Volume 15, Issue 1 (2023)
Iran J War Public Health 2023, 15(1): 55-60 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2022/10/18 | Accepted: 2023/01/28 | Published: 2023/02/18
Received: 2022/10/18 | Accepted: 2023/01/28 | Published: 2023/02/18
How to cite this article
Hosseini S, Alishiri G, Shakibaee A. Correlation between Body Composition and Body Mass Index with Mental Health and Sleepiness in Chemically Injured Veterans:
A Cross-sectional Study. Iran J War Public Health 2023; 15 (1) :55-60
URL: http://ijwph.ir/article-1-1238-en.html
URL: http://ijwph.ir/article-1-1238-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
1- Quran and Hadith Research Center, Baqiyatallah University of Medical Sciences, Tehran, Iran
2- Chemical Injuries Research Center, Baqiyatallah University of Medical Sciences, Tehran, Iran
3- Exercise Physiology Research Center, Lifestyle Institute, Baqiyatallah University of Medical Sciences, Tehran, Iran
2- Chemical Injuries Research Center, Baqiyatallah University of Medical Sciences, Tehran, Iran
3- Exercise Physiology Research Center, Lifestyle Institute, Baqiyatallah University of Medical Sciences, Tehran, Iran
Full-Text (HTML) (896 Views)
Introduction
Chemically injured veterans are very vulnerable, and because of their special situation, they may confront enormous health difficulties. They are also affected by many biological, mental, and environmental factors [1]. Most chemical veterans are suffering from psychological and physical disorders [2]. Common mental disorders include a range of problems anxiety and depression are among its manifestations [3]. Mental disorders are among the major burden of disease [4]. A study has shown that 29.2% of people experience common mental illness during their lifetime [5]. Several risk factors have been identified for common mental disorders [6-9]. Some of the risk factors for mental disorders are the Body Mass Index (BMI) and body composition [10-12].
Worldwide studies show an increase in the prevalence of obesity and overweight over the past years. Overweight and obesity have increased in children and adolescents in developed countries and developing countries [13]. Body composition indexes, such as waist circumference (WC), BMI, waist-to-hip ratio, and waist-to-height ratio [14], are used for assessing fat distribution, weight gain, and obesity. In men with obesity or android obesity, the fat often is over the waist, and in women with obesity or ganoid obesity, the fat is under the waist, hip, and thigh area. Abdominal obesity, which is assessed by increasing waist-to-hip ratio and waist-to-height ratio, is recognized as one of the risk factors for cardiovascular [15] and diabetes type 2 disease [16].
Body composition, especially fat and muscle mass, is one of the factors affecting common health, diseases [17-19], and also the mental health of people. In obese people, fat distribution in the body has a main role in obesity disorders' incidence [20].
Ghoddousi et al. research showed that the prevalence of obesity among chemical veterans is more than the normal population [21]. Also, recent research revealed the importance of body composition in general and mental health [17, 18]. Walter et al. found that more depression symptoms and low emotional support were accompanied by worse body composition [17]. Hong's study showed that sarcopenic obesity was more in women than men, and it was related to high blood pressure and arthritis. These people also had mobility and self-care problems [18]. Body composition is associated with various aspects of health, including mortality [22], musculoskeletal pain [23], and ischemic stroke [24].
On the other hand, sleepiness and sleep disorders are the results of body composition and obesity, and it is increasingly harmful to health [25-27]. Much research shows that body composition affects sleep quality [26, 27]. For example, St-Onge and Shechter [27] reported that short sleep duration was related to weight increase, and also obesity was one of the risk factors for obstructive sleep apnea, which affected the quality of sleep. Hayley et al.'s survey on the excessive daytime sleepiness and body composition in an adult population showed that excessive sleepiness was related to several anthropometric adiposity profiles, which were independent life style and health factors. Among women, symptoms of sleepiness were higher in overweight and obese subjects than in the normal population [28].
A lot of studies have been done about the relationship between body composition and obesity with medical diseases [21]. But research about the relationship between body composition and psychological health and sleep condition is limited. So this study aimed to determine the correlation between body composition and BMI with mental health and sleepiness in chemically injured veterans.
Instruments and Methods
Study design and population
This cross-sectional study was conducted on chemical veterans referred to the rheumatology ward in Karaj province in 2017-2018. 131 patients were selected through the available sampling method. Recalling 1100 chemical veterans of Karaj province, 131 veterans were visited, and their monitoring plan was carried out. After eating breakfast and a group meeting, they became familiar with the process and objectives of the project. Two hours after breakfast with a BC device, the body composition was detected using a Bio impedance analyzer. After the presence of the researchers in the studied population, descriptive and demographic indexes were surveyed, and then the research questionnaires were given to them to answer.
Body composition
For body composition analysis, chemical veterans went to the laboratory on specific days, and by a bioelectric impedance body analyzer, model PlusAvis 333 (Jawon company; South Korea) the weight, Percent of Body Fat (PBF), Mass of Body Fat (MBF), and Soft Lean Mass (SLM) were measured.
Body Mass Index (BMI)
Height and weight were measured, and then BMI was calculated. On the basis of World Health Organization instructions, people with 25≤BMI<30 were considered overweight, and BMI≥30 were considered as obese [29]. In the present research, body mass index was used as a continuous variable.
General Health Questionnaire (GHQ-28)
General Health Questionnaire-28 (GHQ-28) is a standard tool that consists of 28 questions. GHQ assesses somatic symptoms, anxiety, insomnia, social dysfunction, and depression. We used likert scoring. For each question, the score was between 0-3, so the total score was between 0-84. The high scores show the bad condition of common health [30, 31].
Epworth Sleepiness Scale
Epworth Sleepiness Scale measures the likelihood of a person's napping in everyday activities such as watching TV, sitting inactive on a place, and sitting as a passenger in a bus or taxi. The total score between 0-6 shows adequate sleeping, 7-10 low to moderate sleepiness, 11-15 severe sleepiness and 16-24 dangerous sleepiness [32]. The results of other researches showed that the total score more than 10 in this test was a sign of extensive daily sleepiness [33].
Statistical analysis
Data were analyzed using descriptive indexes and Pearson correlation coefficient. SPSS 19 software was used to analyze the results.
Findings
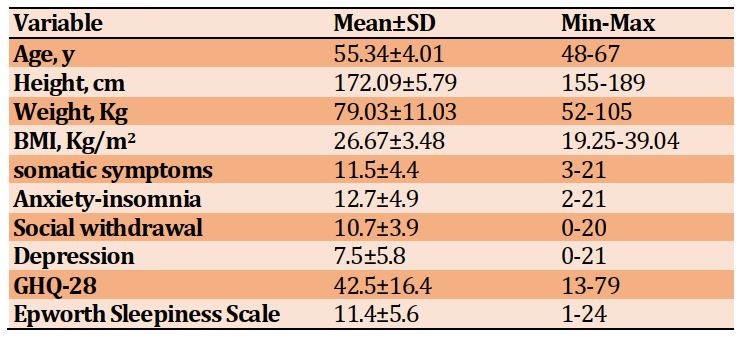
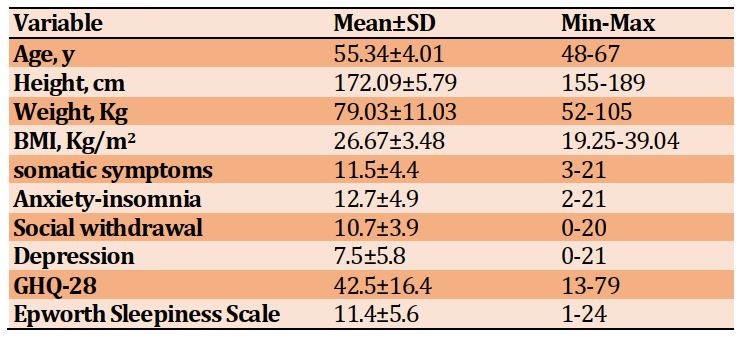
The mean age, height, weight, and BMI were 55.34±4.01 years, 172.09±5.79 cm, 79.03±11.03 kg, and 26.67±3.48 Kg/m2, respectively. In the General Health Questionnaire, the sub-scales of somatic symptoms, anxiety-insomnia, social dysfunction, and depression were 48.9%, 57.2%, 44.3%, and 28.2%, respectively, in the moderate to severe range. The mean score of components of health and sleep are presented in Table 1.
The total mean score for general health was 42.5±16.4, and the mean score for sleepiness was 11.4±5.6.
Table1) Mean anthropometric variables and GHQ scores and its subscales and sleepiness
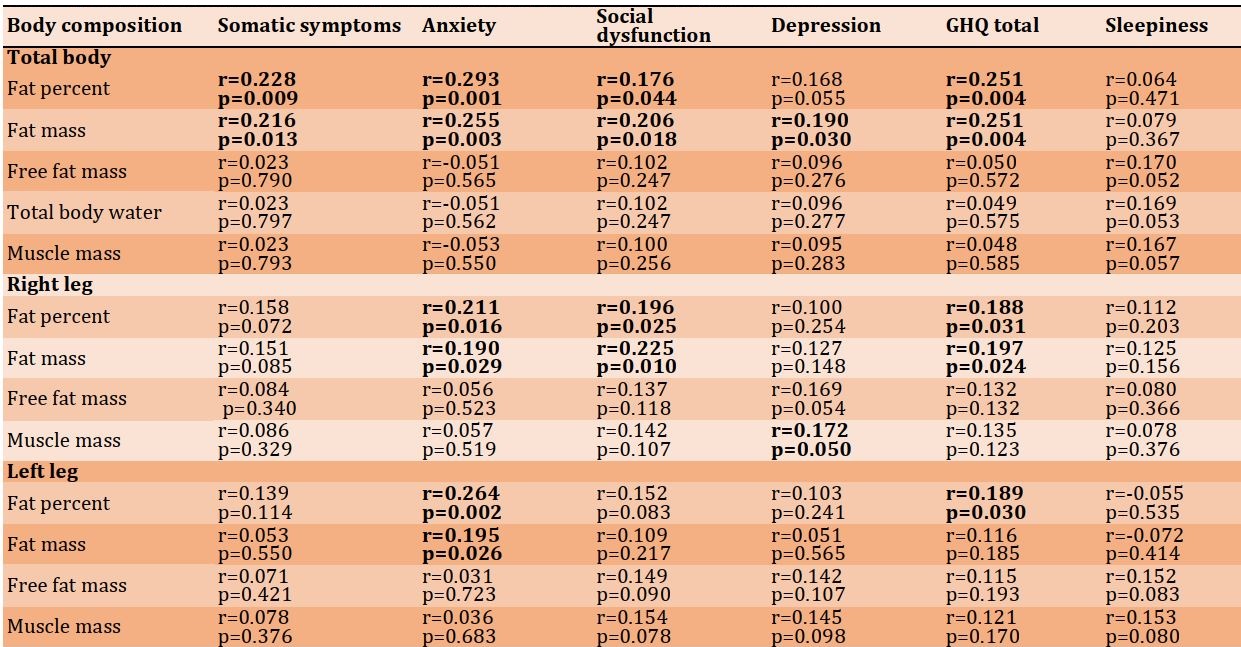
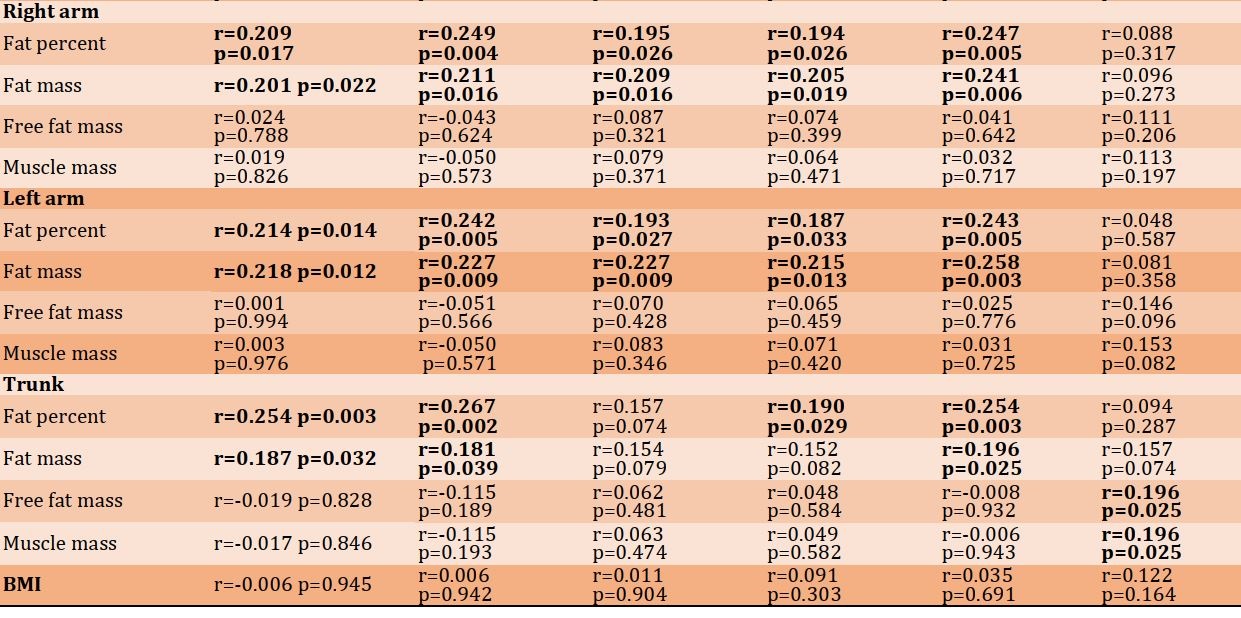
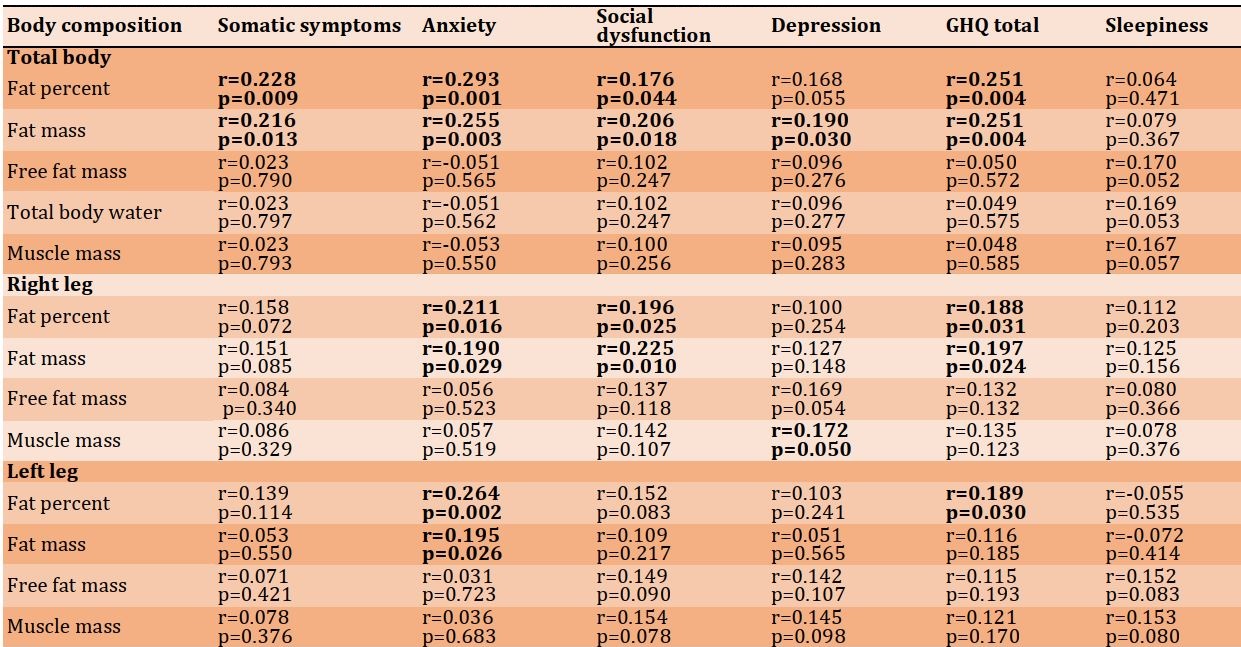
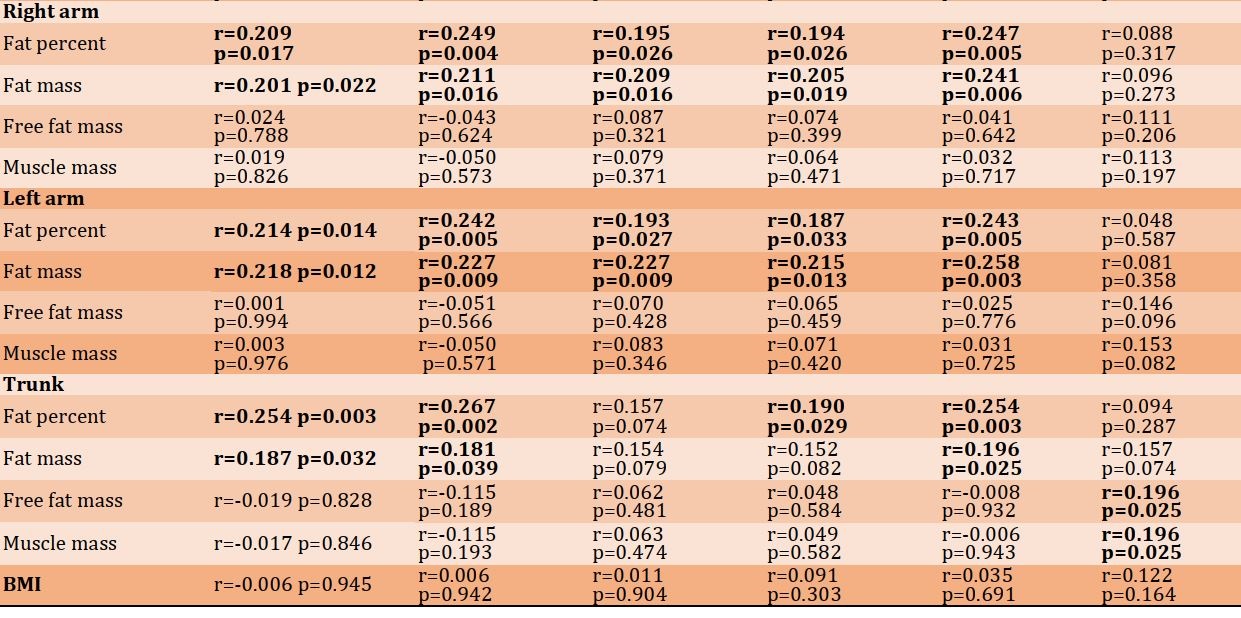
The body composition index, including fat percent (r=0.251; p=0.004) and fat mass (r=0.251; p=0.004), had a significant correlation with the general health score but had no significant correlation with the Epworth sleepiness score. Also, free fat mass, body water percent, and muscle mass had no significant correlation with the general health and Epworth sleepiness scores (Table 2).
Table 2) Correlation between body composition with GHQ and Epworth sleepiness scores
Discussion
The purpose of this study was to investigate the relationship between body composition and BMI with mental health and sleepiness. Accordingly, 131 war chemical injured veterans were examined in dimensions of the body composition, including fat percent, fat mass, free fat mass, total body water, and muscle mass. After reviewing the results, the findings showed that fat percent and fat mass were correlated with total GHQ, including somatic symptoms, anxiety, social dysfunction, and depression. This finding is consistent with the findings which have shown that body fat percentage is associated with the severity of symptoms of depression [34, 35]. Also, findings from another study have shown that fat percentage has a significant correlation with both depression and anxiety [36].
The relationship between body fat and depression can include two psychological and biological mechanisms [35]. From a psychological point of view, perceived weight, physical image, and stigmatization can play a role in this regard [37-40]. Biologically, obesity is associated with several endocrine and metabolic disorders, which are related to mental health, particularly depression [41]. Studies have also shown that body fat is associated with foot pain [42], and this pain can increase the risk of depression [43]. Also, in the case of anxiety and anxiety disorders, studies have shown that obesity is correlated with anxiety [44]. In general, body fat is associated with low quality of life, so higher body fat is associated with worse quality of life [45]. Body fat is associated with various physiological problems, which can lead to a decrease in the level of psychological health of the individual. For example, fat mass and body fat are associated with an increased risk of musculoskeletal pain [23, 46].
Another goal of the present study was to evaluate the amount of sleepiness based on the body composition. However, the findings showed that body composition had no significant relationship with sleepiness. Only trunk free fat mass and Muscle mass were associated with sleepiness. Another similar study in the past showed that there was a positive association between fat mass percentage and sleep quality [47].
Another finding of this study showed that there is no significant relationship between BMI with mental health and sleepiness. No significant relationship between BMI and sleep is in contrast to previous studies, which showed a significant relationship between BMI and sleep and insomnia [48-51]. Studies that show a correlation between BMI and sleep are common in the general population, while the current study was conducted on chemically injured veterans. A systematic review study [52] has shown that obesity is a risk factor for depression, but the present study did not find a correlation between BMI and depression. Given that the current study was conducted on men, this finding is consistent with the previous systematic review, which showed no significant association between overweight and obesity with depression in men [52]. In explaining these findings, it should also be taken into account that psychiatric disorders may lead to changes in body composition and body mass index, as studies have shown [53]. But because of the cross-sectional nature of the present study, it is not possible to determine the direction of the association. Studies have also indicated that depression is associated with obesity [54]. In the study of the effects of sleep problems on obesity, studies have shown that there is a relationship between sleep loss and obesity [55].
This study contains limitations that should be considered when interpreting the results. This is a cross-sectional study, and the causality relationship cannot be extracted, and future studies should examine this issue using a longitudinal research. This study was conducted on people with chemical injuries, and because they were exposed to chemical damage, so generalizing the results to the general population should happen cautiously. This study included males and did not include women, so the generalization of the results is restricted.
By these findings, we must essentially notice the body composition, especially fat percent and fat mass, in common health and sleepiness of chemically injured veterans. Starting interventions and effective exercise programs to solve this problem can promote their health.
Conclusion
Body composition, particularly fat percent and fat mass, is associated with general health in chemically injured veterans.
Acknowledgements: Hereby, we are grateful for the cooperation of “Clinical Research Development Center of Baqiyatullah Hospital”.
Ethical Permission: This protocol was approved by Ethical Committee of Baqiyatallah University of Medical Science (IR.BMSU.REC.1394.56).
Conflict of Interests: There is nothing to declare.
Authors’ Contribution: Hosseini SM (First Author), Methodologist/Main Researcher/Statistical Analyst/Discussion Writer (35%); Alishiri Gh (Second Author), Introduction Writer/Assistant Researcher/Discussion Writer (30%); Shakibaee A (Third Author), Introduction Writer/Main Researcher/Statistical Analyst/Discussion Writer (35%)
Funding: There is nothing to declare.
Chemically injured veterans are very vulnerable, and because of their special situation, they may confront enormous health difficulties. They are also affected by many biological, mental, and environmental factors [1]. Most chemical veterans are suffering from psychological and physical disorders [2]. Common mental disorders include a range of problems anxiety and depression are among its manifestations [3]. Mental disorders are among the major burden of disease [4]. A study has shown that 29.2% of people experience common mental illness during their lifetime [5]. Several risk factors have been identified for common mental disorders [6-9]. Some of the risk factors for mental disorders are the Body Mass Index (BMI) and body composition [10-12].
Worldwide studies show an increase in the prevalence of obesity and overweight over the past years. Overweight and obesity have increased in children and adolescents in developed countries and developing countries [13]. Body composition indexes, such as waist circumference (WC), BMI, waist-to-hip ratio, and waist-to-height ratio [14], are used for assessing fat distribution, weight gain, and obesity. In men with obesity or android obesity, the fat often is over the waist, and in women with obesity or ganoid obesity, the fat is under the waist, hip, and thigh area. Abdominal obesity, which is assessed by increasing waist-to-hip ratio and waist-to-height ratio, is recognized as one of the risk factors for cardiovascular [15] and diabetes type 2 disease [16].
Body composition, especially fat and muscle mass, is one of the factors affecting common health, diseases [17-19], and also the mental health of people. In obese people, fat distribution in the body has a main role in obesity disorders' incidence [20].
Ghoddousi et al. research showed that the prevalence of obesity among chemical veterans is more than the normal population [21]. Also, recent research revealed the importance of body composition in general and mental health [17, 18]. Walter et al. found that more depression symptoms and low emotional support were accompanied by worse body composition [17]. Hong's study showed that sarcopenic obesity was more in women than men, and it was related to high blood pressure and arthritis. These people also had mobility and self-care problems [18]. Body composition is associated with various aspects of health, including mortality [22], musculoskeletal pain [23], and ischemic stroke [24].
On the other hand, sleepiness and sleep disorders are the results of body composition and obesity, and it is increasingly harmful to health [25-27]. Much research shows that body composition affects sleep quality [26, 27]. For example, St-Onge and Shechter [27] reported that short sleep duration was related to weight increase, and also obesity was one of the risk factors for obstructive sleep apnea, which affected the quality of sleep. Hayley et al.'s survey on the excessive daytime sleepiness and body composition in an adult population showed that excessive sleepiness was related to several anthropometric adiposity profiles, which were independent life style and health factors. Among women, symptoms of sleepiness were higher in overweight and obese subjects than in the normal population [28].
A lot of studies have been done about the relationship between body composition and obesity with medical diseases [21]. But research about the relationship between body composition and psychological health and sleep condition is limited. So this study aimed to determine the correlation between body composition and BMI with mental health and sleepiness in chemically injured veterans.
Instruments and Methods
Study design and population
This cross-sectional study was conducted on chemical veterans referred to the rheumatology ward in Karaj province in 2017-2018. 131 patients were selected through the available sampling method. Recalling 1100 chemical veterans of Karaj province, 131 veterans were visited, and their monitoring plan was carried out. After eating breakfast and a group meeting, they became familiar with the process and objectives of the project. Two hours after breakfast with a BC device, the body composition was detected using a Bio impedance analyzer. After the presence of the researchers in the studied population, descriptive and demographic indexes were surveyed, and then the research questionnaires were given to them to answer.
Body composition
For body composition analysis, chemical veterans went to the laboratory on specific days, and by a bioelectric impedance body analyzer, model PlusAvis 333 (Jawon company; South Korea) the weight, Percent of Body Fat (PBF), Mass of Body Fat (MBF), and Soft Lean Mass (SLM) were measured.
Body Mass Index (BMI)
Height and weight were measured, and then BMI was calculated. On the basis of World Health Organization instructions, people with 25≤BMI<30 were considered overweight, and BMI≥30 were considered as obese [29]. In the present research, body mass index was used as a continuous variable.
General Health Questionnaire (GHQ-28)
General Health Questionnaire-28 (GHQ-28) is a standard tool that consists of 28 questions. GHQ assesses somatic symptoms, anxiety, insomnia, social dysfunction, and depression. We used likert scoring. For each question, the score was between 0-3, so the total score was between 0-84. The high scores show the bad condition of common health [30, 31].
Epworth Sleepiness Scale
Epworth Sleepiness Scale measures the likelihood of a person's napping in everyday activities such as watching TV, sitting inactive on a place, and sitting as a passenger in a bus or taxi. The total score between 0-6 shows adequate sleeping, 7-10 low to moderate sleepiness, 11-15 severe sleepiness and 16-24 dangerous sleepiness [32]. The results of other researches showed that the total score more than 10 in this test was a sign of extensive daily sleepiness [33].
Statistical analysis
Data were analyzed using descriptive indexes and Pearson correlation coefficient. SPSS 19 software was used to analyze the results.
Findings
The mean age, height, weight, and BMI were 55.34±4.01 years, 172.09±5.79 cm, 79.03±11.03 kg, and 26.67±3.48 Kg/m2, respectively. In the General Health Questionnaire, the sub-scales of somatic symptoms, anxiety-insomnia, social dysfunction, and depression were 48.9%, 57.2%, 44.3%, and 28.2%, respectively, in the moderate to severe range. The mean score of components of health and sleep are presented in Table 1.
The total mean score for general health was 42.5±16.4, and the mean score for sleepiness was 11.4±5.6.
Table1) Mean anthropometric variables and GHQ scores and its subscales and sleepiness
The body composition index, including fat percent (r=0.251; p=0.004) and fat mass (r=0.251; p=0.004), had a significant correlation with the general health score but had no significant correlation with the Epworth sleepiness score. Also, free fat mass, body water percent, and muscle mass had no significant correlation with the general health and Epworth sleepiness scores (Table 2).
Table 2) Correlation between body composition with GHQ and Epworth sleepiness scores
Discussion
The purpose of this study was to investigate the relationship between body composition and BMI with mental health and sleepiness. Accordingly, 131 war chemical injured veterans were examined in dimensions of the body composition, including fat percent, fat mass, free fat mass, total body water, and muscle mass. After reviewing the results, the findings showed that fat percent and fat mass were correlated with total GHQ, including somatic symptoms, anxiety, social dysfunction, and depression. This finding is consistent with the findings which have shown that body fat percentage is associated with the severity of symptoms of depression [34, 35]. Also, findings from another study have shown that fat percentage has a significant correlation with both depression and anxiety [36].
The relationship between body fat and depression can include two psychological and biological mechanisms [35]. From a psychological point of view, perceived weight, physical image, and stigmatization can play a role in this regard [37-40]. Biologically, obesity is associated with several endocrine and metabolic disorders, which are related to mental health, particularly depression [41]. Studies have also shown that body fat is associated with foot pain [42], and this pain can increase the risk of depression [43]. Also, in the case of anxiety and anxiety disorders, studies have shown that obesity is correlated with anxiety [44]. In general, body fat is associated with low quality of life, so higher body fat is associated with worse quality of life [45]. Body fat is associated with various physiological problems, which can lead to a decrease in the level of psychological health of the individual. For example, fat mass and body fat are associated with an increased risk of musculoskeletal pain [23, 46].
Another goal of the present study was to evaluate the amount of sleepiness based on the body composition. However, the findings showed that body composition had no significant relationship with sleepiness. Only trunk free fat mass and Muscle mass were associated with sleepiness. Another similar study in the past showed that there was a positive association between fat mass percentage and sleep quality [47].
Another finding of this study showed that there is no significant relationship between BMI with mental health and sleepiness. No significant relationship between BMI and sleep is in contrast to previous studies, which showed a significant relationship between BMI and sleep and insomnia [48-51]. Studies that show a correlation between BMI and sleep are common in the general population, while the current study was conducted on chemically injured veterans. A systematic review study [52] has shown that obesity is a risk factor for depression, but the present study did not find a correlation between BMI and depression. Given that the current study was conducted on men, this finding is consistent with the previous systematic review, which showed no significant association between overweight and obesity with depression in men [52]. In explaining these findings, it should also be taken into account that psychiatric disorders may lead to changes in body composition and body mass index, as studies have shown [53]. But because of the cross-sectional nature of the present study, it is not possible to determine the direction of the association. Studies have also indicated that depression is associated with obesity [54]. In the study of the effects of sleep problems on obesity, studies have shown that there is a relationship between sleep loss and obesity [55].
This study contains limitations that should be considered when interpreting the results. This is a cross-sectional study, and the causality relationship cannot be extracted, and future studies should examine this issue using a longitudinal research. This study was conducted on people with chemical injuries, and because they were exposed to chemical damage, so generalizing the results to the general population should happen cautiously. This study included males and did not include women, so the generalization of the results is restricted.
By these findings, we must essentially notice the body composition, especially fat percent and fat mass, in common health and sleepiness of chemically injured veterans. Starting interventions and effective exercise programs to solve this problem can promote their health.
Conclusion
Body composition, particularly fat percent and fat mass, is associated with general health in chemically injured veterans.
Acknowledgements: Hereby, we are grateful for the cooperation of “Clinical Research Development Center of Baqiyatullah Hospital”.
Ethical Permission: This protocol was approved by Ethical Committee of Baqiyatallah University of Medical Science (IR.BMSU.REC.1394.56).
Conflict of Interests: There is nothing to declare.
Authors’ Contribution: Hosseini SM (First Author), Methodologist/Main Researcher/Statistical Analyst/Discussion Writer (35%); Alishiri Gh (Second Author), Introduction Writer/Assistant Researcher/Discussion Writer (30%); Shakibaee A (Third Author), Introduction Writer/Main Researcher/Statistical Analyst/Discussion Writer (35%)
Funding: There is nothing to declare.
Keywords:
References
1. Razavi SM, Negahban Z, Pirhosseinloo M, Razavi MS, Hadjati G, Salamati P. Sulfur mustard effects on mental health and quality-of-life: a review. Iran J Psychiatry Behav Sci. 2014;8(3):11-21. [Link]
2. Khateri S, Ghanei M, Keshavarz S, Soroush M, Haines D. Incidence of lung, eye, and skin lesions as late complications in 34,000 Iranians with wartime exposure to mustard agent. J Occup Environ Med. 2003;45(11):1136-43. [Link] [DOI:10.1097/01.jom.0000094993.20914.d1]
3. Goldberg DP, Huxley P. Common mental disorders: A bio-social model. London: Tavistock; 1992. [Link]
4. Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012;380(9859):2163-96. [Link] [DOI:10.1016/S0140-6736(12)61729-2]
5. Steel Z, Marnane C, Iranpour C, Chey T, Jackson JW, Patel V, et al. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980-2013. Int J Epidemiol. 2014;43(2):476-93. [Link] [DOI:10.1093/ije/dyu038]
6. Patel V, Kirkwood BR, Pednekar S, Weiss H, Mabey D. Risk factors for common mental disorders in women. Population-based longitudinal study. Br J Psychiatry. 2006;189:547-55. [Link] [DOI:10.1192/bjp.bp.106.022558]
7. Carlotto MS, Câmara SG. Prevalence and risk factors of common mental disorders among teachers. Revista de Psicología del Trabajo y de las Organizaciones. 2015;31(3):201-6. [Link] [DOI:10.1016/j.rpto.2015.04.003]
8. Trautmann S, Schönfeld S, Heinrich A, Schäfer J, Zimmermann P, Wittchen HU. Risk factors for common mental disorders in the context of military deployment: a longitudinal study. Euro Psychiatry. 2015;30:303. [Link] [DOI:10.1016/S0924-9338(15)30244-3]
9. de Heer EW, Have MT, van Marwijk HWJ , Dekker J , de Graaf R, Beekman ATF. Pain as a risk factor for common mental disorders. Results from the Netherlands Mental Health Survey and Incidence Study-2: a longitudinal, population-based study. Pain. 2018;159(4):712-8. [Link] [DOI:10.1097/j.pain.0000000000001133]
10. McCrea RL, Berger YG, King MB. Body mass index and common mental disorders: exploring the shape of the association and its moderation by age, gender and education. Int J Obes (Lond). 2012;36(3):414-21. [Link] [DOI:10.1038/ijo.2011.65]
11. Pasco JA, Williams LJ, Jacka FN, Stupka N, Brennan-Olsen SL, Holloway KL, et al. Sarcopenia and the common mental disorders: a potential regulatory role of skeletal muscle on brain function? Curr Osteoporos Rep. 2015;13(5):351-7. [Link] [DOI:10.1007/s11914-015-0279-7]
12. Abera M, Tesfaye M, Hanlon C, Admassu B, Girma T, Wells JC, et al. Body composition during early infancy and mental health outcomes at 5 years of age: a prospective cohort study of ethiopian children. J Pediatr. 2018;200:225-31. [Link] [DOI:10.1016/j.jpeds.2018.04.055]
13. Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the global burden of disease study 2013. Lancet. 2014;384(9945):766-81. [Link] [DOI:10.1016/S0140-6736(14)60460-8]
14. Mushtaq MU, Gull S, Abdullah HM, Shahid U, Shad MA, Javed Akram J. Waist circumference, waist-hip ratio and waist-height ratio percentiles and central obesity among Pakistani children aged five to twelve years. BMC Pediatr. 2011;11:105. [Link] [DOI:10.1186/1471-2431-11-105]
15. Bovet P, Arlabosse T, Viswanathan B, Myers G. Association between obesity indices and cardiovascular risk factors in late adolescence in the Seychelles. BMC Pediatr. 2012;12:176. [Link] [DOI:10.1186/1471-2431-12-176]
16. Manjoo P, Joseph L, Dasgupta K. Abdominal adiposity and daily step counts as determinants of glycemic control in a cohort of patients with type 2 diabetes mellitus. Nutr Diabetes. 2012;2(1):e25. [Link] [DOI:10.1038/nutd.2011.22]
17. Walther A, Philipp M, Lozza N, Ehlert U. Emotional support, depressive symptoms, and age-related alterations in male body composition: cross-sectional findings from the men's health 40+ study. Front Psychol. 2017;8:1075. [Link] [DOI:10.3389/fpsyg.2017.01075]
18. Hong SY. Body composition and its association with health outcomes among elderly South Koreans. Pacific Sci Rev. 2014;16(2):110-6. [Link] [DOI:10.1016/j.pscr.2014.08.021]
19. Pasdar Y, Niazi P, Darbandi M, Khalvandi F, Izadi N. Effect of physical activity on body composition and quality of life among women staff of Kermanshah University of Medical Sciences in 2013. J Rafsanjan Univ Med Sci. 2015;14(2):99-110. [Persian] [Link]
20. Abente EJ, Subramanian M, Ramachandran V, Najafi-Shoushtari SH. MicroRNAs in obesity-associated disorders. Arch Biochem Biophys. 2016;589:108-19. [Link] [DOI:10.1016/j.abb.2015.09.018]
21. Ghoddousi K, Ghanei M, Bahaeloo Horeh S, Khoddami Vishteh H. Body mass index in veterans exposed to chemical warfare agents with chronic bronchiolitis. Iran J Endocrinol Metab. 2007;9(3):285-90. [Persian] [Link]
22. Lee DH, EL Giovannucci EL. Body composition and mortality in the general population: A review of epidemiologic studies. Exp Biol Med (Maywood). 2018;243(17-18):1275-85. [Link] [DOI:10.1177/1535370218818161]
23. Yoo JJ, Cho NH, Lim SH, Kim HA. Relationships between body mass index, fat mass, muscle mass, and musculoskeletal pain in community residents. Arthritis Rheumatol. 2014;66(12):3511-20. [Link] [DOI:10.1002/art.38861]
24. Zahn K, Linseisen J, Heier M, Peters A, Thorand B, Nairz F, et al. Body fat distribution and risk of incident ischemic stroke in men and women aged 50 to 74 years from the general population. The KORA Augsburg cohort study. PLoS One. 2018;13(2):e0191630. [Link] [DOI:10.1371/journal.pone.0191630]
25. Wolkow AP, Dickinson DL, Rajaratnam SM, Drummond SP. 0963 Sleep debt and daytime sleepiness mediate the relationship between sleep and mental health outcomes in young adults: a cross-sectional study. Sleep. 2018;41(suppl_1):A357-8. [Link] [DOI:10.1093/sleep/zsy061.962]
26. Rshikesan PB, Subramanya P, Singh D. Sleep quality and body composition variations in obese male adults after 14 weeks of yoga intervention: a randomized controlled trial. Int J Yoga. 2017;10(3):128-37. [Link] [DOI:10.4103/ijoy.IJOY_53_16]
27. St-Onge MP, Shechter A. Sleep disturbances, body fat distribution, food intake and/or energy expenditure: pathophysiological aspects. Horm Mol Biol Clin Investig. 2014;17(1):29-37. [Link] [DOI:10.1515/hmbci-2013-0066]
28. Hayley AC, Williams LJ, Kennedy GA, Berk M, Brennan SL, Pasco JA. Excessive daytime sleepiness and body composition: a population-based study of adults. PLoS One. 2014;9(11):e112238. [Link] [DOI:10.1371/journal.pone.0112238]
29. World Health Organization. Obesity : preventing and managing the global epidemic [Internet]. Geneva: World Health Organization; 2000 [cited 2019 May 11]. Available from: https://apps.who.int/iris/handle/10665/42330 [Link]
30. Nazifi M, Mokarami H, Akbaritabar A, Faraji Kujerdi M, Tabrizi R, Rahi A. Reliability, validity and factor structure of the persian translation of General Health Questionnire (GHQ-28) in hospitals of Kerman University of Medical Sciences. J Adv Bio Med Sci. 2013;3(4):336-42. [Persian] [Link] [DOI:10.17795/jhealthscope-15547]
31. Khosravi A, Mousavi SA, Chaman R, Kish MS, Ashrafi E, Khalili M, et al. Reliability and validity of the Persian ver-sion of the World Health Organization-five well-being index. Int J Health Stud. 2015;1(1):9-17. [Link]
32. Soroush AR, Hamedi Seresht E, Dabiran S. Assessment of sleep depriva and fatigue among general surgerg residents: Is it necessary to reduce residence's work hours? Hakim J. 2008;11(3):35-41. [Persian] [Link]
33. Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540-5. [Link] [DOI:10.1093/sleep/14.6.540]
34. Koksal UI, Erturk Z, Koksal AR, Ozsenel EB, Kaptanogullari OH. What is the importance of body composition in obesity-related depression? Eurasian J Med. 2017;49(2):102-6. [Link] [DOI:10.5152/eurasianjmed.2017.16129]
35. Speed MS, Jefsen OH, Børglum Ad, Speed D, Østergaard SD. Investigating the association between body fat and depression via mendelian randomization. Transl Psychiatry. 2019:9:184. [Link] [DOI:10.1038/s41398-019-0516-4]
36. Guedes EP, Madeira E, Mafort TT, Madeira M, Moreira Ro, Mendonça LM, et al. Body composition and depressive/anxiety symptoms in overweight and obese individuals with metabolic syndrome. Diabetol Metab Syndr. 2013;5(1):82. [Link] [DOI:10.1186/1758-5996-5-82]
37. Levy BR, Pilver CE. Residual stigma: psychological distress among the formerly overweight. Soc Sci Med. 2012;75(2):297-9. [Link] [DOI:10.1016/j.socscimed.2012.03.007]
38. Hunger JM, Major B. Weight stigma mediates the association between BMI and self-reported health. Health Psychol. 2015;34(2):172-5. [Link] [DOI:10.1037/hea0000106]
39. Robinson E, Sutin A, Daly M. Perceived weight discrimination mediates the prospective relation between obesity and depressive symptoms in U.S. and U.K. adults. Health Psychol. 2017;36(2):112-21. [Link] [DOI:10.1037/hea0000426]
40. Stevens SD, Herbozo S, Morrell HE, Schaefer LM, Thompson JK. Adult and childhood weight influence body image and depression through weight stigmatization. J Health Psychol. 2017;22(8):1084-93. [Link] [DOI:10.1177/1359105315624749]
41. Hryhorczuk C, Sharma S, Fulton SE. Metabolic disturbances connecting obesity and depression. Frontiers Neurosci. 2013;7:177. [Link] [DOI:10.3389/fnins.2013.00177]
42. Butterworth PA, Menz HB, Urquhart DM, Cicuttini FM, Landorf KB, Pasco JA, et al. Fat mass is associated with foot pain in men: the geelong osteoporosis study. J Rheumatol. 2016;43(1):138-43. [Link] [DOI:10.3899/jrheum.141331]
43. Awale A, Dufour AB, Katz P, Menz HB, Hannan MT. Link between foot pain severity and prevalence of depressive symptoms. Arthritis Care Res (Hoboken). 2016;68(6):871-6. [Link] [DOI:10.1002/acr.22779]
44. Amiri S, Behnezhad S. Obesity and anxiety symptoms: a systematic review and meta-analysis. Neuropsychiatr. 2019;33(2):72-89. [Link] [DOI:10.1007/s40211-019-0302-9]
45. Kalantar-Zadeh K, Kuwae N, Wu DY, Shantouf RS, Fouque D, Anker SD, et al. Associations of body fat and its changes over time with quality of life and prospective mortality in hemodialysis patients. Am J Clin Nutr. 2006;83(2):202-10. [Link] [DOI:10.1093/ajcn/83.2.202]
46. Walsh TP, Arnold JB, Evans AM, Yaxley A, Damarell RA, Shanahan EM. The association between body fat and musculoskeletal pain: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2018;19(1):233. [Link] [DOI:10.1186/s12891-018-2137-0]
47. Jurado-Fasoli L, Amaro-Gahete FJ, De-la-O A, Dote-Montero M, Gutiérrez A, Castillo MJ. Association between Sleep Quality and Body Composition in Sedentary Middle-Aged Adults. Medicina (Kaunas, Lithuania). 2018;54(5):91. [Link] [DOI:10.3390/medicina54050091]
48. Sivertsen B, Pallesen S, Sand L, Hysing M. Sleep and body mass index in adolescence: results from a large population-based study of Norwegian adolescents aged 16 to 19 years. BMC Pediatr. 2014;14(1):204. [Link] [DOI:10.1186/1471-2431-14-204]
49. Pearson NJ, Johnson LL, Nahin RL. Insomnia, trouble sleeping, and complementary and alternative medicine: Analysis of the 2002 national health interview survey data. Arch Intern Med. 2006;166(16):1775-82. [Link] [DOI:10.1001/archinte.166.16.1775]
50. Singareddy R, Vgontzas AN, Fernandez-Mendoza J, Liao D, Calhoun S, Shaffer ML et al. Risk factors for incident chronic insomnia: a general population prospective study. Sleep Med. 2012;13(4):346-53. [Link] [DOI:10.1016/j.sleep.2011.10.033]
51. Vgontzas AN, Lin HM, Papaliaga M, Calhoun S, Vela-Bueno A, Chrousos GP, et al. Short sleep duration and obesity: the role of emotional stress and sleep disturbances. Int J Obes (Lond). 2008;32(5):801-9. [Link] [DOI:10.1038/ijo.2008.4]
52. Amiri S, Behnezhad S, Nadinlui KB. Body Mass Index (BMI) and risk of depression in adults: A systematic review and meta-analysis of longitudinal studies. Obes Med. 2018;12:1-12. [Link] [DOI:10.1016/j.obmed.2018.10.001]
53. Williams LJ, Pasco JA, Henry MJ, Jacka FN, Dodd S, Nicholson GC, et al. Lifetime psychiatric disorders and body composition: a population-based study. J Affect Disord. 2009;118(1-3):173-9. [Link] [DOI:10.1016/j.jad.2009.02.001]
54. de Wit L, Luppino F, van Straten A, Penninx B, Zitman F, Cuijpers P. Depression and obesity: a meta-analysis of community-based studies. Psychiatry Res. 2010;178(2):230-5. [Link] [DOI:10.1016/j.psychres.2009.04.015]
55. Beccuti G, Pannain S. Sleep and obesity. Current opinion in clinical nutrition and metabolic care. 2011;14(4):402-12. [Link] [DOI:10.1097/MCO.0b013e3283479109]











