Volume 15, Issue 4 (2023)
Iran J War Public Health 2023, 15(4): 435-439 |
Back to browse issues page
Article Type:
Subject:
Ethics code: IR.IUMS.FMD.REC.1399.827
History
Received: 2023/11/29 | Accepted: 2024/04/4 | Published: 2024/04/20
Received: 2023/11/29 | Accepted: 2024/04/4 | Published: 2024/04/20
How to cite this article
Tavassoli F, Aghabiklooei A, Azimi M, Baghai Wadji M, Ahmadi S, Ameri M. Economics of Hospitalization and Medication Therapy for Old COVID-19 Patients; an Experience from a Tertiary Center in Iran. Iran J War Public Health 2023; 15 (4) :435-439
URL: http://ijwph.ir/article-1-1417-en.html
URL: http://ijwph.ir/article-1-1417-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
1- Student Research Committee, Iran University of Medical Sciences, Tehran, Iran
2- “Firoozgar Clinical Research Development Center (FCRDC)” and “Department of Forensic Medicine, Faculty of Medicine”, Iran University of Medical Sciences, Tehran, Iran
3- “Firoozgar Clinical Research Development Center (FCRDC)” and “Department of Internal Medicine, Faculty of Medicine”, Iran University of Medical Sciences, Tehran, Iran
4- “Firoozgar Clinical Research Development Center (FCRDC)” and “Department of Surgery, Faculty of Medicine”, Iran University of Medical Sciences, Tehran, Iran
5- “Preventive Medicine and Public Health Research Center” and “Psychosocial Health Research Institute”, Iran University of Medical Sciences, Tehran, Iran
2- “Firoozgar Clinical Research Development Center (FCRDC)” and “Department of Forensic Medicine, Faculty of Medicine”, Iran University of Medical Sciences, Tehran, Iran
3- “Firoozgar Clinical Research Development Center (FCRDC)” and “Department of Internal Medicine, Faculty of Medicine”, Iran University of Medical Sciences, Tehran, Iran
4- “Firoozgar Clinical Research Development Center (FCRDC)” and “Department of Surgery, Faculty of Medicine”, Iran University of Medical Sciences, Tehran, Iran
5- “Preventive Medicine and Public Health Research Center” and “Psychosocial Health Research Institute”, Iran University of Medical Sciences, Tehran, Iran
Full-Text (HTML) (559 Views)
Introduction
Like many other diseases, the coronavirus disease of 2019 (COVID-19) has a heavy burden on societies and healthcare systems [1-4]. The burden may be greater in developing countries [5]. The burden of COVID-19 is described as a “post-pandemic double burden”, meaning that it has an excessive burden on the health system for managing non-communicable diseases, resulting in a post-pandemic crisis [6].
Other than COVID-19, there will be other similar pandemics in the future. Therefore, it is critical to find an economic plan in such conditions. The experience of 28 countries showed that the COVID-19 pandemic was a shocking event manifesting weak points of governments. The key elements of highly effective country responses were to activate comprehensive responses, adapt health system capacity, preserve health system functions and resources, and reduce vulnerability [7]. For such challenges of the COVID-19 era, economic issues are of great importance. Decision-makers should reach flexible policies that regard economic and ethical issues [8-12].
It is essential to know whether the policies are cost-effective. COVID-19 hospitalization is not an exception and there are economic issues [13, 14]. Among the aspects of the COVID-19 burden, the economic burden of COVID-19 is considerable [3, 15, 16]. For instance, it should be clear whether hospitalization of old COVID-19 patients is helpful and cost-effective. In addition, many drugs used in the management of COVID-19 have unclear rules. COVID-19 is not the first example of a challenge in the treatment of old-aged patients. Senescence has always been a big challenge in health economics. Hence, economic issues are considered in managing elderly diseases [17]. Cost payment for elderlies is not necessarily harmful to the governments. In the US, more than one out of five more than 65-year-old Americans live in high-risk regions of COVID-19, and many of them rely on earnings. Therefore, it is considered economic insecurity [18]. It means that costs for old patients may result in the enhancement of public health in old populations. An editorial emphasized adequate social and medical support for older adults regarding COVID-19 [19].
Due to the controversies about the costs imposed on surveillance and the health system for treating old patients and patients with end-stage disease, the present health economic evaluation study was performed to find the cost-effectiveness of hospitalization and antiviral treatment of COVID-19 in old patients among Iranian cases.
Instrument and Methods
A health economic evaluation as a single-center primary study with a cross-sectional design was performed based on the Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) statement [20] in Firoozgar Hospital, Tehran, Iran, as a referral and tertiary center during the second half of 2020 through a simple random sampling. A health information system (HIS) was used for sampling and access to the data. All the hospitalized cases of COVID-19 at 65 years of age and more were eligible for the study. Confirmation of COVID-19 was through polymerase chain reaction (PCR) or typical involvement in chest computed tomography (CT) scan. The perspective of the study was from healthcare providers. The time horizon of the study was limited to the hospitalization period in which the health outcomes were the Length of Stay (LoS) in day and death as a binary outcome. Due to the limited time horizon, a discount rate was not used. This study was approved by the ethics committee of Iran University of Medical Sciences with registration number IR.IUMS.FMD.REC.1399.827.
Total bed-day costs during admission and the costs of antiviral medications were calculated. The costs were in Iranian Rials (IRR), which were converted to US dollars based on the integrated currency trading system of Iran (locally called NIMA) at the time of data analysis (May 2022). Thus, each dollar was considered to be 250000 IRR.
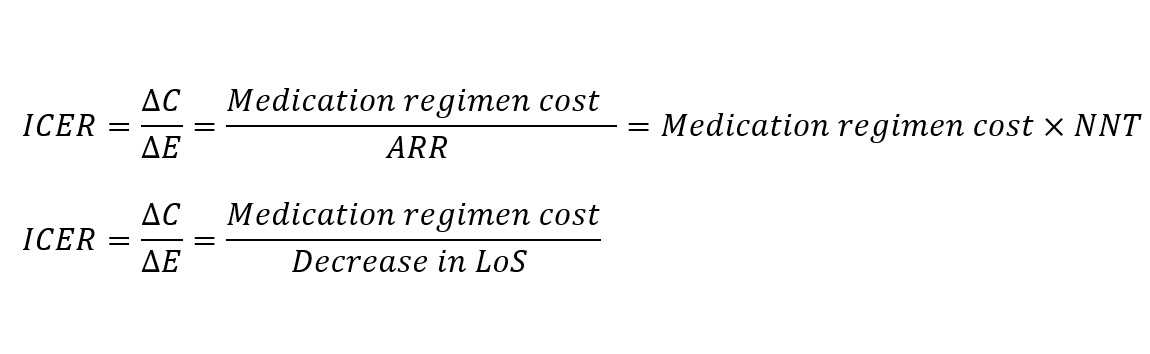
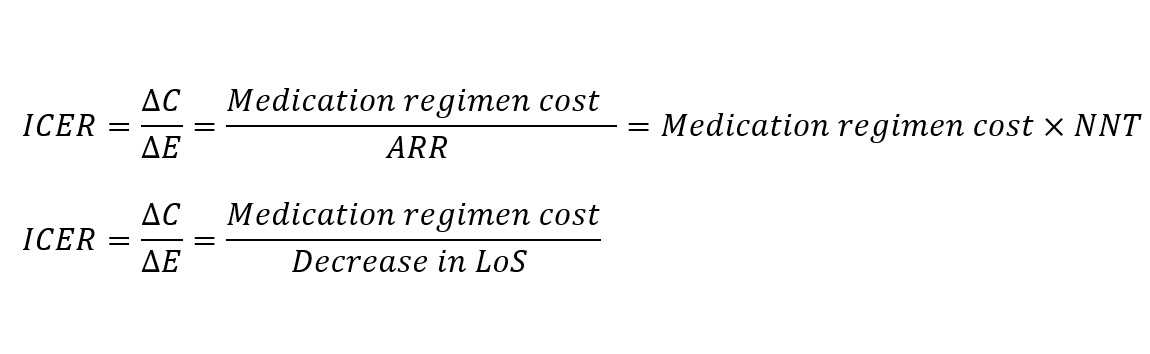
Cost-effectiveness was calculated using the Incremental Cost-Effectiveness Ratio (ICER). ICER was calculated as the following for death and LoS outcomes, respectively. For death outcomes, drugs with a significant absolute risk reduction (ARR) were eligible for ICER calculation. Calculation of ICER based on the Number Needed to Treat (NNT) has been previously used by other researchers [21, 22]. For LOS outcome, drugs with a significant decrease in LoS were eligible for ICER calculation. Stata14 (Stata Corp; USA) was used for data analysis.
Findings
Demographic
Of the admitted patients, 347 cases over 65 were selected for the study. 173 patients (49.86%) were in the age range of 65-74, 69 patients (31.41%) were in the age range of 75-84, and 65 patients (18.73%) were 85 and more. Sex-wise, 145 patients (41.79%) were female and 202 patients (58.21%) were male. 104 patients (29.97%) were admitted to the ward, and 243 patients (70.30%) were admitted to the ICU.
In terms of diagnosis method, 8 patients (2.31%) were diagnosed only by PCR, and the rest, in addition to the positive PCR in chest CT scan were involved by COVID-19. Among the people who had involvement in their CT scans, the average involvement score was 13.09±7.01 from 25. For the number of hospitalizations (for any reason), each patient had an average history of 2.00±3.07 (1 to 29) days of hospitalization. In terms of frequency of underlying diseases, 42.94% had cardiovascular disease, 15.85% had lung disease, 14.12% had kidney disease, 3.17% had rheumatology disease, 59.94% had hypertension, 37.75% had diabetes mellitus, 12.96% had cancer, and 11.24% had a history of cerebrovascular events. For habits, 10.09% used cigarettes, 7.78% used opium, and one person used alcohol. Regarding clinical symptoms, 28.53% had myalgia, 41.50% had a fever, 71.76% had respiratory symptoms, 49.28% had weakness and lethargy, 25.65% had digestive symptoms, 15.85% had a decreased level of consciousness, 5.76% had chest pain, and 3.46% had sweating.
The average admission time oxygen saturation percentage without supplemental oxygen was 88.63±7.36 (60 to 99%). Regarding receiving general medications, 93.66% took antibiotics, 94.81% took proton pump inhibitors, 63.69% took interferon, 68.59% took hydroxychloroquine, and 88.86% took corticosteroids. Also, 13.54% took tocilizumab (Actemra). For antiviral medications, 24.21% took favipiravir, 34.29% took remdesivir, 57.93% took sofosbuvir/daclatasvir, 20.46% took ledipasvir, 6.05% took lopinavir/ritonavir, and 5.48% took atazanavir/ritonavir.
Clinical
One hundred ninety-nine patients (57.35%) survived, and 148 patients (42.65%) died. The mean of LoS was 11.40±7.01 days, with the mean at the ward being 5.24±5.44 days and at the ICU 6.15±6.94 days.
Economic
The mean cost of a bed day was 35.41±32.03 dollars, with a right-skewed distribution (Table 1, Figure 1).
Table 1. Central and dispersion statistics for total bed-day cost of admission
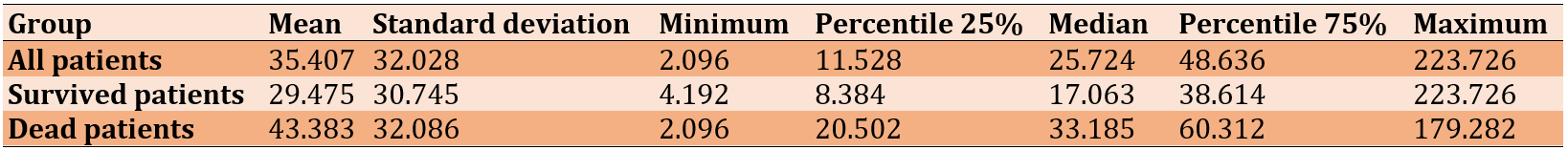
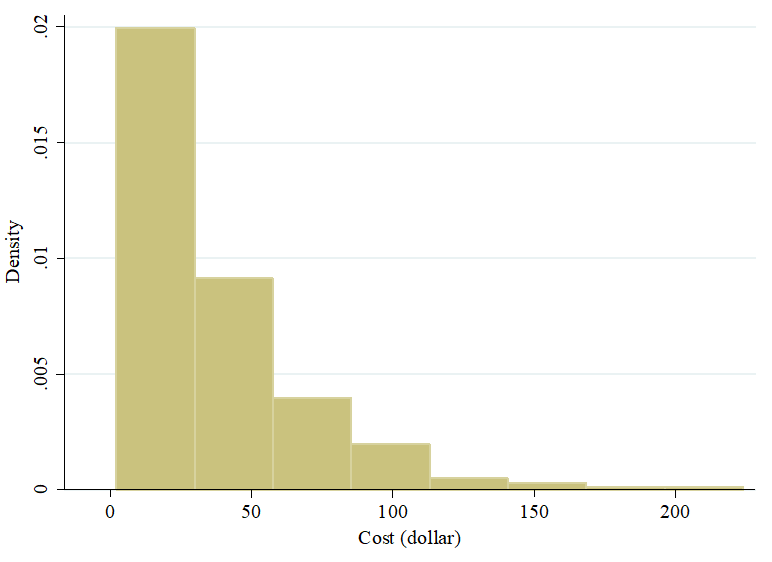
Figure 1. Histogram of total bed-day cost of admission
Total bed-day cost was compared between survived and dead patients (Figure 2). The difference in the median was 16.122 dollars. Based on the Mann-Whitney U test, dead patients had higher costs rank-wise (p<0.001).
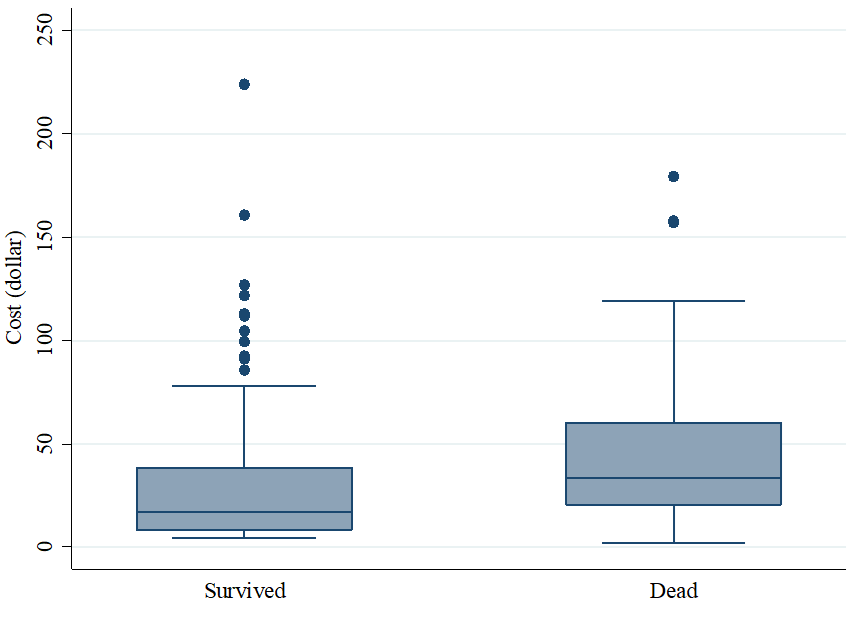
Figure 2. Box plot of total bed-day cost of admission divided by disease outcome
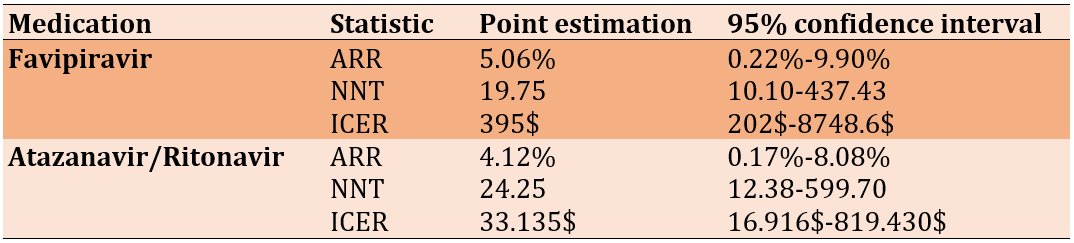
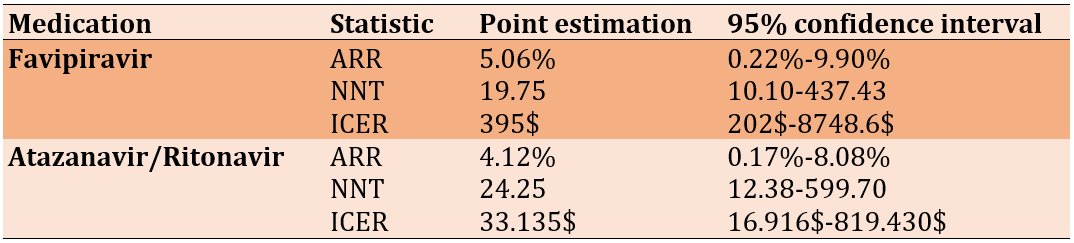
For antiviral drugs, cross-table analysis was performed for death outcomes in all possible conditions of drug-ward/ICU/total admission (not shown). Accordingly, favipiravir and atazanavir/ritonavir showed significant ARR at a 95% confidence interval in ward-admitted patients (Table 2).
Table 2. Economic evaluation of antivirals in reduction of death among ward admitted patients
LoS was compared between antiviral recipients and non-recipients among survived patients. No significant LoS reduction was observed, so ICER was not calculated.
Discussion
The present study was conducted to find the cost-effectiveness of COVID-19 management in old-aged patients in Iran, as our country has specific economic conditions. Regarding the cost-effectiveness of oral antiviral treatments, no antiviral medication was found to reduce mortality in ICU-admitted patients of our population. Two medications were found that had significant ARR in ward-admitted patients. Due to the approximate similar effectiveness of favipiravir and atazanavir/ritonavir and on the other hand, the lower cost of atazanavir/ritonavir, the more economical medication is suggested. However, considering these wide confidence intervals of NNTs and ICERs showing a wide range of uncertainty, we understand that our point estimations are not generalizable to the parameter of the population. Nevertheless, regarding the cost-effectiveness of hospitalization, the self-of hospitalization and ICU admission were helpful in indicated patients as bed-days cost was not high in Iran. In our culture, saving elderly lives is of spiritual importance for families. On the other hand, their hospitalization brings overall high costs for our government. In such conditions, increasing out-of-pocket payments may be a solution to make a balance between these two facts.
As we mentioned, saving the life of elderlies and improving their quality of life in Iranian culture is a value. Some studies in this regard were performed before the COVID-19 pandemic. Daddoust et al. investigated the vulnerability of the Iranian elderly in disasters as a qualitative study. They found that there were personal and social factors other than age that could affect this vulnerability to disasters [23]. Therefore, planning on these factors may be helpful and cos-effective.
The economic burden of COVID-19 is of great importance. Gaffari Darab et al.'s Iranian experience with 477 patients showed the direct and indirect costs of COVID-19. Their study included 100 (21%) of patients with an age of more than 65 [24]. However, there was no comparison between the costs of elderly patients and other age groups. In the present study, we directly calculated the costs of elderly patients.
A systematic review was performed by Rezapour et al. about the economic evaluation programs in COVID-19. They reviewed 23 studies based on the CHEERS checklist. Most studies have used the suspected-infected-recovered (SIR) model for outcomes. The most cost-effective actions were social distancing and screening tests. Only three studies had focused on treatment and vaccination [25]. In the present study, we investigated treatment in elderlies. In general, elderlies have always been noteworthy, even from the economic point of view as they are vulnerable and they have high mortality regarding COVID-19 [26]. Also, from the viewpoint of human rights, providing health and welfare for elderlies is necessary as most COVID-19 mortalities are at the age of 60 years and older [27].
Although we had some limitations, our study had enough novelty. During the literature search, we found no document investigating the health economics of COVID-19 in old people as a primary study. The most important limitation was that we did not have access to the patients who needed hospitalization, but they were not hospitalized, and this investigation was not ethically possible. Also, we did not have any control group from the younger population. In addition, we did not investigate the quality of life as an important factor in health economic studies. As a single-center study in a tertiary hospital, the study results are generalizable merely to our own population. Briefly, the hospitalization of old patients considerably costs our healthcare system. But ethically, we should admit all the patients who need admission. In order to generalize the results globally, further primary studies are needed. Then the evidence may be generalizable to any similar pandemic in the future.
Conclusion
A mean cost of 88.711$ is needed for the survival of one patient, assuming that all the ICU-needed patients would die if there was a lack of hospital admission. Considering all ward and ICU admitted patients, 44.854$ is needed to save one old patient's life assuming this logic.
Acknowledgement: The present paper was a part of the MD thesis of FT supported by Iran University of Medical Sciences.
Ethical permissions: This study was approved by the ethics committee of Iran University of Medical Sciences with registration number IR.IUMS.FMD.REC.1399.827.
Conflicts of Interest: There is no conflict of interest.
Authors contribution: Tavassoli F (First Author), Introduction Writer/Methodologist/Discussion Writer (30%); Aghabiklooei A (Second Author), Main or Assistant Researcher/Statistical Analyst (10%); Azimi M (Third Author), Methodologist/Assistant Researcher (10%); Baghai Wadji M (Fourth Author), Main Researcher/Discussion Writer (10%); Ahmadi SAY (Fifth Author) Methodologist/Assistant Researcher (10%); Ameri M (Sixth Author) Methodologist/Statistical Analyst (30%)
Funding/Support: Iran University of Medical Sciences
Like many other diseases, the coronavirus disease of 2019 (COVID-19) has a heavy burden on societies and healthcare systems [1-4]. The burden may be greater in developing countries [5]. The burden of COVID-19 is described as a “post-pandemic double burden”, meaning that it has an excessive burden on the health system for managing non-communicable diseases, resulting in a post-pandemic crisis [6].
Other than COVID-19, there will be other similar pandemics in the future. Therefore, it is critical to find an economic plan in such conditions. The experience of 28 countries showed that the COVID-19 pandemic was a shocking event manifesting weak points of governments. The key elements of highly effective country responses were to activate comprehensive responses, adapt health system capacity, preserve health system functions and resources, and reduce vulnerability [7]. For such challenges of the COVID-19 era, economic issues are of great importance. Decision-makers should reach flexible policies that regard economic and ethical issues [8-12].
It is essential to know whether the policies are cost-effective. COVID-19 hospitalization is not an exception and there are economic issues [13, 14]. Among the aspects of the COVID-19 burden, the economic burden of COVID-19 is considerable [3, 15, 16]. For instance, it should be clear whether hospitalization of old COVID-19 patients is helpful and cost-effective. In addition, many drugs used in the management of COVID-19 have unclear rules. COVID-19 is not the first example of a challenge in the treatment of old-aged patients. Senescence has always been a big challenge in health economics. Hence, economic issues are considered in managing elderly diseases [17]. Cost payment for elderlies is not necessarily harmful to the governments. In the US, more than one out of five more than 65-year-old Americans live in high-risk regions of COVID-19, and many of them rely on earnings. Therefore, it is considered economic insecurity [18]. It means that costs for old patients may result in the enhancement of public health in old populations. An editorial emphasized adequate social and medical support for older adults regarding COVID-19 [19].
Due to the controversies about the costs imposed on surveillance and the health system for treating old patients and patients with end-stage disease, the present health economic evaluation study was performed to find the cost-effectiveness of hospitalization and antiviral treatment of COVID-19 in old patients among Iranian cases.
Instrument and Methods
A health economic evaluation as a single-center primary study with a cross-sectional design was performed based on the Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) statement [20] in Firoozgar Hospital, Tehran, Iran, as a referral and tertiary center during the second half of 2020 through a simple random sampling. A health information system (HIS) was used for sampling and access to the data. All the hospitalized cases of COVID-19 at 65 years of age and more were eligible for the study. Confirmation of COVID-19 was through polymerase chain reaction (PCR) or typical involvement in chest computed tomography (CT) scan. The perspective of the study was from healthcare providers. The time horizon of the study was limited to the hospitalization period in which the health outcomes were the Length of Stay (LoS) in day and death as a binary outcome. Due to the limited time horizon, a discount rate was not used. This study was approved by the ethics committee of Iran University of Medical Sciences with registration number IR.IUMS.FMD.REC.1399.827.
Total bed-day costs during admission and the costs of antiviral medications were calculated. The costs were in Iranian Rials (IRR), which were converted to US dollars based on the integrated currency trading system of Iran (locally called NIMA) at the time of data analysis (May 2022). Thus, each dollar was considered to be 250000 IRR.
Cost-effectiveness was calculated using the Incremental Cost-Effectiveness Ratio (ICER). ICER was calculated as the following for death and LoS outcomes, respectively. For death outcomes, drugs with a significant absolute risk reduction (ARR) were eligible for ICER calculation. Calculation of ICER based on the Number Needed to Treat (NNT) has been previously used by other researchers [21, 22]. For LOS outcome, drugs with a significant decrease in LoS were eligible for ICER calculation. Stata14 (Stata Corp; USA) was used for data analysis.
Findings
Demographic
Of the admitted patients, 347 cases over 65 were selected for the study. 173 patients (49.86%) were in the age range of 65-74, 69 patients (31.41%) were in the age range of 75-84, and 65 patients (18.73%) were 85 and more. Sex-wise, 145 patients (41.79%) were female and 202 patients (58.21%) were male. 104 patients (29.97%) were admitted to the ward, and 243 patients (70.30%) were admitted to the ICU.
In terms of diagnosis method, 8 patients (2.31%) were diagnosed only by PCR, and the rest, in addition to the positive PCR in chest CT scan were involved by COVID-19. Among the people who had involvement in their CT scans, the average involvement score was 13.09±7.01 from 25. For the number of hospitalizations (for any reason), each patient had an average history of 2.00±3.07 (1 to 29) days of hospitalization. In terms of frequency of underlying diseases, 42.94% had cardiovascular disease, 15.85% had lung disease, 14.12% had kidney disease, 3.17% had rheumatology disease, 59.94% had hypertension, 37.75% had diabetes mellitus, 12.96% had cancer, and 11.24% had a history of cerebrovascular events. For habits, 10.09% used cigarettes, 7.78% used opium, and one person used alcohol. Regarding clinical symptoms, 28.53% had myalgia, 41.50% had a fever, 71.76% had respiratory symptoms, 49.28% had weakness and lethargy, 25.65% had digestive symptoms, 15.85% had a decreased level of consciousness, 5.76% had chest pain, and 3.46% had sweating.
The average admission time oxygen saturation percentage without supplemental oxygen was 88.63±7.36 (60 to 99%). Regarding receiving general medications, 93.66% took antibiotics, 94.81% took proton pump inhibitors, 63.69% took interferon, 68.59% took hydroxychloroquine, and 88.86% took corticosteroids. Also, 13.54% took tocilizumab (Actemra). For antiviral medications, 24.21% took favipiravir, 34.29% took remdesivir, 57.93% took sofosbuvir/daclatasvir, 20.46% took ledipasvir, 6.05% took lopinavir/ritonavir, and 5.48% took atazanavir/ritonavir.
Clinical
One hundred ninety-nine patients (57.35%) survived, and 148 patients (42.65%) died. The mean of LoS was 11.40±7.01 days, with the mean at the ward being 5.24±5.44 days and at the ICU 6.15±6.94 days.
Economic
The mean cost of a bed day was 35.41±32.03 dollars, with a right-skewed distribution (Table 1, Figure 1).
Table 1. Central and dispersion statistics for total bed-day cost of admission
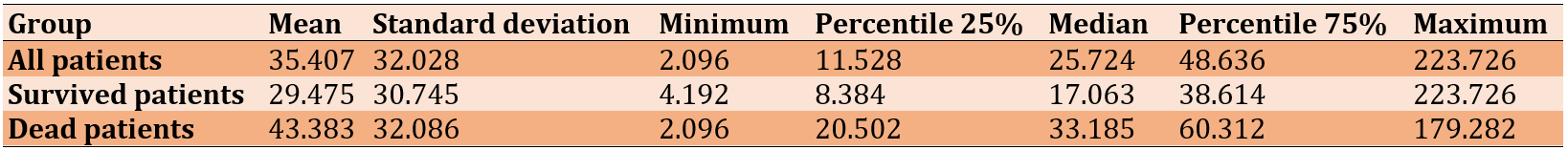
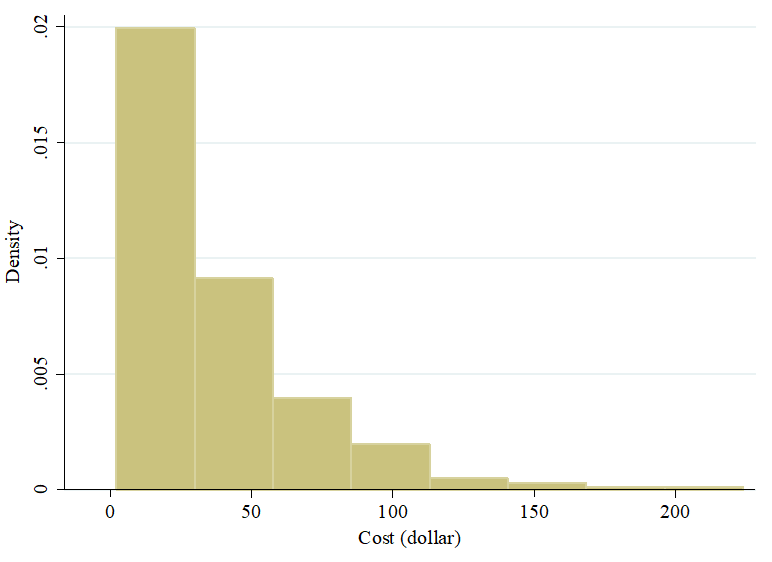
Figure 1. Histogram of total bed-day cost of admission
Total bed-day cost was compared between survived and dead patients (Figure 2). The difference in the median was 16.122 dollars. Based on the Mann-Whitney U test, dead patients had higher costs rank-wise (p<0.001).
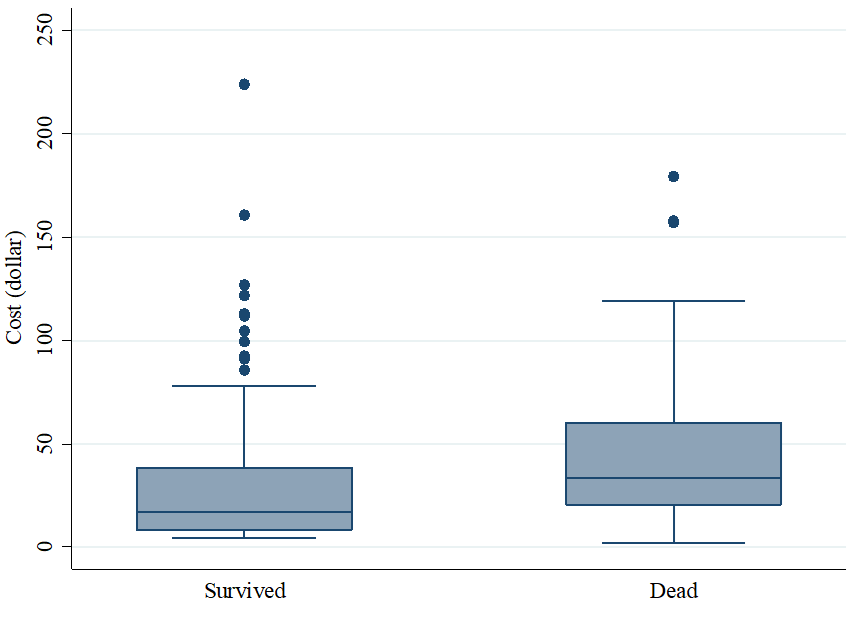
Figure 2. Box plot of total bed-day cost of admission divided by disease outcome
For antiviral drugs, cross-table analysis was performed for death outcomes in all possible conditions of drug-ward/ICU/total admission (not shown). Accordingly, favipiravir and atazanavir/ritonavir showed significant ARR at a 95% confidence interval in ward-admitted patients (Table 2).
Table 2. Economic evaluation of antivirals in reduction of death among ward admitted patients
LoS was compared between antiviral recipients and non-recipients among survived patients. No significant LoS reduction was observed, so ICER was not calculated.
Discussion
The present study was conducted to find the cost-effectiveness of COVID-19 management in old-aged patients in Iran, as our country has specific economic conditions. Regarding the cost-effectiveness of oral antiviral treatments, no antiviral medication was found to reduce mortality in ICU-admitted patients of our population. Two medications were found that had significant ARR in ward-admitted patients. Due to the approximate similar effectiveness of favipiravir and atazanavir/ritonavir and on the other hand, the lower cost of atazanavir/ritonavir, the more economical medication is suggested. However, considering these wide confidence intervals of NNTs and ICERs showing a wide range of uncertainty, we understand that our point estimations are not generalizable to the parameter of the population. Nevertheless, regarding the cost-effectiveness of hospitalization, the self-of hospitalization and ICU admission were helpful in indicated patients as bed-days cost was not high in Iran. In our culture, saving elderly lives is of spiritual importance for families. On the other hand, their hospitalization brings overall high costs for our government. In such conditions, increasing out-of-pocket payments may be a solution to make a balance between these two facts.
As we mentioned, saving the life of elderlies and improving their quality of life in Iranian culture is a value. Some studies in this regard were performed before the COVID-19 pandemic. Daddoust et al. investigated the vulnerability of the Iranian elderly in disasters as a qualitative study. They found that there were personal and social factors other than age that could affect this vulnerability to disasters [23]. Therefore, planning on these factors may be helpful and cos-effective.
The economic burden of COVID-19 is of great importance. Gaffari Darab et al.'s Iranian experience with 477 patients showed the direct and indirect costs of COVID-19. Their study included 100 (21%) of patients with an age of more than 65 [24]. However, there was no comparison between the costs of elderly patients and other age groups. In the present study, we directly calculated the costs of elderly patients.
A systematic review was performed by Rezapour et al. about the economic evaluation programs in COVID-19. They reviewed 23 studies based on the CHEERS checklist. Most studies have used the suspected-infected-recovered (SIR) model for outcomes. The most cost-effective actions were social distancing and screening tests. Only three studies had focused on treatment and vaccination [25]. In the present study, we investigated treatment in elderlies. In general, elderlies have always been noteworthy, even from the economic point of view as they are vulnerable and they have high mortality regarding COVID-19 [26]. Also, from the viewpoint of human rights, providing health and welfare for elderlies is necessary as most COVID-19 mortalities are at the age of 60 years and older [27].
Although we had some limitations, our study had enough novelty. During the literature search, we found no document investigating the health economics of COVID-19 in old people as a primary study. The most important limitation was that we did not have access to the patients who needed hospitalization, but they were not hospitalized, and this investigation was not ethically possible. Also, we did not have any control group from the younger population. In addition, we did not investigate the quality of life as an important factor in health economic studies. As a single-center study in a tertiary hospital, the study results are generalizable merely to our own population. Briefly, the hospitalization of old patients considerably costs our healthcare system. But ethically, we should admit all the patients who need admission. In order to generalize the results globally, further primary studies are needed. Then the evidence may be generalizable to any similar pandemic in the future.
Conclusion
A mean cost of 88.711$ is needed for the survival of one patient, assuming that all the ICU-needed patients would die if there was a lack of hospital admission. Considering all ward and ICU admitted patients, 44.854$ is needed to save one old patient's life assuming this logic.
Acknowledgement: The present paper was a part of the MD thesis of FT supported by Iran University of Medical Sciences.
Ethical permissions: This study was approved by the ethics committee of Iran University of Medical Sciences with registration number IR.IUMS.FMD.REC.1399.827.
Conflicts of Interest: There is no conflict of interest.
Authors contribution: Tavassoli F (First Author), Introduction Writer/Methodologist/Discussion Writer (30%); Aghabiklooei A (Second Author), Main or Assistant Researcher/Statistical Analyst (10%); Azimi M (Third Author), Methodologist/Assistant Researcher (10%); Baghai Wadji M (Fourth Author), Main Researcher/Discussion Writer (10%); Ahmadi SAY (Fifth Author) Methodologist/Assistant Researcher (10%); Ameri M (Sixth Author) Methodologist/Statistical Analyst (30%)
Funding/Support: Iran University of Medical Sciences
Keywords:
References
1. Smith Jervelund S, Eikemo TA. The double burden of COVID-19. Scand J Public Health. 2021;49(1):1-4. [Link] [DOI:10.1177/1403494820984702]
2. Khan JR, Awan N, Islam MM, Muurlink O. Healthcare capacity, health expenditure, and civil society as predictors of COVID-19 case fatalities: a global analysis. Front Public Health. 2020;8:347. [Link] [DOI:10.3389/fpubh.2020.00347]
3. Di Fusco M, Shea KM, Lin J, Nguyen JL, Angulo FJ, Benigno M, et al. Health outcomes and economic burden of hospitalized COVID-19 patients in the United States. J Med Econ. 2021;24(1):308-17. [Link] [DOI:10.1080/13696998.2021.1886109]
4. Bisht R, Saharia R, Sarma J. COVID-19 and the burden of ill-health: a double crisis of disruptions and inequalities. J Soc Econ Dev. 2021;23:342-56. [Link] [DOI:10.1007/s40847-020-00117-x]
5. Levin AT, Owusu-Boaitey N, Pugh S, Fosdick BK, Zwi AB, Malani A, et al. Assessing the burden of COVID-19 in developing countries: systematic review, meta-analysis and public policy implications. BMJ Glob Health. 2022;7(5):e008477. [Link] [DOI:10.1136/bmjgh-2022-008477]
6. Chan AHY, Horne R. Preventing a post-pandemic double burden of disease in the COVID-19 pandemic. Glob Adv Health Med. 2021;10:21649561211010137. [Link] [DOI:10.1177/21649561211010137]
7. Haldane V, De Foo C, Abdalla SM, Jung A-S, Tan M, Wu S, et al. Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries. Nat Med. 2021;27(6):964-80. [Link] [DOI:10.1038/s41591-021-01381-y]
8. Reddy SG. Population health, economics and ethics in the age of COVID-19. BMJ Glob Health. 2020;5(7):e003259. [Link] [DOI:10.1136/bmjgh-2020-003259]
9. Figari F, Fiorio C. Welfare resilience in the immediate aftermath of the COVID-19 outbreak in Italy. Covid Economics. 2020;2020(8):106-33. [Link] [DOI:10.4324/9781003095590-7]
10. Herron TL, Manuel T. Ethics of US government policy responses to the COVID‐19 pandemic: A utilitarianism perspective. Business Soc Rev. 2022;127(51):343-67. [Link] [DOI:10.1111/basr.12259]
11. Hodges R, Caperchione E, Van Helden J, Reichard C, Sorrentino D. The role of scientific expertise in COVID-19 policy-making: evidence from four European countries. Public Organization Rev. 2022;22(2):249-67. [Link] [DOI:10.1007/s11115-022-00614-z]
12. Mazza M, Attanasio M, Pino MC, Masedu F, Tiberti S, Sarlo M, Valenti M. Moral decision-making, stress, and social cognition in frontline workers vs. population groups during the COVID-19 pandemic: An explorative study. Frontiers in psychology. 2020;11:588159. [Link] [DOI:10.3389/fpsyg.2020.588159]
13. Sheinson D, Dang J, Shah A, Meng Y, Elsea D, Kowal S. A cost-effectiveness framework for COVID-19 treatments for hospitalized patients in the United States. Adv Ther. 2021;38(4):1811-31. [Link] [DOI:10.1007/s12325-021-01654-5]
14. Li B, Chen L, Shi L. Determinants of Hospitalization Costs among Moderate Cases of COVID-19. INQUIRY. 2022;59:00469580211059483. [Link] [DOI:10.1177/00469580211059483]
15. Richards F, Kodjamanova P, Chen X, Li N, Atanasov P, Bennetts L, et al. Economic burden of COVID-19: A systematic review. Clinicoecon Outcomes Res. 2022:293-307. [Link] [DOI:10.2147/CEOR.S338225]
16. Kolbin A, Belousov DY, Gomon YM, Balykina YE, Ivanov I. Socio-economic burden of COVID-19 in the Russian Federation. Value Health. 2020;23:S556. [Link] [DOI:10.1016/j.jval.2020.08.906]
17. Coast J, Flynn T, Sutton E, Al-Janabi H, Vosper J, Lavender S, et al. Investigating Choice Experiments for Preferences of Older People (ICEPOP): Evaluative spaces in health economics. J Health Services Res Policy. 2008;13(3 suppl):31-7. [Link] [DOI:10.1258/jhsrp.2008.008024]
18. Li Y, Mutchler JE. Older adults and the economic impact of the COVID-19 pandemic. J Aging Soc Policy. 2020;32(4-5):477-87. [Link] [DOI:10.1080/08959420.2020.1773191]
19. Kar N. COVID-19 and older adults: In the face of a global disaster. J Geriatric Care and Res. 2020;7(1):1-2. [Link]
20. Husereau D, Drummond M, Augustovski F, de Bekker-Grob E, Briggs AH, Carswell C, et al. Consolidated health economic evaluation reporting standards (CHEERS) 2022 explanation and elaboration: A report of the ISPOR CHEERS II Good Practices Task Force. Value in Health. 2022;25(1):10-31. [Link] [DOI:10.1016/j.jval.2021.10.008]
21. Weiss M, Grom F, Porzsolt F. Costs of additional treatment success (COATS) based on numbers needed to treat (NNT) is a simplified calculation method to facilitate physicians medical decisions with regards to monetary costs. Br J Med Medical Res. 2012;2(4):636. [Link] [DOI:10.9734/BJMMR/2012/1379]
22. Boonacker CW, van der Veen EL, van der Wilt GJ, Schilder AG, Rovers MM. Trimethoprim-sulfamethoxazole in children with chronic otitis media: A randomized comparison of costs and effects. Otol Neurotol. 2008;29(7):961-4. [Link] [DOI:10.1097/MAO.0b013e3181859a66]
23. Daddoust L, Khankeh H, Ebadi A, Sahaf R, Nakhaei M, Asgary A. The vulnerability of the Iranian elderly in disasters: Qualitative content analysis. Iran J Nurs Midwifery Res. 2018;23(5):402-8. [Link] [DOI:10.4103/ijnmr.IJNMR_127_17]
24. Ghaffari Darab M, Keshavarz K, Sadeghi E, Shahmohamadi J, Kavosi Z. The economic burden of coronavirus disease 2019 (COVID-19): Evidence from Iran. BMC Health Serv Res. 2021;21(1):1-7. [Link] [DOI:10.1186/s12913-021-06126-8]
25. Rezapour A, Souresrafil A, Peighambari MM, Heidarali M, Tashakori-Miyanroudi M. Economic evaluation of programs against COVID-19: A systematic review. Int J Surg. 2021;85:10-8. [Link] [DOI:10.1016/j.ijsu.2020.11.015]
26. Panneer S, Kantamaneni K, Palaniswamy U, Bhat L, Pushparaj RRB, Nayar KR, et al. Health, Economic and Social Development Challenges of the COVID-19 Pandemic: Strategies for Multiple and Interconnected Issues. Healthcare (Basel). 2022;10(5):770. [Link] [DOI:10.3390/healthcare10050770]
27. Baidhowi AD. Human Rights for The Elderly Group in Indonesia: Elderly in The Era of Covid 19. NEGREI. 2022;2(1):23-34. [Link] [DOI:10.29240/negrei.v2i1.3629]









