Volume 16, Issue 3 (2024)
Iran J War Public Health 2024, 16(3): 253-259 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2024/09/1 | Accepted: 2024/10/1 | Published: 2024/11/1
Received: 2024/09/1 | Accepted: 2024/10/1 | Published: 2024/11/1
How to cite this article
Threesittidath K, Chunawa C, Khutok K. Effect of Personal Factors, Occupation, and Pain Location on Pain Levels of Patients with Musculoskeletal Disorders in Rural Areas of Thailand. Iran J War Public Health 2024; 16 (3) :253-259
URL: http://ijwph.ir/article-1-1505-en.html
URL: http://ijwph.ir/article-1-1505-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
1- “Department of Physical Therapy, School of Allied Health Sciences” and “Movement Sciences and Exercise Research Center”, Walailak University, Nakhon Si Thammarat, Thailand
2- Physical Therapy Department, Phrom Khiri Hospital, Nakhon Si Thammarat, Thailand
2- Physical Therapy Department, Phrom Khiri Hospital, Nakhon Si Thammarat, Thailand
Full-Text (HTML) (471 Views)
Introduction
Musculoskeletal disorders (MSDs) refer to any condition causing discomfort or irreversible and disabling injury affecting the motor organs, muscles, tendons, bones, cartilage, ligaments, and nerves [1]. Patients with MSDs often experience physical impairments, such as pain or body discomfort, muscle weakness, and joint stiffness [1, 2]. MSDs are a significant health problem and a leading cause of pain and disability, frequently requiring medical treatment [1]. Furthermore, MSDs limit social participation, increase self-care costs, contribute to more days off work, and reduce the working population [2, 3]. The prevalence of MSDs varies depending on occupation and injury location, with injury rates among occupational groups ranging from 56% to 90% [4, 5]. Previous studies have reported that back injuries are the highest among medical professionals at 76% [5], lower back injuries are prevalent among office workers at 72% [2], and lower limb injuries are widespread among farmers at 65% [6]. Moreover, meta-analyses have revealed that musculoskeletal pain is significantly more prevalent in rural populations globally than in urban populations [7]. Musculoskeletal injuries are also more common in rural areas, where access to healthcare is limited. Patients in these regions often have to travel long distances for treatment, leading to significant delays in diagnosis and management. This highlights the urgent need for improved healthcare access in these areas [7]. Understanding the specific challenges faced by these populations is critical for developing effective treatment and prevention strategies.
Pain is the most common presenting symptom in patients with MSDs [8]. The definition of pain is an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage [9]. Injury-related issues often lead patients with MSDs to decide whether to seek medical treatment based on their pain. The pain factors used in the assessment to comply with the treatment plan include pain level, activity limitations in daily life caused by pain, and pain patterns [8, 10]. The severity of musculoskeletal injuries can be classified using the principles of the International Classification of Functioning, Disability, and Health (ICF), a framework that provides a comprehensive understanding of health and health-related states, which divides severity into three mild, moderate, and severe levels [11]. The most commonly used pain scale in clinical assessment is the Numeric Rating Scale (NRS) [12]. This scale has 11 points, ranging from zero to ten, with no pain rated as zero, mild pain as one to three, moderate pain as four to six, and severe pain as seven to ten [13, 14]. The pain associated with MSDs is often severe, with approximately a quarter of adult patients reporting pain levels of seven or higher on the NRS [15].
Musculoskeletal impairments are influenced by various internal factors, such as age, gender, weight, and stress [16-18]. External factors, including work characteristics like heavy lifting, improper working posture, repetitive tasks, poor workstation design, and the overall workstation environment, can also contribute to injuries [19-21]. Moreover, individuals with lower levels of education have a higher incidence of musculoskeletal injuries compared to those with higher levels of education [22]. Patients from diverse cultural, socioeconomic, and educational backgrounds agree on pain intensity [23-25]. This underscores the importance of adopting a comprehensive pain management approach that considers various socio-cultural factors.
Screening patients is crucial for identifying high-risk or vulnerable groups affected by MSDs. However, understanding the comprehensive impact of MSDs on patients in rural areas remains limited. Therefore, the objective of the study was to identify factors such as personal characteristics, occupation, and pain location that could differentiate patients with MSDs at various pain levels. By elucidating these factors, healthcare providers can develop targeted treatment plans and preventive strategies to mitigate the burden of MSDs among rural populations, ultimately improving patient outcomes and reducing healthcare costs. This research aimed to investigate the influence of personal factors, occupation, and pain location on pain levels in patients with MSDs in a rural area.
Instrument and Methods
Study design and population
This cross-sectional study was conducted on 400 patients with MSDs assessed in the physical therapy department at Phrom Khiri Hospital in Nakhon Si Thammarat Province, Thailand, from 2022 to 2023. Convenience sampling was used to select these patients. The sample size was calculated using the Yamane formula [26], based on a study on the prevalence of musculoskeletal pain in Thailand [27]. The inclusion criteria were volunteers over 18 years old who experienced musculoskeletal pain defined as pain in one of the anatomical areas, including neck, shoulder, upper back, elbow, wrist/hand, lower back, hip/thigh, knee, or ankle/foot and having pain in only one body region, as identified by the NRS. Participants were excluded if they had other systemic symptoms (e.g., symptoms in the nervous, respiratory, or cardiovascular systems) related to pain levels. Furthermore, patients with major musculoskeletal pathologies, such as fractures, spinal cord injuries, or infections were also excluded.
Data collection procedures
This research involved retrospective data collection; therefore, a waiver of the need for informed patient consent was obtained from the hospital. The data were collected in an aggregated form without personal identification. Additionally, this cross-sectional study was approved by the Ethics Committee of Human Research prior to data collection.
Patient self-reports and medical records were used to collect data. All data were anonymized and aggregated for analysis. The collected factors comprised demographic characteristics, including age, weight, height, gender, occupation, location of MSD pain, and baseline pain intensity. Data management grouped pain levels into three categories according to the NRS, including mild pain (scores one to three), moderate pain (scores four to six), and severe pain (scores seven to ten) [13, 14]. The area of pain was grouped into nine body regions following the Nordic standard questionnaire, which demonstrated satisfactory validity [28, 29]. The body mass index (BMI) was calculated using weight (kg) divided by height (m) squared. BMI categories were underweight (<18.50kg/m2), normal (18.50-24.99kg/m2), and overweight (>25.00kg/m2) [30].
Data analysis
Descriptive statistical analysis was used to calculate participant characteristics and the prevalence of MSDs. The factors were analyzed using SPSS 22.0 software. The data were evaluated to determine statistical significance (p<0.05). The distribution of normality of the data was assessed using the Kolmogorov-Smirnov test. The effects of the factors, including age, gender, weight, height, BMI, occupation, and location of pain in participants with MSDs, were analyzed using multiple discriminant analyses.
Findings
A total of 400 participants, including 109 males (27.25%) and 291 females (72.75%), participated in this study. The mean age for participants with mild, moderate, and severe pain was 60.00±14.30, 59.44±12.97, and 59.15±14.32 years, respectively, while pain intensity was 2.43±0.57, 5.05±0.70, and 7.46±0.55. The mean weight for participants with mild, moderate, and severe pain was 58.42±11.40, 61.78±11.20, and 59.57±10.60kg, respectively, while the mean height was 160.90±8.98, 158.06±7.68, and 157.21±7.46cm. The average BMI was 24.19kg/m².
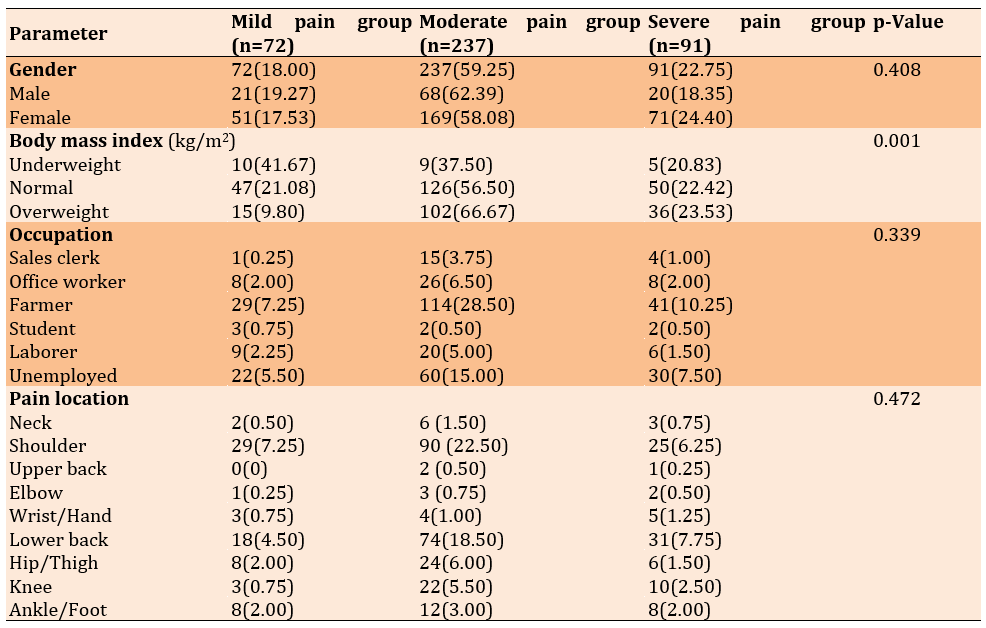
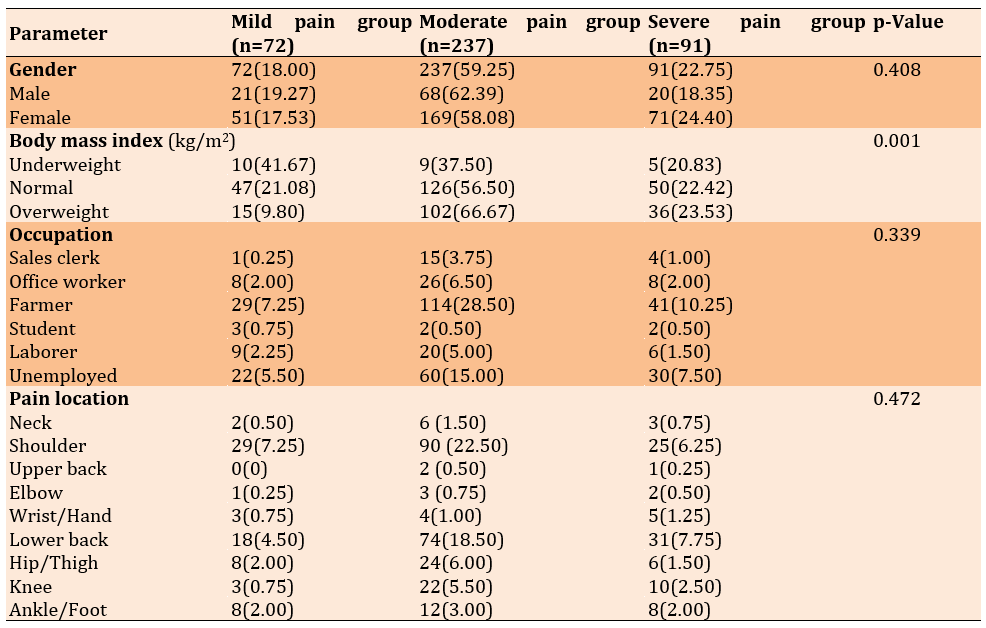
The participants were primarily farmers, comprising 184 individuals (46.00%). The location of pain was distributed across nine regions, including shoulder 144 (36.00%), lower back 123 (30.75%), hip/thigh 38 (9.50%), knee 35 (8.75%), ankle/foot 28 (7.00%), wrist/hand 12 (3.00%), neck 11 (2.75%), elbow 6 (1.50%), and upper back 3 (0.75%; Table 1).
Table 1. Frequency of demographic characteristics of the participants (n=400)
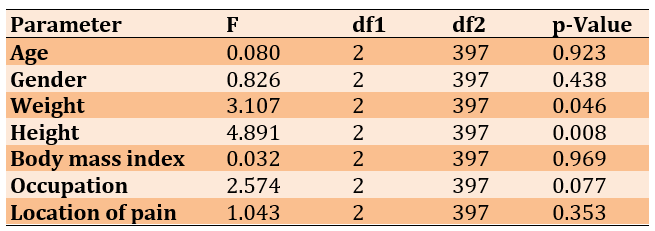
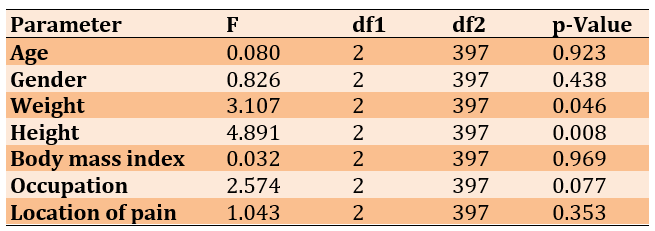
There was a significant difference in weight (p=0.046) and height (p=0.008) among the three groups of mild, moderate, and severe pain. In contrast, there were no significant differences in age, gender, BMI, occupation, and location of pain (p>0.05; Table 2).
Table 2. Difference of factors among the three groups
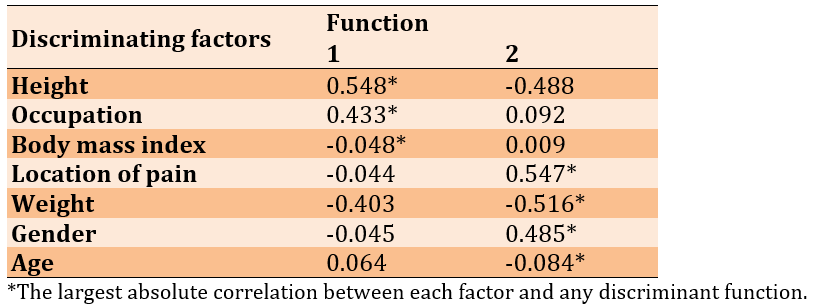
The discriminant analysis identified two functions that distinguished between the groups. The first function, characterized by an eigenvalue of 0.068, accounted for 80% of the variance, while the second function, with an eigenvalue of 0.017, explained the remaining 20%. A canonical correlation of 0.253 for the first function reflected a moderate association between group membership and the discriminant function, whereas the second function, with a correlation of 0.130, exhibited a weaker relationship. The combined Wilks’ Lambda value of 0.920 and a chi-squared statistic of 32.750 (p=0.003) indicated that all factors significantly predicted pain levels for MSDs across the groups. However, the second function alone, with a Wilks’ Lambda of 0.983 (p=0.351), did not demonstrate a statistically significant distinction between the groups.
The data analysis led to the development of formulas that could predict pain levels in each group.
Mild pain=-294.012+0.690 (age)+15.558 (gender)-0.361 (weight)+3.229 (height)+6.481 (BMI)+1.782 (occupation)-0.672 (location of pain)
Moderate pain=-283.057+0.689 (age)+15.422 (gender)-0.307 (weight)+3.149 (height)+6.274 (BMI)+1.555 (occupation)-0.679 (Location of pain)
Severe pain=-282.344+0.681 (age)+15.780 (gender)-0.328 (weight)+3.148 (height)+6.333 (BMI)+1.594 (occupation)-0.754 (location of pain) influence of pain level on personal factors, occupation, and location of pain.
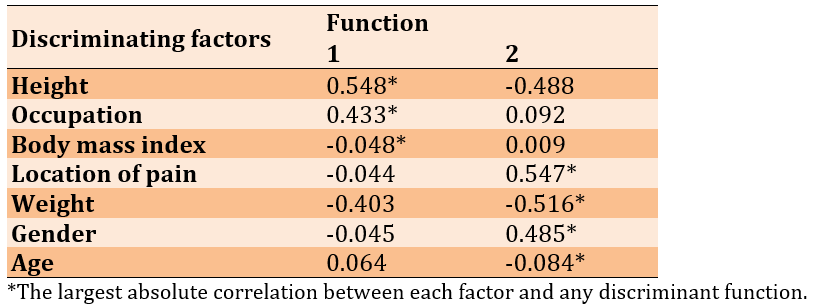
The data analysis revealed the functions of group centroids, indicating that each factor influenced the pain classification within each group. The mild and moderate pain level groups were represented in Function 1, while the severe pain level group was represented in Function 2. The interpretation indicated that participants with MSDs in the mild pain level group were predicted by height and occupation. In contrast, the severe pain level group was predicted by location of pain, gender, and weight. However, the moderate pain level group showed predictions based on a combination of height and occupation (Table 3).
Table 3. Factors influencing pain classification
The discriminant model for predicting group membership found that 39 of 72 participants (54.17%) were accurately classified as having mild pain. A moderate pain level was correctly classified for 91 of 237 participants (38.40%), while a severe pain level was correctly classified for 31 of 91 participants (34.07%). The classification model indicated that 41.25% of the originally grouped 400 participants with MSDs were classified with the correct pain level.
Discussion
This research aimed to investigate the influence of personal factors, occupation, and pain location on pain levels in patients with musculoskeletal disorders in a rural area. To determine the influence of personal factors, occupation, and pain location on pain intensity in patients with MSDs, the results showed that participants in the mild pain level group had a pain score that could be predicted by height and occupation. Additionally, severe pain levels were predicted by the location of pain, gender, and weight. However, a combination of height and occupation predicted a moderate pain level.
Pain is caused by noxious stimuli that stimulate the sensory perception of pain and aggravate pain impulse pathways, which enter the spinal cord and brain. The nerve fibers responsible for pain perception include A-delta and C-fiber fibers. After the pain impulse reaches the brain, sensory-discriminative processing occurs, allowing for conscious awareness of pain intensity [31]. Additionally, physiological mechanisms and the neuroimmune system change after injury, leading to nociceptive responses that indicate pain through central nervous system (CNS) signals [31]. Pain in patients with MSDs affects their daily activities and overall quality of life. A cause of pain after injury arises from the adaptation of tissues, which leads to neuroplasticity and subsequent CNS sensitization in the brain [32]. Furthermore, processing following a musculoskeletal injury induces neuroimmune activation, resulting in the release of pain mediators, including nitric oxide, substance P, and glutamate. These mediators lead to neuronal hypersensitivity, causing patients with MSDs to experience heightened feelings of pain [31]. Pain assessment is essential for implementing proper pain management interventions. The intensity of pain is related to a highly subjective experience, which was reported within the three groups, including mild, moderate, and severe pain levels [33].
The location of MSD pain is associated with activity in the somatosensory cortex during human pain processing. This location can predict pain intensity due to the coding mechanisms in the brain that generate signals [34]. Moreover, previous studies have found that the distributed processing of pain intensity within the human brain can detect tissue injury associated with both the primary and secondary somatosensory cortices, which exhibit differences in pain levels [34]. Additionally, research has shown that neuropathic symptoms can lead to musculoskeletal pain, particularly in the neck, back, and shoulders [35, 36]. This study, along with previous research, supports the findings that the location of pain can predict severe discomfort in patients with MSD.
Occupation could predict the pain scale in the mild and moderate pain level groups. Several studies on work disability related to the causes of musculoskeletal pain have focused on physical exposures, including manual material handling, repetitive movements, awkward postures, and vibrations [17, 19, 20]. Repetitive movements, such as performing a mono task during work, can induce musculoskeletal injuries that lead to pain symptoms [19, 37]. Moreover, the type of exposure varies between occupational groups and significantly correlates with an increase in the prevalence of MSDs [10, 38]. However, the study indicated that the pain experienced by individuals in the severe pain group was not related to occupation, possibly due to differences in individual variability, psychosocial factors, and adaptive mechanisms.
There are differences between genders in the way individuals perceive pain and exhibit greater sensitivity to experimentally induced pain [39]. Women appear to have lower pain thresholds, higher pain ratings, and a greater ability to distinguish between unpleasant sensations and lower pain tolerance [40]. Previous research has demonstrated that experts generally agree that a few factors, such as physiological mechanisms and perceptual capacity, account for gender variations in pain and its treatment [40]. Similarly, women tend to experience pain in more anatomical regions of the body and report pain more frequently and for longer durations than men, indicating a higher prevalence of pain among women [39]. According to the study, the severe pain group had 3.5 times more females than males, which significantly impacted those experiencing severe pain.
Body height is primarily influenced by genetic factors; however, conditions during fetal development and childhood, malnutrition, past illnesses, and psychosocial factors also play significant roles [41]. A previous study found that height is related to the risk of injury. Patients who are at least 170cm tall and do not have lower back pain (LBP) at baseline have a 19% higher risk of developing LBP compared to patients shorter than 160cm [42]. This finding aligns with another study reporting a statistically significant but low positive correlation between pain intensity and height [43]. The results of this study showed that participants in the mild pain group have an average height greater than those in the moderate and severe pain groups. Therefore, height may affect pain intensity in patients with MSDs in the mild pain group.
Numerous studies have shown that MSDs in the back, hip, knee, ankle, foot, and shoulder are linked to a patient’s body weight [18, 44, 45]. Excessive loading of the musculoskeletal system can lead to stress and strain on connective tissues, such as muscles, nerves, joints, and bones. Changes in biomechanics due to weight can impact skeletal alignment and muscle condition [45, 46]. Therefore, body weight can be a reliable indicator of pain levels in individuals experiencing severe pain due to structural changes.
This study found that BMI alone is insufficient to predict a patient’s pain level and needs to be combined with other determinants. However, previous research has indicated a strong connection between BMI and pain intensity in patients with MSDs, especially in those who are overweight or obese due to the load-bearing on joints [46]. Additionally, a previous study reported that pain intensity had a positive correlation with BMI in patients who experienced neck pain, with the majority being overweight or obese individuals suffering from severe pain [43]. Another possibility is that individuals with patellofemoral pain presented with a higher BMI compared to those without patellofemoral pain [47]. This study revealed that the average BMI of the patients was primarily within the normal range. Therefore, BMI in the present study was not a factor that predicted pain intensity in all groups. Furthermore, another factor that was insufficient to indicate pain levels in patients with MSDs was age. This finding is inconsistent with previous studies indicating age-related MSDs in patients from rural areas [6, 48, 49]. Previous research has shown that age influences pain perception due to differences in nociceptive fibers. Elderly individuals tend to rely more on C-fibers for input when reporting pain compared to young adults [16, 50]. However, this study demonstrated that age was not a significant factor in pain levels. This may be due to other factors, such as underlying diseases, lifestyle, or mental conditions, that may not be readily apparent in individuals. The findings of the present study, which identified factors influencing pain levels and formulated a predictive model for pain, have the potential to revolutionize the treatment and management of MSDs. Additionally, the study revealed unique characteristics associated with each pain level that were previously unreported. These insights could significantly enhance the planning of treatments and management strategies for MSDs, offering hope for improved patient outcomes.
For participants with mild pain levels, their pain scores could be predicted by height and occupation. In contrast, the combination of gender and weight predicted severe pain levels, while the combination of height and occupation predicted moderate pain levels. These findings suggest that individuals with MSD should be mindful of factors that can exacerbate their pain, as addressing these factors could aid in planning effective treatments and managing MSDs, potentially reducing the risk of future disability.
The study had some limitations. Firstly, this study relies on the pain intensity level, which depends on the subjective experience of pain. However, this method is one of the best outcomes for monitoring patient symptoms in a clinical setting. Secondly, the participants primarily came from rural areas, which may involve different factors compared to patients in urban areas. Lastly, the number of participants and the location of pain among the three groups were not equal. For future studies, the researchers are interested in using objective measures of pain, examining the effects of psychosocial factors as potential risk factors, and identifying effective treatment management strategies for each pain level group.
Conclusion
Personal factors, occupation, and location of pain are predictors of pain levels in patients with MSDs.
Acknowledgments: The authors express their gratitude to the School of Allied Health Sciences at Walailak University and Phrom Khiri Hospital in Nakhon Si Thammarat, Thailand, for their support of this study. We would also like to thank all the participants and Mr. David C. Chang for his assistance with English manuscript editing.
Ethical Permissions: This study was approved by the Human Research Committee of Walailak University (Approval number WUEC-22-268-01).
Conflicts of Interests: The authors declared no conflicts of interests.
Authors' Contribution: Threesittidath K (First Author), Introduction Writer/Original Researcher/Methodologist/Statistical Analyst/Discussion Writer (45%); Chunawa Ch (Second Author), Assistant Researcher/Methodologist (15%); Khutok K (Third Author), Introduction Writer/Assistant Researcher/Statistical Analyst/Discussion Writer (40%)
Funding/Support: The authors reported no funding.
Musculoskeletal disorders (MSDs) refer to any condition causing discomfort or irreversible and disabling injury affecting the motor organs, muscles, tendons, bones, cartilage, ligaments, and nerves [1]. Patients with MSDs often experience physical impairments, such as pain or body discomfort, muscle weakness, and joint stiffness [1, 2]. MSDs are a significant health problem and a leading cause of pain and disability, frequently requiring medical treatment [1]. Furthermore, MSDs limit social participation, increase self-care costs, contribute to more days off work, and reduce the working population [2, 3]. The prevalence of MSDs varies depending on occupation and injury location, with injury rates among occupational groups ranging from 56% to 90% [4, 5]. Previous studies have reported that back injuries are the highest among medical professionals at 76% [5], lower back injuries are prevalent among office workers at 72% [2], and lower limb injuries are widespread among farmers at 65% [6]. Moreover, meta-analyses have revealed that musculoskeletal pain is significantly more prevalent in rural populations globally than in urban populations [7]. Musculoskeletal injuries are also more common in rural areas, where access to healthcare is limited. Patients in these regions often have to travel long distances for treatment, leading to significant delays in diagnosis and management. This highlights the urgent need for improved healthcare access in these areas [7]. Understanding the specific challenges faced by these populations is critical for developing effective treatment and prevention strategies.
Pain is the most common presenting symptom in patients with MSDs [8]. The definition of pain is an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage [9]. Injury-related issues often lead patients with MSDs to decide whether to seek medical treatment based on their pain. The pain factors used in the assessment to comply with the treatment plan include pain level, activity limitations in daily life caused by pain, and pain patterns [8, 10]. The severity of musculoskeletal injuries can be classified using the principles of the International Classification of Functioning, Disability, and Health (ICF), a framework that provides a comprehensive understanding of health and health-related states, which divides severity into three mild, moderate, and severe levels [11]. The most commonly used pain scale in clinical assessment is the Numeric Rating Scale (NRS) [12]. This scale has 11 points, ranging from zero to ten, with no pain rated as zero, mild pain as one to three, moderate pain as four to six, and severe pain as seven to ten [13, 14]. The pain associated with MSDs is often severe, with approximately a quarter of adult patients reporting pain levels of seven or higher on the NRS [15].
Musculoskeletal impairments are influenced by various internal factors, such as age, gender, weight, and stress [16-18]. External factors, including work characteristics like heavy lifting, improper working posture, repetitive tasks, poor workstation design, and the overall workstation environment, can also contribute to injuries [19-21]. Moreover, individuals with lower levels of education have a higher incidence of musculoskeletal injuries compared to those with higher levels of education [22]. Patients from diverse cultural, socioeconomic, and educational backgrounds agree on pain intensity [23-25]. This underscores the importance of adopting a comprehensive pain management approach that considers various socio-cultural factors.
Screening patients is crucial for identifying high-risk or vulnerable groups affected by MSDs. However, understanding the comprehensive impact of MSDs on patients in rural areas remains limited. Therefore, the objective of the study was to identify factors such as personal characteristics, occupation, and pain location that could differentiate patients with MSDs at various pain levels. By elucidating these factors, healthcare providers can develop targeted treatment plans and preventive strategies to mitigate the burden of MSDs among rural populations, ultimately improving patient outcomes and reducing healthcare costs. This research aimed to investigate the influence of personal factors, occupation, and pain location on pain levels in patients with MSDs in a rural area.
Instrument and Methods
Study design and population
This cross-sectional study was conducted on 400 patients with MSDs assessed in the physical therapy department at Phrom Khiri Hospital in Nakhon Si Thammarat Province, Thailand, from 2022 to 2023. Convenience sampling was used to select these patients. The sample size was calculated using the Yamane formula [26], based on a study on the prevalence of musculoskeletal pain in Thailand [27]. The inclusion criteria were volunteers over 18 years old who experienced musculoskeletal pain defined as pain in one of the anatomical areas, including neck, shoulder, upper back, elbow, wrist/hand, lower back, hip/thigh, knee, or ankle/foot and having pain in only one body region, as identified by the NRS. Participants were excluded if they had other systemic symptoms (e.g., symptoms in the nervous, respiratory, or cardiovascular systems) related to pain levels. Furthermore, patients with major musculoskeletal pathologies, such as fractures, spinal cord injuries, or infections were also excluded.
Data collection procedures
This research involved retrospective data collection; therefore, a waiver of the need for informed patient consent was obtained from the hospital. The data were collected in an aggregated form without personal identification. Additionally, this cross-sectional study was approved by the Ethics Committee of Human Research prior to data collection.
Patient self-reports and medical records were used to collect data. All data were anonymized and aggregated for analysis. The collected factors comprised demographic characteristics, including age, weight, height, gender, occupation, location of MSD pain, and baseline pain intensity. Data management grouped pain levels into three categories according to the NRS, including mild pain (scores one to three), moderate pain (scores four to six), and severe pain (scores seven to ten) [13, 14]. The area of pain was grouped into nine body regions following the Nordic standard questionnaire, which demonstrated satisfactory validity [28, 29]. The body mass index (BMI) was calculated using weight (kg) divided by height (m) squared. BMI categories were underweight (<18.50kg/m2), normal (18.50-24.99kg/m2), and overweight (>25.00kg/m2) [30].
Data analysis
Descriptive statistical analysis was used to calculate participant characteristics and the prevalence of MSDs. The factors were analyzed using SPSS 22.0 software. The data were evaluated to determine statistical significance (p<0.05). The distribution of normality of the data was assessed using the Kolmogorov-Smirnov test. The effects of the factors, including age, gender, weight, height, BMI, occupation, and location of pain in participants with MSDs, were analyzed using multiple discriminant analyses.
Findings
A total of 400 participants, including 109 males (27.25%) and 291 females (72.75%), participated in this study. The mean age for participants with mild, moderate, and severe pain was 60.00±14.30, 59.44±12.97, and 59.15±14.32 years, respectively, while pain intensity was 2.43±0.57, 5.05±0.70, and 7.46±0.55. The mean weight for participants with mild, moderate, and severe pain was 58.42±11.40, 61.78±11.20, and 59.57±10.60kg, respectively, while the mean height was 160.90±8.98, 158.06±7.68, and 157.21±7.46cm. The average BMI was 24.19kg/m².
The participants were primarily farmers, comprising 184 individuals (46.00%). The location of pain was distributed across nine regions, including shoulder 144 (36.00%), lower back 123 (30.75%), hip/thigh 38 (9.50%), knee 35 (8.75%), ankle/foot 28 (7.00%), wrist/hand 12 (3.00%), neck 11 (2.75%), elbow 6 (1.50%), and upper back 3 (0.75%; Table 1).
Table 1. Frequency of demographic characteristics of the participants (n=400)
There was a significant difference in weight (p=0.046) and height (p=0.008) among the three groups of mild, moderate, and severe pain. In contrast, there were no significant differences in age, gender, BMI, occupation, and location of pain (p>0.05; Table 2).
Table 2. Difference of factors among the three groups
The discriminant analysis identified two functions that distinguished between the groups. The first function, characterized by an eigenvalue of 0.068, accounted for 80% of the variance, while the second function, with an eigenvalue of 0.017, explained the remaining 20%. A canonical correlation of 0.253 for the first function reflected a moderate association between group membership and the discriminant function, whereas the second function, with a correlation of 0.130, exhibited a weaker relationship. The combined Wilks’ Lambda value of 0.920 and a chi-squared statistic of 32.750 (p=0.003) indicated that all factors significantly predicted pain levels for MSDs across the groups. However, the second function alone, with a Wilks’ Lambda of 0.983 (p=0.351), did not demonstrate a statistically significant distinction between the groups.
The data analysis led to the development of formulas that could predict pain levels in each group.
Mild pain=-294.012+0.690 (age)+15.558 (gender)-0.361 (weight)+3.229 (height)+6.481 (BMI)+1.782 (occupation)-0.672 (location of pain)
Moderate pain=-283.057+0.689 (age)+15.422 (gender)-0.307 (weight)+3.149 (height)+6.274 (BMI)+1.555 (occupation)-0.679 (Location of pain)
Severe pain=-282.344+0.681 (age)+15.780 (gender)-0.328 (weight)+3.148 (height)+6.333 (BMI)+1.594 (occupation)-0.754 (location of pain) influence of pain level on personal factors, occupation, and location of pain.
The data analysis revealed the functions of group centroids, indicating that each factor influenced the pain classification within each group. The mild and moderate pain level groups were represented in Function 1, while the severe pain level group was represented in Function 2. The interpretation indicated that participants with MSDs in the mild pain level group were predicted by height and occupation. In contrast, the severe pain level group was predicted by location of pain, gender, and weight. However, the moderate pain level group showed predictions based on a combination of height and occupation (Table 3).
Table 3. Factors influencing pain classification
The discriminant model for predicting group membership found that 39 of 72 participants (54.17%) were accurately classified as having mild pain. A moderate pain level was correctly classified for 91 of 237 participants (38.40%), while a severe pain level was correctly classified for 31 of 91 participants (34.07%). The classification model indicated that 41.25% of the originally grouped 400 participants with MSDs were classified with the correct pain level.
Discussion
This research aimed to investigate the influence of personal factors, occupation, and pain location on pain levels in patients with musculoskeletal disorders in a rural area. To determine the influence of personal factors, occupation, and pain location on pain intensity in patients with MSDs, the results showed that participants in the mild pain level group had a pain score that could be predicted by height and occupation. Additionally, severe pain levels were predicted by the location of pain, gender, and weight. However, a combination of height and occupation predicted a moderate pain level.
Pain is caused by noxious stimuli that stimulate the sensory perception of pain and aggravate pain impulse pathways, which enter the spinal cord and brain. The nerve fibers responsible for pain perception include A-delta and C-fiber fibers. After the pain impulse reaches the brain, sensory-discriminative processing occurs, allowing for conscious awareness of pain intensity [31]. Additionally, physiological mechanisms and the neuroimmune system change after injury, leading to nociceptive responses that indicate pain through central nervous system (CNS) signals [31]. Pain in patients with MSDs affects their daily activities and overall quality of life. A cause of pain after injury arises from the adaptation of tissues, which leads to neuroplasticity and subsequent CNS sensitization in the brain [32]. Furthermore, processing following a musculoskeletal injury induces neuroimmune activation, resulting in the release of pain mediators, including nitric oxide, substance P, and glutamate. These mediators lead to neuronal hypersensitivity, causing patients with MSDs to experience heightened feelings of pain [31]. Pain assessment is essential for implementing proper pain management interventions. The intensity of pain is related to a highly subjective experience, which was reported within the three groups, including mild, moderate, and severe pain levels [33].
The location of MSD pain is associated with activity in the somatosensory cortex during human pain processing. This location can predict pain intensity due to the coding mechanisms in the brain that generate signals [34]. Moreover, previous studies have found that the distributed processing of pain intensity within the human brain can detect tissue injury associated with both the primary and secondary somatosensory cortices, which exhibit differences in pain levels [34]. Additionally, research has shown that neuropathic symptoms can lead to musculoskeletal pain, particularly in the neck, back, and shoulders [35, 36]. This study, along with previous research, supports the findings that the location of pain can predict severe discomfort in patients with MSD.
Occupation could predict the pain scale in the mild and moderate pain level groups. Several studies on work disability related to the causes of musculoskeletal pain have focused on physical exposures, including manual material handling, repetitive movements, awkward postures, and vibrations [17, 19, 20]. Repetitive movements, such as performing a mono task during work, can induce musculoskeletal injuries that lead to pain symptoms [19, 37]. Moreover, the type of exposure varies between occupational groups and significantly correlates with an increase in the prevalence of MSDs [10, 38]. However, the study indicated that the pain experienced by individuals in the severe pain group was not related to occupation, possibly due to differences in individual variability, psychosocial factors, and adaptive mechanisms.
There are differences between genders in the way individuals perceive pain and exhibit greater sensitivity to experimentally induced pain [39]. Women appear to have lower pain thresholds, higher pain ratings, and a greater ability to distinguish between unpleasant sensations and lower pain tolerance [40]. Previous research has demonstrated that experts generally agree that a few factors, such as physiological mechanisms and perceptual capacity, account for gender variations in pain and its treatment [40]. Similarly, women tend to experience pain in more anatomical regions of the body and report pain more frequently and for longer durations than men, indicating a higher prevalence of pain among women [39]. According to the study, the severe pain group had 3.5 times more females than males, which significantly impacted those experiencing severe pain.
Body height is primarily influenced by genetic factors; however, conditions during fetal development and childhood, malnutrition, past illnesses, and psychosocial factors also play significant roles [41]. A previous study found that height is related to the risk of injury. Patients who are at least 170cm tall and do not have lower back pain (LBP) at baseline have a 19% higher risk of developing LBP compared to patients shorter than 160cm [42]. This finding aligns with another study reporting a statistically significant but low positive correlation between pain intensity and height [43]. The results of this study showed that participants in the mild pain group have an average height greater than those in the moderate and severe pain groups. Therefore, height may affect pain intensity in patients with MSDs in the mild pain group.
Numerous studies have shown that MSDs in the back, hip, knee, ankle, foot, and shoulder are linked to a patient’s body weight [18, 44, 45]. Excessive loading of the musculoskeletal system can lead to stress and strain on connective tissues, such as muscles, nerves, joints, and bones. Changes in biomechanics due to weight can impact skeletal alignment and muscle condition [45, 46]. Therefore, body weight can be a reliable indicator of pain levels in individuals experiencing severe pain due to structural changes.
This study found that BMI alone is insufficient to predict a patient’s pain level and needs to be combined with other determinants. However, previous research has indicated a strong connection between BMI and pain intensity in patients with MSDs, especially in those who are overweight or obese due to the load-bearing on joints [46]. Additionally, a previous study reported that pain intensity had a positive correlation with BMI in patients who experienced neck pain, with the majority being overweight or obese individuals suffering from severe pain [43]. Another possibility is that individuals with patellofemoral pain presented with a higher BMI compared to those without patellofemoral pain [47]. This study revealed that the average BMI of the patients was primarily within the normal range. Therefore, BMI in the present study was not a factor that predicted pain intensity in all groups. Furthermore, another factor that was insufficient to indicate pain levels in patients with MSDs was age. This finding is inconsistent with previous studies indicating age-related MSDs in patients from rural areas [6, 48, 49]. Previous research has shown that age influences pain perception due to differences in nociceptive fibers. Elderly individuals tend to rely more on C-fibers for input when reporting pain compared to young adults [16, 50]. However, this study demonstrated that age was not a significant factor in pain levels. This may be due to other factors, such as underlying diseases, lifestyle, or mental conditions, that may not be readily apparent in individuals. The findings of the present study, which identified factors influencing pain levels and formulated a predictive model for pain, have the potential to revolutionize the treatment and management of MSDs. Additionally, the study revealed unique characteristics associated with each pain level that were previously unreported. These insights could significantly enhance the planning of treatments and management strategies for MSDs, offering hope for improved patient outcomes.
For participants with mild pain levels, their pain scores could be predicted by height and occupation. In contrast, the combination of gender and weight predicted severe pain levels, while the combination of height and occupation predicted moderate pain levels. These findings suggest that individuals with MSD should be mindful of factors that can exacerbate their pain, as addressing these factors could aid in planning effective treatments and managing MSDs, potentially reducing the risk of future disability.
The study had some limitations. Firstly, this study relies on the pain intensity level, which depends on the subjective experience of pain. However, this method is one of the best outcomes for monitoring patient symptoms in a clinical setting. Secondly, the participants primarily came from rural areas, which may involve different factors compared to patients in urban areas. Lastly, the number of participants and the location of pain among the three groups were not equal. For future studies, the researchers are interested in using objective measures of pain, examining the effects of psychosocial factors as potential risk factors, and identifying effective treatment management strategies for each pain level group.
Conclusion
Personal factors, occupation, and location of pain are predictors of pain levels in patients with MSDs.
Acknowledgments: The authors express their gratitude to the School of Allied Health Sciences at Walailak University and Phrom Khiri Hospital in Nakhon Si Thammarat, Thailand, for their support of this study. We would also like to thank all the participants and Mr. David C. Chang for his assistance with English manuscript editing.
Ethical Permissions: This study was approved by the Human Research Committee of Walailak University (Approval number WUEC-22-268-01).
Conflicts of Interests: The authors declared no conflicts of interests.
Authors' Contribution: Threesittidath K (First Author), Introduction Writer/Original Researcher/Methodologist/Statistical Analyst/Discussion Writer (45%); Chunawa Ch (Second Author), Assistant Researcher/Methodologist (15%); Khutok K (Third Author), Introduction Writer/Assistant Researcher/Statistical Analyst/Discussion Writer (40%)
Funding/Support: The authors reported no funding.
Keywords:
References
1. Liu S, Wang B, Fan S, Wang Y, Zhan Y, Ye D. Global burden of musculoskeletal disorders and attributable factors in 204 countries and territories: A secondary analysis of the Global Burden of Disease 2019 study. BMJ Open. 2022;12(6):e062183. [Link] [DOI:10.1136/bmjopen-2022-062183]
2. Murgatroyd DF, Casey PP, Cameron ID, Harris IA. The effect of financial compensation on health outcomes following musculoskeletal injury: Systematic review. PloS One. 2015;10(2):e0117597. [Link] [DOI:10.1371/journal.pone.0117597]
3. Png ME, Mason KJ, Marshall M, Jordan KP, Bailey J, Frisher M, et al. Estimating the direct healthcare utilisation and cost of musculoskeletal pain among people with comorbidity: A retrospective electronic health record study. Curr Med Res Opin. 2023;39(11):1473-80. [Link] [DOI:10.1080/03007995.2023.2271862]
4. Osborne A, Blake C, Fullen BM, Meredith D, Phelan J, McNamara J, et al. Prevalence of musculoskeletal disorders among farmers: A systematic review. Am J Ind Med. 2012;55(2):143-58. [Link] [DOI:10.1002/ajim.21033]
5. Soylar P, Ozer A. Evaluation of the prevalence of musculoskeletal disorders in nurses: A systematic review. Med Sci. 2018;7(3):1. [Link] [DOI:10.5455/medscience.2017.06.8747]
6. Kaewdok T, Sirisawasd S, Taptagaporn S. Agricultural risk factors related musculoskeletal disorders among older farmers in Pathum Thani province, Thailand. J Agromedicine. 2021;26(2):185-92. [Link] [DOI:10.1080/1059924X.2020.1795029]
7. Mesa-Castrillon CI, Beckenkamp PR, Ferreira M, Simic M, Davis PR, Michell A, et al. Global prevalence of musculoskeletal pain in rural and urban populations. A systematic review with meta-analysis. Musculoskeletal pain in rural and urban populations. Aust J Rural Health. 2024;32(5):864-76. [Link] [DOI:10.1111/ajr.13161]
8. Goulet JL, Kerns RD, Bair M, Becker WC, Brennan P, Burgess DJ, et al. The musculoskeletal diagnosis cohort: Examining pain and pain care among veterans. Pain. 2016;157(8):1696-703. [Link] [DOI:10.1097/j.pain.0000000000000567]
9. Raja SN, Carr DB, Cohen M, Finnerup NB, Flor H, Gibson S, et al. The revised international association for the study of pain definition of pain: Concepts, challenges, and compromises. Pain. 2020;161(9):1976-82. [Link] [DOI:10.1097/j.pain.0000000000001939]
10. Cimmino MA, Ferrone C, Cutolo M. Epidemiology of chronic musculoskeletal pain. Best Pract Res Clin Rheumatol. 2011;25(2):173-83. [Link] [DOI:10.1016/j.berh.2010.01.012]
11. Steiner WA, Ryser L, Huber E, Uebelhart D, Aeschlimann A, Stucki G. Use of the ICF model as a clinical problem-solving tool in physical therapy and rehabilitation medicine. Phys Ther. 2002;82(11):1098-107. [Link] [DOI:10.1093/ptj/82.11.1098]
12. Williamson A, Hoggart B. Pain: A review of three commonly used pain rating scales. J Clin Nurs. 2005;14(7):798-804. [Link] [DOI:10.1111/j.1365-2702.2005.01121.x]
13. Boonstra AM, Preuper HRS, Balk GA, Stewart RE. Cut-off points for mild, moderate, and severe pain on the visual analogue scale for pain in patients with chronic musculoskeletal pain. Pain. 2014;155(12):2545-50. [Link] [DOI:10.1016/j.pain.2014.09.014]
14. Palos GR, Mendoza TR, Mobley GM, Cantor SB, Cleeland CS. Asking the community about cutpoints used to describe mild, moderate, and severe pain. J Pain. 2006;7(1):49-56. [Link] [DOI:10.1016/j.jpain.2005.07.012]
15. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789-858. [Link] [DOI:10.1016/S0140-6736(18)32279-7]
16. Lautenbacher S, Peters JH, Heesen M, Scheel J, Kunz M. Age changes in pain perception: A systematic-review and meta-analysis of age effects on pain and tolerance thresholds. Neurosci Biobehav Rev. 2017;75:104-13. [Link] [DOI:10.1016/j.neubiorev.2017.01.039]
17. Punnett L, Wegman DH. Work-related musculoskeletal disorders: The epidemiologic evidence and the debate. J Electromyogr Kinesiol. 2004;14(1):13-23. [Link] [DOI:10.1016/j.jelekin.2003.09.015]
18. Onyemaechi NO, Anyanwu GE, Obikili EN, Onwuasoigwe O, Nwankwo OE. Impact of overweight and obesity on the musculoskeletal system using lumbosacral angles. Patient Prefer Adherence. 2016;10:291-6. [Link] [DOI:10.2147/PPA.S90967]
19. Lomond KV, Côté JN. Differences in posture-movement changes induced by repetitive arm motion in healthy and shoulder-injured individuals. Clin Biomech. 2011;26(2):123-9. [Link] [DOI:10.1016/j.clinbiomech.2010.09.012]
20. Messing K, Stock S, Côté J, Tissot F. Is sitting worse than static standing? How a gender analysis can move us toward understanding determinants and effects of occupational standing and walking. J Occup Environ Hyg. 2015;12(3):D11-7. [Link] [DOI:10.1080/15459624.2014.987388]
21. Mata C, Taneepanichskul N, Taneepanichskul S. Prevalence and risk factors associated with musculoskeletal disorder in maintenance workers of lignite power plant in Thailand. J Health Res. 2017;29(Suppl 2):S169-75. [Link]
22. Atijosan O, Rischewski D, Simms V, Kuper H, Linganwa B, Nuhi A, et al. A national survey of musculoskeletal impairment in Rwanda: Prevalence, causes and service implications. PLoS One. 2008;3(7):e2851. [Link] [DOI:10.1371/journal.pone.0002851]
23. Brady B, Veljanova I, Chipchase L. Are multidisciplinary interventions multicultural? A topical review of the pain literature as it relates to culturally diverse patient groups. Pain. 2016;157(2):321-8. [Link] [DOI:10.1097/j.pain.0000000000000412]
24. Brekke M, Hjortdahl P, Kvien TK. Severity of musculoskeletal pain: Relations to socioeconomic inequality. Soc Sci Med. 2002;54(2):221-8. [Link] [DOI:10.1016/S0277-9536(01)00018-1]
25. Köppen PJ, Dorner TE, Stein KV, Simon J, Crevenna R. Health literacy, pain intensity and pain perception in patients with chronic pain. WIENER KLINISCHE WOCHENSCHRIFT. 2018;130(1-2):23-30. [Link] [DOI:10.1007/s00508-017-1309-5]
26. Louangrath P, Sutanapong C. Minimum sample size calculation using cumulative distribution function. Int J Res Methodol Soc Sci. 2019;5(1):100-13. [Link]
27. Chaiklieng S, Poochada W, Suggaravetsiri P. Work-related diseases among agriculturists in Thailand: A systematic review. Songklanakarin J Sci Technol. 2021;43(3):638-47. [Link]
28. Kuorinka I, Jonsson B, Kilbom A, Vinterberg H, Biering-Sørensen F, Andersson G, et al. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon. 1987;18(3):233-7. [Link] [DOI:10.1016/0003-6870(87)90010-X]
29. Dawson AP, Steele EJ, Hodges PW, Stewart S. Development and test-retest reliability of an extended version of the Nordic Musculoskeletal Questionnaire (NMQ-E): A screening instrument for musculoskeletal pain. J Pain. 2009;10(5):517-26. [Link] [DOI:10.1016/j.jpain.2008.11.008]
30. Zierle-Ghosh A, Jan A. Physiology, body mass index. In: StatPearls. Treasure Island: StatPearls Publishing; 2023. [Link]
31. Winkelstein BA. Mechanisms of central sensitization, neuroimmunology & injury biomechanics in persistent pain: implications for musculoskeletal disorders. J Electromyogr Kinesiol. 2004;14(1):87-93. [Link] [DOI:10.1016/j.jelekin.2003.09.017]
32. Bingel U, Tracey I. Imaging CNS modulation of pain in humans. Physiology. 2008;23(6):371-80. [Link] [DOI:10.1152/physiol.00024.2008]
33. Sluka KA. Pain mechanisms involved in musculoskeletal disorders. J Orthop Sports Phys Ther. 1996;24(4):240-54. [Link] [DOI:10.2519/jospt.1996.24.4.240]
34. Timmermann L, Ploner M, Haucke K, Schmitz F, Baltissen R, Schnitzler A. Differential coding of pain intensity in the human primary and secondary somatosensory cortex. J Neurophysiol. 2001;86(3):1499-503. [Link] [DOI:10.1152/jn.2001.86.3.1499]
35. Fenton BW, Shih E, Zolton J. The neurobiology of pain perception in normal and persistent pain. Pain Manag. 2015;5(4):297-317. [Link] [DOI:10.2217/pmt.15.27]
36. Giske L, Bautz-Holter E, Sandvik L, Røe C. Relationship between pain and neuropathic symptoms in chronic musculoskeletal pain. Pain Med. 2009;10(5):910-7. [Link] [DOI:10.1111/j.1526-4637.2009.00622.x]
37. Coenen P, Willenberg L, Parry S, Shi JW, Romero L, Blackwood DM, et al. Associations of occupational standing with musculoskeletal symptoms: A systematic review with meta-analysis. Br J Sports Med. 2018;52(3):176-83. [Link] [DOI:10.1136/bjsports-2016-096795]
38. Holmström E, Engholm G. Musculoskeletal disorders in relation to age and occupation in Swedish construction workers. Am J Ind Med. 2003;44(4):377-84. [Link] [DOI:10.1002/ajim.10281]
39. Bartley EJ, Palit S. Gender and pain. Curr Anesthesiol Rep. 2016;6(4):344-53. [Link] [DOI:10.1007/s40140-016-0177-2]
40. Vallerand AH, Polomano RC. The relationship of gender to pain. Pain Manag Nurs. 2000;1(3 Suppl 1):8-15. [Link] [DOI:10.1053/jpmn.2000.9759]
41. Shen T, Habicht JP, Chang Y. Effect of economic reforms on child growth in urban and rural areas of China. N Engl J Med. 1996;335(6):400-6. [Link] [DOI:10.1056/NEJM199608083350606]
42. Heuch I, Heuch I, Hagen K, Zwart JA. Association between body height and chronic low back pain: A follow-up in the Nord-Trøndelag health study. BMJ Open. 2015;5(6):e006983. [Link] [DOI:10.1136/bmjopen-2014-006983]
43. Weerakoon T, Dissanayake P, Jayakody S, Weerasekera M, Yasawardene S. Intensity of neck pain and its association with anthropometric measurements. Sri Lanka Anat J. 2021;5(1):19-28. [Link] [DOI:10.4038/slaj.v5i1.130]
44. Higgins DM, Buta E, Heapy AA, Driscoll MA, Kerns RD, Masheb R, et al. The relationship between body mass index and pain intensity among veterans with musculoskeletal disorders: Findings from the MSD cohort study. Pain Med. 2020;21(10):2563-72. [Link] [DOI:10.1093/pm/pnaa043]
45. Wearing SC, Hennig EM, Byrne NM, Steele JR, Hills AP. Musculoskeletal disorders associated with obesity: A biomechanical perspective. Obes Rev. 2006;7(3):239-50. [Link] [DOI:10.1111/j.1467-789X.2006.00251.x]
46. Aekplakorn W, Hogan MC, Chongsuvivatwong V, Tatsanavivat P, Chariyalertsak S, Boonthum A, et al. Trends in obesity and associations with education and urban or rural residence in Thailand. Obesity. 2007;15(12):3113-21. [Link] [DOI:10.1038/oby.2007.371]
47. Ferreira AS, Mentiplay BF, Taborda B, Pazzinatto MF, De Azevedo FM, De Oliveira Silva D. Exploring overweight and obesity beyond body mass index: A body composition analysis in people with and without patellofemoral pain. J Sport Health Sci. 2023;12(5):630-8. [Link] [DOI:10.1016/j.jshs.2021.06.003]
48. Kang F, He Z, Feng B, Qu W, Zhang B, Wang Z. Prevalence and risk factors for MSDs in vegetable greenhouse farmers: A cross-sectional survey from Shandong rural area, China. Med Lav. 2021;112(5):377-86. [Link]
49. Njaka S, Yusoff DM, Anua SM, Kueh YC, Edeogu CO. Musculoskeletal disorders (MSDs) and their associated factors among quarry workers in Nigeria: A cross-sectional study. Heliyon. 2021;7(2):e06130. [Link] [DOI:10.1016/j.heliyon.2021.e06130]
50. Choi K, Park JH, Cheong HK. Prevalence of musculoskeletal symptoms related with activities of daily living and contributing factors in Korean adults. J Prev Med Public Health. 2013;46(1):39-49. [Link] [DOI:10.3961/jpmph.2013.46.1.39]









