Volume 15, Issue 4 (2023)
Iran J War Public Health 2023, 15(4): 375-380 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2023/10/27 | Accepted: 2023/12/6 | Published: 2023/12/19
Received: 2023/10/27 | Accepted: 2023/12/6 | Published: 2023/12/19
How to cite this article
Vafadar Z, Javadzade H, Behzadnia M, Moayed M. Effects of Interdisciplinary Education about War Victim Triage on Knowledge and Practice of Healthcare Science Students. Iran J War Public Health 2023; 15 (4) :375-380
URL: http://ijwph.ir/article-1-1408-en.html
URL: http://ijwph.ir/article-1-1408-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
1- “Health Management Research Center” and “Department of Medical-Surgical, Faculty of Nursing”, Baqiyatallah University of Medical Sciences, Tehran, Iran
2- “Trauma Research Center” and “Department of Emergency Medicine, Faculty of Medicine”, Baqiyatallah University of Medical Sciences, Tehran, Iran
3- “Trauma Research Center, Clinical Sciences Institute” and “Faculty of Nursing”, Baqiyatallah University of Medical Sciences, Tehran, Iran
2- “Trauma Research Center” and “Department of Emergency Medicine, Faculty of Medicine”, Baqiyatallah University of Medical Sciences, Tehran, Iran
3- “Trauma Research Center, Clinical Sciences Institute” and “Faculty of Nursing”, Baqiyatallah University of Medical Sciences, Tehran, Iran
Full-Text (HTML) (597 Views)
Introduction
Triage is the first step in care provision for war and disaster victims. Derived from the French term “trier,” triage was first used by a French surgeon during the war and refers to resource allocation or rationing [1]. In war, triage refers to prioritizing victims for healthcare services based on injury severity, prognosis, available resources, and extent of mass casualties. Its results are used to prioritize victim transfer to healthcare settings. This prioritization system is an essential and undeniable necessity in war conditions [2]. The enormous destructive power of modern weapons and rapid changes in war missions require healthcare providers to provide healthcare services to many victims, even under enemy fire [3]. In such conditions, triage is a dynamic time- and place-dependent process for resuscitation and care provision [4]. According to the aim, condition, place, available equipment, and competencies of the involved staff, triage is classified into different types, including triage in war, a subcategory of triage in crisis. The primary and most important method for triage in war is the START pattern, a simple and rapid method based on the four colors red, yellow, green, and black. Triage in war may differ based on the attack's type and extent [5].
Effective triage can reduce complications and mortality rates. A study reported that during World Wars I and II, the Vietnam War, the Korean War, and the Persian Gulf War, triage reduced the mortality rate from 5% in World War II to 1% in the Vietnam War [6]. On the other hand, ineffective triage is associated with many different consequences. For example, it wastes resources and leads to serious complications and even death. A study showed that 25% of the victims of an attack died despite low injury severity scores and limited injuries to their vital organs [7].
Triage in war zones is usually performed by physicians, nurses, and other healthcare providers [8]. Nonetheless, most physicians and nurses in war zones have no previous experience of war conditions [9]. Studies into the triage-related knowledge and practice of nurses revealed that most had limited knowledge about triage. For example, a study showed that 52% of nurses could not accurately perform triage [10]. A study into the prehospital challenges of military missions in France also reported the lengthiness of the time of victim evacuation and transfer, the inadequacy of experienced physicians and nurses, and the need for adequate equipment and long-term education as the most important challenges in this area [11].
Triage staff’s limited knowledge about triage highlights education as a very important intervention to reduce mortality and improve survival among war victims [12, 13]. Moreover, while effective triage in war zones needs a coherent and systematic interdisciplinary approach to address victims’ needs appropriately, evidence shows that most healthcare providers do not have the necessary ability and skills to play their professional roles in interdisciplinary teams, and hence, education is essential to manage these problems [13].
Interdisciplinary education (IDE) is an educational approach that prepares healthcare providers to provide better care to their clients in a participatory atmosphere. A qualitative study into the non-technical competencies affecting healthcare teams in disasters reported that the most important competencies in this area were the ability to establish interpersonal and interprofessional communication, the ability to lead teams, the ability to manage conflicts, flexibility, responsibility, the physical and mental self-care, and interdisciplinary collaboration [14]. According to the World Health Organization, educational programs for nurses need to use interdisciplinary approaches and focus on the development of competencies such as effective interpersonal and interprofessional communication, interdisciplinary team leadership, problem-solving, decision-making in challenging ethical and legal situations, critical thinking, conflict management, prioritization for service provision, commitment to protect the safety of individuals and families, and care provision based on scientific standards [15, 16].
IDE is associated with many different positive outcomes such as improvement of staff motivation, reciprocal understanding, respect, and confidence, improvement of interprofessional collaboration and interactions, enhancement of job satisfaction, improvement of educational dynamicity, greater attention to the needs of healthcare clients, and their caregivers, improvement of care quality, better respect for the integrity and contribution of each discipline, and better learning of healthcare providers from, with, and about each other [17, 18]. In the mixed-method study, researchers demonstrated that interdisciplinary education increases awareness of team members’ roles, enhances communication and collaboration, and can lead to better care for COVID-19 patients [19]. Another study explained that interdisciplinary education could lead to highly coordinated and effective patient care in healthcare settings [20]. Moreover, a study found that IDE promoted positive learning among military staff and nursing and paramedic students [13].
However, most crisis management programs do not adequately address these competencies [14]. An integrative review of 190 articles on the most effective educational approaches to improve nursing students’ crisis management abilities reported IDE and simulation as the best educational methods. Still, more rigorous research is needed in this area since all published articles lacked methodologies, especially in data collection and analysis. Disaster preparedness education was a suitable activity for interprofessional education [21]. Furthermore, based on a meta-analysis, Cherney et al. recommend conducting more research with different experimental methodologies on Online Learner Collaboration between multidiscipline groups to gather practical suggestions for online course instructors and students [22].
One of the key topics in teaching and learning is micro-learning. Micro-learning supports learning in more easily accessible bites of information productively designed online. Therefore, professors, educators, and researchers must be responsible for using this learning method because of its extensive benefits to help students learn better in the right direction [23, 24].
Ball et al., in a study, showed that students who viewed the video podcast showed significant improvement in knowledge; furthermore, their confidence in responding to violence significantly improved [25]. Another study confirmed that educational intervention by SMS significantly increased nurses' knowledge and practice toward clinical guidelines for PIVC placement [26]. In a scoping review, researchers demonstrated that microlearning as an educational strategy has a positive effect on the knowledge and confidence of health profession students in performing procedures and engaging in collaborative learning [27].
Despite the well-known effectiveness of online micro-learning and IDE on different healthcare-related outcomes, there is limited information about their concurrent effects on healthcare providers’ and students’ knowledge and practice respecting triage in war. Researchers did not find a study that was conducted in scope. On the other hand, the nature of war is very different from other crises. Therefore, this study aimed to evaluate the effects of OMIDE on war victim triage on triage-related knowledge and practice of healthcare science students.
Materials and Methods
This quasi-experimental study was conducted in 2021 with a single-group pretest-posttest design. Participants were eighty male students from the three fields of medicine (n=50), nursing (n=20), and medical emergencies (n=10) selected from Baqiyatallah University of Medical Sciences, Iran. Because all eligible students were male, the sampling was done with the males. Inclusion criteria were an agreement for participation and having passed the Emergency Care theoretical course, which included triage. Accordingly, third- and fourth-year medical students, third-year nursing students, and second-year medical emergency students were eligible for the study. Exclusion criteria were participation in any other similar educational program on triage, reluctance to stay in the study, irregular attendance at the intervention sessions, and loss to follow-up at the posttest. Sampling was purposively performed online because educational activities at universities were performed online during the study due to the coronavirus disease 2019 pandemic. Accordingly, ten interdisciplinary WhatsApp groups were created and participants were randomly allocated. Each group consisted of five medical students, two nursing students, and one medical emergency student. Based on Altman’s nomogram, the sample size was calculated to be 75. Sample size calculation parameters were a confidence level of 0.95, a power of 0.90, and an effect size reported in a previous study [28]. Considering a probable withdrawal rate of 5%, the sample size was increased to 78, and finally, 80 students were recruited for the study.
A demographic questionnaire, a war victim triage knowledge questionnaire, and six scenarios about war victim triage practice were used for data collection. The items of the demographic questionnaire were on age and field of education. The war victim triage knowledge questionnaire had thirteen multiple-choice questions, each with only one correct answer. The total score of the questionnaire was 20. This questionnaire was developed through the modified Delphi technique, in which three experts in military medicine and two experts in emergency medicine from military medical universities were invited to formulate questions to assess students’ knowledge about war victim triage. Their questions were assessed and discussed in a single online session consisting of the study authors, military medicine experts, and emergency medicine experts, and questions with the greatest agreement were included in the final questionnaire. The content validity of the questionnaire was assessed by experts in military medicine, emergency medicine, and disaster care selected from Artesh University of Medical Sciences and the University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. All questionnaire items obtained a content validity ratio and index of more than 0.80 and 0.89, respectively. For reliability assessment, fifteen students external to the study twice completed this questionnaire with a two-week interval Cronbach’s alpha was calculated to be 0.92, and inter-class correlation coefficient was 0.94.
To develop the scenarios for assessing participants’ practice respecting war victim triage, twenty experts in military medicine and emergency medicine from military universities of medical sciences in Tehran, Iran, were asked through email to propose ten scenarios with appropriate evaluation questions. They were asked to develop the scenarios using a patient management problem (PMP) format. PMP simulates a real clinical situation in which a healthcare provider faces a patient or victim. Accordingly, the healthcare provider needs to assess the patient’s condition and decide upon the most appropriate interventions. Then, the healthcare provider receives a series of measures that may be useful, non-useful, or even harmful and contraindicated for that clinical situation and should select the best measures to manage that situation. Accordingly, his/her practice is evaluated using seven criteria. During a two-week interval, seven experts provided their scenarios. Then, a panel of seven experts from military medical universities evaluated the scenarios and their corresponding questions, and six scenarios were selected. Scenarios were about triage in chemical, biological, radiological, and nuclear attacks, aerial triage, ethics in triage, field hospital triage, hospital triage, and battlefield triage. For validity assessment, ten military and emergency medicine experts were invited through email to comment on the scenarios. Then the scenarios' content validity ratio and index were calculated to be 0.79 and 0.87, respectively. The Cronbach’s alpha and the test-retest intraclass correlation coefficient of the scenarios were also 0.84 and 0.80, respectively. The total possible score of the scenarios was between –107 and +140.
The study intervention was video-based micro-learning education about war victim triage. Videos were created by an emergency medicine expert with great military medicine experience. Videos were recorded in an audiovisual service center by an expert in creating educational videos. Videos and study instruments were uploaded to a virtual education system, and a personal account was created for each participant. Through the WhatsApp groups, participants were provided with clear explanations about the study intervention, how to answer the study instruments, and how to collaborate and consult with other group members for appropriate triage. Initially, participants completed the study's informed consent form and answered the knowledge questionnaire in ten minutes. Then, the scenarios were provided to them to watch and answer their corresponding questions. Participants in each group could interact with each other and discuss the scenarios to choose the best answers to the scenario questions. They finally answered the questions after reaching a group agreement. After that, the educational videos were provided to them in ninety minutes through a virtual education system. Participants could watch each video just once. Educational materials were about triage on the battlefield, chemical-microbial attacks, triage under fire, triage in field hospitals, aerial triage, and ethics in triage, respectively. Immediately and one month after the intervention, participants re-completed the knowledge questionnaire and answered the questions of the scenario.
The SPSS 22 software was used for data analysis. The Kolmogorov-Smirnov test revealed the normal distribution of the study variables (p>0.05). Accordingly, the data were described through the measures of descriptive statistics and were analyzed through the repeated measures analysis of variance.
Findings
Participants were 50 medical students (62.5%), 20 nursing students (25%), and 10 medical emergency students (12.5%). The mean of participants’ age was 23.07±1.51 years in total, 23.23±0.86 years for medical students, 23.05±2.6 years for nursing students, and 22.22±0.97 years for medical emergencies students (p=0.182).
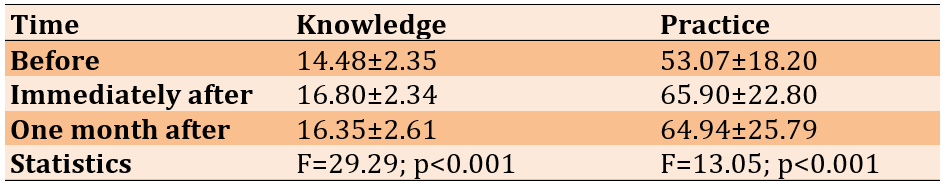
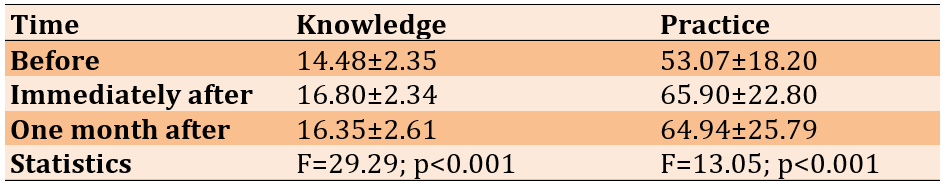
The repeated measures analysis of variance showed significant differences in the mean scores of knowledge and practice respecting war victim triage across the three measurement time points (p<0.001; Table 1).
Table 1. Within-group comparison (repeated measures analysis of variance) respecting the mean scores of triage-related knowledge and practice across the three measurement time points
Discussion
This study aimed to evaluate the effects of OMIDE about war victim triage on triage-related knowledge and practice of healthcare science students. Findings revealed that students had poor knowledge and practice respecting war victim triage, and OMIDE significantly improved their knowledge and practice. A study in line with our findings showed that triage education through iterative multi-manikin simulation significantly increased students’ triage abilities and efficiency [29]. Another study showed that the students' satisfaction scores for simulation-based triage training, awareness, clinical decision-making, team communication, staff safety, and skills were high. Simulation-based training can be used to improve the triage skills of undergraduate students. In addition, it concluded that this training should be supported in graduate programs because of their lower performance in some triage categories [30].
Moreover, a study reported the significant positive effects of simulation-based education on the ability to perform triage [31] and the learning experiences of students [32]. Another study into the educational needs of aerial evacuation clinicians in the United States showed that simulation-based education about oxygen therapy, negative pressure wound management, and care provision to populations with special needs, such as patients with burn injuries, had the potential to improve the competencies for triage and aerial transfer of victims [33].
Managing the scene and the injured in CBRNE incidents was one of the designed scenarios. A study in line with our study emphasizes that preparation and delivery of training are important requirements for sending training healthcare teams to CBRNE scenes [34]. A study found that communication and mutual awareness among participants led to better teamwork. The lessons provided in the course enabled a suitable level of competence in CBRN matters, which was necessary for analyzing all aspects of CBRN events in an exercise [35].
The most important attribute of our educational intervention was participants’ interactions and learning in interdisciplinary groups. Several other studies also revealed the significant positive effects of interdisciplinary approaches on participants’ abilities to respond to crises, their respect for other professional groups involved in crisis management, and their teamwork and interdisciplinary collaboration [36, 37]. A study confirmed that Interprofessional crisis management education brings together professional groups involved in a crisis, empowering military nurses to collaborate effectively and enhancing their ability to cope with different crises [17].
Of course, evaluation in those studies was face-to-face, while evaluation in the present study was web-based. Moreover, the interventions of those studies lasted from several days to nine months, while our intervention was around two hours. Contrary to our findings, a study found that after a simulation-based disaster-related education, students still had cognitive and functional problems respecting inter-professional collaboration, understanding of each other’s roles and responsibilities, teamwork, conflict management, and client-centeredness and hence, recommended the necessity of integrating inter-professional competencies into disaster management educational programs [38].
OMIDE, through interdisciplinary groups in the present study, allowed students to interact and collaborate, discuss triage conditions, and make the best triage-related decisions in different simulated war situations. In line with our findings, a study reported education type as a factor significantly affecting the collaboration and performance of military forces and healthcare providers [13]. Moreover, another study found that web-based education also significantly improved the ability of emergency medical staff to manage eye injuries in chemical wars [39]. Virtual training with dynamic virtual patients effectively trains healthcare teams in managing mass-casualty incidents, especially for uncommon incidents [40]. Micro-learning can effectively promote and retain knowledge of trauma care and increase nursing students' satisfaction. It is suggested as a new educational approach that can complement or replace traditional methods in conveying important concepts [41].
Traditional educational programs face difficulty retaining knowledge after the course is over due to the forgetting curve. However, our study found that learning remained stable a month after the intervention, with no significant difference in scores of students' knowledge and practice.
Among the strengths of the present study were modern educational approaches, the use of micro learning, virtual education, interdisciplinary groups, PMP, and clinical reasoning in triage. The study's limitations were the lack of a control group and the greater number of medical students in the study sample. All of the students were male because of the nature of the military university context.
Conclusion
Online micro-learning interdisciplinary education about war victim triage has positive effects on interactions and clinical reasoning in the knowledge and practice of healthcare science students regarding war victim triage.
Acknowledgements: Thanks for the support, guidance, and advice from the “Clinical Research Development Unit of Baqiyatallah Hospital." The authors hereby extend their gratitude to all students who participated in this study and appreciate it.
Ethical Permissions: IR.BMSU.BAQ.REC.1399.006
Conflicts of Interests: The authors declare that the research was conducted without any commercial or financial relationships that could be construed as a potential conflict of interest.
Authors’ Contribution: Vafadar Z (First Author), Methodologist/Assistant Researcher/Statistical Analyst (25%); Javadzadeh H (Second Author), Introduction Writer/Methodologist/Assistant Researcher (25%); Behzadnia MJ (Third Author), Discussion Writer (10%); Moayed MS (Fourth Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (40%)
Funding/Support: No funding was received for this study.
Triage is the first step in care provision for war and disaster victims. Derived from the French term “trier,” triage was first used by a French surgeon during the war and refers to resource allocation or rationing [1]. In war, triage refers to prioritizing victims for healthcare services based on injury severity, prognosis, available resources, and extent of mass casualties. Its results are used to prioritize victim transfer to healthcare settings. This prioritization system is an essential and undeniable necessity in war conditions [2]. The enormous destructive power of modern weapons and rapid changes in war missions require healthcare providers to provide healthcare services to many victims, even under enemy fire [3]. In such conditions, triage is a dynamic time- and place-dependent process for resuscitation and care provision [4]. According to the aim, condition, place, available equipment, and competencies of the involved staff, triage is classified into different types, including triage in war, a subcategory of triage in crisis. The primary and most important method for triage in war is the START pattern, a simple and rapid method based on the four colors red, yellow, green, and black. Triage in war may differ based on the attack's type and extent [5].
Effective triage can reduce complications and mortality rates. A study reported that during World Wars I and II, the Vietnam War, the Korean War, and the Persian Gulf War, triage reduced the mortality rate from 5% in World War II to 1% in the Vietnam War [6]. On the other hand, ineffective triage is associated with many different consequences. For example, it wastes resources and leads to serious complications and even death. A study showed that 25% of the victims of an attack died despite low injury severity scores and limited injuries to their vital organs [7].
Triage in war zones is usually performed by physicians, nurses, and other healthcare providers [8]. Nonetheless, most physicians and nurses in war zones have no previous experience of war conditions [9]. Studies into the triage-related knowledge and practice of nurses revealed that most had limited knowledge about triage. For example, a study showed that 52% of nurses could not accurately perform triage [10]. A study into the prehospital challenges of military missions in France also reported the lengthiness of the time of victim evacuation and transfer, the inadequacy of experienced physicians and nurses, and the need for adequate equipment and long-term education as the most important challenges in this area [11].
Triage staff’s limited knowledge about triage highlights education as a very important intervention to reduce mortality and improve survival among war victims [12, 13]. Moreover, while effective triage in war zones needs a coherent and systematic interdisciplinary approach to address victims’ needs appropriately, evidence shows that most healthcare providers do not have the necessary ability and skills to play their professional roles in interdisciplinary teams, and hence, education is essential to manage these problems [13].
Interdisciplinary education (IDE) is an educational approach that prepares healthcare providers to provide better care to their clients in a participatory atmosphere. A qualitative study into the non-technical competencies affecting healthcare teams in disasters reported that the most important competencies in this area were the ability to establish interpersonal and interprofessional communication, the ability to lead teams, the ability to manage conflicts, flexibility, responsibility, the physical and mental self-care, and interdisciplinary collaboration [14]. According to the World Health Organization, educational programs for nurses need to use interdisciplinary approaches and focus on the development of competencies such as effective interpersonal and interprofessional communication, interdisciplinary team leadership, problem-solving, decision-making in challenging ethical and legal situations, critical thinking, conflict management, prioritization for service provision, commitment to protect the safety of individuals and families, and care provision based on scientific standards [15, 16].
IDE is associated with many different positive outcomes such as improvement of staff motivation, reciprocal understanding, respect, and confidence, improvement of interprofessional collaboration and interactions, enhancement of job satisfaction, improvement of educational dynamicity, greater attention to the needs of healthcare clients, and their caregivers, improvement of care quality, better respect for the integrity and contribution of each discipline, and better learning of healthcare providers from, with, and about each other [17, 18]. In the mixed-method study, researchers demonstrated that interdisciplinary education increases awareness of team members’ roles, enhances communication and collaboration, and can lead to better care for COVID-19 patients [19]. Another study explained that interdisciplinary education could lead to highly coordinated and effective patient care in healthcare settings [20]. Moreover, a study found that IDE promoted positive learning among military staff and nursing and paramedic students [13].
However, most crisis management programs do not adequately address these competencies [14]. An integrative review of 190 articles on the most effective educational approaches to improve nursing students’ crisis management abilities reported IDE and simulation as the best educational methods. Still, more rigorous research is needed in this area since all published articles lacked methodologies, especially in data collection and analysis. Disaster preparedness education was a suitable activity for interprofessional education [21]. Furthermore, based on a meta-analysis, Cherney et al. recommend conducting more research with different experimental methodologies on Online Learner Collaboration between multidiscipline groups to gather practical suggestions for online course instructors and students [22].
One of the key topics in teaching and learning is micro-learning. Micro-learning supports learning in more easily accessible bites of information productively designed online. Therefore, professors, educators, and researchers must be responsible for using this learning method because of its extensive benefits to help students learn better in the right direction [23, 24].
Ball et al., in a study, showed that students who viewed the video podcast showed significant improvement in knowledge; furthermore, their confidence in responding to violence significantly improved [25]. Another study confirmed that educational intervention by SMS significantly increased nurses' knowledge and practice toward clinical guidelines for PIVC placement [26]. In a scoping review, researchers demonstrated that microlearning as an educational strategy has a positive effect on the knowledge and confidence of health profession students in performing procedures and engaging in collaborative learning [27].
Despite the well-known effectiveness of online micro-learning and IDE on different healthcare-related outcomes, there is limited information about their concurrent effects on healthcare providers’ and students’ knowledge and practice respecting triage in war. Researchers did not find a study that was conducted in scope. On the other hand, the nature of war is very different from other crises. Therefore, this study aimed to evaluate the effects of OMIDE on war victim triage on triage-related knowledge and practice of healthcare science students.
Materials and Methods
This quasi-experimental study was conducted in 2021 with a single-group pretest-posttest design. Participants were eighty male students from the three fields of medicine (n=50), nursing (n=20), and medical emergencies (n=10) selected from Baqiyatallah University of Medical Sciences, Iran. Because all eligible students were male, the sampling was done with the males. Inclusion criteria were an agreement for participation and having passed the Emergency Care theoretical course, which included triage. Accordingly, third- and fourth-year medical students, third-year nursing students, and second-year medical emergency students were eligible for the study. Exclusion criteria were participation in any other similar educational program on triage, reluctance to stay in the study, irregular attendance at the intervention sessions, and loss to follow-up at the posttest. Sampling was purposively performed online because educational activities at universities were performed online during the study due to the coronavirus disease 2019 pandemic. Accordingly, ten interdisciplinary WhatsApp groups were created and participants were randomly allocated. Each group consisted of five medical students, two nursing students, and one medical emergency student. Based on Altman’s nomogram, the sample size was calculated to be 75. Sample size calculation parameters were a confidence level of 0.95, a power of 0.90, and an effect size reported in a previous study [28]. Considering a probable withdrawal rate of 5%, the sample size was increased to 78, and finally, 80 students were recruited for the study.
A demographic questionnaire, a war victim triage knowledge questionnaire, and six scenarios about war victim triage practice were used for data collection. The items of the demographic questionnaire were on age and field of education. The war victim triage knowledge questionnaire had thirteen multiple-choice questions, each with only one correct answer. The total score of the questionnaire was 20. This questionnaire was developed through the modified Delphi technique, in which three experts in military medicine and two experts in emergency medicine from military medical universities were invited to formulate questions to assess students’ knowledge about war victim triage. Their questions were assessed and discussed in a single online session consisting of the study authors, military medicine experts, and emergency medicine experts, and questions with the greatest agreement were included in the final questionnaire. The content validity of the questionnaire was assessed by experts in military medicine, emergency medicine, and disaster care selected from Artesh University of Medical Sciences and the University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. All questionnaire items obtained a content validity ratio and index of more than 0.80 and 0.89, respectively. For reliability assessment, fifteen students external to the study twice completed this questionnaire with a two-week interval Cronbach’s alpha was calculated to be 0.92, and inter-class correlation coefficient was 0.94.
To develop the scenarios for assessing participants’ practice respecting war victim triage, twenty experts in military medicine and emergency medicine from military universities of medical sciences in Tehran, Iran, were asked through email to propose ten scenarios with appropriate evaluation questions. They were asked to develop the scenarios using a patient management problem (PMP) format. PMP simulates a real clinical situation in which a healthcare provider faces a patient or victim. Accordingly, the healthcare provider needs to assess the patient’s condition and decide upon the most appropriate interventions. Then, the healthcare provider receives a series of measures that may be useful, non-useful, or even harmful and contraindicated for that clinical situation and should select the best measures to manage that situation. Accordingly, his/her practice is evaluated using seven criteria. During a two-week interval, seven experts provided their scenarios. Then, a panel of seven experts from military medical universities evaluated the scenarios and their corresponding questions, and six scenarios were selected. Scenarios were about triage in chemical, biological, radiological, and nuclear attacks, aerial triage, ethics in triage, field hospital triage, hospital triage, and battlefield triage. For validity assessment, ten military and emergency medicine experts were invited through email to comment on the scenarios. Then the scenarios' content validity ratio and index were calculated to be 0.79 and 0.87, respectively. The Cronbach’s alpha and the test-retest intraclass correlation coefficient of the scenarios were also 0.84 and 0.80, respectively. The total possible score of the scenarios was between –107 and +140.
The study intervention was video-based micro-learning education about war victim triage. Videos were created by an emergency medicine expert with great military medicine experience. Videos were recorded in an audiovisual service center by an expert in creating educational videos. Videos and study instruments were uploaded to a virtual education system, and a personal account was created for each participant. Through the WhatsApp groups, participants were provided with clear explanations about the study intervention, how to answer the study instruments, and how to collaborate and consult with other group members for appropriate triage. Initially, participants completed the study's informed consent form and answered the knowledge questionnaire in ten minutes. Then, the scenarios were provided to them to watch and answer their corresponding questions. Participants in each group could interact with each other and discuss the scenarios to choose the best answers to the scenario questions. They finally answered the questions after reaching a group agreement. After that, the educational videos were provided to them in ninety minutes through a virtual education system. Participants could watch each video just once. Educational materials were about triage on the battlefield, chemical-microbial attacks, triage under fire, triage in field hospitals, aerial triage, and ethics in triage, respectively. Immediately and one month after the intervention, participants re-completed the knowledge questionnaire and answered the questions of the scenario.
The SPSS 22 software was used for data analysis. The Kolmogorov-Smirnov test revealed the normal distribution of the study variables (p>0.05). Accordingly, the data were described through the measures of descriptive statistics and were analyzed through the repeated measures analysis of variance.
Findings
Participants were 50 medical students (62.5%), 20 nursing students (25%), and 10 medical emergency students (12.5%). The mean of participants’ age was 23.07±1.51 years in total, 23.23±0.86 years for medical students, 23.05±2.6 years for nursing students, and 22.22±0.97 years for medical emergencies students (p=0.182).
The repeated measures analysis of variance showed significant differences in the mean scores of knowledge and practice respecting war victim triage across the three measurement time points (p<0.001; Table 1).
Table 1. Within-group comparison (repeated measures analysis of variance) respecting the mean scores of triage-related knowledge and practice across the three measurement time points
Discussion
This study aimed to evaluate the effects of OMIDE about war victim triage on triage-related knowledge and practice of healthcare science students. Findings revealed that students had poor knowledge and practice respecting war victim triage, and OMIDE significantly improved their knowledge and practice. A study in line with our findings showed that triage education through iterative multi-manikin simulation significantly increased students’ triage abilities and efficiency [29]. Another study showed that the students' satisfaction scores for simulation-based triage training, awareness, clinical decision-making, team communication, staff safety, and skills were high. Simulation-based training can be used to improve the triage skills of undergraduate students. In addition, it concluded that this training should be supported in graduate programs because of their lower performance in some triage categories [30].
Moreover, a study reported the significant positive effects of simulation-based education on the ability to perform triage [31] and the learning experiences of students [32]. Another study into the educational needs of aerial evacuation clinicians in the United States showed that simulation-based education about oxygen therapy, negative pressure wound management, and care provision to populations with special needs, such as patients with burn injuries, had the potential to improve the competencies for triage and aerial transfer of victims [33].
Managing the scene and the injured in CBRNE incidents was one of the designed scenarios. A study in line with our study emphasizes that preparation and delivery of training are important requirements for sending training healthcare teams to CBRNE scenes [34]. A study found that communication and mutual awareness among participants led to better teamwork. The lessons provided in the course enabled a suitable level of competence in CBRN matters, which was necessary for analyzing all aspects of CBRN events in an exercise [35].
The most important attribute of our educational intervention was participants’ interactions and learning in interdisciplinary groups. Several other studies also revealed the significant positive effects of interdisciplinary approaches on participants’ abilities to respond to crises, their respect for other professional groups involved in crisis management, and their teamwork and interdisciplinary collaboration [36, 37]. A study confirmed that Interprofessional crisis management education brings together professional groups involved in a crisis, empowering military nurses to collaborate effectively and enhancing their ability to cope with different crises [17].
Of course, evaluation in those studies was face-to-face, while evaluation in the present study was web-based. Moreover, the interventions of those studies lasted from several days to nine months, while our intervention was around two hours. Contrary to our findings, a study found that after a simulation-based disaster-related education, students still had cognitive and functional problems respecting inter-professional collaboration, understanding of each other’s roles and responsibilities, teamwork, conflict management, and client-centeredness and hence, recommended the necessity of integrating inter-professional competencies into disaster management educational programs [38].
OMIDE, through interdisciplinary groups in the present study, allowed students to interact and collaborate, discuss triage conditions, and make the best triage-related decisions in different simulated war situations. In line with our findings, a study reported education type as a factor significantly affecting the collaboration and performance of military forces and healthcare providers [13]. Moreover, another study found that web-based education also significantly improved the ability of emergency medical staff to manage eye injuries in chemical wars [39]. Virtual training with dynamic virtual patients effectively trains healthcare teams in managing mass-casualty incidents, especially for uncommon incidents [40]. Micro-learning can effectively promote and retain knowledge of trauma care and increase nursing students' satisfaction. It is suggested as a new educational approach that can complement or replace traditional methods in conveying important concepts [41].
Traditional educational programs face difficulty retaining knowledge after the course is over due to the forgetting curve. However, our study found that learning remained stable a month after the intervention, with no significant difference in scores of students' knowledge and practice.
Among the strengths of the present study were modern educational approaches, the use of micro learning, virtual education, interdisciplinary groups, PMP, and clinical reasoning in triage. The study's limitations were the lack of a control group and the greater number of medical students in the study sample. All of the students were male because of the nature of the military university context.
Conclusion
Online micro-learning interdisciplinary education about war victim triage has positive effects on interactions and clinical reasoning in the knowledge and practice of healthcare science students regarding war victim triage.
Acknowledgements: Thanks for the support, guidance, and advice from the “Clinical Research Development Unit of Baqiyatallah Hospital." The authors hereby extend their gratitude to all students who participated in this study and appreciate it.
Ethical Permissions: IR.BMSU.BAQ.REC.1399.006
Conflicts of Interests: The authors declare that the research was conducted without any commercial or financial relationships that could be construed as a potential conflict of interest.
Authors’ Contribution: Vafadar Z (First Author), Methodologist/Assistant Researcher/Statistical Analyst (25%); Javadzadeh H (Second Author), Introduction Writer/Methodologist/Assistant Researcher (25%); Behzadnia MJ (Third Author), Discussion Writer (10%); Moayed MS (Fourth Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (40%)
Funding/Support: No funding was received for this study.
Keywords:
Triage [MeSH], Healthcare [MeSH], Student [MeSH], Battlefield , Interdisciplinary Education [MeSH], War [MeSH], Learning [MeSH]
References
1. Aljazairi AF. Triage. London: Emergency Medicine and Traum; 2019. [Link] [DOI:10.5772/intechopen.86227]
2. Rigal S, Pons F. Triage of mass casualties in war conditions: Realities and lessons learned. Int Orthop. 2013;37(8):1433-8. [Link] [DOI:10.1007/s00264-013-1961-y]
3. Pasquier P, Dubost C, Boutonnet M, Chrisment A, Villevieille T, Batjom E, et al. Predeployment training for forward medicalisation in a combat zone: The specific policy of the French Military Health Service. Injury. 2014;45(9):1307-11. [Link] [DOI:10.1016/j.injury.2014.05.037]
4. Falzone E, Pasquier P, Hoffmann C, Barbier O, Boutonnet M, Salvadori A, et al. Triage in military settings. Anaesth Crit Care Pain Med. 2017;36(1):43-51. [Link] [DOI:10.1016/j.accpm.2016.05.004]
5. Elbaih AH, Alnasser SR. Teaching approach for START triage in disaster management. Medicine. 2020;9(4):1109-12. [Link] [DOI:10.5455/medscience.2020.07.147]
6. Butler FK, Smith DJ, Carmona RH. Implementing and preserving the advances in combat casualty care from Iraq and Afghanistan throughout the US Military. J Trauma Acute Care Surg. 2015;79(2):321-6. [Link] [DOI:10.1097/TA.0000000000000745]
7. Araghizadeh H, Khoshmohabat H, Hossini SH, Moayed MS. Pattern of injury and outcome of victims in Ahvaz terrorist attack. Trauma Monthly. 2021;26(2):100-5. [Link]
8. Elder R, Neal C, Davis BA, Almes E, Whitledge L, Littlepage N. Patient satisfaction with triage nursing in a rural hospital emergency department. J Nurs Care Qual. 2004;19(3):263-8. [Link] [DOI:10.1097/00001786-200407000-00013]
9. Saghafinia M, Khatami SM, Nafisi N. Triage of war-injured troops in the Iran-Iraq war. J Res Med Sci. 2008;13(1):8-11. [Persian] [Link]
10. Aloyce R, Leshabari S, Brysiewicz P. Assessment of knowledge and skills of triage amongst nurses working in the emergency centres in Dar es Salaam, Tanzania. African J Emerg Med. 2014;4(1):14-8. [Link] [DOI:10.1016/j.afjem.2013.04.009]
11. Travers S, Carfantan C, Luft A, Aigle L, Pasquier P, Martinaud C, et al. Five years of prolonged field care: Prehospital challenges during recent French military operations. Transfusion. 2019;59(S2):1459-66. [Link] [DOI:10.1111/trf.15262]
12. Eastridge BJ, Mabry RL, Seguin P, Cantrell J, Tops T, Uribe P, et al. Death on the battlefield (2001-2011): Implications for the future of combat casualty care. J Trauma Acute Care Surg. 2012;73(6):S431-7. [Link] [DOI:10.1097/TA.0b013e3182755dcc]
13. Murray B, Judge D, Morris T, Opsahl A. Interprofessional education: A disaster response simulation activity for military medics, nursing, & paramedic science students. Nurse Educ Pract. 2019;39:67-72. [Link] [DOI:10.1016/j.nepr.2019.08.004]
14. Willems A, Waxman B, Bacon AK, Smith J, Peller J, Kitto S. Interprofessional non-technical skills for surgeons in disaster response: A qualitative study of the Australian perspective. J Interprof Care. 2013;27(2):177-83. [Link] [DOI:10.3109/13561820.2012.706337]
15. Green BN, Johnson CD. Interprofessional collaboration in research, education, and clinical practice: Working together for a better future. J Chiropr Educ. 2015;29(1):1-10. [Link] [DOI:10.7899/JCE-14-36]
16. World Health Organization. Framework for action on interprofessional education and collaborative practice. Geneva: WHO; 2010- [cited 2023, 24 July]. Available from: https://www.who.int/publications-detail-redirect/framework-for-action-on-interprofessional-education-collaborative-practice. [Link]
17. Vafadar Z, Aghaei MH, Ebadi A. Military nurses' experiences of interprofessional education in Crisis Management: A qualitative content analysis. J Adv Med Educ Professionalism. 2021;9(2):85-93. [Link]
18. Oyarzun B, Martin F. Systematic review of research on online learner collaboration from 2012-21: Collaboration technologies, design, facilitation, and outcomes. Online Learn. 2023;27(1):71-106. [Link] [DOI:10.24059/olj.v27i1.3407]
19. Singh J, Matthees B. Facilitating interprofessional education in an online environment during the COVID-19 pandemic: A mixed method study. Healthcare; 2021;9(5):567. [Link] [DOI:10.3390/healthcare9050567]
20. Doherty RB, Crowley RA. Principles supporting dynamic clinical care teams: an American College of Physicians position paper. Ann Intern Med. 2013;159(9):620-6. [Link] [DOI:10.7326/0003-4819-159-9-201311050-00710]
21. Jose MM, Dufrene C. Educational competencies and technologies for disaster preparedness in undergraduate nursing education: An integrative review. Nurse Educ Today. 2014;34(4):543-51. [Link] [DOI:10.1016/j.nedt.2013.07.021]
22. Cherney MR, Fetherston M, Johnsen LJ. Online course student collaboration literature: A review and critique. Small Group Res. 2018;49(1):98-128. [Link] [DOI:10.1177/1046496417721627]
23. Leong K, Sung A, Au D, Blanchard CJJoW-AM. A review of the trend of microlearning. J Work Applied Manag. 2020;13(1). [Link] [DOI:10.1108/JWAM-10-2020-0044]
24. Major A, Calandrino TJFJ. Beyond chunking: Micro-learning secrets for effective online design. FDLA J. 2018;3(1):13. [Link]
25. Ball CA, Kurtz AM, Reed T. Evaluating violent person management training for medical students in an emergency medicine clerkship. South Med J. 2015;108(9):520-3. [Link] [DOI:10.14423/SMJ.0000000000000337]
26. Mousavi H, Ghanbari A, Karkhah S, Alizadeh J, Kazemnejad Leyli E, Jafaraghaee F. The effect of clinical guideline education on the knowledge and practice of nurses for peripheral intravenous catheter placement based on short message service: A quasi-experimental study. J Vasc Access. 2022:11297298221101804. [Link] [DOI:10.1177/11297298221101804]
27. De Gagne JC, Park HK, Hall K, Woodward A, Yamane S, Kim SS. Microlearning in health professions education: Scoping review. JMIR Med Educ. 2019;5(2):e13997. [Link] [DOI:10.2196/13997]
28. Aghaei MH, Ebadi A, Aliakbari F, Vafadar Z. The Effectiveness of Crisis Management Education Based on InterProfessional Approach on Military Nurses' Ability to Confront with Crisis. J Military Med. 2020;22(1):54-63. [Link]
29. Vincent DS, Burgess L, Berg BW, Connolly KK. Teaching mass casualty triage skills using iterative multimanikin simulations. Prehosp Emerg Care. 2009;13(2):241-6. [Link] [DOI:10.1080/10903120802706088]
30. Uslu Y, Unver V, Karabacak U. Hybrid simulation in triage training. Int J Caring Sci. 2019;12(3):1626. [Link]
31. Hu F, Yang J, Yang BX, Zhang FJ, Yu SH, Liu Q, et al. The impact of simulation-based triage education on nursing students' self-reported clinical reasoning ability: A quasi-experimental study. Nurse Educ Pract. 2021;50:102949. [Link] [DOI:10.1016/j.nepr.2020.102949]
32. Mills B, Dykstra P, Hansen S, Miles A, Rankin T, Hopper L, et al. Virtual reality triage training can provide comparable simulation efficacy for paramedicine students compared to live simulation-based scenarios. Prehosp Emerg Care. 2020;24(4):525-36. [Link] [DOI:10.1080/10903127.2019.1676345]
33. De Jong MJ, Dukes SF, Losekamp T. Gap analysis to identify clinical education needs of aeromedical evacuation clinicians. Dimens Crit Care Nurs. 2019;38(2):83-9. [Link] [DOI:10.1097/DCC.0000000000000349]
34. Bertrand C, Lecarpentier E, Herodin F, Dorandeu F. Triage issues in a CBRNE crisis: experiences from European projects. Ethics and Law Chem Biolo Radiol Nuclear Explosive Crises. 2019:173-83. [Link] [DOI:10.1007/978-3-030-11977-5_14]
35. Malizia A, Group CM. Disaster management in case of CBRNe events: An innovative methodology to improve the safety knowledge of advisors and first responders. Defense Sec Analysis. 2016;32(1):79-90. [Link] [DOI:10.1080/14751798.2015.1130319]
36. Livingston LL, West CA, Livingston JL, Landry KA, Watzak BC, Graham LL. Simulated disaster day: benefit from lessons learned through years of transformation from silos to interprofessional education. Simulation in healthcare: J Soc Simulation Healthcare. 2016;11(4):293-8. [Link] [DOI:10.1097/SIH.0000000000000173]
37. Kim TE, Shankel T, Reibling ET, Paik J, Wright D, Buckman M, et al. Healthcare students interprofessional critical event/disaster response course. Am J Disaster Med. 2017;12(1):11-26. [Link] [DOI:10.5055/ajdm.2017.0254]
38. Digregorio H, Graber JS, Saylor J, Ness M. Assessment of interprofessional collaboration before and after a simulated disaster drill experience. Nurse Educ Today. 2019;79:194-7. [Link] [DOI:10.1016/j.nedt.2019.05.023]
39. Gershon R, Canton AN, Magda LA, DiMaggio C, Gonzalez D, Dul MW. Web-based training on weapons of mass destruction response for emergency medical services personnel. Am J Disaster Med. 2009;4(3):153-61. [Link] [DOI:10.5055/ajdm.2009.0024]
40. Jung Y. Virtual reality simulation for disaster preparedness training in hospitals: Integrated review. J Med Internet Res. 2022;24(1):e30600. [Link] [DOI:10.2196/30600]
41. Haghighat H, Shiri M, Esmaeili Abdar M, Taher Harikandee SS, Tayebi Z. The effect of micro-learning on trauma care knowledge and learning satisfaction in nursing students. BMC Med Educ. 2023;23(1):622. [Link] [DOI:10.1186/s12909-023-04609-2]