Volume 16, Issue 4 (2024)
Iran J War Public Health 2024, 16(4): 341-346 |
Back to browse issues page
Article Type:
Subject:
Ethics code: 116/UN29.20.1/ETIK/2024
History
Received: 2024/10/27 | Accepted: 2024/11/29 | Published: 2024/12/5
Received: 2024/10/27 | Accepted: 2024/11/29 | Published: 2024/12/5
How to cite this article
Kusnan A, DP Sartiah, Majid R, Asriati A, Jumu L, Rahmawati R. Utilization of Voluntary Counselling and Testing Clinic in Elderly Male HIV/AIDS Patients. Iran J War Public Health 2024; 16 (4) :341-346
URL: http://ijwph.ir/article-1-1538-en.html
URL: http://ijwph.ir/article-1-1538-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
1- Department of Nursing, Faculty of Medical, Halu Oleo University, Kendari, Indonesia
2- Department of Public Health, Faculty of Public Health, Halu Oleo University, Kendari, Indonesia
3- Department of Medical Community, Faculty of Medical, Halu Oleo University, Kendari, Indonesia
4- Department of Nursing, Health Polytechnic of Ministry of Health Jayapura, Papua, Indonesia
2- Department of Public Health, Faculty of Public Health, Halu Oleo University, Kendari, Indonesia
3- Department of Medical Community, Faculty of Medical, Halu Oleo University, Kendari, Indonesia
4- Department of Nursing, Health Polytechnic of Ministry of Health Jayapura, Papua, Indonesia
Full-Text (HTML) (485 Views)
Introduction
Globalization has profoundly influenced Indonesian society, leading to a shift from traditional values to modern lifestyles often characterized by consumerism and high-risk behaviors [1, 2]. The surge in infectious diseases, particularly Human Immunodeficiency Virus (HIV) and Acquired Immune Deficiency Syndrome (AIDS), has emerged as a pressing global health issue. These illnesses have significantly affected Indonesia, with infection rates steadily climbing, including in rural regions. HIV compromises the immune system, increasing susceptibility to opportunistic infections, and is primarily spread through the exchange of infected bodily fluids such as blood, semen, and vaginal secretions [3-5].
The HIV epidemic continues to be a significant health issue globally. As of 2022, about 39 million people were living with HIV, with the African region experiencing the highest prevalence [6, 7]. In Southeast Asia, Indonesia stands out with one of the highest HIV rates among adults aged 15-49, at 0.5%, following Thailand and Myanmar. Despite ongoing efforts to curb the epidemic, the increasing number of new HIV/AIDS cases in Indonesia emphasizes the need for more effective interventions, especially for vulnerable groups like men who have sex with men (MSM) [8, 9].
MSM (Men who have sex with men) is a phenomenon that has existed for a long time and cannot be regarded as something new in society [10]. This group significantly contributes to the increasing proportion of HIV/AIDS cases worldwide, including in Indonesia. The causes of MSM behavior are highly complex and influenced by various factors, such as sexual orientation, social pressures, past trauma, social environments, and exposure to evolving cultural norms and values. Biological and psychosocial factors can also significantly shape a person's preferences or behaviors [11, 12].
According to the Indonesian Ministry of Health, cumulative HIV/AIDS cases in the country will surpass 540,000 by 2022, with an upward trend in annual incidence [10]. In Southeast Sulawesi Province, the number of HIV/AIDS cases has risen significantly, with Kendari City reporting the highest proportion of cases. In the last five years, Kendari City has seen a consistent rise in new HIV cases among men who have sex with men, with 173 reported cases in 2023 [13]. Factors such as stigma, discrimination, and limited access to healthcare services continue to drive the high transmission rates within this population [14].
Voluntary Counseling and Testing (VCT) services represent a strategic approach to addressing HIV/AIDS, offering individuals, particularly at-risk populations, the opportunity to voluntarily determine their HIV status [15-17]. These services encompass pre- and post-test counseling as well as treatment for individuals diagnosed with HIV. VCT seeks to promote awareness, foster preventive actions, and minimize the likelihood of HIV transmission, especially within high-risk groups such as men who have sex with men (MSM) [18-20].
Despite its potential, several barriers hinder the utilization of VCT services, including limited knowledge, stigma, fear of test results, and restricted access. At Kendari City General Hospital (RSUD Kendari), the treatment adherence rate among patients reached 95.6%. However, the proportion of MSM accessing VCT services remains a point for improvement. Preliminary observations indicate that 428 MSM visited the VCT Clinic at RSUD Kendari in 2023, reflecting a significant increase in recent years. The present study intends to explore the factors that affect the use of Voluntary Counseling and Testing (VCT) services by HIV-positive men who have sex with men (MSM) at Kendari City Hospital. The results are expected to contribute to shaping health policies and strategies aimed at preventing HIV/AIDS transmission, both locally and nationally.
Instrument and Methods
Design & Samples
This study adopted an observational analytic design with a cross-sectional approach, a method used in research to collect data at a particular moment rather than over a period of time [21]. The research focused on men who have sex with men (MSM) living with HIV/AIDS who had visited the VCT Clinic at Kendari City Hospital by March 2024, with a total population of 428 individuals. Using the Slovin formula, a sample of 82 participants was selected with a 90% confidence level (α=0.1) through simple random sampling. Eligibility criteria included being at least 45 years old, having a confirmed or temporary HIV/AIDS diagnosis, being fluent in Indonesian, and having visited the VCT Clinic within the specified timeframe. Respondents with critical or unstable health conditions that prevented them from participating in interviews were excluded from the study.
Instrument
The research utilized validated structured questionnaires, including Guttman scales to assess knowledge, family support, peer support, and Likert scales for measuring attitude and action. The utilization of the VCT Clinic was determined based on the number of visits in the past year, with visits categorized as "good" if they occurred six times or more and "less" if fewer than six were made. Data for the study were gathered through interviews conducted with structured questionnaires, while secondary data were obtained from the records at Kendari City Hospital and pertinent literature. The research instrument was tested for validity through correlation analysis between individual question items and the total variable score. All items had correlation values greater than 0.3, confirming their validity. To assess reliability, Cronbach’s Alpha was applied, resulting in a coefficient of 0.87, above the acceptable minimum of 0.7, demonstrating that the instrument has high internal consistency.
Procedure
The first step involved obtaining informed consent from the respondents. Before beginning data collection, the researcher provided an overview of the study's objectives, explained the steps involved, and informed participants about their rights, including confidentiality of their responses and the option to join or withdraw from the study at any point without any repercussions. Following the acquisition of written consent, data collection commenced with structured interviews. These interviews were conducted using a validated questionnaire and covered key research variables, including knowledge, attitude, family support, peer support, and utilization of the VCT Clinic. The researcher personally conducted the interviews, ensuring respondents fully understood the questions and their responses were accurately recorded. Additionally, secondary data were collected from Kendari City Hospital’s documentation, which provided information on the number of visits made by HIV/AIDS patients to the VCT Clinic over the past year. This data was used to categorize service utilization as “good” or “less”.
Three trained enumerators supported the researchers in facilitating the data collection process. These enumerators played a crucial role in conducting direct interviews with respondents, recording their answers, and completing questionnaires according to established procedures. With the enumerators' assistance, the researchers ensured that the data collection process was conducted effectively, resulting in more accurate and representative data.
Data analysis
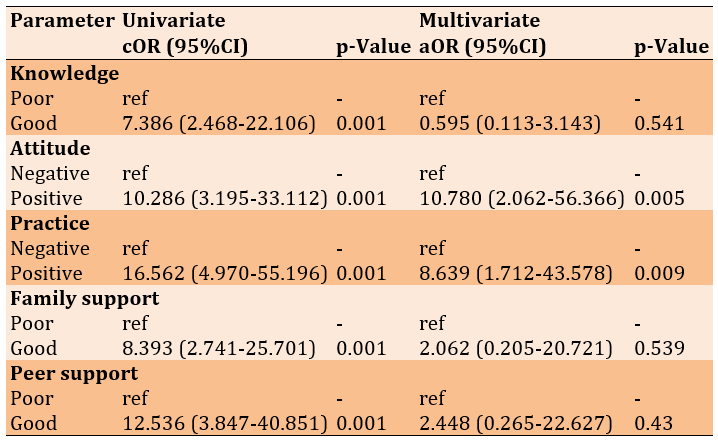
For data analysis, the researcher followed a stepwise approach. The analysis began with univariate analysis to describe the frequency distribution of each variable. Next, a bivariate analysis was conducted using the Chi-Square test to explore the associations between independent variables (such as knowledge, family support, peer support, and attitude) and the dependent variable (use of the VCT Clinic). A multivariate analysis with logistic regression was performed to identify significant factors impacting VCT Clinic utilization. The findings are reported as Adjusted Odds Ratios (aOR) with 95% Confidence Intervals (CI), reflecting the probability of independent variables affecting the dependent variable after accounting for other factors. Additionally, a Crude Odds Ratio (cOR) was calculated in the initial phase to examine the unadjusted relationships between the variables.
Findings
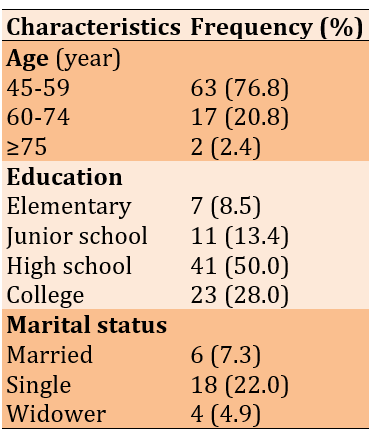
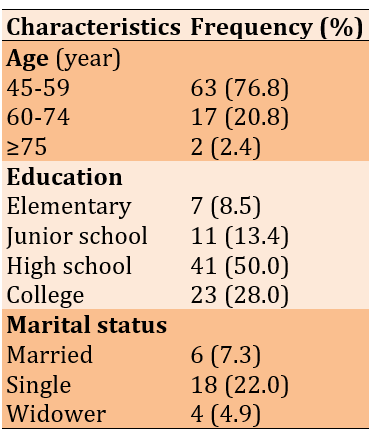
Most participants (76.8%) fell within the 45-59 age group, had completed high school (50.0%), and were single (22.0%; Table 1).
Table 1. Distribution of respondent characteristics by frequency
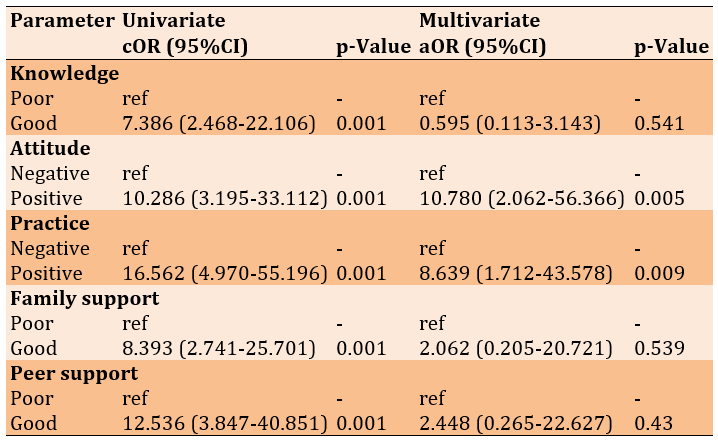
Sufficient knowledge was associated with 7.386 times higher odds of utilizing the VCT Clinic than insufficient knowledge (p=0.001). A positive attitude was identified as a significant factor in the univariate (p=0.001) and multivariate analyses (p=0.005). Engaging in positive actions also had a significant impact, with odds 16.562 times higher in the univariate analysis (p=0.001), and it remained significant in the multivariate analysis (p=0.009). Adequate family support significantly correlated with VCT Clinic utilization in the univariate analysis (p=0.001). Sufficient peer support had a notable effect on the univariate analysis (p=0.001; Table 2).
Table 2. Binary logistic regression analysis of VCT Clinic utilization
Discussion
The findings of this study show that a significant proportion of male sex workers (MSM) in Kendari City, specifically 74.4%, make optimal use of Voluntary Counseling and Testing (VCT) services. This strong utilization rate may reflect the success of HIV/AIDS education and prevention programs, although challenges remain in ensuring equal access across all key populations. Knowledge about HIV/AIDS and VCT services is a crucial first step in promoting positive health behaviors. Individuals with a good understanding of HIV risks, the benefits of VCT, and the safe process of counseling and testing are more likely to feel confident in utilizing these services. Knowledge helps reduce fear or anxiety often caused by a lack of accurate information while also dispelling myths and stigma associated with HIV. By increasing knowledge, individuals are more encouraged to be aware of their health status and take the necessary preventive measures [22-24].
While knowledge demonstrated a meaningful relationship in the preliminary analysis, it did not emerge as a significant factor in the multivariate analysis. This suggests that sufficient knowledge does not necessarily lead to behavior change, particularly in contexts with social stigma. To address this, a more contextualized educational approach is needed to provide information and emphasize how that knowledge can be applied in practical actions [25, 26].
A positive attitude emerged as a key factor in increasing the use of VCT services. A positive attitude toward the importance of knowing one's HIV status, the belief in the benefits of VCT services, and trust in healthcare providers can encourage individuals to utilize these services voluntarily. The multivariate analysis revealed that respondents with a positive attitude were 10.78 times more likely to use the service than those with a negative attitude. This result supports earlier research highlighting the critical role of cultivating positive views toward health services in encouraging proactive health behaviors [27, 28]. Consequently, campaigns that emphasize the benefits of VCT and address stigma within the community are essential [28].
Positive action was another significant factor influencing VCT utilization. Respondents who took proactive steps to maintain their health were 8.63 times more likely to use the service. This highlights the crucial role of individual awareness and the willingness to take concrete actions, such as regular visits to VCT clinics, in preventing and controlling the spread of HIV/AIDS. Reinforcing positive behaviors should be a priority in public health programs [29].
Peer support plays an important role in encouraging individuals to access VCT services. Peers can provide moral encouragement, share positive experiences related to VCT, and serve as trusted sources of information. In the MSM community, peer support can also help overcome fear and anxiety caused by the stigma attached to HIV [30]. Family support also contributes to increased utilization of VCT services. Supportive families tend to provide emotional encouragement, help reduce fear of diagnosis, and motivate individuals to get tested. Family support can create a safe and comfortable environment for individuals, ultimately increasing their willingness to use VCT services [28, 31]. However, this effect became insignificant in the multivariate analysis. This may be due to the influence of other more dominant variables, such as individual attitudes and actions. Nevertheless, social support remains an essential factor in helping individuals navigate the stigma and discrimination often faced by MSM. Community-based programs that strengthen the role of family and peers in providing moral and emotional support could be beneficial [32].
Several other factors may influence an individual's decision not to visit VCT services regularly despite having adequate knowledge. Although they understand the importance of an HIV test to know their health status, fear of a positive test result remains a major barrier. A positive result can trigger anxiety about their future, including social, psychological, and medical consequences. The fear of these consequences, such as concerns about long-term treatment or its impact on social and work life, can prevent them from returning to VCT services, even though they are aware of the importance of the test. Additionally, individuals may have good knowledge, but without sustained social support from family, peers, or the community, they may feel less motivated to visit VCT services regularly [33, 34].
In the local context, this study offers valuable insights into the unique challenges MSM faces in Kendari City. Stigma, limited access to services, and fear of diagnosis are significant barriers that must be addressed through a multisectoral approach. To increase their effectiveness, efforts to improve VCT programs should focus on engaging key stakeholders, including government bodies, NGOs, and local communities.
Conclusion
The use of Voluntary Counseling and Testing services by male workers living with HIV/AIDS in Kendari City is largely driven by their positive attitudes and behaviors, while social support and knowledge act as contributing factors. While most respondents utilized the service effectively, barriers such as stigma, fear of diagnosis, and limited access continue to impact certain groups.
Acknowledgments: The author expresses heartfelt thanks to the Dean of the Faculty of Medicine at the University of Halu Oleo (UHO) for their continuous support, mentorship, and provision of resources throughout the research. This support played a crucial role in the study's success. Additionally, the author is deeply grateful to the Head of the Research and Community Service Institute at Halu Oleo University for their insightful guidance and assistance during the research process.
Ethical Permissions: The Research Ethics Committee of the Faculty of Medicine at Halu Oleo University granted ethical approval for this study under approval number 116/UN29.20.1/ETIK/2024. Before the study commenced, all procedures were thoroughly evaluated and approved, adhering to the ethical standards for health research outlined in the Declaration of Helsinki.
Conflicts of Interests: The authors reported no conflict of interest.
Authors' Contribution: Kusnan A (First Author), Introduction Writer/Methodologist/Original or Assistant Researcher/Discussion Writer/Statistical Analyst (35%); DP S (Second Author), Introduction Writer/Methodologist/Original or Assistant Researcher/Discussion Writer/Statistical Analyst (10%); Majid R (Third Author), Introduction Writer/Methodologist/Original or Assistant Researcher/Discussion Writer/Statistical Analyst (10%); Asriati A (Fourth Author), Introduction Writer/Methodologist/Original or Assistant Researcher/Discussion Writer/Statistical Analyst (10%); Jumu L (Fifth Author), Introduction Writer/Methodologist/Original or Assistant Researcher/Discussion Writer/Statistical Analyst (10%); Rachmawati R (Sixth Author), Introduction Writer/Methodologist/Original or Assistant Researcher/Discussion Writer/Statistical Analyst (25%)
Funding/Support: This research was not funded; no financial support was received from any government, private, or non-profit organizations.
Globalization has profoundly influenced Indonesian society, leading to a shift from traditional values to modern lifestyles often characterized by consumerism and high-risk behaviors [1, 2]. The surge in infectious diseases, particularly Human Immunodeficiency Virus (HIV) and Acquired Immune Deficiency Syndrome (AIDS), has emerged as a pressing global health issue. These illnesses have significantly affected Indonesia, with infection rates steadily climbing, including in rural regions. HIV compromises the immune system, increasing susceptibility to opportunistic infections, and is primarily spread through the exchange of infected bodily fluids such as blood, semen, and vaginal secretions [3-5].
The HIV epidemic continues to be a significant health issue globally. As of 2022, about 39 million people were living with HIV, with the African region experiencing the highest prevalence [6, 7]. In Southeast Asia, Indonesia stands out with one of the highest HIV rates among adults aged 15-49, at 0.5%, following Thailand and Myanmar. Despite ongoing efforts to curb the epidemic, the increasing number of new HIV/AIDS cases in Indonesia emphasizes the need for more effective interventions, especially for vulnerable groups like men who have sex with men (MSM) [8, 9].
MSM (Men who have sex with men) is a phenomenon that has existed for a long time and cannot be regarded as something new in society [10]. This group significantly contributes to the increasing proportion of HIV/AIDS cases worldwide, including in Indonesia. The causes of MSM behavior are highly complex and influenced by various factors, such as sexual orientation, social pressures, past trauma, social environments, and exposure to evolving cultural norms and values. Biological and psychosocial factors can also significantly shape a person's preferences or behaviors [11, 12].
According to the Indonesian Ministry of Health, cumulative HIV/AIDS cases in the country will surpass 540,000 by 2022, with an upward trend in annual incidence [10]. In Southeast Sulawesi Province, the number of HIV/AIDS cases has risen significantly, with Kendari City reporting the highest proportion of cases. In the last five years, Kendari City has seen a consistent rise in new HIV cases among men who have sex with men, with 173 reported cases in 2023 [13]. Factors such as stigma, discrimination, and limited access to healthcare services continue to drive the high transmission rates within this population [14].
Voluntary Counseling and Testing (VCT) services represent a strategic approach to addressing HIV/AIDS, offering individuals, particularly at-risk populations, the opportunity to voluntarily determine their HIV status [15-17]. These services encompass pre- and post-test counseling as well as treatment for individuals diagnosed with HIV. VCT seeks to promote awareness, foster preventive actions, and minimize the likelihood of HIV transmission, especially within high-risk groups such as men who have sex with men (MSM) [18-20].
Despite its potential, several barriers hinder the utilization of VCT services, including limited knowledge, stigma, fear of test results, and restricted access. At Kendari City General Hospital (RSUD Kendari), the treatment adherence rate among patients reached 95.6%. However, the proportion of MSM accessing VCT services remains a point for improvement. Preliminary observations indicate that 428 MSM visited the VCT Clinic at RSUD Kendari in 2023, reflecting a significant increase in recent years. The present study intends to explore the factors that affect the use of Voluntary Counseling and Testing (VCT) services by HIV-positive men who have sex with men (MSM) at Kendari City Hospital. The results are expected to contribute to shaping health policies and strategies aimed at preventing HIV/AIDS transmission, both locally and nationally.
Instrument and Methods
Design & Samples
This study adopted an observational analytic design with a cross-sectional approach, a method used in research to collect data at a particular moment rather than over a period of time [21]. The research focused on men who have sex with men (MSM) living with HIV/AIDS who had visited the VCT Clinic at Kendari City Hospital by March 2024, with a total population of 428 individuals. Using the Slovin formula, a sample of 82 participants was selected with a 90% confidence level (α=0.1) through simple random sampling. Eligibility criteria included being at least 45 years old, having a confirmed or temporary HIV/AIDS diagnosis, being fluent in Indonesian, and having visited the VCT Clinic within the specified timeframe. Respondents with critical or unstable health conditions that prevented them from participating in interviews were excluded from the study.
Instrument
The research utilized validated structured questionnaires, including Guttman scales to assess knowledge, family support, peer support, and Likert scales for measuring attitude and action. The utilization of the VCT Clinic was determined based on the number of visits in the past year, with visits categorized as "good" if they occurred six times or more and "less" if fewer than six were made. Data for the study were gathered through interviews conducted with structured questionnaires, while secondary data were obtained from the records at Kendari City Hospital and pertinent literature. The research instrument was tested for validity through correlation analysis between individual question items and the total variable score. All items had correlation values greater than 0.3, confirming their validity. To assess reliability, Cronbach’s Alpha was applied, resulting in a coefficient of 0.87, above the acceptable minimum of 0.7, demonstrating that the instrument has high internal consistency.
Procedure
The first step involved obtaining informed consent from the respondents. Before beginning data collection, the researcher provided an overview of the study's objectives, explained the steps involved, and informed participants about their rights, including confidentiality of their responses and the option to join or withdraw from the study at any point without any repercussions. Following the acquisition of written consent, data collection commenced with structured interviews. These interviews were conducted using a validated questionnaire and covered key research variables, including knowledge, attitude, family support, peer support, and utilization of the VCT Clinic. The researcher personally conducted the interviews, ensuring respondents fully understood the questions and their responses were accurately recorded. Additionally, secondary data were collected from Kendari City Hospital’s documentation, which provided information on the number of visits made by HIV/AIDS patients to the VCT Clinic over the past year. This data was used to categorize service utilization as “good” or “less”.
Three trained enumerators supported the researchers in facilitating the data collection process. These enumerators played a crucial role in conducting direct interviews with respondents, recording their answers, and completing questionnaires according to established procedures. With the enumerators' assistance, the researchers ensured that the data collection process was conducted effectively, resulting in more accurate and representative data.
Data analysis
For data analysis, the researcher followed a stepwise approach. The analysis began with univariate analysis to describe the frequency distribution of each variable. Next, a bivariate analysis was conducted using the Chi-Square test to explore the associations between independent variables (such as knowledge, family support, peer support, and attitude) and the dependent variable (use of the VCT Clinic). A multivariate analysis with logistic regression was performed to identify significant factors impacting VCT Clinic utilization. The findings are reported as Adjusted Odds Ratios (aOR) with 95% Confidence Intervals (CI), reflecting the probability of independent variables affecting the dependent variable after accounting for other factors. Additionally, a Crude Odds Ratio (cOR) was calculated in the initial phase to examine the unadjusted relationships between the variables.
Findings
Most participants (76.8%) fell within the 45-59 age group, had completed high school (50.0%), and were single (22.0%; Table 1).
Table 1. Distribution of respondent characteristics by frequency
Sufficient knowledge was associated with 7.386 times higher odds of utilizing the VCT Clinic than insufficient knowledge (p=0.001). A positive attitude was identified as a significant factor in the univariate (p=0.001) and multivariate analyses (p=0.005). Engaging in positive actions also had a significant impact, with odds 16.562 times higher in the univariate analysis (p=0.001), and it remained significant in the multivariate analysis (p=0.009). Adequate family support significantly correlated with VCT Clinic utilization in the univariate analysis (p=0.001). Sufficient peer support had a notable effect on the univariate analysis (p=0.001; Table 2).
Table 2. Binary logistic regression analysis of VCT Clinic utilization
Discussion
The findings of this study show that a significant proportion of male sex workers (MSM) in Kendari City, specifically 74.4%, make optimal use of Voluntary Counseling and Testing (VCT) services. This strong utilization rate may reflect the success of HIV/AIDS education and prevention programs, although challenges remain in ensuring equal access across all key populations. Knowledge about HIV/AIDS and VCT services is a crucial first step in promoting positive health behaviors. Individuals with a good understanding of HIV risks, the benefits of VCT, and the safe process of counseling and testing are more likely to feel confident in utilizing these services. Knowledge helps reduce fear or anxiety often caused by a lack of accurate information while also dispelling myths and stigma associated with HIV. By increasing knowledge, individuals are more encouraged to be aware of their health status and take the necessary preventive measures [22-24].
While knowledge demonstrated a meaningful relationship in the preliminary analysis, it did not emerge as a significant factor in the multivariate analysis. This suggests that sufficient knowledge does not necessarily lead to behavior change, particularly in contexts with social stigma. To address this, a more contextualized educational approach is needed to provide information and emphasize how that knowledge can be applied in practical actions [25, 26].
A positive attitude emerged as a key factor in increasing the use of VCT services. A positive attitude toward the importance of knowing one's HIV status, the belief in the benefits of VCT services, and trust in healthcare providers can encourage individuals to utilize these services voluntarily. The multivariate analysis revealed that respondents with a positive attitude were 10.78 times more likely to use the service than those with a negative attitude. This result supports earlier research highlighting the critical role of cultivating positive views toward health services in encouraging proactive health behaviors [27, 28]. Consequently, campaigns that emphasize the benefits of VCT and address stigma within the community are essential [28].
Positive action was another significant factor influencing VCT utilization. Respondents who took proactive steps to maintain their health were 8.63 times more likely to use the service. This highlights the crucial role of individual awareness and the willingness to take concrete actions, such as regular visits to VCT clinics, in preventing and controlling the spread of HIV/AIDS. Reinforcing positive behaviors should be a priority in public health programs [29].
Peer support plays an important role in encouraging individuals to access VCT services. Peers can provide moral encouragement, share positive experiences related to VCT, and serve as trusted sources of information. In the MSM community, peer support can also help overcome fear and anxiety caused by the stigma attached to HIV [30]. Family support also contributes to increased utilization of VCT services. Supportive families tend to provide emotional encouragement, help reduce fear of diagnosis, and motivate individuals to get tested. Family support can create a safe and comfortable environment for individuals, ultimately increasing their willingness to use VCT services [28, 31]. However, this effect became insignificant in the multivariate analysis. This may be due to the influence of other more dominant variables, such as individual attitudes and actions. Nevertheless, social support remains an essential factor in helping individuals navigate the stigma and discrimination often faced by MSM. Community-based programs that strengthen the role of family and peers in providing moral and emotional support could be beneficial [32].
Several other factors may influence an individual's decision not to visit VCT services regularly despite having adequate knowledge. Although they understand the importance of an HIV test to know their health status, fear of a positive test result remains a major barrier. A positive result can trigger anxiety about their future, including social, psychological, and medical consequences. The fear of these consequences, such as concerns about long-term treatment or its impact on social and work life, can prevent them from returning to VCT services, even though they are aware of the importance of the test. Additionally, individuals may have good knowledge, but without sustained social support from family, peers, or the community, they may feel less motivated to visit VCT services regularly [33, 34].
In the local context, this study offers valuable insights into the unique challenges MSM faces in Kendari City. Stigma, limited access to services, and fear of diagnosis are significant barriers that must be addressed through a multisectoral approach. To increase their effectiveness, efforts to improve VCT programs should focus on engaging key stakeholders, including government bodies, NGOs, and local communities.
Conclusion
The use of Voluntary Counseling and Testing services by male workers living with HIV/AIDS in Kendari City is largely driven by their positive attitudes and behaviors, while social support and knowledge act as contributing factors. While most respondents utilized the service effectively, barriers such as stigma, fear of diagnosis, and limited access continue to impact certain groups.
Acknowledgments: The author expresses heartfelt thanks to the Dean of the Faculty of Medicine at the University of Halu Oleo (UHO) for their continuous support, mentorship, and provision of resources throughout the research. This support played a crucial role in the study's success. Additionally, the author is deeply grateful to the Head of the Research and Community Service Institute at Halu Oleo University for their insightful guidance and assistance during the research process.
Ethical Permissions: The Research Ethics Committee of the Faculty of Medicine at Halu Oleo University granted ethical approval for this study under approval number 116/UN29.20.1/ETIK/2024. Before the study commenced, all procedures were thoroughly evaluated and approved, adhering to the ethical standards for health research outlined in the Declaration of Helsinki.
Conflicts of Interests: The authors reported no conflict of interest.
Authors' Contribution: Kusnan A (First Author), Introduction Writer/Methodologist/Original or Assistant Researcher/Discussion Writer/Statistical Analyst (35%); DP S (Second Author), Introduction Writer/Methodologist/Original or Assistant Researcher/Discussion Writer/Statistical Analyst (10%); Majid R (Third Author), Introduction Writer/Methodologist/Original or Assistant Researcher/Discussion Writer/Statistical Analyst (10%); Asriati A (Fourth Author), Introduction Writer/Methodologist/Original or Assistant Researcher/Discussion Writer/Statistical Analyst (10%); Jumu L (Fifth Author), Introduction Writer/Methodologist/Original or Assistant Researcher/Discussion Writer/Statistical Analyst (10%); Rachmawati R (Sixth Author), Introduction Writer/Methodologist/Original or Assistant Researcher/Discussion Writer/Statistical Analyst (25%)
Funding/Support: This research was not funded; no financial support was received from any government, private, or non-profit organizations.
Keywords:
References
1. Sadarang RAI. Prevalence and factors affecting discrimination towards people living with HIV/AIDS in Indonesia. J Prev Med Public Health. 2022;55(2):205-12. [Link] [DOI:10.3961/jpmph.21.502]
2. Riono P, Jazant S. The current situation of the HIV/AIDS epidemic in Indonesia. AIDS Educ Prev. 2004;16(3 Suppl A):78-90. [Link] [DOI:10.1521/aeap.16.3.5.78.35531]
3. Ali A, Osman E. Factors influencing HIV voluntary counseling and testing (Vct) among pregnant women in Kassala, Eastern Sudan. J Womens Health Care. 2014;3(6):198. [Link]
4. Wardhani BDK, Grulich AE, Kawi NH, Prasetia Y, Luis H, Wirawan GBS, et al. Very high HIV prevalence and incidence among men who have sex with men and transgender women in Indonesia: A retrospective observational cohort study in Bali and Jakarta, 2017-2020. J Int AIDS Soc. 2024;27(11):e26386. [Link] [DOI:10.1002/jia2.26386]
5. Sherr L, Lopman B, Kakowa M, Dube S, Chawira G, Nyamukapa C, et al. Voluntary counselling and testing: Uptake, impact on sexual behaviour, and HIV incidence in a rural Zimbabwean cohort. AIDS. 2007;21(7):851-60. [Link] [DOI:10.1097/QAD.0b013e32805e8711]
6. Challacombe SJ. Global inequalities in HIV infection. Oral Dis. 2020;26 Suppl 1:16-21. [Link] [DOI:10.1111/odi.13386]
7. Govender RD, Hashim MJ, Khan MAB, Mustafa H, Khan G. Global epidemiology of HIV/AIDS: A resurgence in North America and Europe. J Epidemiol Glob Health. 2021;11(3):296-301. [Link] [DOI:10.2991/jegh.k.210621.001]
8. Kirichenko A, Kireev D, Lopatukhin A, Murzakova A, Lapovok I, Saleeva D, et al. Prevalence of HIV-1 drug resistance in Eastern European and Central Asian countries. PLoS One. 2022;17(1):e0257731. [Link] [DOI:10.1371/journal.pone.0257731]
9. Nevendorff L, Schroeder SE, Pedrana A, Bourne A, Stoove M. Prevalence of sexualized drug use and risk of HIV among sexually active MSM in East and South Asian countries: Systematic review and meta‐analysis. J Int AIDS Soc. 2023;26(1):e26054. [Link] [DOI:10.1002/jia2.26054]
10. Van De Laar TJW, Van Der Bij AK, Prins M, Bruisten SM, Brinkman K, Ruys TA, et al. Increase in HCV incidence among men who have sex with men in Amsterdam most likely caused by sexual transmission. J Infect Dis. 2007;196(2):230-8. [Link] [DOI:10.1086/518796]
11. Loue S. Defining men who have sex with men (MSM). In: Health issues confronting minority men who have sex with men. New York: Springer; 2008. p. 3-37. [Link] [DOI:10.1007/978-0-387-74539-8_1]
12. Beyrer C, Baral SD, Van Griensven F, Goodreau SM, Chariyalertsak S, Wirtz AL, et al. Global epidemiology of HIV infection in men who have sex with men. Lancet. 2012;380(9839):367-77. [Link] [DOI:10.1016/S0140-6736(12)60821-6]
13. Dinas Kesehatan Provinsi Sulawesi Tenggara. Health Profile of Southeast Sulawesi. Kendari: Dinas Kesehatan Provinsi Sulawesi Tenggara; 2021. [Indonesian] [Link]
14. Obeagu EI, Obeagu GU. Human immunodeficiency virus and tuberculosis infection: A review of prevalence of associated factors. Int J Adv Multidiscip Res. 2023;10(10):56-62. [Link]
15. Apanga PA, Akparibo R, Awoonor-Williams JK. Factors influencing uptake of voluntary counselling and testing services for HIV/AIDS in the Lower Manya Krobo Municipality (LMKM) in the Eastern Region of Ghana: A cross-sectional household survey. J Health Popul Nutr. 2015;33:23. [Link] [DOI:10.1186/s41043-015-0035-8]
16. Epule ET, Mirielle MW, Peng C, Nguh BS, Nyagero JM, Lakati A, et al. Utilization rates and perceptions of (VCT) services in Kisii central district, Kenya. Glob J Health Sci. 2012;5(1):35-43. [Link] [DOI:10.5539/gjhs.v5n1p35]
17. Ekanem EE, Gbadegesin A. Voluntary counselling and testing (VCT) for human immunodeficiency virus: A study on acceptability by Nigerian women attending antenatal clinics. Afr J Reprod Health. 2004;8(2):91-100. [Link] [DOI:10.2307/3583183]
18. Admassu M, Fitaw Y. Factors affecting acceptance of VCT among different professional and community groups in North and South Gondar Administrative zones, north west Ethiopia. Ethiop J Health Dev. 2006;20(1):24-31. [Link] [DOI:10.4314/ejhd.v20i1.10008]
19. Mwangi R, Ngure P, Thiga M, Ngure J. Factors influencing the utilization of voluntary counselling and testing services among university students in Kenya. Glob J Health Sci. 2014;6(4):84-93. [Link] [DOI:10.5539/gjhs.v6n4p84]
20. Alem AT, Sisay MM, Alemayehu AM. Factors affecting voluntary HIV/AIDS counseling and testing service utilization among Youth in Gondar City, Northwest Ethiopia. HIV AIDS. 2020;12:667-73. [Link] [DOI:10.2147/HIV.S267494]
21. Wang Y, Li B, Zheng J, Sengupta S, Emrick CB, Cohen MS, et al. Factors related to female sex workers' willingness to utilize VCT service: A qualitative study in Jinan city, northern China. AIDS Behav. 2009;13(5):866-72. [Link] [DOI:10.1007/s10461-008-9446-5]
22. Van Dyk AC, Van Dyk PJ. "To know or not to know": Service-related barriers to voiuntary HIV counseling and testing (VCT) in South Africa. Curationis. 2003;26(1):4-10. [Link] [DOI:10.4102/curationis.v26i1.1289]
23. Shitaye A, Abseno N, Degu G, Wondmikun Y, Amsalu S. Knowledge and attitude towards voluntary counseling and testing for HIV: A community based study in northwest Ethiopia. Ethiop J Health Dev. 2004;18(2). [Link] [DOI:10.4314/ejhd.v18i2.9942]
24. Mahato PK, Bi P, Burgess T. Voluntary counseling and testing (VCT) services and its role in HIV/AIDS prevention and management in Nepal. South East Asian J Public Health. 2013;3(1):10-6. [Link] [DOI:10.3329/seajph.v3i1.17705]
25. Ditekemena J, Matendo R, Koole O, Colebunders R, Kashamuka M, Tshefu A, et al. Male partner voluntary counselling and testing associated with the antenatal services in Kinshasa, Democratic Republic of Congo: A randomized controlled trial. Int J STD AIDS. 2011;22(3):165-70. [Link] [DOI:10.1258/ijsa.2010.010379]
26. Purwaningsih P, Misutarno M, Imamah SN. Analysis factor related to VCT utilization for the high risk person of HIV/AIDS. Nurs J. 2011;6(1):58-67. [Link] [DOI:10.20473/jn.v6i1.3966]
27. Hirut BM. Factors influencing HIV voluntary counseling and testing (VCT) service utilization among youth of Hawassa town: A health belief model approach, southern Ethiopia. J Sci Dev. 2014;2(1):49-58. [Link]
28. Ndwiga T, Omwono M. A study of factors influencing VCT service utilization among the youths: A case study of kapsabet division, Nandi County, Kenya. World J AIDS. 2014;4:281-6. [Link] [DOI:10.4236/wja.2014.43032]
29. Teklehaimanot HD, Teklehaimanot A, Yohannes M, Biratu D. Factors influencing the uptake of voluntary HIV counseling and testing in rural Ethiopia: A cross sectional study. BMC Public Health. 2016;16:239. [Link] [DOI:10.1186/s12889-016-2918-z]
30. Ernawati E, Hairuddin K, Palallo UD. Factors that influence the use of voluntary counseling and testing (VCT) clinics by people living with HIV/AIDS in MSM group. JURNAL ILMIAH KESEHATAN SANDI HUSADA. 2024;13(2):353-9. [Link] [DOI:10.35816/jiskh.v13i2.1223]
31. Mandagi AM, Sari JDE, Prayoga D, Lailiyah S, Rahman VN, Khoirunnisa A. The role of pregnant women's perception and social support on the utilization of VCT services. J Educ Health Community Psychol. 2022;11(2):479-96. [Link] [DOI:10.12928/jehcp.v11i2.23726]
32. Perdana MV, Demartoto A, Indarto D. Effects of predisposing, enabling, and reinforcing factors on the uptake of voluntary counselling and testing among female sex workers in Grobogan, Central Java. J Health Promot Behav. 2017;2(3):242-56. [Link] [DOI:10.26911/thejhpb.2017.02.03.05]
33. Suryani AI, San Sao MM. The determinants perception of male sex with man (MSM) concerning the utilization of VCT (voluntary counselling and testing) HIV/AIDS in Dili Municipality, Timor-Leste. JURNAL ILMU KESEHATAN. 2021;9(1):22-30. [Link] [DOI:10.30650/jik.v9i1.1952]
34. Shrestha R. Determinants of voluntary HIV counseling and testing (VCT) uptake among men who have sex with men (MSM) in Nepal. Bergen: The University of Bergen; 2015. [Link]