time.
Conflicts of Interests: The authors reported no conflicts of interests concerning the publication of this manuscript.
Authors' Contribution: Zibasokhan Sh (First Author), Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (30%); Sharififar S (Second Author), Methodologist/Assistant Researcher/Discussion Writer (15%); Azizi M (Third Author), Introduction Writer (15%); Teymouri F (Fourth Author), Methodologist/Assistant Researcher (20%); Azarmi S (Fifth Author), Introduction Writer (10%)
Funding/Support: No financial support was received for this study.
The Arbaeen pilgrimage is considered one of the largest peaceful human gatherings in the contemporary world [1]. Every year, approximately 17 to 20 million people from different countries participate in this great march [2]. These events pose significant public health challenges related to the well-being of participants and the provision of healthcare services [3].
If a mass gathering is not carefully managed, it can lead to the spread of infectious diseases, threatening global health security and even the political stability of countries [4]. During the Arbaeen pilgrimage, like any other human gathering, the combination of population density and nonobservance of basic hygiene principles has contributed to the increased spread of communicable diseases [5]. Gastrointestinal diseases are also prevalent due to cultural differences in eating habits across countries [6]. Additionally, heatstroke can occur because of the high temperatures in Iraq during the summer season of the pilgrimage [7]. Musculoskeletal disorders may arise from not adhering to basic walking principles, while skin diseases and blisters on the feet can result from wearing inappropriate shoes or walking nonstop without rest [5]. As a result, pilgrims often seek medical care along the pilgrimage route [1]. According to the Iranian Red Crescent Society, during the 2023 Arbaeen pilgrimage, healthcare services were provided to pilgrims at military temporary medical centers (MTMCs) [8].
MTMCs are practical solutions for meeting health and treatment demands in mass gatherings, such as the Arbaeen pilgrimage [9]. MTMCs have key features, such as rapid deployment for urgent medical needs, increased patient care capacity, addressing a variety of medical needs—including first aid, chronic disease management, and physical and mental preventive care—and providing basic medical services, including triage, treatment, and coordination with local healthcare systems and emergency response teams [10, 11]. In addition, considering the long distances and numerous health challenges that pilgrims face, MTMCs play a vital role in ensuring the health and safety of pilgrims [12, 13].
Various quantitative and qualitative studies in countries, such as China, the United States, and Spain have examined the challenges faced by medical centers and temporary hospitals in disasters. Some of the reported challenges included a lack of human resources and equipment, an inability to predict the number of patients, and communication problems. Additionally, there is the difficulty of sending a large number of experienced specialists with relevant clinical records to these centers [14-17]. Another study that examined the challenges of MTMCs during Arbaeen reported a lack of experienced health workers [18]. Overcoming these challenges and improving MTMCs requires a multifaceted approach. According to a study, strategies such as surge capacity management, staff training, and enhanced communication systems are crucial [14].
According to the aforementioned cases and the special importance of holding the Arbaeen pilgrimage in Islamic countries, especially Iran, health issues and facilities should be taken into consideration. Although studies have been conducted in this field, our understanding of the challenges and promotion strategies of MTMCs within our country’s context is still limited. This study was conducted to address the existing research gap, enhance our understanding of the challenges and promotion strategies of MTMCs during the Arbaeen pilgrimage, and provide new information for improving the health and safety of pilgrims.
Participants and Methods
The present qualitative research with a conventional content analysis approach, utilizing Granheim and Lundman’s method for data analysis, was conducted at the military temporary facilities providing health services along the route where the Arbaeen pilgrimage ritual takes place, including clinics, health treatment centers, and sites located in the Ilam and Khuzestan Provinces in Iran in 2024 [19].
The participants were selected using a purpose-based sampling method with maximum diversity. These individuals are better positioned than others to describe the various aspects of the challenges and promotion strategies of MTMCs. Therefore, sampling with maximum diversity [20] was conducted from MTMCs located in Ilam and Khuzestan Provinces in Iran. The participants included executive directors, policymakers, physicians, nurses, health and paraclinical staff in MTMCs, Iranian patients, and other individuals referred to MTMCs during the Arbaeen days (such as patients’ companions), as well as personnel from cooperating and supporting organizations within the health system during the 2024 Arbaeen event. The interviews continued until data saturation was reached, ensuring that no new issues were raised in subsequent interviews. The participants consisted of 15 individuals, including 4 managers, 8 health workers, 1 patient companion, and 2 patients from MTMCs.
Semi-structured interviews based on an interview guide were used to collect information. From the beginning, the purpose of the study was explained to the participants, and after obtaining written consent and observing ethical considerations (such as keeping information confidential and the right of participants to withdraw from the research at any time), the interviews were conducted and recorded with the participants’ consent. Ten interviews were conducted face-to-face, and five were conducted over the phone, each lasting between 30 and 45 minutes. The interviews were conducted individually. The interviews continued until information saturation was achieved, and no new topics were raised in subsequent interviews [21].
At the beginning of the interview, general questions, such as “Can you describe your experience of a day’s work or attending an MTMC?” and “What are the health challenges in MTMCs during the Arbaeen pilgrimage?” were asked, along with “What strategies do you suggest to improve health services in MTMCs during the Arbaeen pilgrimage for the coming years?” The participants were then asked probing questions such as “Can you elaborate on this?” The interviews followed this format. Finally, the participants were asked to express any additional comments they wished to share. The location of the interviews was determined according to the preferences of the participants. Field notes were another method of data collection considered during the data analysis. In this case, the researcher visited several centers and recorded his observations.
The interviews were first transcribed using Microsoft Word software. The transcripts of the interviews were read several times by the researchers for overall understanding. To analyze the data, Granheim and Lundman’s conventional content analysis method was used [19]. During the data collection process, the researchers performed coding analysis and continuous comparisons. Similar codes were grouped into subcategories and then organized into categories based on the similarities and differences among the subcategories.
Findings
The mean age of the participants was 43 years, and their mean work experience was 14 years (Table 1).
Table 1. Individual characteristics of the participants
The initial codes obtained from the interviews totaled 1,576 codes. After integration through conventional conceptual analysis, these codes were classified into two domains: challenges and promotion strategies. The specific strategies and solutions expressed by the participants for all the existing challenges were categorized and presented.
In the challenges domain, there were 4 main categories and 10 subcategories, including resources and infrastructure (equipment challenges, logistical challenges, environmental challenges), leadership and organization (command and management challenges, manpower challenges), community and knowledge (informational and educational challenges, pilgrims’ challenges), and health and safety (disease control challenges, health challenges, safety and security challenges; Table 2).
Table 2. Categories and sub-categories of challenges at military temporary medical centers (MTMCs)
In the promotion strategies domain, there were 4 main categories and 10 subcategories, including resource optimization (equipment enhancement, environmental adaptation, logistics improvement), leadership and development (effective management, manpower development), community and awareness (support for pilgrims, information and education outreach), and health and safety (safety and security measures, health promotion, disease prevention and control; Table 3).
Table 3. Categories and sub-categories of promotion strategies at military temporary medical centers (MTMCs)
Resources and infrastructure
Equipment challenges
MTMCs in the Arbaeen pilgrimage face a shortage of medical, pharmaceutical, and communication equipment. Due to the tent structure of these centers and the heat of the air, a large amount of cooling equipment is needed. Notably, maintenance and repair of equipment in these difficult conditions is also a major challenge.
One of the participants stated, “The temperature in the area where we were over 50 degrees and the air conditioners did not respond to the entire space of the center, it was very difficult to work in those tents.” [Participant 2]
Logistics challenges
Transporting equipment and medicines to remote and scattered areas, managing traffic and procurement, and addressing storage and financial issues are important logistical challenges. Additionally, the distribution of facilities among centers is also very important.
Environmental challenges
Unfavorable weather conditions, dust, heat, and poor access to roads can negatively affect the performance of MTMCs. These conditions can reduce the efficiency of equipment and increase the risk of weather-related diseases.
One of the participants stated, “The roads had terrible conditions, and we could only go back and forth with a series of special cars, and of course, in that weather, the cars sometimes did not even have air conditioners.” [Participant 11]
Leadership and organization
Command and management challenges
Coordination among different treatment teams, management of human resources and volunteers, appropriate placement of centers, creation of a registration and screening system for patients, and quick decision-making in emergency situations are among the challenges of command and management in these centers. A lack of strong management structures can lead to reduced efficiency and increased risks.
Manpower challenges
A lack of specialized and trained manpower, fatigue, and high work pressure are the most important challenges in this field. Additionally, attracting human resources under harsh environmental conditions is difficult and should be recognized.
One of the participants stated, "Before sending the personnel, people who are experienced in the required fields should be selected. Sometimes people come who do not have the experience and special expertise of the existing conditions and cannot provide special help." [Participant 5]
Community and knowledge
Informational and educational challenges
Proper training for employees and pilgrims regarding disease prevention and management methods, the use of medical equipment, and compliance with health guidelines are among the informational and educational challenges. Furthermore, there is a need for efficient information systems to manage data and information.
Pilgrims’ challenges
Pilgrims may constitute a vulnerable group with specific underlying diseases. Additionally, providing medical services to pilgrims from diverse language and cultural backgrounds is also a major challenge.
One of the participants stated, "You can imagine that almost all languages and cultures are different from the clients, and it was truly difficult to communicate properly with them." [Participant 2]
Health and safety
Disease control challenges
A large gathering of pilgrims in one place can lead to the spread of infectious diseases. The management and control of these diseases require detailed planning and interdepartmental cooperation. Additionally, the provision of sufficient equipment and medicines to address the spread of diseases is also highly important.
One of the participants stated, "There was not much supervision over the cooking and distribution of food, and sometimes you go to the food distribution centers and there is a lot of garbage with flies and mosquitoes." [Participant 10]
Health challenges
The large gathering of pilgrims in one location, along with the lack of sanitary facilities, safe drinking water, and poor environmental hygiene, can lead to numerous physical and mental health problems.
One of the participants stated, "Because most of the processions served food in disposable containers, there was a lot of garbage around the pilgrims' accommodations and routes, and some pilgrims did not expect this situation at all and were very worried about their health." [Participant 8]
Security and safety challenges
Ensuring the safety of pilgrims and employees against various threats, including terrorist attacks and natural disasters, is crucial. Additionally, the safety of equipment and buildings should also be considered.
Resource optimization
Equipment enhancement
Upgrading and improving equipment, as well as modifying the design and structure of MTMCs, play an important role in enhancing the quality of medical services provided to pilgrims. By using advanced and up-to-date medical, welfare, and communication equipment, patients can be treated more effectively, and problems can be prevented.
Environmental adaptation
Adapting MTMCs to the environmental conditions of the Arbaeen pilgrimage, including temperature, humidity, and weather conditions, is of great importance. By adjusting equipment and facilities to these conditions, we can ensure the optimal performance of treatment centers and provide better services to pilgrims.
One of the participants stated: "Almost all roads and trails are dirt, so due to the high dust, tents should be equipped with air purifiers." [Participant 11]
Logistics improvement
Improvement of logistics services in MTMCs, including the timely transfer and distribution of needed items and proper storage, plays a significant role in increasing the efficiency and effectiveness of these centers. With proper resource management and careful planning, we can avoid shortages and logistical issues.
One of the participants stated: "Many times, with planning and distribution management, we can prevent wasted costs and shortages." [Participant 3]
Leadership and development
Effective management
Improving command and management through the establishment of efficient management structures and necessary training for staff can enhance the coordination and efficiency of these centers. With proper management and timely decision-making, we can prevent problems and miscoordination.
Manpower development
Allocating manpower in the appropriate numbers and paying attention to work and rest schedules greatly helps to improve the services provided.
One of the participants stated: "A sufficient number of personnel, especially women, can help a lot." [Participant 9]
Community and awareness
Information and education outreach
Enhancing the skills of staff through specialized training can significantly improve the quality of healthcare services in MTMCs during the Arbaeen pilgrimage. By boosting staff capabilities, we can deliver more effective and higher-quality services.
One of the participants stated: "Personnel should be trained according to the existing conditions before being sent, and great care should be taken in selecting efficient personnel." [Participant 3]
Support pilgrims
In MTMCs during the Arbaeen pilgrimage, it is crucial to adapt healthcare services to accommodate the diverse cultural backgrounds of pilgrims. This includes understanding and respecting different cultural practices and beliefs to provide effective care. Additionally, managing chronic diseases such as diabetes and hypertension is essential, as these conditions can be exacerbated by the physical demands of the pilgrimage.
Health and safety
Disease prevention and control
Paying attention to the quality of water and food, as well as the vectors in the region, along with providing care and prevention methods such as vaccination, greatly helps to control epidemics.
Health promotion
Providing health consultations and distributing hygiene materials such as masks and sanitizers can help reduce the burden of illnesses and health issues during the Arbaeen pilgrimage.
One of the participants stated: "For the paths, a bunch of people are needed to collect the garbage and give the necessary training to the pilgrims." [Participant 8]
Safety and security measures
Improving security and safety in MTMCs through the establishment of appropriate infrastructure and the implementation of safety protocols can help reduce risks and adverse incidents. By creating a safe and secure environment, we can protect the health and well-being of pilgrims.
One of the participants stated: "Safety and security should be given a lot of attention by the officials and specialized teams should be sent for this work" [Participant 10]
The promotion strategies presented included resource optimization, effective management, and tailored health and safety measures. These strategies provide actionable recommendations for policymakers and planners to enhance the efficiency and effectiveness of MTMCs during mass gatherings.
Discussion
This study aimed to examine the challenges faced by military temporary medical centers and identify solutions to overcome these challenges. The results highlight the existence of ten subcategories that express the challenges in MTMCs. Several studies, both inside and outside the country, have investigated the issue of health and the challenges of providing health services in mass gatherings. There is a high prevalence of infectious diseases, such as those observed during the Hajj and Arbaeen pilgrimage, in mass gatherings [22-24]. Infectious diseases are the most common health threat associated with mass gatherings [2, 4]. Viral respiratory infections are a significant public health concern that can cause serious illness, especially in vulnerable populations [25].
The needs and challenges of providing health services in MTMCs during the Arbaeen pilgrimage ceremony vary each year and depend on the season in which the ceremony is held [4]. Those planning mass gatherings should also consider the seasonality of some common conditions, such as flu-like symptoms, which may be more likely to occur in relatively colder months, and cases of diarrhea and food poisoning, which may be more common in warmer months [24]. According to a study by Al-Ansari et al. from Australia in 2021, one out of every five participants in the Arbaeen ceremony has a cough, and one out of eight experiences diarrhea. These results highlight the need for governments, religious authorities, and participants in Arbaeen to plan and implement preventive measures to prevent the spread of more serious infections. Such measures can include health initiatives, health education, health equipment, and proper management of water and sewage resources [26].
Access to health centers can affect the occurrence of infectious diseases in large communities [11]. Soltani et al.'s study on the challenges of health services during the Arbaeen ceremony reveals that the Iraqi health system faces many difficulties during the Arbaeen pilgrimage. These challenges are compounded by the infrastructural deficiencies in the Iraqi health system, the lack of detailed planning, and the ignorance of the participants. To address these challenges and minimize problems, the authorities of the Iraqi health system should cooperate with organizations from other countries participating in the Arbaeen pilgrimage to foster collaboration and provide health and treatment equipment and facilities. Additionally, multiorganizational comprehensive planning and internal and external coordination before the Arbaeen pilgrimage, along with the education of pilgrims, are two key factors that can help ensure better organization of the ceremonies [12].
Additionally, during the days of Arbaeen, the control of contagious diseases is very challenging due to the low readiness of health systems, lack of equipment, inappropriate weather conditions [4], high population density [2, 4, 11], an unresilient health infrastructure, limited control of infectious diseases, and a low understanding of health risk factors among participants [2]. This is consistent with the challenges identified in the present study.
In another study, Kheradmand et al. identified nine main categories as required factors: trauma system, disease care system, health issues, education and health promotion, coordination and command of health cooperation within the health system, information management and communication, response planning, support and resource management, and safety and security [27]. These findings are consistent with our results.
Even with advanced equipment and adequate resources for disease prevention and control, the public health system can be under severe pressure. Facilities can influence the occurrence of infectious diseases in mass gatherings. Therefore, planners should pay attention to these factors during preparation. To prevent infectious diseases and their consequences, comprehensive planning, rapid diagnosis, and effective management are necessary [4]. Additionally, it is essential to have equipment, facilities, and specialized personnel available at the site of health service provision, based on needs assessments and studies [11].
In the review study by Moulaei et al., the most frequent challenges identified include the spread of infectious diseases, poor management of the health system in Iraq regarding the collection and disposal of waste, an increase in the incidence of walking injuries among pilgrims (such as burns, fractures, lacerations, wounds, and blisters), and insufficient knowledge about personal and public health. The most important facilitators to address these challenges are specialized training for pilgrims, focused on vital procedures, extensive coordination among stakeholders (such as Health Ministries and Organizations), and the implementation of an agile syndromic system for rapid monitoring and identification of infectious diseases. These factors have also been identified in the findings of this study [13].
Additionally, Mohammadinia et al. reviewed the condition of outpatients during the Arbaeen pilgrimage as a cross-sectional study in temporary clinics and health stations, where pilgrims required nursing, midwifery, and medical services provided by general and specialist doctors along the route from Najaf to Karbala, Iraq. The most common chief complaints reported by patients include 21% for musculoskeletal problems, 20% for foot blisters, and 20% for skin lesions, indicating the need for more organized services, especially in emergency health care, as well as the necessity of paying increasing attention to the health history of the pilgrims who participated in this ceremony [28]. Furthermore, various studies have emphasized the importance of psychological preparation and the provision of psychological solutions [29, 30].
Limitations of this research include the lack of cooperation from some managers and employees, as well as the unavailability of certain individuals. These challenges often create difficulties in collecting comprehensive data. However, by clearly explaining the research objectives and emphasizing the necessity of coordination within the research team, many of these issues were mitigated.
Our results highlight the undeniable need for MTMCs during the Arbaeen pilgrimage, which significantly impacts the health system’s capacity. However, this necessity also brings substantial challenges in delivering healthcare services. Our study not only addresses all previously identified challenges but also brings attention to several new issues, such as environmental conditions (heat waves, dust, etc.), cultural differences, and personnel adaptation considerations. Solutions such as proper planning, resource allocation, addressing infrastructural gaps, improving coordination, and fostering a spirit of volunteerism can enhance the resilience and adaptability of these centers. Ultimately, the strategies and solutions proposed by the participants aim to improve the health of millions of pilgrims by categorizing and presenting specific approaches to tackle all existing challenges.
Conclusion
The main challenges faced by military temporary medical centers are resources and infrastructure, leadership and organization, community and knowledge, and health and safety, while the promotion strategies encompasses resource optimization, leadership and development, community awareness, and health and safety.
Acknowledgments: We are grateful to all those who assisted us during this study.
Ethical Permissions: This study is in accordance with the Declaration of Helsinki and has been approved as a research project by the Ethics Committee of Aja University of Medical Sciences (Code: IR.AJAUMS.REC.1402.044). The participants provided written and verbal informed consent before the interviews, along with explanations of the study’s objectives and methods. They were assured that the recorded interviews would be deleted after the study concluded and that their personal information would remain confidential. Additionally, they were informed that they could withdraw from the study at any time.
Conflicts of Interests: The authors reported no conflicts of interests concerning the publication of this manuscript.
Authors' Contribution: Zibasokhan Sh (First Author), Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (30%); Sharififar S (Second Author), Methodologist/Assistant Researcher/Discussion Writer (15%); Azizi M (Third Author), Introduction Writer (15%); Teymouri F (Fourth Author), Methodologist/Assistant Researcher (20%); Azarmi S (Fifth Author), Introduction Writer (10%)
Funding/Support: No financial support was received for this study.
Keywords:
Military Personnel [MeSH], Disease [MeSH], Interview [MeSH], Health [MeSH], Qualitative Research [MeSH]
References
1. Farahani AJ, Zijoud SRH. Research and researchers of hygiene, medicine and health field in the service of Arbaeen walk. J Mil Med. 2019;21(6):547-8. [Persian] [Link]
2. Hamdanieh L, Ostadtaghizadeh A. Arbaeen in the context of the COVID-19 pandemic. Disaster Med Public Health Prep. 2021;15(4):e16. [Link] [DOI:10.1017/dmp.2020.362]
3. Memish ZA, Zumla A, Alhakeem RF, Assiri A, Turkestani A, Al Harby KD, et al. Hajj: Infectious disease surveillance and control. Lancet. 2014;383(9934):2073-82. [Link] [DOI:10.1016/S0140-6736(14)60381-0]
4. Karampourian A, Ghomian Z, Khorasani-Zavareh D. Exploring challenges of health system preparedness for communicable diseases in Arbaeen mass gathering: A qualitative study. F1000Res. 2018;7:1448. [Link] [DOI:10.12688/f1000research.15290.1]
5. Mehrabi Tavana A. Examining common diseases in the Arbaeen ceremony and prevention strategies. J Combat Med. 2023;6(1):26-31. [Persian] [Link]
6. Nazari A, Noori G, Mohammadyari E, Taebi G, Tavan H. Survey of infectious and non-infectious diseases and the survival of pilgrims at health centers of Ilam on the day of Arbaeen in 2016. Iran Red Crescent Med J. 2018;20(S1):1-2. [Link] [DOI:10.5812/ircmj.14538]
7. Choi YW, Eltahir E. Heat stress during Arba'een foot‐pilgrimage (world's largest gathering) projected to reach "dangerous" levels due to climate change. Geophys Res Lett. 2022;49. [Link] [DOI:10.1029/2022GL099755]
8. I. R. Crescent. Providing relief to more than 24 thousand people under the relief of Arbaeen 2023 [Internet]. Tehran: Iranian Red Crescent; 2023 [cited 2025 August 28]. Available from: https://rcs.ir/portal/newsview/193956. [Persian] [Link]
9. Brown JF, Smith JG, Tataris K. Medical management of mass gatherings. In: Emergency Medical services: Clinical practice and systems oversight. Hoboken: John Wiley & Sons; 2015. p. 264-71. [Link] [DOI:10.1002/9781118990810.ch101]
10. Park D, Kim Y. Awareness of temporary field emergency medical centers operated by paramedics on a first-come-first-served basis in a mass casualty disaster. Fire Sci Eng. 2021;35(2):101-7. [Link] [DOI:10.7731/KIFSE.5144ce33]
11. Farahmand F, Hayati F, Mousavi-Roknabadi RS, Safaei-Firouzabadi H, Hosseini-Marvast SR, Mohsenian L. Treatment camp and patients in Arbaeen pilgrimage in 2019. Int J Travel Med Glob Health. 2022;10(1):24-31. [Link] [DOI:10.34172/ijtmgh.2022.05]
12. Soltani A, Aram M, Alaeddini F, Ahmadi Marzaleh M. Challenges of health services during Arbaeen pilgrimage in 2019. Iran Red Crescent Med J. 2021;23(4):e678. [Link]
13. Moulaei K, Bastaminejad S, Haghdoost A. Health challenges and facilitators of Arbaeen pilgrimage: A scoping review. BMC Public Health. 2024;24(1):132. [Link] [DOI:10.1186/s12889-024-17640-9]
14. Hamis AA, Md Bukhori AB, Heng PP, Jane Ling MY, Shaharuddin MA, A Fauzi NAF, et al. Strategies, challenges and opportunities in the implementation of COVID-19 field hospitals: A scoping review. BMJ Open. 2023;13(3):e067227. [Link] [DOI:10.1136/bmjopen-2022-067227]
15. Castro Delgado R, Pérez Quesada P, Pintado García E, Marañón Zabalza I, Vallina-Victorero Vázquez M, Escribano Balín R. Alternate care sites for COVID-19 patients: Experience from the H144 hospital of the health service of the principality of Asturias, Spain. Prehosp Disaster Med. 2021;36(6):774-81. [Link] [DOI:10.1017/S1049023X21001102]
16. Chen Z, He S, Li F, Yin J, Chen X. Mobile field hospitals, an effective way of dealing with COVID-19 in China: Sharing our experience. Biosci Trends. 2020;14(3):212-4. [Link] [DOI:10.5582/bst.2020.01110]
17. Baughman AW, Hirschberg RE, Lucas LJ, Suarez ED, Stockmann D, Hutton Johnson S, et al. Pandemic care through collaboration: Lessons from a COVID-19 field hospital. J Am Med Dir Assoc. 2020;21(11):1563-7. [Link] [DOI:10.1016/j.jamda.2020.09.003]
18. Lami F, Ali AA, Fathullah K, Abdullatif H. Assessment of temporary medical clinics during the Arbaeenia mass gathering at Al-Karkh, Baghdad, Iraq, in 2014: Cross-sectional study. JMIR Public Health Surveill. 2019;5(3):e10903. [Link] [DOI:10.2196/10903]
19. Graneheim UH, Lundman B. Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105-12. [Link] [DOI:10.1016/j.nedt.2003.10.001]
20. Pezalla AE, Pettigrew J, Miller-Day M. Researching the researcher-as-instrument: An exercise in interviewer self-reflexivity. Qual Res. 2012;12(2):165-85. [Link] [DOI:10.1177/1468794111422107]
21. Porter DJ, Cooper S. The practice of nursing research: Appraisal, synthesis and generation of evidence. 6th ed. N. Burns, S.K. Grove. Saunders Elsevier, St Louis, Missouri (2009). ISBN: 9781416054689-hbk, £45.99. Int Emerg Nurs. 2009;17(3):188-9. [Link]
22. Al-Lami F, Al-Fatlawi A, Bloland P, Nawwar A, Jetheer A, Hantoosh H, et al. Pattern of morbidity and mortality in Karbala hospitals during Ashura mass gathering at Karbala, Iraq, 2010. East Mediterr Health J. 2013;19 Suppl 2:S13-8. [Link] [DOI:10.26719/2013.19.Supp2.S13]
23. Alqahtani AS, Wiley KE, Tashani M, Willaby HW, Heywood AE, BinDhim NF, et al. Exploring barriers to and facilitators of preventive measures against infectious diseases among Australian Hajj pilgrims: Cross-sectional studies before and after Hajj. Int J Infect Dis. 2016;47:53-9. [Link] [DOI:10.1016/j.ijid.2016.02.005]
24. Lami F, Amiri M, Majeed Y, Barr KM, Nsour MA, Khader YS. Real-time surveillance of infectious diseases, injuries, and chronic conditions during the 2018 Iraq Arba'een mass gathering. Health Secur. 2021;19(3):280-7. [Link] [DOI:10.1089/hs.2020.0074]
25. Alfelali M, Haworth EA, Barasheed O, Badahdah AM, Bokhary H, Tashani M, et al. Facemask against viral respiratory infections among Hajj pilgrims: A challenging cluster-randomized trial. PLoS One. 2020;15(10):e0240287. [Link] [DOI:10.1371/journal.pone.0240287]
26. Al-Ansari F, Al Ansari M, Hill-Cawthorne GA, Abdulzahra MS, Al-Ansari MB, Al-Ansari B, et al. Arbaeen public health concerns: A pilot cross-sectional survey. Travel Med Infect Dis. 2020;35:101546. [Link] [DOI:10.1016/j.tmaid.2019.101546]
27. Kheradmand JA, Khankeh H, Borujeni SMH, Nasiri A, Shahrestanki YA, Ghanbari V, et al. Analysis of healthcare services in 2019 Arbaeen March: A qualitative study. Health Emerg Disasters Q. 2024;9(2):125-36. [Link] [DOI:10.32598/hdq.9.2.524.1]
28. Mohammadinia L, Sharifisadeh M, Lashkari H, Moradian F, Choobineh H. A review of the condition of OPD patients in Arba'een on-foot pilgrimage in 2019. Iran Red Crescent Med J. 2021;23(2). [Link]
29. Akbari K, Zareiyan A, Yari A, Najafi M, Azizi M, Ostadtaghizadeh A. Mental health preparedness and response to epidemics focusing on COVID-19 pandemic: A qualitative study in Iran. BMC Public Health. 2024;24(1):1980. [Link] [DOI:10.1186/s12889-024-19526-2]
30. Madani SMS, Bahramnejad A, Farsi Z, Alizadeh A, Azizi M. The effect of psychological first-aid virtual education on the communication skills of nurses in disasters: A randomized controlled trial. BMC Psychol. 2024;12(1):194. [Link] [DOI:10.1186/s40359-024-01682-0]









