Volume 13, Issue 2 (2021)
Iran J War Public Health 2021, 13(2): 131-138 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2021/09/1 | Accepted: 2021/09/8 | Published: 2021/10/6
Received: 2021/09/1 | Accepted: 2021/09/8 | Published: 2021/10/6
How to cite this article
Samajpaty S. Calculating the Fluid Pressure of Aorta according to the Principles of Hemomechanics in Injuries and Trauma. Iran J War Public Health 2021; 13 (2) :131-138
URL: http://ijwph.ir/article-1-1010-en.html
URL: http://ijwph.ir/article-1-1010-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Authors
S. Samajpaty *
Department of General Medicine, International Faculty, Pirogov Russian National Research Medical University (RNRMU), Moscow, Russian Federation
Full-Text (HTML) (799 Views)
Introduction
For centuries, the physics of the human body has been neglected, especially the properties of fluid inside the human body. It is a fact that without understanding the physio-chemical properties of blood, our knowledge of rheumatology and cardiology is highly insufficient [1-5]. Our explanation for every pathology is highly inefficient, and our understanding of blood pressure is not without mistakes. The basic interpretation of human physiology is full of discrepancies like – blood vessels do not have systole and diastole, so what is the blood pressure in different blood vessels? What role does exactly turbulence play in the dynamics and mechanics of the fluid? What causes differences in fluid pressure in pathological conditions? What difference does it make on some vessels being elastic and some non-elastic, and many more so on?. Negligence of such aspects of hematology is intensively detrimental to the general understanding of human physiology. Lack of knowledge of this is also a hindrance to general surgical practice [6-8]. Throughout the literature of this article, the author would try to find rational answers to such questions.
The article is a mathematical and physical endeavor to resolve the in-depth questions of blood physiology and pathology. A recent article published under the title "Innovation Strategies in Health Economics: A Force That Makes Blood Move and Game of Gravity in It – Futuristic Economic Plans" by Soham Samajpaty and Samrat Ray has provided an exclusive look into the world of fluid mechanics of the blood and that of property of blood as a continuum [1, 9-11]. Mathematical and physical analysis was based on this finding. The aim is to determine the principles of "Hemomechanics", carry out a review of the pathology of hemodynamic disorders in the light of hemo-mechanics concerning already proven chemo-physical basis, and determine the fluid pressure of the aorta through the mathematical application. Specific focus has been made on recurrent pathologies despite successful therapy or surgery, and a probable solution to such a problem has been provided. Thermodynamic parameters of blood vessel boundary have also been determined mathematically, explaining associated pathology. This article aimed to solve the disparities in medical science, specifically from the hematology aspect, and it is expected that the findings if implemented industrially, would result in a gross change in human health and morbidity. Above all, from the perspective of physiology, an essential aspect has been determined – laws of hemo-mechanics.
Calculations and Methods
The blood pressure of the aorta has to be hugely different from the blood pressure of other blood vessels as the aorta is an elastic blood vessel like the pulmonary trunk. Hence, volumetric change of Bulk's modulus is mandatory. From Samajpaty's Pressure for condensed equation, we know (Equation 1):

Where: PB is the pressure on the blood vessel, ꞙ – the force of the blood, Sf – length of the blood vessel, and rv is the radius of the blood vessel.
Now let PB1 be the pressure of the aorta at rest when the aorta is not distended; ꞙ1 be the force of blood, rv1 – radius of the non-distended aorta and Sf is the length of the aorta (until aortic bifurcation). It is not be noted here that the force of the blood is not constant as a change in volume of the aorta provides an opportunity for the increment of a unit volume of hematocrit, on which the "latent shear" force – ꞙ depends. Hence, the pressure formula of the aorta at rest is (Equation 2):

Let PB2 be the pressure of the aorta when distended, I.e., during diastole; ꞙ2 be the force of blood, rv2 – the radius of the distended aorta and Sf is the length of the aorta (until aortic bifurcation). Hence, the pressure formula for the diastolic aorta is (Equation 3):

The change is pressure; hence from equation 2 and equation 3 is (Equation 4):

Incredibly, the author derives the factors α and β which appears to be regulating factor in this case. There are 5 types of leukocytes (WBC)–Monocyte, Lymphocyte, Neutrophil, Basophil, and Eosinophil along with the erythrocytes (RBC) in the unit volume of blood. Hence, there are 6 types of blood cells, neglecting the platelets for the sake of easy calculation. From the findings in the article – "Innovation strategies in health economics: a force that makes blood move and game of gravity in it – futuristic economic plans," we know that (Equation 11):
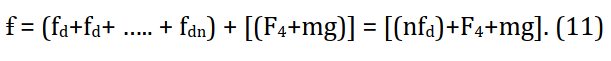
where: fd = 6πrhηv; (rh – radius of hematocrit; η – viscosity; rv – radius of vessel). So, when normal of RBCs is approximately = 4.3 x 1012 and approximate value of WBCs = 3.5 x 109 per micro liter. The value of nfd = 1.548.360 N and that of ꞙ = 1.5 x 106 N. Hence, pressure of the aorta at diastole (Equation 3), ꞙ = 1.5 x 106 N = 1140 x 106 mm Hg (as 1 N = 760 mm Hg); rv2 = 20 mm and Sf = 120 mm (as approximate value in normal population is). Or PB2 = 1140 x 106 / {2π. 20 (120+20)}; or PB2 = 1140 x 106 / 17584; or PB2 = 64.8 x 103. Thus; PB2 = 65 x 103 mm Hg. Hence, this tally approximately with the actual cauterized value of 75mm Hg with ± 10 units of error factor likewise as designed in the scale (Equation 12):

where: (P/ ± 5) = pressure reading on barometer. But from observation, it is noted that the error factor here would be approximately ± 10 units due to the elastic property of the tissue [1-3].
Distention of the aorta, like any other elastic material, is caused by force application on it. When blood from the left ventricle goes into the aorta during ventricular systole, the sudden volume of blood applies the force – "ꞙ" on it, followed by distention of the aorta and volumetric increment. The depression on the wall of the aorta can, however, be calculated in the following manner. If δ depression is caused on the wall of the aorta by ꞙ amount of force when the wall of the aorta under consideration is Sf in length, b in breadth, d in-depth, and γ is the young's modulus, then depression is (Equation 13):

It has to be noted here that the aorta as a system expands volumetrically, which might be explained as such (Equation 14):

β is the bulk modulus; ꞙ is the force; A is the area under consideration; ΔV is the volume change, and Vo is the initial volume.
But while considering the single wall of the aorta – they are elastic in nature and hence, has their Young's modulus (γ). We know that no elastomer can be perfectly elastic, and hence with every expansion, there is a little fatigue, no matter how efficient the elastic might be. Hence, deformity in the elastic fibers of tunica media is inevitable [4, 5-7]. Such molecules get accumulated in the body system to such an extent that there is the failure of liver microsomal enzyme-mediated metabolism. Hence these hydrocarbon compounds and complexes with aromatic rings keep on accumulating in the blood continuum. This is complemented by usual factors of increased low-density lipoprotein (LDL), very-low-density lipoprotein (VLDL), and aging factor.
This increases the value of "n" in the formula (Equation 11), resulting in increased "shear force" followed by increased "δ", thus making the wall of the aorta towards elastic fatigue at a faster rate, resulting in ultimately disruption of elastic fibers of the tunica media – causing "aortic aneurysm". A report titled, "Recurrence of Aneurysm of the Ascending Aorta after Patch Repair: The Fate of an Aortic Patch" showed that 35% of the patients showed significant dilatation of the patch repaired portion; reformation occurred in 27% of the patients after patch repair in 2-14 years. They also cite elasticity change as a possibility of such a negative outcome [6-12]. But we would go one step forward and suggest producing Dacron patch polymer as per Young's modulus of the aorta, keeping the δ value in mind and tally the pressure by using Equation 9.
Based on clinical evidential observations and peer-reviewed data, and mathematical findings with economic schemes of Soham Samajpaty and Samrat Ray, laws of hemomechanics are hence being laid down:
For centuries, the physics of the human body has been neglected, especially the properties of fluid inside the human body. It is a fact that without understanding the physio-chemical properties of blood, our knowledge of rheumatology and cardiology is highly insufficient [1-5]. Our explanation for every pathology is highly inefficient, and our understanding of blood pressure is not without mistakes. The basic interpretation of human physiology is full of discrepancies like – blood vessels do not have systole and diastole, so what is the blood pressure in different blood vessels? What role does exactly turbulence play in the dynamics and mechanics of the fluid? What causes differences in fluid pressure in pathological conditions? What difference does it make on some vessels being elastic and some non-elastic, and many more so on?. Negligence of such aspects of hematology is intensively detrimental to the general understanding of human physiology. Lack of knowledge of this is also a hindrance to general surgical practice [6-8]. Throughout the literature of this article, the author would try to find rational answers to such questions.
The article is a mathematical and physical endeavor to resolve the in-depth questions of blood physiology and pathology. A recent article published under the title "Innovation Strategies in Health Economics: A Force That Makes Blood Move and Game of Gravity in It – Futuristic Economic Plans" by Soham Samajpaty and Samrat Ray has provided an exclusive look into the world of fluid mechanics of the blood and that of property of blood as a continuum [1, 9-11]. Mathematical and physical analysis was based on this finding. The aim is to determine the principles of "Hemomechanics", carry out a review of the pathology of hemodynamic disorders in the light of hemo-mechanics concerning already proven chemo-physical basis, and determine the fluid pressure of the aorta through the mathematical application. Specific focus has been made on recurrent pathologies despite successful therapy or surgery, and a probable solution to such a problem has been provided. Thermodynamic parameters of blood vessel boundary have also been determined mathematically, explaining associated pathology. This article aimed to solve the disparities in medical science, specifically from the hematology aspect, and it is expected that the findings if implemented industrially, would result in a gross change in human health and morbidity. Above all, from the perspective of physiology, an essential aspect has been determined – laws of hemo-mechanics.
Calculations and Methods
The blood pressure of the aorta has to be hugely different from the blood pressure of other blood vessels as the aorta is an elastic blood vessel like the pulmonary trunk. Hence, volumetric change of Bulk's modulus is mandatory. From Samajpaty's Pressure for condensed equation, we know (Equation 1):

Where: PB is the pressure on the blood vessel, ꞙ – the force of the blood, Sf – length of the blood vessel, and rv is the radius of the blood vessel.
Now let PB1 be the pressure of the aorta at rest when the aorta is not distended; ꞙ1 be the force of blood, rv1 – radius of the non-distended aorta and Sf is the length of the aorta (until aortic bifurcation). It is not be noted here that the force of the blood is not constant as a change in volume of the aorta provides an opportunity for the increment of a unit volume of hematocrit, on which the "latent shear" force – ꞙ depends. Hence, the pressure formula of the aorta at rest is (Equation 2):

Let PB2 be the pressure of the aorta when distended, I.e., during diastole; ꞙ2 be the force of blood, rv2 – the radius of the distended aorta and Sf is the length of the aorta (until aortic bifurcation). Hence, the pressure formula for the diastolic aorta is (Equation 3):

The change is pressure; hence from equation 2 and equation 3 is (Equation 4):

Incredibly, the author derives the factors α and β which appears to be regulating factor in this case. There are 5 types of leukocytes (WBC)–Monocyte, Lymphocyte, Neutrophil, Basophil, and Eosinophil along with the erythrocytes (RBC) in the unit volume of blood. Hence, there are 6 types of blood cells, neglecting the platelets for the sake of easy calculation. From the findings in the article – "Innovation strategies in health economics: a force that makes blood move and game of gravity in it – futuristic economic plans," we know that (Equation 11):
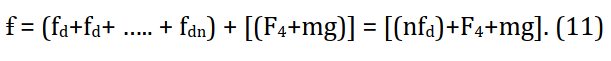
where: fd = 6πrhηv; (rh – radius of hematocrit; η – viscosity; rv – radius of vessel). So, when normal of RBCs is approximately = 4.3 x 1012 and approximate value of WBCs = 3.5 x 109 per micro liter. The value of nfd = 1.548.360 N and that of ꞙ = 1.5 x 106 N. Hence, pressure of the aorta at diastole (Equation 3), ꞙ = 1.5 x 106 N = 1140 x 106 mm Hg (as 1 N = 760 mm Hg); rv2 = 20 mm and Sf = 120 mm (as approximate value in normal population is). Or PB2 = 1140 x 106 / {2π. 20 (120+20)}; or PB2 = 1140 x 106 / 17584; or PB2 = 64.8 x 103. Thus; PB2 = 65 x 103 mm Hg. Hence, this tally approximately with the actual cauterized value of 75mm Hg with ± 10 units of error factor likewise as designed in the scale (Equation 12):

where: (P/ ± 5) = pressure reading on barometer. But from observation, it is noted that the error factor here would be approximately ± 10 units due to the elastic property of the tissue [1-3].
Distention of the aorta, like any other elastic material, is caused by force application on it. When blood from the left ventricle goes into the aorta during ventricular systole, the sudden volume of blood applies the force – "ꞙ" on it, followed by distention of the aorta and volumetric increment. The depression on the wall of the aorta can, however, be calculated in the following manner. If δ depression is caused on the wall of the aorta by ꞙ amount of force when the wall of the aorta under consideration is Sf in length, b in breadth, d in-depth, and γ is the young's modulus, then depression is (Equation 13):

It has to be noted here that the aorta as a system expands volumetrically, which might be explained as such (Equation 14):

β is the bulk modulus; ꞙ is the force; A is the area under consideration; ΔV is the volume change, and Vo is the initial volume.
But while considering the single wall of the aorta – they are elastic in nature and hence, has their Young's modulus (γ). We know that no elastomer can be perfectly elastic, and hence with every expansion, there is a little fatigue, no matter how efficient the elastic might be. Hence, deformity in the elastic fibers of tunica media is inevitable [4, 5-7]. Such molecules get accumulated in the body system to such an extent that there is the failure of liver microsomal enzyme-mediated metabolism. Hence these hydrocarbon compounds and complexes with aromatic rings keep on accumulating in the blood continuum. This is complemented by usual factors of increased low-density lipoprotein (LDL), very-low-density lipoprotein (VLDL), and aging factor.
This increases the value of "n" in the formula (Equation 11), resulting in increased "shear force" followed by increased "δ", thus making the wall of the aorta towards elastic fatigue at a faster rate, resulting in ultimately disruption of elastic fibers of the tunica media – causing "aortic aneurysm". A report titled, "Recurrence of Aneurysm of the Ascending Aorta after Patch Repair: The Fate of an Aortic Patch" showed that 35% of the patients showed significant dilatation of the patch repaired portion; reformation occurred in 27% of the patients after patch repair in 2-14 years. They also cite elasticity change as a possibility of such a negative outcome [6-12]. But we would go one step forward and suggest producing Dacron patch polymer as per Young's modulus of the aorta, keeping the δ value in mind and tally the pressure by using Equation 9.
Based on clinical evidential observations and peer-reviewed data, and mathematical findings with economic schemes of Soham Samajpaty and Samrat Ray, laws of hemomechanics are hence being laid down:
- 1st Law – Blood is a multi-phasic Non-Newtonian emulsion fluid with "latent shear force" for its movement, dependent primarily on the number of erythrocytes, leukocytes, and on another significant amount of dispersed or dissolved materials during a chemical change in pathological conditions.
- 2nd Law – Pressure of a blood vessel is dependent on the "latent shear force", its length, and radius. A blood vessel is considered one based on the change in radius (and not branching).
- 3rd Law – The "Latent shear force" divides into vector components on arriving at a bend and angle Ө of the bend is the inverse function of "tan" of the ratio of the y-axis and x-axis components of the "latent shear force" (Equation 16):

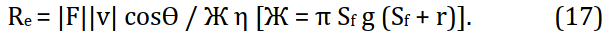
4th Law – The turbulence of blood is dependent on the "latent shear force", the velocity of blood, the cosine of the angle between the two vectors as mentioned earlier, length of the blood vessel, and radius of the blood vessel apart from the parameters of Reynold's equation. Or (Equation 17) [1, 13-20]:
In the paper titled "Innovation strategies in health economics: a force that makes blood move and game of gravity in it – futuristic economic plans" by Samajpaty and Ray, a pressure scale of PB = (P/±5).105 has been mentioned, where, ±5 is correction factor, and P/ is the blood pressure in barometric scale, and PB is the pressure in the author's self-designed mathematical scale [20-25]. Here, the author has suggested neglecting the multiplication factor of 105. We would derive a graphically presentable relationship between the two. To remove this discrepancy and fallacy, we would rewrite the equation as PB = (P/± 5)/105. Now, there is no necessity to neglect the 105 factors . Taking the already given scale after modification: PB = (P/± 5)/105. Taking log on both sides of the equations, we get (Equation 18):

Similarly, as our findings of elastic blood vessels, the equation would be read as Equation 22 (Figures 1a to 1d).


Figure 1) The graphical representation of RHS of equations 21 and 22 when a: (P/+5); b(P/- 5); c(P/+10); d(P/-10)
Findings
Hemodynamic disorders have been effectively explained by the principles of general pathology and chemical physiology. But now, we would leap a step forward and try to analyze the perspectives from a physics point of view, utilizing the principles of Hemo-mechanics. Any injury to the tissue causes an inflammatory reaction. Inflammation is initiated by inflammation mediator chemical compounds. The symptoms classically being – redness, heat, pain, edema, and loss of function. Histamine is released by mast cells located adjacent to the blood vessel, basophils, and platelets. This causes dilation of arterioles and increases venule permeability. Serotonin is released by mast cells when platelet-aggregates contact collagen, resulting in the same as Histamine.
On the other hand, Nitric oxide (NO) synthesized from enzyme nitric oxide synthase (NOS) is released, which acts as a pleiotropic inflammation mediator of inflammation and endothelial smooth muscle relaxing agent. Apart from this, because of injury, there is the breakdown of Arachidonic acid, which results in prostaglandin release. It is to be remembered that the fluid mobility between blood vessels and tissue occurs in the capillary bed. Vasoactive amines, C3a and C5a, Leukotrienes C4, D4, E4, PAF, and Substance P cause an increment in vascular permeability of the capillary walls. The game of pressure in the capillary bed has been effectively mentioned by Starling's equation. We would focus on dynamic and
Now, if an area of a capillary tube increase to A/ and "latent shear force" is also increased due to secretion of multiple chemical factors into circulation, some being described above. So, if the increased latent shear force is ꞙ/, the Bulk modulus can be expressed as Equations 14 and 15. Where: ΔV is the volume change of the capillary and Vo is the initial volume of the capillary. By general definition, the entropy (S) of the unit volume of the blood system will also increase. Resulting in an increment in heat (Q), the temperature being fixed in the same environment. This, again, validates that the capillary process is diabetic. Since (Equation 23):

Where: S is entropy, Q is heat, and T is temperature. On the other hand, an increased entropy will ensure increased freedom of movement across the capillary walls. This results in edema. Thus, putting the mechanical explanation of edema formation forwards. To compare the statement with that of Starling's, capillary hydrostatic pressure increases in the explanation. Naturally, if ꞙ is increased, hydrostatic capillary pressure will also be increased. But effective filtration in case of edema is however increased because of increased capillary oncotic pressure. Starling's equation states that (Equation 24):

where; Jv = fluid movement (ml/min), Kf = hydraulic conductance (ml/min/mm Hg), Pc = capillary hydrostatic pressure (mm Hg), Pi = Interstitial hydrostatic pressure (mm Hg), πc = capillary oncotic pressure (mm Hg) and πi = Interstitial hydrostatic pressure (mm Hg). From the above-stated analogical observation, it's evident that latent shear is directly proportional to hydrostatic capillary pressure and oncotic capillary pressure. Thus (Equation 25):

Gas gangrene is not a hemodynamic disorder, but we would focus on this subject as it involves blood, and the gases found in gas gangrene have such composition – Nitrogen 74.5%, Oxygen 16.1%, Hydrogen 5.9%, and Carbon dioxide 3.4% approximately. But pathologists have failed to explain where and how such a huge gas accumulation occurs inside a human body under the deep fascia. Gas gangrene is specifically caused by infection of Clostridium sp. of multiple strains like C. novyi, C. septicum, C. bifermentans, C. fallax, and C. sordelii by order of prevalence. These bacteria release very fast-acting toxins; alpha-toxin (tissue destruction), beta toxin (tissue necrosis), delta toxin (hemolysin), epsilon toxin (acts like permease that increases cell membrane permeability), iota toxin (tissue necrosis), kappa toxin (acts as collagenase, gelatinase, specifically destroys blood vessel), lambda toxin (protease), mu toxin (hyaluronidase), nu toxin (deoxyribonuclease, hemolytic and necrosis of tissue), and phi toxin (hemolysin and cytolysin as per the finding of C. perferinges). It would be hypothesized and proved with the help of principles of fluid (hemo-) mechanics and applied mathematics that all these gases arise from blood.
The gases mentioned above stay in the dissolved condition in the blood (not liquid but dissolved) under high pressure of the blood vessel at normal conditions. An injury of simple type or any other bacteria does not evolve into gas gangrene for two reasons-(i) all injuries do not cause complete endothelial rupture, and (ii) other bacterial toxins do not initiate spontaneous destruction of the vessel endothelium. The gases under compressed conditions stay dissolved inside the blood vessel, but once the vessel wall is destroyed with such spontaneous action, there is a sudden huge change in pressure of the thermodynamic system in which the gases were until now. Decompression and exposure to a lower pressure of the body cavity or atmosphere (lower) lead to gas formation, and gangrene is simply due to toxin-led necrosis. This gas gets trapped in between fascias and layers in the body. The whole thing is analogical to the sudden opening of an aerated soda can.
If chemical potential energy = μ, Gibb's free energy = G and number of moles = N. We know (Equation 26):

Now, one gas has μ chemical potential energy. Thus, 'n' gases have (μ1+μ2+μ3+ …… +μn) chemical potential energy; similarly, for 'n' gases, there are (N1+N2+N3+ ……. + Nn) moles. So, if Gibb's energy for a dissolved state is represented as Gdis and that of gases state as Ggas, then, for a dissolved state (Equation 28):


Any chemical change is quantified by Gibb's free energy. Simply Ggas has to be greater than Gdis for favoring gas formation. Clinicians have opted for different methods for reducing mortality due to gas gangrene. However, the reason was not very clear behind the situation. An approach of vacuum sealing along with drainage technology has shown a very efficient therapy procedure. The vacuum helps in sucking out the gas formed inside the cavity or abscess. The pathology proceeds very fast, and that's the reason gas production happens spontaneously, by maintaining the thermodynamic parameters.
Emboli is a detached intravascular solid, liquid, or gaseous mass that is transported in the bloodstream to sites away from the place of its origin. This can be thrombus, fat globule or gas bubble, or liquid in liquid embolism, as in the case of amniotic fluid emboli. Until now, the explanation of emboli was very speculative. But in the light of the "latent shear force" of blood postulate and principles of hemo-mechanics, a far-worthy explanation might be put forward. Emboli happen mainly when there is the fulfillment of Virchow's triad. Virchow triad might be caused by many factors; stenosis of valves, calcium and oxalate deposits in the blood-heat circulation system. It comprises three factors in the triad – (i) endothelial injury, (ii) stasis, and (iii) hypercoagulability.
It is to be noted that such pathology will be proceeded by changed blood continuum composition by the influx of inflammatory mediators, cytokines, chemokines, increased volume of metabolic products, etc. This will increase the modulus value of the "latent shear force" of blood—the viscosity of the blood, on the other hand, increases due to hemodilution and blood vessel dilation. Hence, applying the 4th law of Hemo-mechanics (Equation 17). The conclusion might be reached that when other parameters are almost constant (Equation 32):

Hence, turbulence in the blood flow will be noticeable when observed under Doppler ultrasonography. This is not just a mathematical assumption but is verified by clinical research– turbulence was observed in cerebral emboli, and the turbulence proportionate with the degree of stasis. From observation of a clinician's point of view, the liquid in liquid emboli, such as amniotic fluid emboli, appears to be awkward, but a slight understanding of fluid kinematics of the situation would clear the perception. The viscosity of the amniotic fluid is 1.17centimeter poise (cP). Blood viscosity is, however, variable as it is a Non-Newtonian fluid. It's to be noted that amniotic embolic only happens in women with eclampsia or pre-eclampsia. These subjects have immense hypertension. In such conditions, naturally, hematocrit count increases, and clinical research have effectively found that increased hematocrit count highly increases blood viscosity, ranging from 1.81cP – 7.84cP. In such conditions, the amniotic fluid stays no more buoyant in maternal blood, resulting in droplet formation of amniotic fluid in maternal blood, termed as emboli.
Hypertension is a frequent and clinically significant disorder, engulfing patients from all strata of society and almost every age group in today's world. Clinically it is divided into three stages; stage 1 hypertension with a barometric pressure reading of 130-139/80-89mm Hg, stage 2 hypertension with a barometric pressure reading of 140/
140/  90, and stage 3 hypertension or hypertensive crisis with barometric pressure reading of >180/>120. The causes of such disorders are – high sodium salt intake, high fat intake, increased levels of LDL and VLDL in blood circulation, diabetes, genetic predisposition, etc. These, factors as might be understood by our findings – increase the 'latent shear force" of blood.
90, and stage 3 hypertension or hypertensive crisis with barometric pressure reading of >180/>120. The causes of such disorders are – high sodium salt intake, high fat intake, increased levels of LDL and VLDL in blood circulation, diabetes, genetic predisposition, etc. These, factors as might be understood by our findings – increase the 'latent shear force" of blood.
Myocardial Infarction (MI) is mainly attributed due to obstruction of the coronary arteries of the heart. Obstruction due to LDL and VLDL and subsequent plaque formation resulting in lack of oxygen into cardiomyocytes is understandable. But a clinically significant and specific variant of MI with no coronary obstruction with absolutely fine angiography and electrocardiogram report is also evident. This is called MI with no obstructive coronary atherosclerosis (MINOCA). Theories of vasospasm, renal impairment, emboli have been put forward. But it has to be understood that whatever the underlying cause might be, it is not the pathophysiology. From a pathophysiological aspect, such things result from increased latent shear force, resulting in pressure increment and change in fluid character towards turbulence as per Samajpaty-Reynold's condensate equation (leading to vasospasm, renal disturbance, etc.)
Discussion
The paper deals with the detailed evaluation of the new formula given by Samajpaty and Ray. It aims at extending the conception of hemo-mechanics and evaluates its clinical sustainability. Aortic aneurysm and its recurrence are a huge problem in the clinical world. Throughout the world, theoretical and clinical researchers have tried their level best to overcome the lapse of the surgical outcome but with unsatisfactory effect [7, 8]. Using principles of hemo-mechanics, we have put forward how aneurysm surgery patch has to be designed keeping in mind the formula three and elasticity matching of the aorta with the patch keeping in concern the formula 13 for depression of the aortic wall and the formula 15 for assessing the factor of allowance of volumetric expansion and ten as well for pressure maintenance. The four laws of hemo-mechanics that have been put forward effectively explain the principle of therapy and surgery in pathoanatomical changes caused due to change like blood flow.
Review of gas gangrene has made a path-breaking discovery in co-relating thermodynamic barriers and changes in such pathology [11]. The equations 20, 22, 25, 31 have explained how gases from the dissolved state in the blood come out in a gaseous state and conjure up the dreadful pathological situation. Management keeping Gibb's energy change in mind might prove highly effective in the therapy of such diseases. Further, light has been given on the etiology of gas gangrene apart from the already known bacteria which causes it. Drainage catheters constructed in the principle of reversing the situation of Ggas > Gdis might prove highly effective in therapy. The review of emboli is unique in its character. The review under the auspices of the principles of hemo-mechanics has shown that buoyancy is the principal factor of fluid (liquid/gas) in fluid emboli. It has shown how emboli cause blood turbulence by the formula of the 4th law of hemo-mechanics (Equation 17) and has demonstrated the claim with significant clinically proven research data. It has demonstrated that in the delivery of women with pre-eclampsia or eclampsia, hypertension causing change in blood viscosity might cause amniotic emboli in the 2nd or 3rd stage of labor. Indicating vasodilation with sodium nitroprusside intravenous or methyl dopa in patients with such history before delivery might solve this issue and provide the woman a safe and happy post-partum period, followed by a normal lifestyle.
At last, it also has to be noted that intensive practical work in the newly discovered field of hemo-mechanics has to be done. Determination of radius, length, circumference, and other geometrical parameters and physical parameters like Young's modulus and Bulk's modulus has to be made to take advantage of this theory in the clinics [17, 18]. Initially, such experiments might be done in fresh cadavers by inflating the blood vessels with vicious gas from outside using a catheter, and results might be noted using ultrasonography improvisation. Once all data are available, the software can give clinical data to the medical personnel in charge. This would effectively improve hospital management and reduced patient fatality as well. Lack of data is the main hindrance in completely implementing the theory in the clinical scenario.
Rapid clinical research has to be carried out for using the fruit of such a unique theory. Bringing it to clinical practice is the ultimate ambition behind the findings. The paper helps in understanding blood flow in more detail and its mechanical physics, which is essential for the effective understanding of medical students and doctors worldwide. Review of pathology under the auspices of the principles of hemo-mechanics is a unique approach to understand the pathological process of hemodynamic diseases and initiate rapid research and development of the clinical material suggested under the principles. A mathematical conclusion has been reached regarding the blood pressure of the aorta. Although it might look like an improper proposition from the first instance, such possibilities are ruled out completely once the logical-mathematical analysis is reached. The pressure obtained by trans-thoracic catheterization cannot be specifically Aortic blood pressure as it fails to isolate the aorta as a closed system vessel. In such a technical glitch, the high blood pressure reading is obtained, which might be an additive effect of already accumulated fluid inside the heart and a highly time-efficient ongoing cardiac cycle.
This article has made an additional discussion and formula change for elastic blood vessels such as the aorta and pulmonary trunk and vessels. Samajpaty & Ray's article has time and again spoken about software development based on this scale [1]. It is thus again being stressed, hereby. Such software in the nursing station of a hospital ward would highly increase nursing efficiency, and personalized blood pressure data of each patient can be easily recorded and stored by this method for almost all the blood vessels of the body. But before such a step, it's mandatory to conduct forensic research and determine all the formula parameters as per equation (like radius and length) for all necessary blood vessels by inflation [21, 22]. Apart from these, a thorough discussion of the pathology of blood has been made. The focus was primarily on unexplained hemato-pathologies. Explanation and probable solution of such have been given.
Conclusion
The four laws of hemo-mechanics derived here help better understand normal blood physiology, hematology, blood pressure in a broader aspect, and the co-relation of gravitational force with the blood flow in terms of fluidity. The new device sheer scale for blood vessels is of utmost importance. Bringing it into application would reduce nursing time and un-understandable mishaps of bleeding during surgery.
Acknowledgments: There is nothing to be declared.
Ethical Permissions: There is nothing to be declared.
Conflicts of Interests: There is nothing to be declared.
Authors’ Contribution: Samajpaty S., Introduction Writer/Methodologist/Main Researcher/Discussion Writer (100%).
Funding/Support: There is nothing to be declared.
Hemodynamic disorders have been effectively explained by the principles of general pathology and chemical physiology. But now, we would leap a step forward and try to analyze the perspectives from a physics point of view, utilizing the principles of Hemo-mechanics. Any injury to the tissue causes an inflammatory reaction. Inflammation is initiated by inflammation mediator chemical compounds. The symptoms classically being – redness, heat, pain, edema, and loss of function. Histamine is released by mast cells located adjacent to the blood vessel, basophils, and platelets. This causes dilation of arterioles and increases venule permeability. Serotonin is released by mast cells when platelet-aggregates contact collagen, resulting in the same as Histamine.
On the other hand, Nitric oxide (NO) synthesized from enzyme nitric oxide synthase (NOS) is released, which acts as a pleiotropic inflammation mediator of inflammation and endothelial smooth muscle relaxing agent. Apart from this, because of injury, there is the breakdown of Arachidonic acid, which results in prostaglandin release. It is to be remembered that the fluid mobility between blood vessels and tissue occurs in the capillary bed. Vasoactive amines, C3a and C5a, Leukotrienes C4, D4, E4, PAF, and Substance P cause an increment in vascular permeability of the capillary walls. The game of pressure in the capillary bed has been effectively mentioned by Starling's equation. We would focus on dynamic and
Now, if an area of a capillary tube increase to A/ and "latent shear force" is also increased due to secretion of multiple chemical factors into circulation, some being described above. So, if the increased latent shear force is ꞙ/, the Bulk modulus can be expressed as Equations 14 and 15. Where: ΔV is the volume change of the capillary and Vo is the initial volume of the capillary. By general definition, the entropy (S) of the unit volume of the blood system will also increase. Resulting in an increment in heat (Q), the temperature being fixed in the same environment. This, again, validates that the capillary process is diabetic. Since (Equation 23):

Where: S is entropy, Q is heat, and T is temperature. On the other hand, an increased entropy will ensure increased freedom of movement across the capillary walls. This results in edema. Thus, putting the mechanical explanation of edema formation forwards. To compare the statement with that of Starling's, capillary hydrostatic pressure increases in the explanation. Naturally, if ꞙ is increased, hydrostatic capillary pressure will also be increased. But effective filtration in case of edema is however increased because of increased capillary oncotic pressure. Starling's equation states that (Equation 24):

where; Jv = fluid movement (ml/min), Kf = hydraulic conductance (ml/min/mm Hg), Pc = capillary hydrostatic pressure (mm Hg), Pi = Interstitial hydrostatic pressure (mm Hg), πc = capillary oncotic pressure (mm Hg) and πi = Interstitial hydrostatic pressure (mm Hg). From the above-stated analogical observation, it's evident that latent shear is directly proportional to hydrostatic capillary pressure and oncotic capillary pressure. Thus (Equation 25):

Gas gangrene is not a hemodynamic disorder, but we would focus on this subject as it involves blood, and the gases found in gas gangrene have such composition – Nitrogen 74.5%, Oxygen 16.1%, Hydrogen 5.9%, and Carbon dioxide 3.4% approximately. But pathologists have failed to explain where and how such a huge gas accumulation occurs inside a human body under the deep fascia. Gas gangrene is specifically caused by infection of Clostridium sp. of multiple strains like C. novyi, C. septicum, C. bifermentans, C. fallax, and C. sordelii by order of prevalence. These bacteria release very fast-acting toxins; alpha-toxin (tissue destruction), beta toxin (tissue necrosis), delta toxin (hemolysin), epsilon toxin (acts like permease that increases cell membrane permeability), iota toxin (tissue necrosis), kappa toxin (acts as collagenase, gelatinase, specifically destroys blood vessel), lambda toxin (protease), mu toxin (hyaluronidase), nu toxin (deoxyribonuclease, hemolytic and necrosis of tissue), and phi toxin (hemolysin and cytolysin as per the finding of C. perferinges). It would be hypothesized and proved with the help of principles of fluid (hemo-) mechanics and applied mathematics that all these gases arise from blood.
The gases mentioned above stay in the dissolved condition in the blood (not liquid but dissolved) under high pressure of the blood vessel at normal conditions. An injury of simple type or any other bacteria does not evolve into gas gangrene for two reasons-(i) all injuries do not cause complete endothelial rupture, and (ii) other bacterial toxins do not initiate spontaneous destruction of the vessel endothelium. The gases under compressed conditions stay dissolved inside the blood vessel, but once the vessel wall is destroyed with such spontaneous action, there is a sudden huge change in pressure of the thermodynamic system in which the gases were until now. Decompression and exposure to a lower pressure of the body cavity or atmosphere (lower) lead to gas formation, and gangrene is simply due to toxin-led necrosis. This gas gets trapped in between fascias and layers in the body. The whole thing is analogical to the sudden opening of an aerated soda can.
If chemical potential energy = μ, Gibb's free energy = G and number of moles = N. We know (Equation 26):

Now, one gas has μ chemical potential energy. Thus, 'n' gases have (μ1+μ2+μ3+ …… +μn) chemical potential energy; similarly, for 'n' gases, there are (N1+N2+N3+ ……. + Nn) moles. So, if Gibb's energy for a dissolved state is represented as Gdis and that of gases state as Ggas, then, for a dissolved state (Equation 28):


Any chemical change is quantified by Gibb's free energy. Simply Ggas has to be greater than Gdis for favoring gas formation. Clinicians have opted for different methods for reducing mortality due to gas gangrene. However, the reason was not very clear behind the situation. An approach of vacuum sealing along with drainage technology has shown a very efficient therapy procedure. The vacuum helps in sucking out the gas formed inside the cavity or abscess. The pathology proceeds very fast, and that's the reason gas production happens spontaneously, by maintaining the thermodynamic parameters.
Emboli is a detached intravascular solid, liquid, or gaseous mass that is transported in the bloodstream to sites away from the place of its origin. This can be thrombus, fat globule or gas bubble, or liquid in liquid embolism, as in the case of amniotic fluid emboli. Until now, the explanation of emboli was very speculative. But in the light of the "latent shear force" of blood postulate and principles of hemo-mechanics, a far-worthy explanation might be put forward. Emboli happen mainly when there is the fulfillment of Virchow's triad. Virchow triad might be caused by many factors; stenosis of valves, calcium and oxalate deposits in the blood-heat circulation system. It comprises three factors in the triad – (i) endothelial injury, (ii) stasis, and (iii) hypercoagulability.
It is to be noted that such pathology will be proceeded by changed blood continuum composition by the influx of inflammatory mediators, cytokines, chemokines, increased volume of metabolic products, etc. This will increase the modulus value of the "latent shear force" of blood—the viscosity of the blood, on the other hand, increases due to hemodilution and blood vessel dilation. Hence, applying the 4th law of Hemo-mechanics (Equation 17). The conclusion might be reached that when other parameters are almost constant (Equation 32):

Hence, turbulence in the blood flow will be noticeable when observed under Doppler ultrasonography. This is not just a mathematical assumption but is verified by clinical research– turbulence was observed in cerebral emboli, and the turbulence proportionate with the degree of stasis. From observation of a clinician's point of view, the liquid in liquid emboli, such as amniotic fluid emboli, appears to be awkward, but a slight understanding of fluid kinematics of the situation would clear the perception. The viscosity of the amniotic fluid is 1.17centimeter poise (cP). Blood viscosity is, however, variable as it is a Non-Newtonian fluid. It's to be noted that amniotic embolic only happens in women with eclampsia or pre-eclampsia. These subjects have immense hypertension. In such conditions, naturally, hematocrit count increases, and clinical research have effectively found that increased hematocrit count highly increases blood viscosity, ranging from 1.81cP – 7.84cP. In such conditions, the amniotic fluid stays no more buoyant in maternal blood, resulting in droplet formation of amniotic fluid in maternal blood, termed as emboli.
Hypertension is a frequent and clinically significant disorder, engulfing patients from all strata of society and almost every age group in today's world. Clinically it is divided into three stages; stage 1 hypertension with a barometric pressure reading of 130-139/80-89mm Hg, stage 2 hypertension with a barometric pressure reading of
 140/
140/  90, and stage 3 hypertension or hypertensive crisis with barometric pressure reading of >180/>120. The causes of such disorders are – high sodium salt intake, high fat intake, increased levels of LDL and VLDL in blood circulation, diabetes, genetic predisposition, etc. These, factors as might be understood by our findings – increase the 'latent shear force" of blood.
90, and stage 3 hypertension or hypertensive crisis with barometric pressure reading of >180/>120. The causes of such disorders are – high sodium salt intake, high fat intake, increased levels of LDL and VLDL in blood circulation, diabetes, genetic predisposition, etc. These, factors as might be understood by our findings – increase the 'latent shear force" of blood.Myocardial Infarction (MI) is mainly attributed due to obstruction of the coronary arteries of the heart. Obstruction due to LDL and VLDL and subsequent plaque formation resulting in lack of oxygen into cardiomyocytes is understandable. But a clinically significant and specific variant of MI with no coronary obstruction with absolutely fine angiography and electrocardiogram report is also evident. This is called MI with no obstructive coronary atherosclerosis (MINOCA). Theories of vasospasm, renal impairment, emboli have been put forward. But it has to be understood that whatever the underlying cause might be, it is not the pathophysiology. From a pathophysiological aspect, such things result from increased latent shear force, resulting in pressure increment and change in fluid character towards turbulence as per Samajpaty-Reynold's condensate equation (leading to vasospasm, renal disturbance, etc.)
Discussion
The paper deals with the detailed evaluation of the new formula given by Samajpaty and Ray. It aims at extending the conception of hemo-mechanics and evaluates its clinical sustainability. Aortic aneurysm and its recurrence are a huge problem in the clinical world. Throughout the world, theoretical and clinical researchers have tried their level best to overcome the lapse of the surgical outcome but with unsatisfactory effect [7, 8]. Using principles of hemo-mechanics, we have put forward how aneurysm surgery patch has to be designed keeping in mind the formula three and elasticity matching of the aorta with the patch keeping in concern the formula 13 for depression of the aortic wall and the formula 15 for assessing the factor of allowance of volumetric expansion and ten as well for pressure maintenance. The four laws of hemo-mechanics that have been put forward effectively explain the principle of therapy and surgery in pathoanatomical changes caused due to change like blood flow.
Review of gas gangrene has made a path-breaking discovery in co-relating thermodynamic barriers and changes in such pathology [11]. The equations 20, 22, 25, 31 have explained how gases from the dissolved state in the blood come out in a gaseous state and conjure up the dreadful pathological situation. Management keeping Gibb's energy change in mind might prove highly effective in the therapy of such diseases. Further, light has been given on the etiology of gas gangrene apart from the already known bacteria which causes it. Drainage catheters constructed in the principle of reversing the situation of Ggas > Gdis might prove highly effective in therapy. The review of emboli is unique in its character. The review under the auspices of the principles of hemo-mechanics has shown that buoyancy is the principal factor of fluid (liquid/gas) in fluid emboli. It has shown how emboli cause blood turbulence by the formula of the 4th law of hemo-mechanics (Equation 17) and has demonstrated the claim with significant clinically proven research data. It has demonstrated that in the delivery of women with pre-eclampsia or eclampsia, hypertension causing change in blood viscosity might cause amniotic emboli in the 2nd or 3rd stage of labor. Indicating vasodilation with sodium nitroprusside intravenous or methyl dopa in patients with such history before delivery might solve this issue and provide the woman a safe and happy post-partum period, followed by a normal lifestyle.
At last, it also has to be noted that intensive practical work in the newly discovered field of hemo-mechanics has to be done. Determination of radius, length, circumference, and other geometrical parameters and physical parameters like Young's modulus and Bulk's modulus has to be made to take advantage of this theory in the clinics [17, 18]. Initially, such experiments might be done in fresh cadavers by inflating the blood vessels with vicious gas from outside using a catheter, and results might be noted using ultrasonography improvisation. Once all data are available, the software can give clinical data to the medical personnel in charge. This would effectively improve hospital management and reduced patient fatality as well. Lack of data is the main hindrance in completely implementing the theory in the clinical scenario.
Rapid clinical research has to be carried out for using the fruit of such a unique theory. Bringing it to clinical practice is the ultimate ambition behind the findings. The paper helps in understanding blood flow in more detail and its mechanical physics, which is essential for the effective understanding of medical students and doctors worldwide. Review of pathology under the auspices of the principles of hemo-mechanics is a unique approach to understand the pathological process of hemodynamic diseases and initiate rapid research and development of the clinical material suggested under the principles. A mathematical conclusion has been reached regarding the blood pressure of the aorta. Although it might look like an improper proposition from the first instance, such possibilities are ruled out completely once the logical-mathematical analysis is reached. The pressure obtained by trans-thoracic catheterization cannot be specifically Aortic blood pressure as it fails to isolate the aorta as a closed system vessel. In such a technical glitch, the high blood pressure reading is obtained, which might be an additive effect of already accumulated fluid inside the heart and a highly time-efficient ongoing cardiac cycle.
This article has made an additional discussion and formula change for elastic blood vessels such as the aorta and pulmonary trunk and vessels. Samajpaty & Ray's article has time and again spoken about software development based on this scale [1]. It is thus again being stressed, hereby. Such software in the nursing station of a hospital ward would highly increase nursing efficiency, and personalized blood pressure data of each patient can be easily recorded and stored by this method for almost all the blood vessels of the body. But before such a step, it's mandatory to conduct forensic research and determine all the formula parameters as per equation (like radius and length) for all necessary blood vessels by inflation [21, 22]. Apart from these, a thorough discussion of the pathology of blood has been made. The focus was primarily on unexplained hemato-pathologies. Explanation and probable solution of such have been given.
Conclusion
The four laws of hemo-mechanics derived here help better understand normal blood physiology, hematology, blood pressure in a broader aspect, and the co-relation of gravitational force with the blood flow in terms of fluidity. The new device sheer scale for blood vessels is of utmost importance. Bringing it into application would reduce nursing time and un-understandable mishaps of bleeding during surgery.
Acknowledgments: There is nothing to be declared.
Ethical Permissions: There is nothing to be declared.
Conflicts of Interests: There is nothing to be declared.
Authors’ Contribution: Samajpaty S., Introduction Writer/Methodologist/Main Researcher/Discussion Writer (100%).
Funding/Support: There is nothing to be declared.
Keywords:
References
1. Samajpaty S, Ray S. Innovation strategies in health economics: a force that makes blood move and game of gravity in it-futuristic economic plans. Mosc Econ J. 2020 September. [Link]
2. Paruchuri V, Salhab KF, Kuzmik G, Gubernikoff G, Fang H, Rizzo JA, et al. Aortic size distribution in the general population: explaining the size paradox in aortic dissection. Cardiology. 2015;131(4):265-72. [Link] [DOI:10.1159/000381281] [PMID]
3. Nakayama Y, Tsumura K, Yamashita N, Yoshimaru K, Hayashi T. Pulsatility of ascending aortic pressure waveform is a powerful predictor of restenosis after percutaneous transluminal coronary angioplasty. Circulation. 2000;101(5):470-2. [Link] [DOI:10.1161/01.CIR.101.5.470] [PMID]
4. Umebayashi R, Uchida HA, Wada J. Abdominal aortic aneurysm in aged population. Aging (Albany NY). 2018;10(12):3650-1. [Link] [DOI:10.18632/aging.101702] [PMID] [PMCID]
5. Skydan О, Nykolyuk О, Pyvovar P, Topolnytskyi P. Assessment of the social security level in the context of coronavirus contagion (COVID-19). Sci Horiz. 2020;06(91):7-18. [Link]
6. Tochii M, Amano K, Sakurai Y, Ishikawa H, Ishida M, Higuchi,Y, et al. Recurrence of aneurysm of the ascending aorta after patch repair: the fate of an aortic patch. Ann Vasc Dis. 2016;9(4):322-5. [Link] [DOI:10.3400/avd.cr.16-00043] [PMID] [PMCID]
7. Vasenko O, Zinchenko I, Tsytlishvili K, Bikasov V. Research of methods of inactivation of the antibiotic cyprofloxacin in order to prevent environmental pollution and protect human health. Sci Horiz. 2020;7(92):19-25. [Link] [DOI:10.33249/2663-2144-2020-92-7-19-25]
8. Tsaplin GV, Grishin SS, Baberkina EP, Popkov SV, Talismanov VS, Karmanova OG, et al. Investigation and optimization synthesis pathway of antibacterial drug ethonium. Rasayan J Chem. 2021;14(3):1816-20. [Link] [DOI:10.31788/RJC.2021.1436574]
9. Hymon Ch, Wong WH. Capillary filtration coefficient in the extremities of man in high environmental temperatures. Circ Res. 1968;22(2):251-61. [Link] [DOI:10.1161/01.RES.22.2.251] [PMID]
10. Chi CH, Chen KW, Huang JJ, Chuang YC, Wu MH. Gas composition in Clostridium septicum gas gangrene. J Formos Med Assoc. 1995;94(12):757-9. [Link]
11. Bogaevskaya O, Batrakova I, Slyusar O, Talismanov V. Pharmacogenetic testing: Effectiveness of the use of the indirect anticoagulant warfarin. J Glob Pharma Technol. 2020;12:160-9. [Link]
12. Liu Zh, Zhao D, Wang B. Improved vacuum sealing drainage in the treatment of gas gangrene: a case report. Int J Clinl Exp Med. 2015;8(10):19626-8. [Link]
13. Can Ç, Gulacti U, Kalemci S, Topacoglu H. Investigation of relationship between blood viscosity level and acute pulmonary embolism among adult patients in emergency settings. Int Med J. 2016;23(3):272-4. [Link]
14. Yang Y, Grosset DG, Li Q, Shuaib A, Lees KR. Turbulence and circulating cerebral emboli detectable at Doppler ultrasonography: a differentiation study in a stenotic middle cerebral artery model. AJNR Am J Neuroradiol. 2002;23(7):1229-36. [Link]
15. Rosati P, Pola P, Riccardi P, Flore R, Tondi P, Bellati U. The use of amniotic fluid viscosity measurements to establish fetal lung maturity. Int J Gynecol Obstet. 1991;35(4):351-5. [Link] [DOI:10.1016/0020-7292(91)90672-R]
16. Pirofsky B. The determination of blood viscosity in man by a method based on Poiseuille's law. J Clin Invest. 1953;32(4):292-8. [Link] [DOI:10.1172/JCI102738] [PMID] [PMCID]
17. Talismanov VS, Popkov SV, Karmanova OG, Zykova SS, Shustov MV, Zhuravleva LA, et al. 3-(imidazol-1-yl)propane-1,2-diol and 3-(1,2,4-triazol-1-yl)propane-1,2-diol: Synthesis and their transformation to bioactive cyclic ketals. Rasayan J Chem. 2021;14(3):1711-16. [Link] [DOI:10.31788/RJC.2021.1436537]
18. Haghpanahi M, Salmanzadeh MS. A 3D simulation and experimental in-vitro study of magnetic fluid hyperthermia in a tissue containing micro and macro blood perfusions. Iran J War Public Health. 2011;3(3):45-53. [Persian] [Link]
19. Ziaolhagh J, Choobineh S, Gaeini A, Alizadeh M, Arab M. The effect of carbohydrate meals with high or low glycemic index on blood glucose concentration following prolonged strenuous exercise. Iran J War Public Health. 2012;4(2):41-7. [Persian] [Link]
20. Parvizpour F, Ghazanfari T, Salimi H, Faghihzadeh S, Yaraee R, Sharifnia Z, et al. NFκB gene expression survey in peripheral blood cell of Sardasht warfare agent victims 20 years after exposure to sulfur mustard. Iran J War Public Health. 2011;3(4):38-47. [Link]
21. Assaf A, Sakhi R, Michels M, Roos-Hesselink JW, Verhagen JMA, Bhagwandien RE, et al. Implantable loop recorders in patients with heart disease: comparison between patients with and without syncope. Open Heart. 2021;8(2):e001748. [Link] [DOI:10.1136/openhrt-2021-001748] [PMID] [PMCID]
22. Lira-Junior R, Boström EA, Gustafsson A. Periodontitis is associated to increased systemic inflammation in postmyocardial infarction patients. Open Heart. 2021;8(2):e001674. [Link] [DOI:10.1136/openhrt-2021-001674] [PMID] [PMCID]
23. Boyalla V, Jarman JWE, Markides V, Hussain W, Wong T, Mead R.H, et al. Internationally validated score to predict the outcome of non-paroxysmal atrial fibrillation ablation: the 'FLAME score'. Open Heart. 2021;8(2):e001653. [Link] [DOI:10.1136/openhrt-2021-001653] [PMID] [PMCID]
24. Morici N, Tavazzi G. Mechanical circulatory support in CS: device or patient? Open Heart. 2021;8(2):e001733. [Link] [DOI:10.1136/openhrt-2021-001733] [PMID]
25. McPhillips R, Capobianco L, Cooper BG, Husain Z, Wells A. Cardiac rehabilitation patients experiences and understanding of group metacognitive therapy: a qualitative study. Open Heart. 2021;8(2):e001708. [Link] [DOI:10.1136/openhrt-2021-001708] [PMID] [PMCID]