Volume 17, Issue 3 (2025)
Iran J War Public Health 2025, 17(3): 319-323 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2025/05/23 | Accepted: 2025/06/28 | Published: 2025/07/8
Received: 2025/05/23 | Accepted: 2025/06/28 | Published: 2025/07/8
How to cite this article
NagaRaju D, Subramanian S, Koganti V, Shekhar S, Himabindu K, Alagesan J, et al . Persistent Musculoskeletal, Cardiopulmonary, Neurological, and Psychiatric Symptoms Among COVID-19 Survivors. Iran J War Public Health 2025; 17 (3) :319-323
URL: http://ijwph.ir/article-1-1599-en.html
URL: http://ijwph.ir/article-1-1599-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Authors
D. NagaRaju1, S. Subramanian *1, V.B. Koganti2, S.P.C. Shekhar3, K. Himabindu4, J. Alagesan5, D. Indrani1, S. Vishnuram1
1- Saveetha College of Physiotherapy, Saveetha Institute of Medical and Technical Sciences, Chennai, India
2- Department of Physiotherapy, Nimra Institute of Medical Sciences, Jupudi, India
3- Department of Physiotherapy, Faculty of Cardio Physiotherapy., KNR University of Health Sciences, Hyderabad, India
4- Department of Physiotherapy, School of Health Sciences, Apollo University, Murukampattu, India
5- Department of Physiotherapy, School of Paramedical, Mohan Babu University, Tirupati, India
2- Department of Physiotherapy, Nimra Institute of Medical Sciences, Jupudi, India
3- Department of Physiotherapy, Faculty of Cardio Physiotherapy., KNR University of Health Sciences, Hyderabad, India
4- Department of Physiotherapy, School of Health Sciences, Apollo University, Murukampattu, India
5- Department of Physiotherapy, School of Paramedical, Mohan Babu University, Tirupati, India
Full-Text (HTML) (3 Views)
Introduction
The COVID-19 pandemic has emerged as one of the most profound global health challenges since its onset in late 2019 [1]. While much of the existing literature has concentrated on the acute phase of the disease—characterized by respiratory distress, fever, and systemic inflammation—recent attention has shifted toward the long-term symptoms experienced by survivors [2]. These persistent symptoms, commonly referred to as “Long COVID” or “Post-acute Sequelae of SARS-CoV-2 Infection” (PASC), encompass a broad spectrum of physical, neurological, and psychological effects that may persist for months or even years after the initial recovery [2-5].
“Long COVID” is now increasingly recognized as a complex, multisystem condition that significantly impairs quality of life and continues to strain healthcare systems worldwide [2-6]. Evidence suggests that a substantial proportion of individuals experience persistent symptoms regardless of the severity of their initial infection [6-8]. Commonly reported manifestations include musculoskeletal symptoms such as muscle pain, joint discomfort, and fatigue, which negatively impact physical function and daily activities [7, 9, 10]. Cardiopulmonary symptoms, including dyspnea and chest pain, may indicate ongoing respiratory or cardiovascular dysfunction and are sometimes associated with complications like pulmonary fibrosis or myocarditis [10, 11].
Neurological symptoms, such as cognitive impairment (“brain fog”), paresthesia, and insomnia indicate the neurotropic potential of SARS-CoV-2 and its effects on the central and peripheral nervous systems [8, 12-14]. Psychiatric manifestations, including depression, anxiety, and social withdrawal, further complicate recovery, highlighting the interplay between mental and physical health in the post-COVID-19 phase [15]. The diversity and persistence of these symptoms underscore the need for comprehensive investigations that quantify their prevalence, duration, and impact on survivors’ overall well-being.
Despite the growing body of evidence, significant gaps remain in the understanding of Long COVID, particularly among non-hospitalized individuals and in underrepresented regions such as South Asia. Most existing studies have focused on Western populations or hospitalized cohorts, offering limited insight into communities with different healthcare access, cultural contexts, and recovery environments [16, 17]. Furthermore, the underlying mechanisms—potentially involving chronic inflammation, immune dysregulation, or viral persistence—are still being explored, reinforcing the need for epidemiological data to guide post-COVID clinical management and rehabilitation [11, 14].
Musculoskeletal symptoms, in particular, have emerged as a predominant feature in several studies; however, their long-term course and associated risk factors remain poorly understood [18]. Addressing these knowledge gaps is critical for developing targeted rehabilitation interventions.
Therefore, this study aimed to investigate the prevalence and persistence of musculoskeletal, cardiopulmonary, neurological, and psychiatric symptoms among COVID-19 survivors who attended NRI General Hospital in Andhra Pradesh, India. The objective was to categorize the most prevalent symptoms, examine their duration (ranging from three months to over one year post-recovery), and identify the domains most affected, thereby contributing to the global understanding of post-COVID-19 sequelae and the need for specialized rehabilitation approaches.
Instrument and Methods
This cross-sectional study was conducted at NRI General Hospital in Andhra Pradesh, India, over a one-year period from February 2023 to February 2024. The required sample size was calculated using the formula for cross-sectional studies:
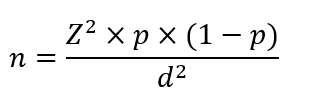
Where Z=1.96 for a 95% confidence level, p=0.5 as the assumed prevalence of persistent symptoms from previous literature, and d=0.09 as the margin of error. Thus, the minimum required sample size was 119 participants. A total of 119 individuals, both men and women under the age of 55 who had recovered from COVID-19, were enrolled from the hospital’s post-COVID follow-up database. Individuals with pre-existing chronic diseases, such as cardiac, respiratory, or autoimmune conditions, as well as those without confirmed COVID-19 infection, were excluded to minimize potential confounding factors.
Data were collected using a structured COVID-19 Survivor Symptom Questionnaire developed and adapted from previously validated tools used in studies on post-acute COVID-19 sequelae. The questionnaire consisted of four main domains—musculoskeletal, cardiopulmonary, neurological, and psychiatric symptoms. The musculoskeletal domain included items, such as muscle pain, joint pain, fatigue, and stiffness; the cardiopulmonary domain covered symptoms like shortness of breath, chest discomfort, palpitations, and cough; the neurological domain assessed headache, dizziness, paresthesia, cognitive impairment, and sleep disturbances; and the psychiatric domain included anxiety, depression, irritability, and social withdrawal. Each participant indicated the presence and duration of each symptom using a four-point ordinal scale, where 1 corresponded to symptoms lasting up to three months, 2 for up to six months, 3 for up to twelve months, and 4 for more than twelve months.
The questionnaire demonstrated good internal consistency, with a Cronbach’s alpha value of 0.86, and its content validity was established through expert evaluation by three physiotherapists and two physicians. The survey was administered in person by trained staff members to ensure clarity, accuracy, and completeness of responses.
The study protocol received approval from the Institutional Ethics Committee of NRI General Hospital and adhered to the ethical standards outlined in the Declaration of Helsinki. Written informed consent was obtained from all participants prior to data collection to ensure voluntary participation and confidentiality.
Data were analyzed using SPSS version 26. To explore associations between demographic factors, such as age and sex and the persistence of symptoms, Chi-square tests were applied, while one-way ANOVA was used to compare the mean duration scores across the four symptom domains. A p-value of less than 0.05 was considered statistically significant.
Findings
A total of 119 participants who had recovered from COVID-19 were included. Among them, musculoskeletal symptoms were the most prevalent, affecting 77 individuals (65%), followed by cardiopulmonary symptoms in 24 participants (20%), neurological symptoms in 12 (10%), and psychiatric symptoms in 6 (5%). The prevalence of musculoskeletal symptoms was significantly higher than that of other categories (p<0.001).
Within the musculoskeletal category, muscle pain was the most commonly reported symptom, experienced by 54 participants (70% of the musculoskeletal group, 45% of the total sample). Joint pain was reported by 39 individuals (50%, 33%), followed by fatigue in 23 (30%, 19%) and muscle weakness in 15 participants (20%, 13%). A substantial proportion of those with fatigue (60%) and muscle weakness (53%) reported symptom persistence beyond 12 months.
Cardiopulmonary symptoms were noted in 24 participants, predominantly shortness of breath (10 participants, 42%) and chest pain (6 participants, 25%), followed by reduced work capacity (5 participants, 21%) and fast or irregular heartbeat (3 participants, 13%). Most of these symptoms showed gradual improvement, with the majority resolving within 6 to 12 months after recovery.
Among the 12 participants who experienced neurological symptoms, cognitive impairments were the most frequent (5 participants, 42%), followed by paraesthesia in 3 (25%), and insomnia and dizziness in 2 participants each (17%). Chi-square analysis revealed that neurological symptoms were more likely to persist for longer durations compared to cardiopulmonary symptoms (p=0.03), particularly cognitive impairments, which often lasted beyond one year.
Psychiatric symptoms were the least reported, affecting only six participants (5% of the total sample). Of these, depression was noted in 3 individuals (50%), anxiety in 2 (33%), and social isolation in 1 (17%). While the prevalence was low, these symptoms underscore the psychological burden that may accompany physical recovery in some COVID-19 survivors. A few participants also reported miscellaneous symptoms that did not fit into the predefined categories but were mild and transient.
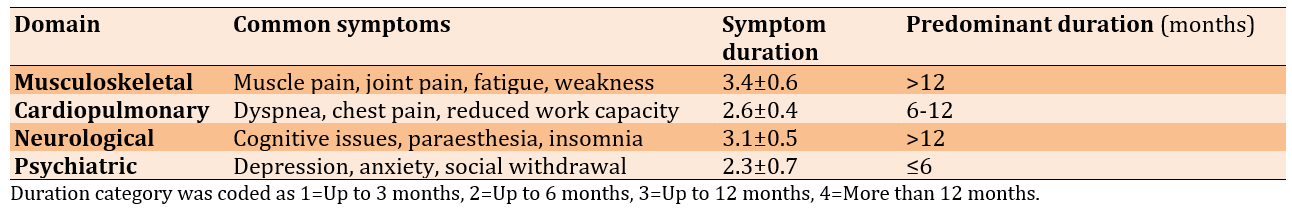
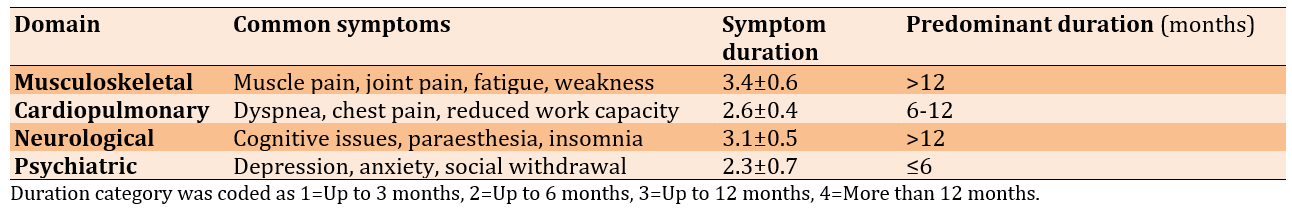
The mean duration scores among the four symptom domains indicated a statistically significant difference (p=0.01), with musculoskeletal symptoms demonstrating the highest mean persistence score, followed by neurological, cardiopulmonary, and psychiatric domains (Table 1).
Table 1. Mean symptom duration among COVID-19 survivors (n=119)
Discussion
This study aimed to investigate the prevalence and persistence of musculoskeletal, cardiopulmonary, neurological, and psychiatric symptoms among COVID-19 survivors. It underscores the significant burden of persistent physical, neurological, and psychological symptoms among individuals recovering from COVID-19, highlighting the multifaceted nature of post-COVID sequelae. Musculoskeletal symptoms, particularly muscle pain, joint pain, and fatigue, were the most frequently reported, affecting nearly half of the participants. This observation is in line with previous research, suggesting that skeletal muscle involvement and prolonged fatigue are among the most disabling consequences of COVID-19 recovery [7, 15, 19]. These manifestations may stem from inflammatory myopathy, mitochondrial dysfunction, and prolonged inactivity during hospitalization or quarantine periods [20, 21]. Furthermore, the persistence of muscle weakness beyond one year in a considerable proportion of participants emphasizes the chronic impact of the virus on functional capacity and overall quality of life.
Cardiopulmonary complaints, although less prevalent than musculoskeletal symptoms, remain clinically relevant. Shortness of breath was the most frequently reported symptom within this domain, often resolving within 6 to 12 months. This finding mirrors trends reported in previous longitudinal studies, which attribute gradual recovery to improved pulmonary rehabilitation strategies and early physiotherapeutic interventions that target respiratory endurance, thoracic mobility, and aerobic reconditioning [21]. The relatively shorter duration of these symptoms in our cohort may reflect the benefits of structured follow-up care and increased awareness of respiratory rehabilitation among post-COVID individuals.
Neurological symptoms, particularly cognitive dysfunction often referred to as “brain fog,” were another important finding. These issues have been hypothesized to result from neuroinflammatory processes, microvascular injury, and direct viral invasion of neural tissues [5, 17-22]. While less common than physical symptoms, their prolonged persistence suggests potential long-term neurocognitive consequences that warrant ongoing monitoring and interdisciplinary rehabilitation approaches. Cognitive training, graded activity programs, and neuromotor exercises may play a vital role in mitigating these effects and restoring functional independence.
Psychiatric symptoms, such as depression, anxiety, and social withdrawal were less frequently reported in our sample but should not be underestimated. The psychological aftermath of COVID-19, influenced by isolation, uncertainty, and physical debilitation, aligns with evidence from recent meta-analyses indicating an increased prevalence of post-traumatic stress and mood disturbances among survivors [6, 23, 24]. These findings reinforce the importance of integrating mental health screening and counseling into post-COVID rehabilitation pathways to promote holistic recovery.
The predominance of long-lasting musculoskeletal impairments highlights an urgent need for structured, evidence-based rehabilitation strategies tailored to post-COVID patients. Physiotherapy-led interventions—such as progressive resistance training, balance and coordination exercises, and digital tele-rehabilitation—have shown substantial efficacy in improving mobility, muscle strength, and activities of daily living [25]. Early initiation of these programs, along with patient education on pacing and graded activity, could prevent deconditioning and enhance recovery outcomes.
Overall, the study contributes to the growing body of evidence emphasizing the long-term functional impact of COVID-19 and the indispensable role of physiotherapists in managing post-COVID syndromes. Future research should focus on longitudinal outcomes, explore gender and age-related differences, and evaluate the effectiveness of specific rehabilitation protocols across diverse patient populations. Addressing these long-lasting issues requires dedicated rehabilitation strategies to improve quality of life and enhance function. Although less frequent, cardiopulmonary, neurological, and psychiatric symptoms continue to affect many individuals, highlighting the need for inclusive post-COVID management plans.
Conclusion
Musculoskeletal symptoms, namely muscle and joint pain, fatigue, and muscle weakness, remain common and often persist for more than a year among COVID-19 survivors.
Acknowledgments: The authors would like to acknowledge all the participants who voluntarily took part in this study. We also extend our sincere thanks to the institutional authorities for their support and cooperation during the conduct of this research.
Ethical Permissions: Ethical approval was obtained from the Institutional Ethics Committee prior to the commencement of the study.
Conflicts of Interests: The authors declared no conflicts of interests.
Authors' Contribution: NagaRaju D (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (20%); Subramanian S (Second Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (15%); Koganti VB (Third Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer (15%); Shekhar SPC (Fourth Author), Methodologist/Assistant Researcher/Discussion Writer (10%); Himabindu K (Fifth Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer (10%); Alagesan J (Sixth Author), Methodologist/Assistant Researcher/Statistical Analyst (10%); Indrani D (Seventh Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer (10%); Vishnuram S (Eighth Author), Methodologist/Assistant Researcher/Statistical Analyst (10%)
Funding/Support: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The COVID-19 pandemic has emerged as one of the most profound global health challenges since its onset in late 2019 [1]. While much of the existing literature has concentrated on the acute phase of the disease—characterized by respiratory distress, fever, and systemic inflammation—recent attention has shifted toward the long-term symptoms experienced by survivors [2]. These persistent symptoms, commonly referred to as “Long COVID” or “Post-acute Sequelae of SARS-CoV-2 Infection” (PASC), encompass a broad spectrum of physical, neurological, and psychological effects that may persist for months or even years after the initial recovery [2-5].
“Long COVID” is now increasingly recognized as a complex, multisystem condition that significantly impairs quality of life and continues to strain healthcare systems worldwide [2-6]. Evidence suggests that a substantial proportion of individuals experience persistent symptoms regardless of the severity of their initial infection [6-8]. Commonly reported manifestations include musculoskeletal symptoms such as muscle pain, joint discomfort, and fatigue, which negatively impact physical function and daily activities [7, 9, 10]. Cardiopulmonary symptoms, including dyspnea and chest pain, may indicate ongoing respiratory or cardiovascular dysfunction and are sometimes associated with complications like pulmonary fibrosis or myocarditis [10, 11].
Neurological symptoms, such as cognitive impairment (“brain fog”), paresthesia, and insomnia indicate the neurotropic potential of SARS-CoV-2 and its effects on the central and peripheral nervous systems [8, 12-14]. Psychiatric manifestations, including depression, anxiety, and social withdrawal, further complicate recovery, highlighting the interplay between mental and physical health in the post-COVID-19 phase [15]. The diversity and persistence of these symptoms underscore the need for comprehensive investigations that quantify their prevalence, duration, and impact on survivors’ overall well-being.
Despite the growing body of evidence, significant gaps remain in the understanding of Long COVID, particularly among non-hospitalized individuals and in underrepresented regions such as South Asia. Most existing studies have focused on Western populations or hospitalized cohorts, offering limited insight into communities with different healthcare access, cultural contexts, and recovery environments [16, 17]. Furthermore, the underlying mechanisms—potentially involving chronic inflammation, immune dysregulation, or viral persistence—are still being explored, reinforcing the need for epidemiological data to guide post-COVID clinical management and rehabilitation [11, 14].
Musculoskeletal symptoms, in particular, have emerged as a predominant feature in several studies; however, their long-term course and associated risk factors remain poorly understood [18]. Addressing these knowledge gaps is critical for developing targeted rehabilitation interventions.
Therefore, this study aimed to investigate the prevalence and persistence of musculoskeletal, cardiopulmonary, neurological, and psychiatric symptoms among COVID-19 survivors who attended NRI General Hospital in Andhra Pradesh, India. The objective was to categorize the most prevalent symptoms, examine their duration (ranging from three months to over one year post-recovery), and identify the domains most affected, thereby contributing to the global understanding of post-COVID-19 sequelae and the need for specialized rehabilitation approaches.
Instrument and Methods
This cross-sectional study was conducted at NRI General Hospital in Andhra Pradesh, India, over a one-year period from February 2023 to February 2024. The required sample size was calculated using the formula for cross-sectional studies:
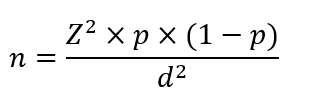
Where Z=1.96 for a 95% confidence level, p=0.5 as the assumed prevalence of persistent symptoms from previous literature, and d=0.09 as the margin of error. Thus, the minimum required sample size was 119 participants. A total of 119 individuals, both men and women under the age of 55 who had recovered from COVID-19, were enrolled from the hospital’s post-COVID follow-up database. Individuals with pre-existing chronic diseases, such as cardiac, respiratory, or autoimmune conditions, as well as those without confirmed COVID-19 infection, were excluded to minimize potential confounding factors.
Data were collected using a structured COVID-19 Survivor Symptom Questionnaire developed and adapted from previously validated tools used in studies on post-acute COVID-19 sequelae. The questionnaire consisted of four main domains—musculoskeletal, cardiopulmonary, neurological, and psychiatric symptoms. The musculoskeletal domain included items, such as muscle pain, joint pain, fatigue, and stiffness; the cardiopulmonary domain covered symptoms like shortness of breath, chest discomfort, palpitations, and cough; the neurological domain assessed headache, dizziness, paresthesia, cognitive impairment, and sleep disturbances; and the psychiatric domain included anxiety, depression, irritability, and social withdrawal. Each participant indicated the presence and duration of each symptom using a four-point ordinal scale, where 1 corresponded to symptoms lasting up to three months, 2 for up to six months, 3 for up to twelve months, and 4 for more than twelve months.
The questionnaire demonstrated good internal consistency, with a Cronbach’s alpha value of 0.86, and its content validity was established through expert evaluation by three physiotherapists and two physicians. The survey was administered in person by trained staff members to ensure clarity, accuracy, and completeness of responses.
The study protocol received approval from the Institutional Ethics Committee of NRI General Hospital and adhered to the ethical standards outlined in the Declaration of Helsinki. Written informed consent was obtained from all participants prior to data collection to ensure voluntary participation and confidentiality.
Data were analyzed using SPSS version 26. To explore associations between demographic factors, such as age and sex and the persistence of symptoms, Chi-square tests were applied, while one-way ANOVA was used to compare the mean duration scores across the four symptom domains. A p-value of less than 0.05 was considered statistically significant.
Findings
A total of 119 participants who had recovered from COVID-19 were included. Among them, musculoskeletal symptoms were the most prevalent, affecting 77 individuals (65%), followed by cardiopulmonary symptoms in 24 participants (20%), neurological symptoms in 12 (10%), and psychiatric symptoms in 6 (5%). The prevalence of musculoskeletal symptoms was significantly higher than that of other categories (p<0.001).
Within the musculoskeletal category, muscle pain was the most commonly reported symptom, experienced by 54 participants (70% of the musculoskeletal group, 45% of the total sample). Joint pain was reported by 39 individuals (50%, 33%), followed by fatigue in 23 (30%, 19%) and muscle weakness in 15 participants (20%, 13%). A substantial proportion of those with fatigue (60%) and muscle weakness (53%) reported symptom persistence beyond 12 months.
Cardiopulmonary symptoms were noted in 24 participants, predominantly shortness of breath (10 participants, 42%) and chest pain (6 participants, 25%), followed by reduced work capacity (5 participants, 21%) and fast or irregular heartbeat (3 participants, 13%). Most of these symptoms showed gradual improvement, with the majority resolving within 6 to 12 months after recovery.
Among the 12 participants who experienced neurological symptoms, cognitive impairments were the most frequent (5 participants, 42%), followed by paraesthesia in 3 (25%), and insomnia and dizziness in 2 participants each (17%). Chi-square analysis revealed that neurological symptoms were more likely to persist for longer durations compared to cardiopulmonary symptoms (p=0.03), particularly cognitive impairments, which often lasted beyond one year.
Psychiatric symptoms were the least reported, affecting only six participants (5% of the total sample). Of these, depression was noted in 3 individuals (50%), anxiety in 2 (33%), and social isolation in 1 (17%). While the prevalence was low, these symptoms underscore the psychological burden that may accompany physical recovery in some COVID-19 survivors. A few participants also reported miscellaneous symptoms that did not fit into the predefined categories but were mild and transient.
The mean duration scores among the four symptom domains indicated a statistically significant difference (p=0.01), with musculoskeletal symptoms demonstrating the highest mean persistence score, followed by neurological, cardiopulmonary, and psychiatric domains (Table 1).
Table 1. Mean symptom duration among COVID-19 survivors (n=119)
Discussion
This study aimed to investigate the prevalence and persistence of musculoskeletal, cardiopulmonary, neurological, and psychiatric symptoms among COVID-19 survivors. It underscores the significant burden of persistent physical, neurological, and psychological symptoms among individuals recovering from COVID-19, highlighting the multifaceted nature of post-COVID sequelae. Musculoskeletal symptoms, particularly muscle pain, joint pain, and fatigue, were the most frequently reported, affecting nearly half of the participants. This observation is in line with previous research, suggesting that skeletal muscle involvement and prolonged fatigue are among the most disabling consequences of COVID-19 recovery [7, 15, 19]. These manifestations may stem from inflammatory myopathy, mitochondrial dysfunction, and prolonged inactivity during hospitalization or quarantine periods [20, 21]. Furthermore, the persistence of muscle weakness beyond one year in a considerable proportion of participants emphasizes the chronic impact of the virus on functional capacity and overall quality of life.
Cardiopulmonary complaints, although less prevalent than musculoskeletal symptoms, remain clinically relevant. Shortness of breath was the most frequently reported symptom within this domain, often resolving within 6 to 12 months. This finding mirrors trends reported in previous longitudinal studies, which attribute gradual recovery to improved pulmonary rehabilitation strategies and early physiotherapeutic interventions that target respiratory endurance, thoracic mobility, and aerobic reconditioning [21]. The relatively shorter duration of these symptoms in our cohort may reflect the benefits of structured follow-up care and increased awareness of respiratory rehabilitation among post-COVID individuals.
Neurological symptoms, particularly cognitive dysfunction often referred to as “brain fog,” were another important finding. These issues have been hypothesized to result from neuroinflammatory processes, microvascular injury, and direct viral invasion of neural tissues [5, 17-22]. While less common than physical symptoms, their prolonged persistence suggests potential long-term neurocognitive consequences that warrant ongoing monitoring and interdisciplinary rehabilitation approaches. Cognitive training, graded activity programs, and neuromotor exercises may play a vital role in mitigating these effects and restoring functional independence.
Psychiatric symptoms, such as depression, anxiety, and social withdrawal were less frequently reported in our sample but should not be underestimated. The psychological aftermath of COVID-19, influenced by isolation, uncertainty, and physical debilitation, aligns with evidence from recent meta-analyses indicating an increased prevalence of post-traumatic stress and mood disturbances among survivors [6, 23, 24]. These findings reinforce the importance of integrating mental health screening and counseling into post-COVID rehabilitation pathways to promote holistic recovery.
The predominance of long-lasting musculoskeletal impairments highlights an urgent need for structured, evidence-based rehabilitation strategies tailored to post-COVID patients. Physiotherapy-led interventions—such as progressive resistance training, balance and coordination exercises, and digital tele-rehabilitation—have shown substantial efficacy in improving mobility, muscle strength, and activities of daily living [25]. Early initiation of these programs, along with patient education on pacing and graded activity, could prevent deconditioning and enhance recovery outcomes.
Overall, the study contributes to the growing body of evidence emphasizing the long-term functional impact of COVID-19 and the indispensable role of physiotherapists in managing post-COVID syndromes. Future research should focus on longitudinal outcomes, explore gender and age-related differences, and evaluate the effectiveness of specific rehabilitation protocols across diverse patient populations. Addressing these long-lasting issues requires dedicated rehabilitation strategies to improve quality of life and enhance function. Although less frequent, cardiopulmonary, neurological, and psychiatric symptoms continue to affect many individuals, highlighting the need for inclusive post-COVID management plans.
Conclusion
Musculoskeletal symptoms, namely muscle and joint pain, fatigue, and muscle weakness, remain common and often persist for more than a year among COVID-19 survivors.
Acknowledgments: The authors would like to acknowledge all the participants who voluntarily took part in this study. We also extend our sincere thanks to the institutional authorities for their support and cooperation during the conduct of this research.
Ethical Permissions: Ethical approval was obtained from the Institutional Ethics Committee prior to the commencement of the study.
Conflicts of Interests: The authors declared no conflicts of interests.
Authors' Contribution: NagaRaju D (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (20%); Subramanian S (Second Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (15%); Koganti VB (Third Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer (15%); Shekhar SPC (Fourth Author), Methodologist/Assistant Researcher/Discussion Writer (10%); Himabindu K (Fifth Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer (10%); Alagesan J (Sixth Author), Methodologist/Assistant Researcher/Statistical Analyst (10%); Indrani D (Seventh Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer (10%); Vishnuram S (Eighth Author), Methodologist/Assistant Researcher/Statistical Analyst (10%)
Funding/Support: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Keywords:
References
1. Pollard CA, Morran MP, Nestor-Kalinoski AL. The COVID-19 pandemic: A global health crisis. Physiol Genomics. 2020;52(11):549-57. [Link] [DOI:10.1152/physiolgenomics.00089.2020]
2. Gorman EA, O'Kane CM, McAuley DF. Acute respiratory distress syndrome in adults: Diagnosis, outcomes, long-term sequelae, and management. Lancet. 2022;400(10358):1157-70. [Link] [DOI:10.1016/S0140-6736(22)01439-8]
3. Parums DV. Long COVID or post-acute sequelae of SARS-CoV-2 infection (PASC) and the urgent need to identify diagnostic biomarkers and risk factors. Med Sci Monit. 2024;30:e946512. [Link] [DOI:10.12659/MSM.946512]
4. Conti V, Corbi G, Sabbatino F, De Pascale D, Sellitto C, Stefanelli B, et al. Long COVID: Clinical framing, biomarkers, and therapeutic approaches. J Pers Med. 2023;13(2):334. [Link] [DOI:10.3390/jpm13020334]
5. Ozanic K, Watanabe AS, Machado AB, Da Silva VL, Dias VC, Diniz CG. Long COVID: General perceptions and challenges in diagnosis and management. COVID. 2025;5(3):41. [Link] [DOI:10.3390/covid5030041]
6. Swarnakar R, Jenifa S, Wadhwa S. Musculoskeletal complications in long COVID-19: A systematic review. World J Virol. 2022;11(6):485-95. [Link] [DOI:10.5501/wjv.v11.i6.485]
7. Filatov A, Sharma P, Hindi F, Espinosa PS. Neurological complications of coronavirus disease (COVID-19): Encephalopathy. Cureus. 2020;12(3):e7352. [Link] [DOI:10.7759/cureus.7352]
8. Tedjasukmana R, Budikayanti A, Islamiyah WR, Witjaksono AMAL, Hakim M. Sleep disturbance in post COVID-19 conditions: Prevalence and quality of life. Front Neurol. 2023;13:1095606. [Link] [DOI:10.3389/fneur.2022.1095606]
9. SeyedAlinaghi S, Afsahi AM, MohsseniPour M, Behnezhad F, Salehi MA, Barzegary A, et al. Late complications of COVID-19; A systematic review of current evidence. Arch Acad Emerg Med. 2021;9(1):e14. [Link] [DOI:10.5501/wjv.v9.i5.79]
10. Pergolizzi JV, Raffa RB, Varrassi G, Magnusson P, LeQuang JA, Paladini A, et al. Potential neurological manifestations of COVID-19: A narrative review. Postgrad Med. 2022;134(4):395-405. [Link] [DOI:10.1080/00325481.2020.1837503]
11. Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020;77(6):683-90. [Link] [DOI:10.1001/jamaneurol.2020.1127]
12. Singh SJ, Baldwin MM, Daynes E, Evans RA, Greening NJ, Jenkins RG, et al. Respiratory sequelae of COVID-19: Pulmonary and extrapulmonary origins, and approaches to clinical care and rehabilitation. Lancet Respir Med. 2023;11(8):709-25. [Link] [DOI:10.1016/S2213-2600(23)00159-5]
13. Dos Santos PK, Sigoli E, Bragança LJG, Cornachione AS. The musculoskeletal involvement after mild to moderate COVID-19 infection. Front Physiol. 2022;13:813924. [Link] [DOI:10.3389/fphys.2022.813924]
14. Estebanez-Pérez MJ, Pastora-Bernal JM, Martín-Valero R. The effectiveness of a four-week digital physiotherapy intervention to improve functional capacity and adherence to intervention in patients with long COVID-19. Int J Environ Res Public Health. 2022;19(15):9566. [Link] [DOI:10.3390/ijerph19159566]
15. Dubba NR, Muthukumaran J, Dasarapu I. Effect of body weight exercises for COVID-19 survivors. INTI J. 2023;2023:42. [Link] [DOI:10.61453/INTIj.202342]
16. Tharani SA, Borkar P. Prevalence of musculoskeletal disorders in post-COVID-19 patients-a systematic review. Int J Health Sci Res. 2022;12(3):374-80. [Link] [DOI:10.52403/ijhsr.20220349]
17. Shanbehzadeh S, Tavahomi M, Zanjari N, Ebrahimi-Takamjani I, Amiri-Arimi S. Physical and mental health complications post-COVID-19: Scoping review. J Psychosom Res. 2021;147:110525. [Link] [DOI:10.1016/j.jpsychores.2021.110525]
18. Walia N, Lat JO, Tariq R, Tyagi S, Qazi AM, Salari SW, et al. Post-acute sequelae of COVID-19 and the mental health implications. Discoveries. 2021;9(4):e140. [Link] [DOI:10.15190/d.2021.19]
19. Sepehrinezhad A, Shahbazi A, Negah SS. COVID-19 virus may have neuroinvasive potential and cause neurological complications: A perspective review. J Neurovirol. 2020;26(3):324-9. [Link] [DOI:10.1007/s13365-020-00851-2]
20. Gentil P, De Lira CAB, Coswig V, Barroso WKS, Vitorino PVO, Ramirez-Campillo R, et al. Practical recommendations relevant to the use of resistance training for COVID-19 survivors. Front Physiol. 2021;12:637590. [Link] [DOI:10.3389/fphys.2021.637590]
21. Fernandez-De-Las-Peñas C, Notarte KI, Macasaet R, Velasco JV, Catahay JA, Ver AT, et al. Persistence of post-COVID symptoms in the general population two years after SARS-CoV-2 infection: A systematic review and meta-analysis. J Infect. 2024;88(2):77-88. [Link] [DOI:10.1016/j.jinf.2023.12.004]
22. Aiyegbusi OL, Hughes SE, Turner G, Rivera SC, McMullan C, Chandan JS, et al. Symptoms, complications and management of long COVID: A review. J R Soc Med. 2021;114(9):428-42. [Link] [DOI:10.1177/01410768211032850]
23. Engin AB, Engin ED, Engin A. Current opinion in neurological manifestations of SARS-CoV-2 infection. Curr Opin Toxicol. 2021;25:49-56. [Link] [DOI:10.1016/j.cotox.2021.03.004]
24. Ramani SL, Samet J, Franz CK, Hsieh C, Nguyen CV, Horbinski C, et al. Musculoskeletal involvement of COVID-19: Review of imaging. Skeletal Radiol. 2021;50(9):1763-73. [Link] [DOI:10.1007/s00256-021-03734-7]
25. Yang G, Li Z, Li Z, Huang L, Liang P, Liu L, et al. Meta-analysis of the impact of physical activity on the recovery of physical function in COVID-19 patients. Heliyon. 2023;9(9):e19339. [Link] [DOI:10.1016/j.heliyon.2023.e19339]









