Volume 17, Issue 1 (2025)
Iran J War Public Health 2025, 17(1): 63-74 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2025/01/6 | Accepted: 2025/02/9 | Published: 2025/03/1
Received: 2025/01/6 | Accepted: 2025/02/9 | Published: 2025/03/1
How to cite this article
Ghaffari F, Pishgooie S, Zareiyan A, Sharififar S, Azarmi S. Factors Affecting the Preparedness of Hospital Emergency Department Staff in Responding to Hazardous Materials and Chemical, Biological, Radiological, and Nuclear Incidents. Iran J War Public Health 2025; 17 (1) :63-74
URL: http://ijwph.ir/article-1-1544-en.html
URL: http://ijwph.ir/article-1-1544-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
1- Department of Health in Disasters and Emergencies, Faculty of Nursing, AJA University of Medical Sciences, Tehran, Iran
2- Department of Critical Care, Faculty of Member, AJA University of Medical Sciences, Tehran, Iran
3- Department of Military Nursing, Faculty of Nursing, AJA University of Medical Sciences, Tehran, Iran
2- Department of Critical Care, Faculty of Member, AJA University of Medical Sciences, Tehran, Iran
3- Department of Military Nursing, Faculty of Nursing, AJA University of Medical Sciences, Tehran, Iran
Full-Text (HTML) (794 Views)
Introduction
In recent years, the world has witnessed numerous disasters and calamities. With advancements in technology, the risk of non-natural disasters such as Chemical, Biological, Radiological, and Nuclear (CBRN) incidents has increased, leaving fatal consequences both in terms of human lives and financial costs over several decades. Hazardous Materials (HazMat) and CBRN incidents occur either accidentally or intentionally. These incidents are often unpredictable and invisible, causing fear and anxiety, disrupting social well-being and mental health, and impairing the delivery of healthcare services in the community. Diagnosing symptoms related to CBRN agents is challenging due to the rarity of these incidents and the similarity of their symptoms to other diseases [1-3]. There are national and international concerns regarding CBRN incidents, primarily due to the unexpected nature of these events and the resulting consequences caused by a lack of awareness, resources, planning, and preparedness [4]. Whether intentional or accidental, CBRN incidents are significant from economic, political, social, security, and medical perspectives [5]. The primary concern for people during such incidents is health; Hence, hospitals and healthcare system staff, especially Emergency Departments (ED), are heavily involved [4, 6]. Hospitals bear the brunt of admissions and treatment of affected individuals, and ED serves as the "first gateway" for those needing care [7]. ED staff, referred to as first receivers include doctors, nurses, healthcare specialists, and non-clinical staff [2].
A 2020 study among 308 nurses from selected hospitals in Tehran found that the highest willingness and ability were related to participation in natural disasters like floods and earthquakes, while the lowest willingness and ability were reported for participation in CBRN incidents [8]. Additionally, another study indicated a low likelihood of nurses responding to nuclear/radiological disasters [9].
The potential consequences and costs of unpreparedness for HazMat and CBRN incidents can be immense [10]. Quick and appropriate responses to CBRN incidents can significantly reduce the harmful effects on physical health, decrease mortality, and mitigate the psychological impacts, all of which depend on the preparedness of hospital ED staff [11, 12]. Lack of preparedness can lead to ineffective crisis management, increased fear and anxiety among the public and hospital staff, and potentially inadequate care for the injured, setting the stage for a larger socio-psychological crisis [13]. Preparedness is a significant part of the disaster management cycle. The World Health Organization has identified it as a critical component of sustainable development, emphasizing prior planning and implementation of necessary activities. They have noted that many hospitals are still not adequately prepared for such incidents and face various challenges due to the differing pathophysiology of these events [10, 14]. Hospitals can appropriately respond to nuclear incidents with trained staff [14]. Those responding to these incidents face highly stressful situations that impact their physical and mental health. However, prior planning can minimize these effects and facilitate decision-making [15]. ED staff must prevent contamination by using PPE. Training ED staff about radiation hazards enables them to provide safe care to patients [16]. Despite recognizing the need for emergency preparedness training and programs in the healthcare sector, preparedness levels vary across countries, as does the level of understanding and training among ED staff [17]. Even though hospitals have developed response plans and regularly conduct exercises for HazMat and CBRN incidents in Hong Kong, studies have shown that clinical staff, such as nurses, do not feel adequately prepared and need further training [18]. The role of emergency physicians in preparing for and responding to CBRN and HazMat incidents is crucial worldwide [19].
A report from a medical institute indicated that EDs are better prepared for such incidents than before but still have a long way to go [7, 20]. One challenge for ED staff is the ambiguity in diagnosing the type of contaminant when a patient or victim arrives at the triage area. Another challenge is patient decontamination, which is related to the use of PPE. These are examples of the challenges faced by ED staff in responding to HazMat and CBRN incidents. Training is the only means to enhance the ED's response preparedness for HazMat and CBRN incidents, but it faces obstacles such as staff shortages and frequent relocation of trained staff [2]. Various studies in Iran and worldwide have evaluated hospital preparedness for CBRN incidents, yet differing information exists. Each study has highlighted certain factors affecting hospital staff preparedness, and no comprehensive scoping reviews were found that examined all aspects of ED preparedness for CBRN and HAZMAT incidents. Therefore, the researcher conducted a comprehensive and targeted study to determine the factors that affected the preparedness of ED for HazMat and CBRN incidents. This study employed the scoping review method, utilizing the findings of studies conducted worldwide.
Information and Methods
This article is the result of a scoping review study. The study utilized all five stages proposed by Arksey & O'Malley [21]. Levac et al. recommendations were considered during data charting [22].
Stage 1: Identifying and stating the research questions
This study aimed to determine the factors influencing the preparedness of ED staff in HazMat and CBRN incidents. The following research questions were adopted to guide the review:
1. What factors influence the preparedness of ED staff and their components in facing HazMat and CBRN incidents?
2. What methods can enhance the preparedness of ED staff in facing HazMat and CBRN incidents?
Stage 2: Identifying relevant studies
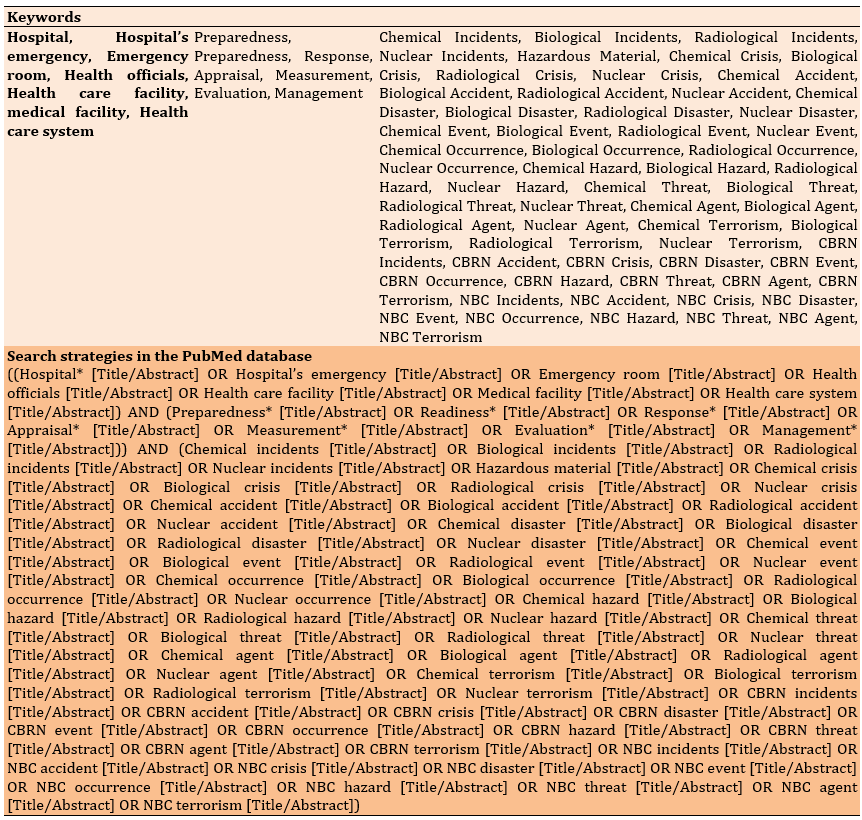
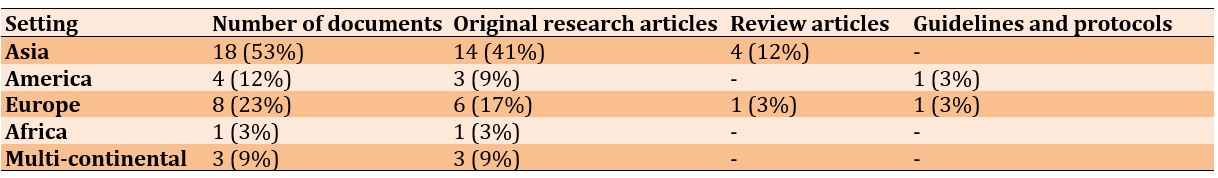
The search components were preparedness, emergency departments, HazMat, and CBRN incidents. The term "staff" was removed from the search process after consulting the research team to maximize the number of articles retrieved. Additionally, after an initial internet search to identify relevant keywords and subject phrases, the Medical Subject Heading (MeSH) website and consultation with relevant specialists were used to determine keywords in Persian and English. The literature search was conducted using Persian and international databases, including Scopus, PubMed, Cochrane Library, Web of Science, ProQuest, and Magiran, from January 1, 2005, to April 1, 2024 (Table 1).
Table 1. Keywords and search strategies
Stage 3: Study selection
In this stage, an overview of the selected articles and sources for the review was provided. After identifying the relevant studies, they were screened for duplicates and assessed for relevance according to the inclusion and exclusion criteria. Inclusion criteria included research results in all countries from January 2005 to April 2024, all research methods, and relevance to the study topic and research question. Exclusion criteria included articles in languages other than English and Persian (due to the researcher's lack of knowledge of languages other than these two), abstracts of seminar and conference articles, articles that assessed the preparedness of emergency and hospital staff other than HazMat and CBRN incidents, and articles that did not meet the required quality according to the statement of Strobe and COREQ. After excluding all articles that did not meet the inclusion criteria, the full texts of all articles that met the criteria were obtained and reviewed. It is important to note that no articles were excluded due to a lack of full-text access to ensure comprehensive coverage of all countries.
Out of the 361 articles and documents gathered during the search, 154 were found to be relevant, and 34 articles were ultimately included in the study. The overall study selection process is illustrated in the PRISMA diagram (Figure 1).
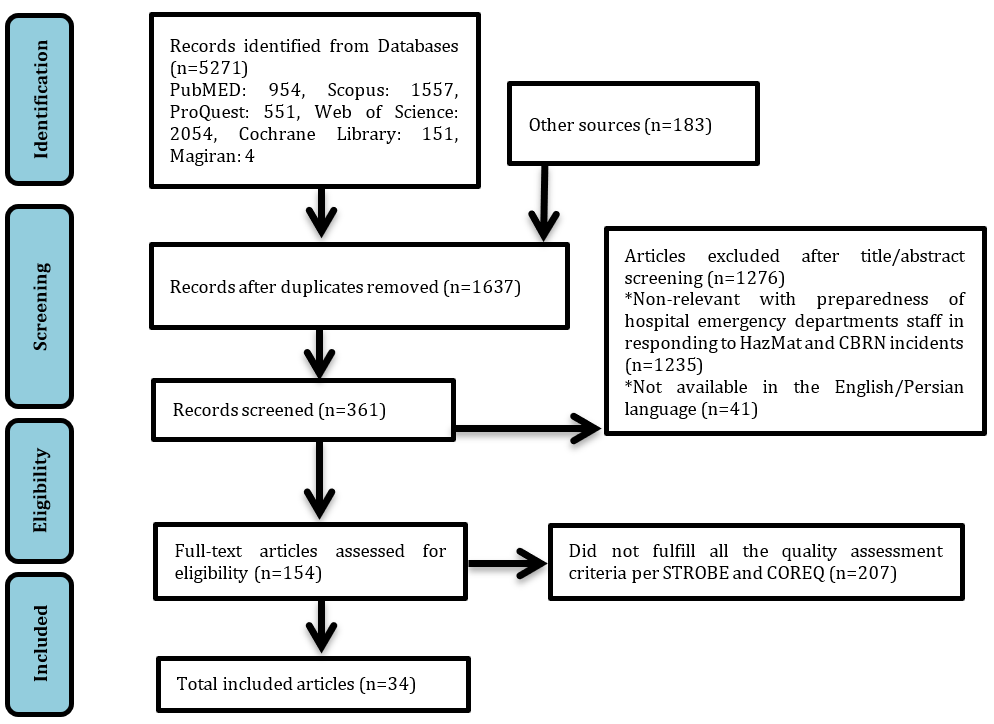
Figure 1. Diagram of the selection process of related articles based on the PRISMA method
Findings
Stage 4: Data charting and synthesis (content analysis)
Quality assessment of studies
The tools for reviewing and assessing the quality of studies and selecting articles eligible for inclusion in the study were evaluated using the STROBE statement and COREQ criteria [23, 24]. Following the quality assessment of articles using these checklists, articles that did not meet the minimum quality standards were excluded from the study. STROBE checklist consisted of 22 items for critiquing observational studies, with the first item on the checklist relating to the title and abstract and the second and third items on the introduction. Items 4-12 related to methodology, items 13-17 related to results, items 18-21 related to discussion, and item 22 related to funding sources. The COREQ checklist consisted of 32 items in three dimensions: Research team and interaction with research units, study design and implementation, data analysis, and results.
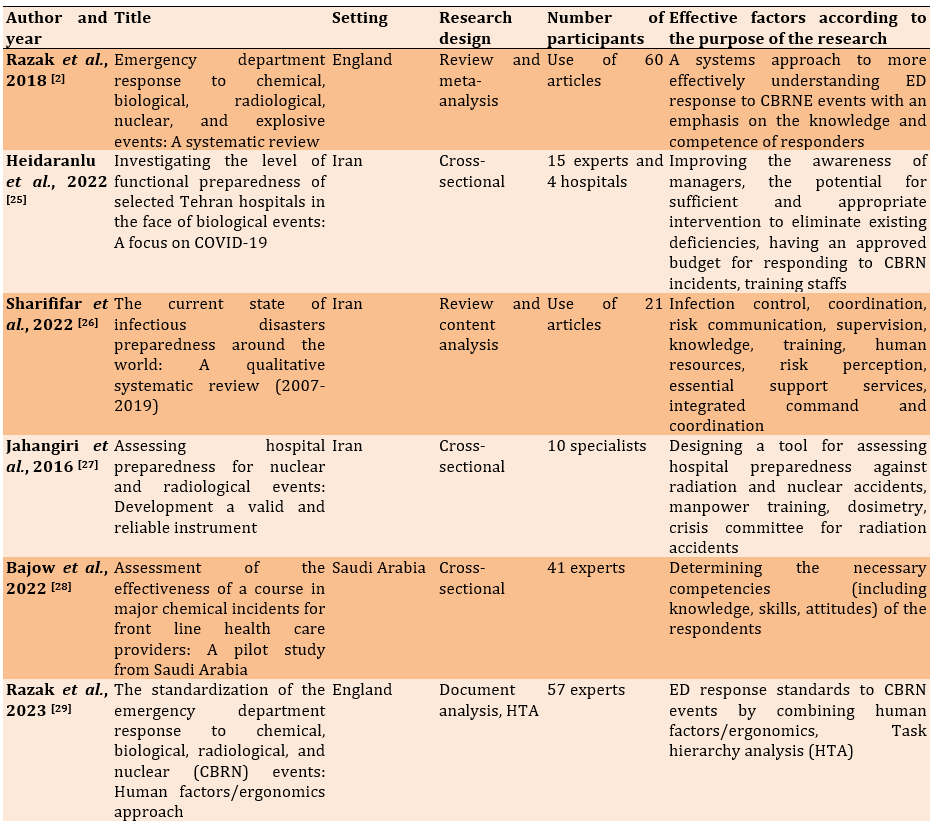
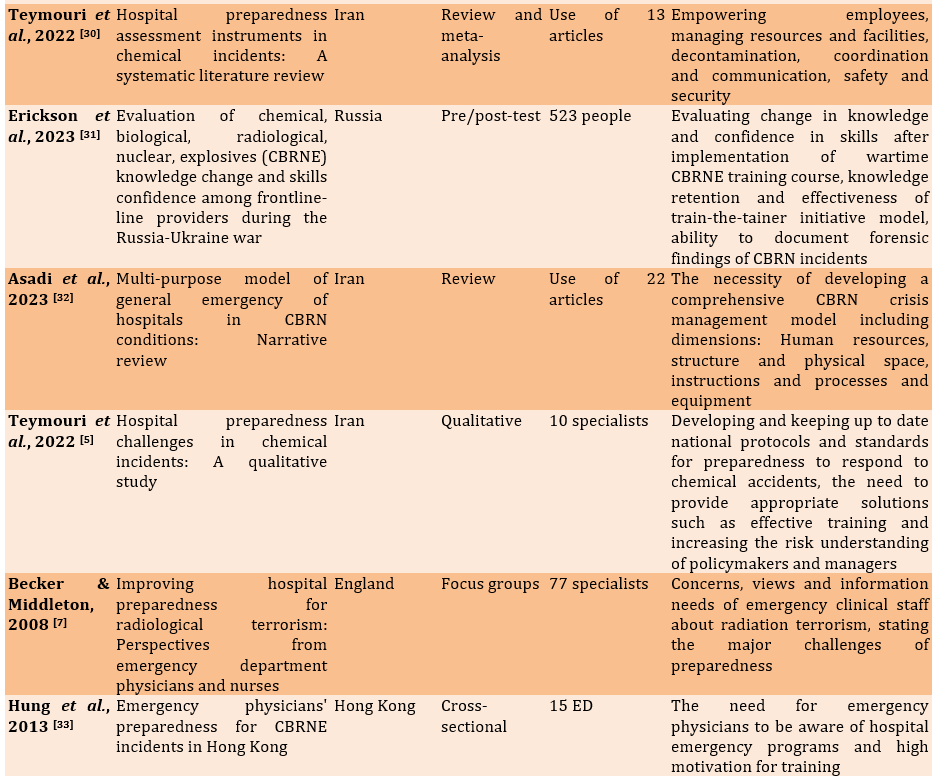
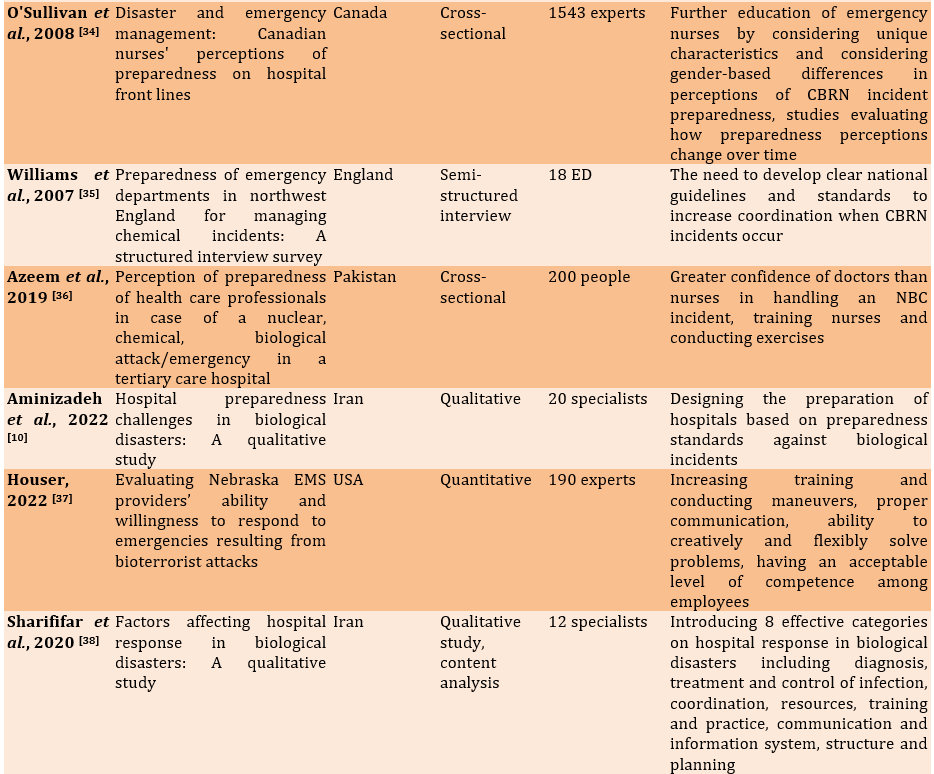
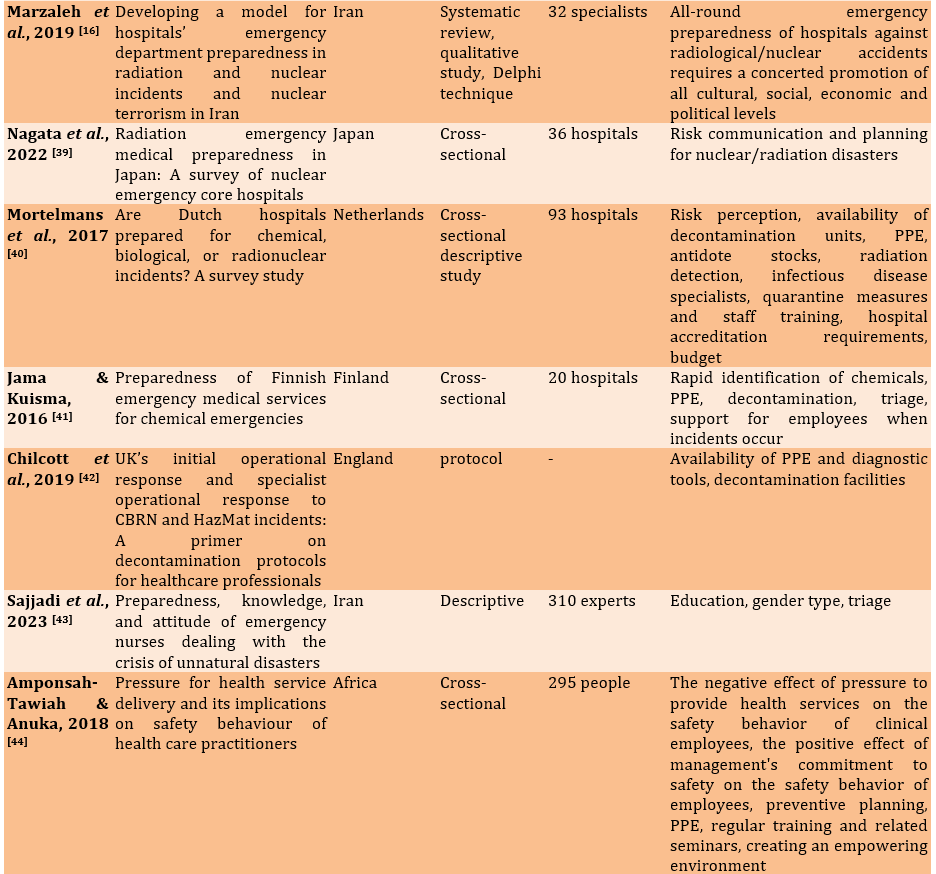
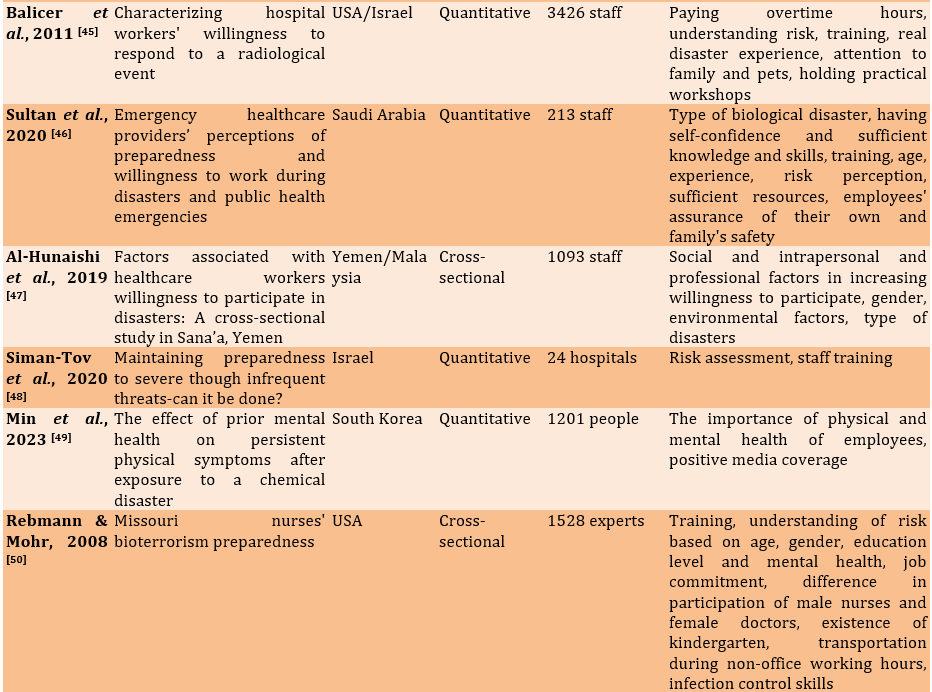
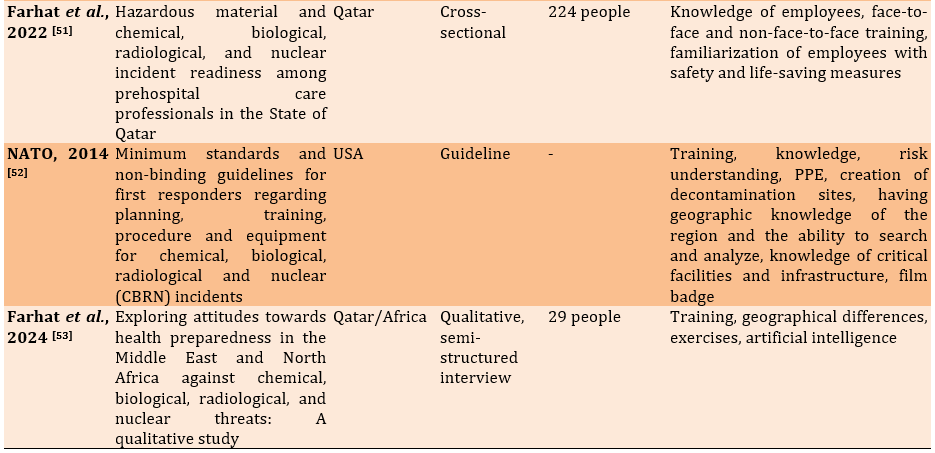
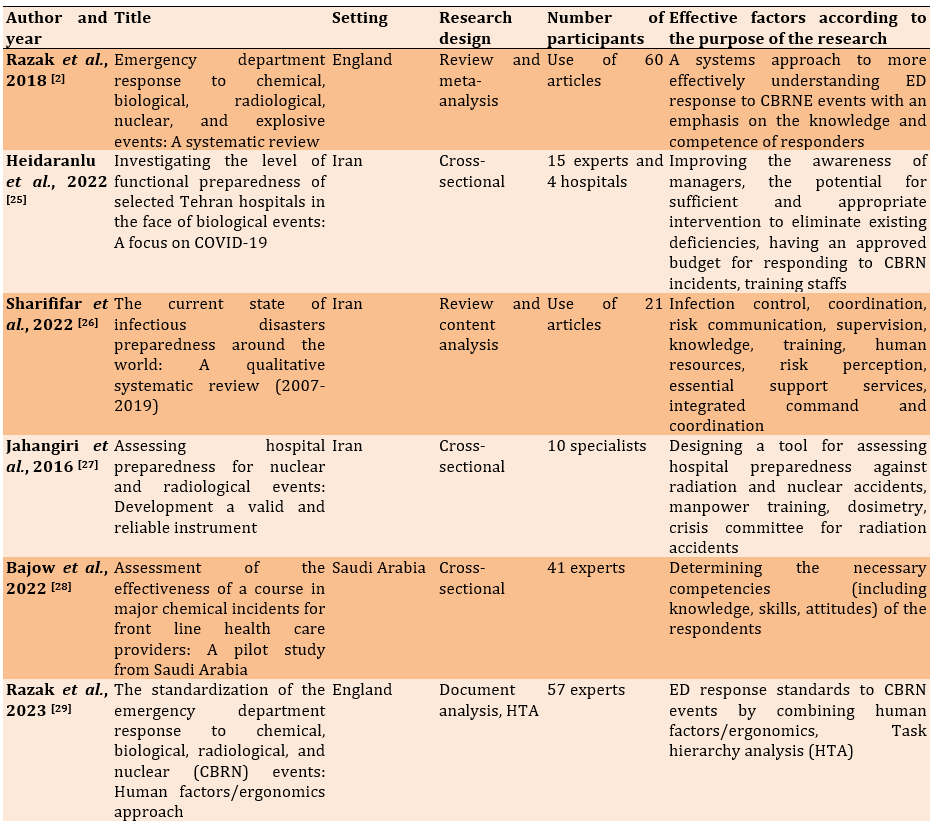
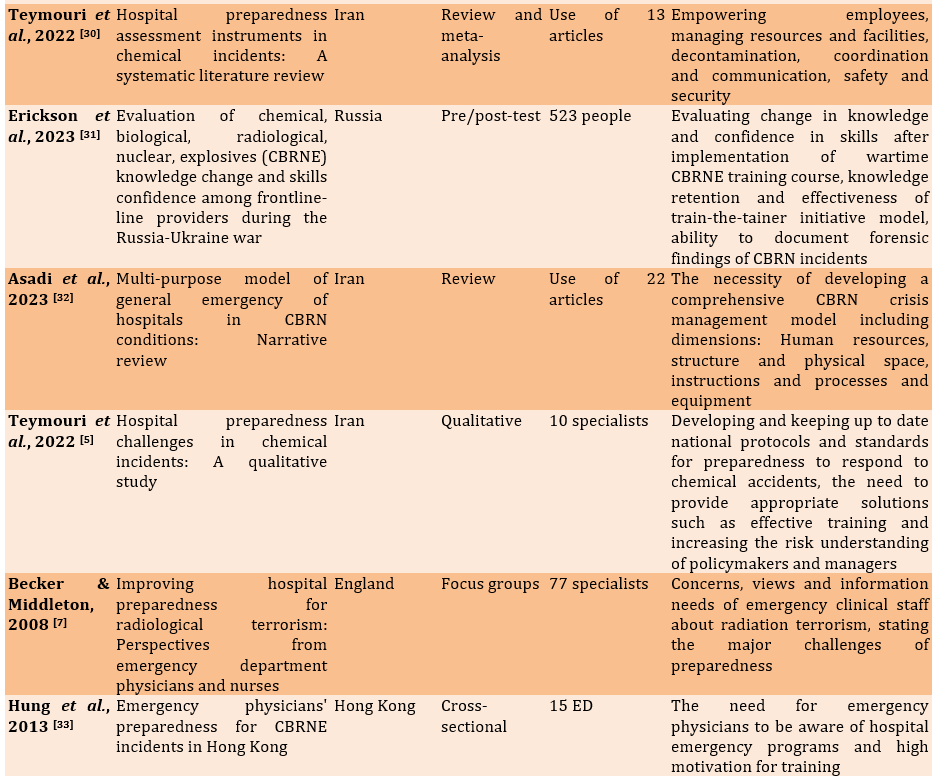
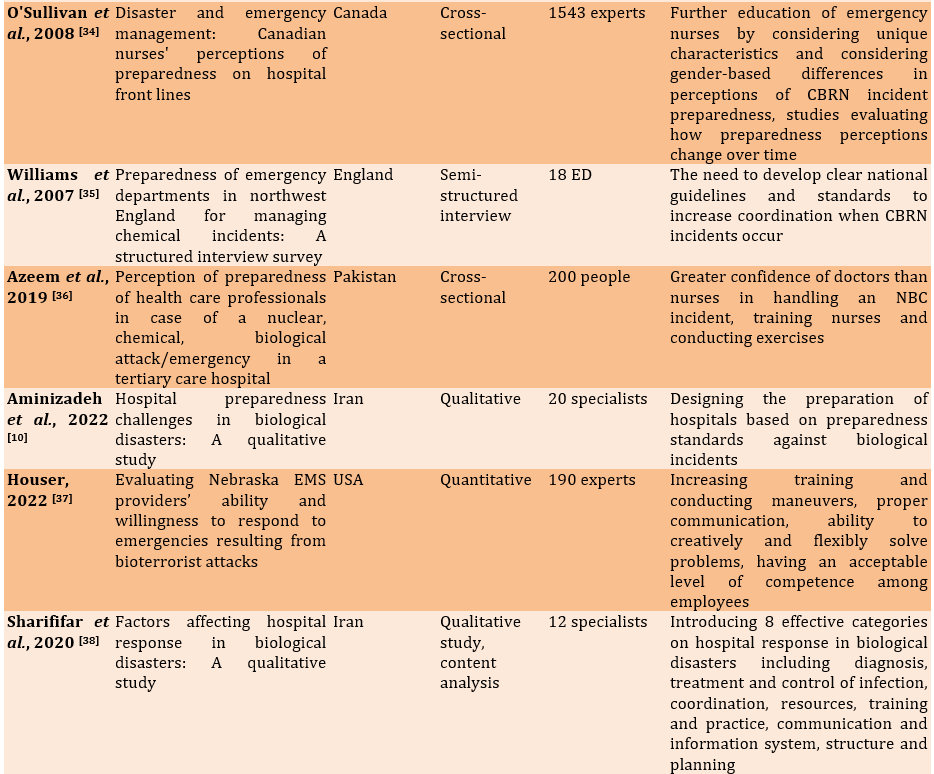
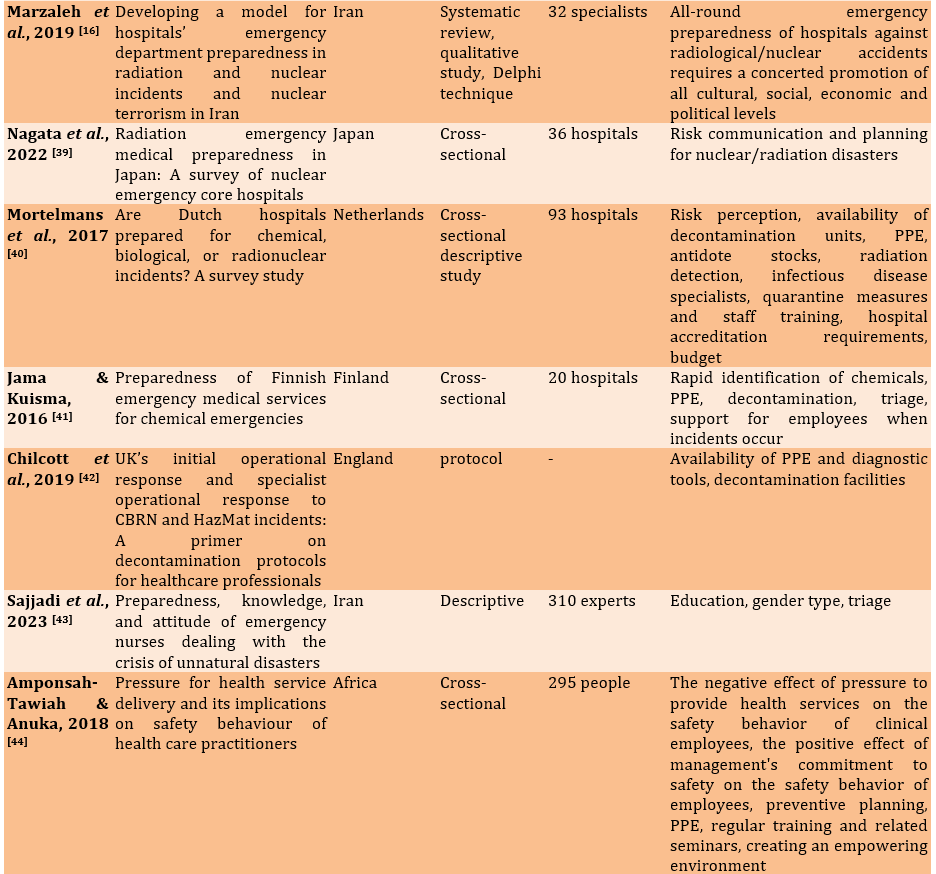
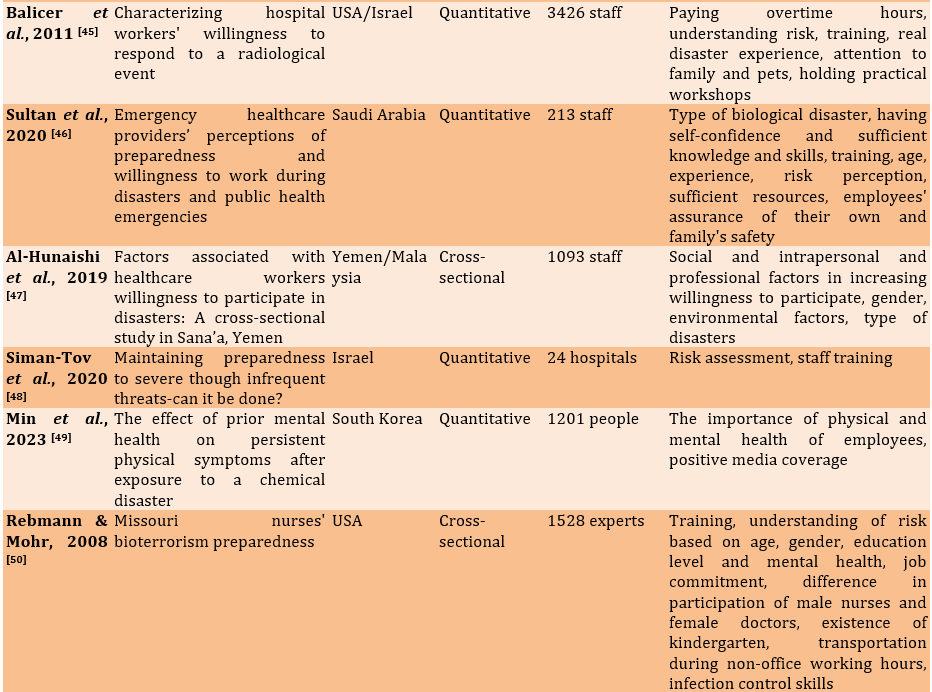
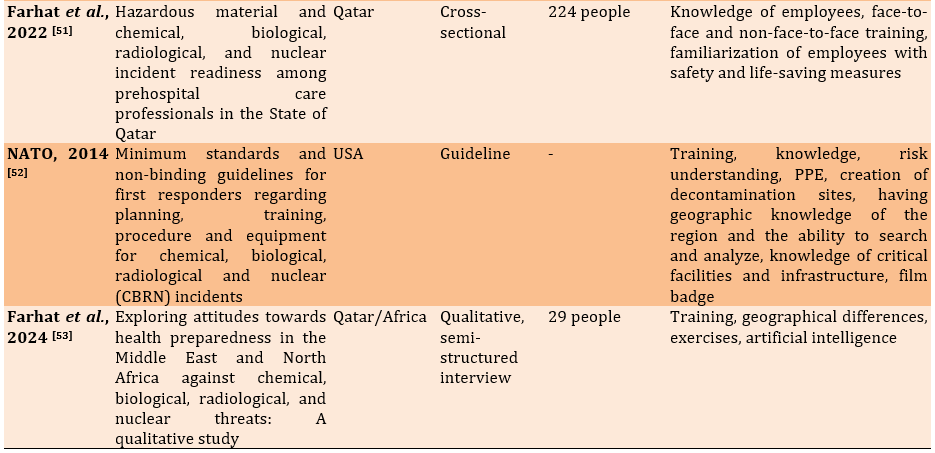
At the end of the search, and after omitting duplicates, 2 research team members screened articles and documents according to their titles and abstracts, considering the inclusion and exclusion criteria. In case of any disagreement, a third author was consulted. In this study, an inter-rater reliability score of 75% was considered. Finally, details of the selected articles, including the first author, year of publication, article title, country, study type, number of participants, and relevant results according to the research objective (factors influencing the preparedness of ED staff in facing HazMat and CBRN incidents) were extracted (Table 2). After completing this form, the results obtained from the review of the articles (content analysis) were summarized and reported.
Table 2. Summary of reviewed studies results
Description of studies
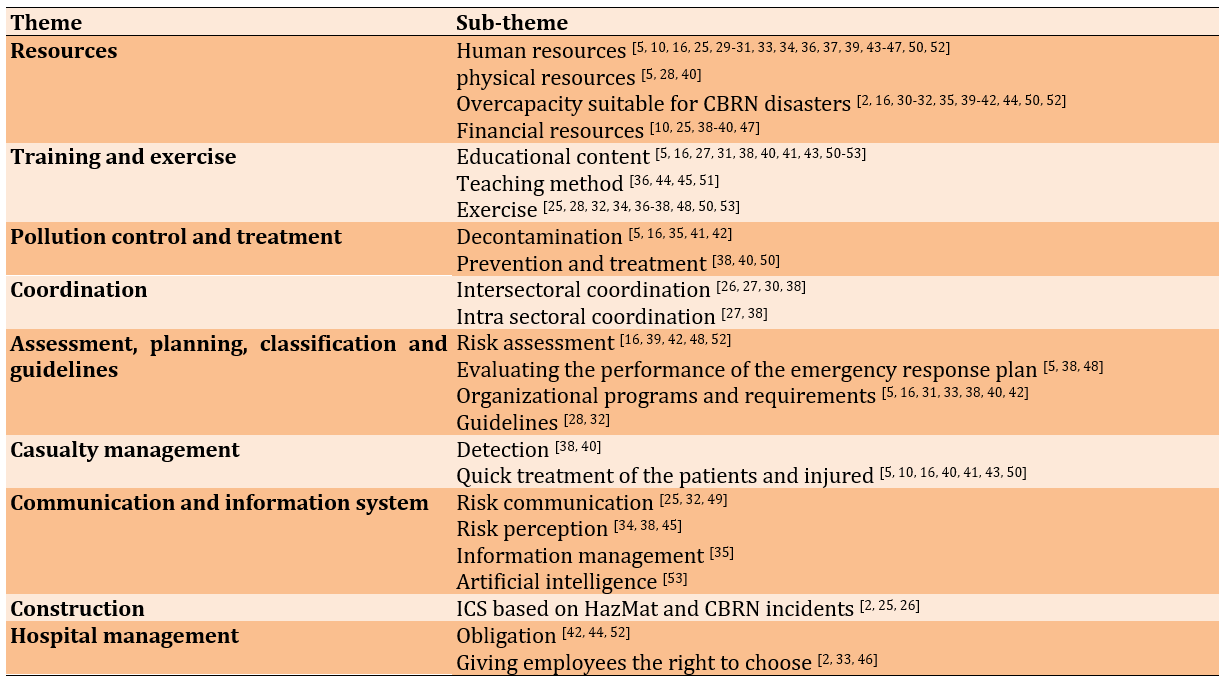
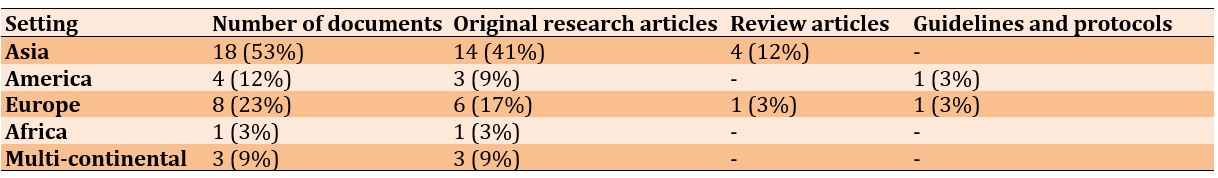
Most of the reviewed articles were cross-sectional research studies. Eighteen articles (53%) were conducted in Asian hospitals, eight articles (23%) in European hospitals, four articles (12%) in hospitals in the Americas, one article (3%) in an African hospital and three articles (9%) involved hospitals across more than one continent. Of the total studies, 79% were research or original articles, 15% were review articles and 6% were guidelines and protocols (Table 3).
Table 3. Number of articles encoded by world region and type of documents
Stage 5: Summarizing and reporting the results
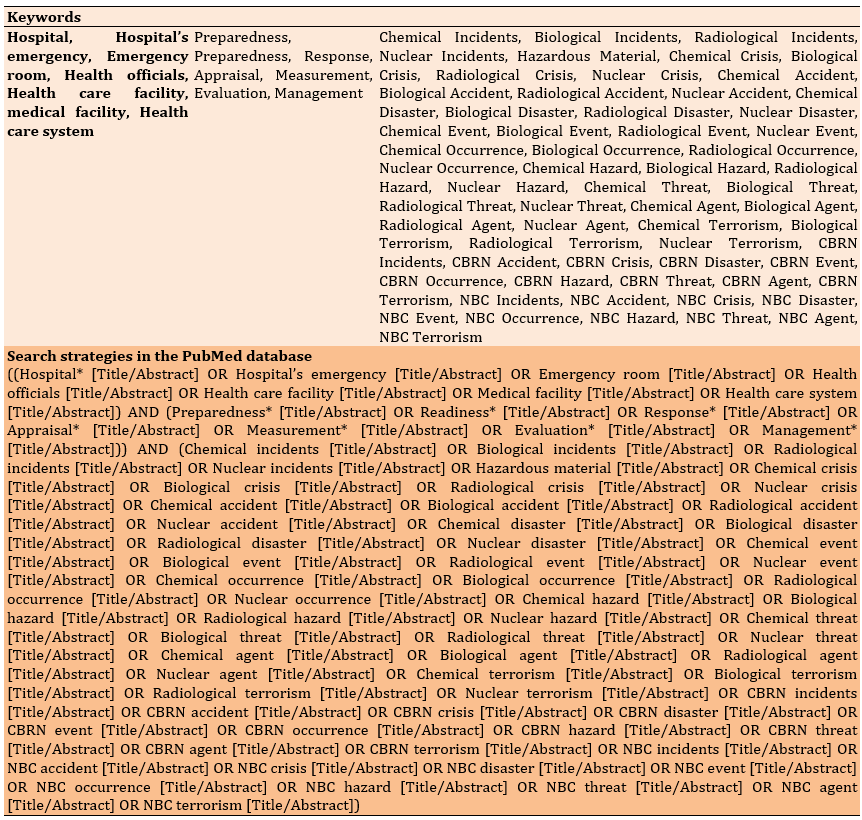
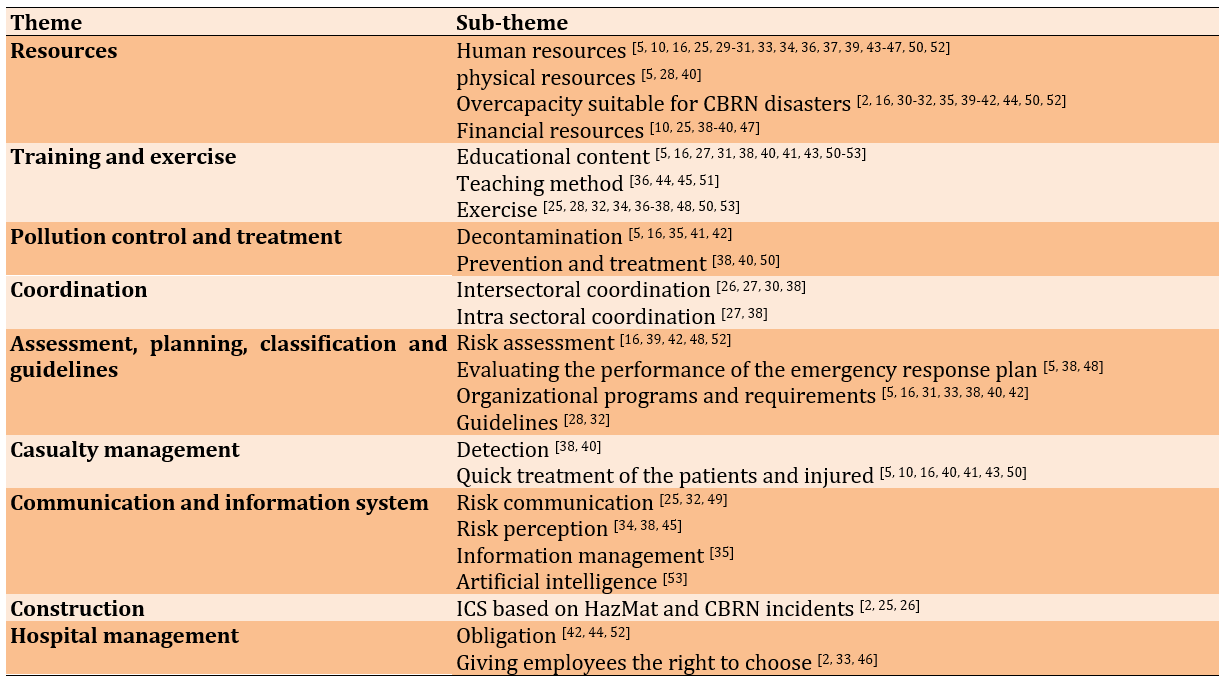
To extract and synthesize data, based on the review, the articles were carefully read several times and the most important points were extracted and summarized and utilizing content analysis, the meaningful units related to the research questions were categorized into 24 subcategories. Categories were defined emergently. These subcategories were then grouped based on similarities and differences into 9 main categories: Resources, training and exercise, contamination control and treatment, coordination, assessment and planning and classification and guidelines, casualty management, communications and information systems, structure, and hospital management (Table 4).
Table 4. Theme and sub-themes
Discussion
Training and exercise are crucial factors in enhancing the preparedness of ED staff for HazMat and CBRN incidents. Recent studies emphasize the importance of well-trained ED staff responding appropriately to HazMat and CBRN events. Without effective training and exercise, ED staff lack the capacity for an adequate response [1, 54]. Physicians, nurses, and ED support staff are the three main groups that require training. Updated training guides are essential for enabling ED staff to respond appropriately to disasters [55]. Educational deficiencies in responding to nuclear/radiological disasters among emergency medical staff in the USA and the UK, as well as during the Ebola epidemic in East Africa, were evident [1, 56]. On the other hand, 66% of emergency physicians in Hong Kong reported having participated in CBRNE incident training, most of which was received within the past five years [33]. O'Sullivan et al. study on Canadian nurses shows that additional training and information are needed to enhance the preparedness of frontline healthcare workers, who are critical in responding to CBRN incidents. This study is consistent with Williams et al. study of British emergency room nurses [34, 35]. The reviewed articles and documents showed that more than 60% of articles addressed this topic, highlighting its importance and frequency as a factor affecting the preparedness of ED staff for HazMat and CBRN incidents [5, 16, 25, 27, 28, 31, 32, 34, 36-38, 40, 41, 43-45, 48, 50-53].
Coordination is one of the main challenges in disasters, especially in CBRN incidents. Hospital EDs must coordinate the mobilization of hospital resources during CBRN incidents [30]. HazMat and CBRN incidents are complex and successful management of this complexity results from the coordination of various functions both within and outside the hospital [38]. Sharififar et al. identified coordination as one of the key factors influencing hospital response to biological disasters, and Teymouri et al. emphasized coordination and communication as key challenges in HazMat and CBRN incidents [30, 38]. Regarding coordination, the Iranian healthcare system and hospitals scored an average rating in response to the COVID-19 pandemic [57]. Coordination with external organizations (responders and supporters) and establishing memorandums of understanding and cooperation plans with other hospitals and local and national centers can improve the management of HazMat and CBRN incidents. These incidents require the coordination of many aspects, such as PPE and decontamination.
Full-scale coordination may sometimes be challenging and disruptive for the hospital ED. To address this, emergency preparedness planning for major incidents should focus on key areas [58].
Evaluation, planning, classification of actions and the presence of specific guidelines are other key elements that influence the preparedness of ED staff in responding to HazMat and CBRN incidents. According to study results, only 31% of nuclear EDs in Japan had predicted and assessed nuclear/radiological incidents [39]. Without risk assessment, prioritizing risk reduction measures can lead to resource loss and parallel efforts [38].
In Razak et al.'s studies and NATO guidelines, was mentioned that without planning, the emergency response of departments to HazMat and CBRN incidents will be limited. Planning for HazMat and CBRN response preparedness, as well as training programs, should be considered at three organizational, technological and individual levels, as well as in short, medium and long-term durations [2, 52].
Physicians and nurses in the EDs of hospitals in three US states identified the lack of specific guidelines for nuclear/radiological threats as a significant factor in reducing preparedness to respond to such incidents [7]. Also, classification and division of actions against CBRN incidents into different phases will enhance staff preparedness for an effective response [28]. This study showed that more than 50% of the studies emphasized the need for assessment, planning, classification, and guidelines in preparing ED staff.
Based on the data analysis results, human resources, physical resources, financial resources, and appropriate capacity for CBRN disasters were subsets under the category of resources [2, 5, 10, 16, 25, 29-37, 40, 42-44, 50, 52]. The presence of essential competencies in ED staff, such as the ability to creatively solve and flexibly address incident problems, documentation skills, and forensic medical analysis results, as well as marital status, age, education, skills, and gender of ED staff, are effective in their preparedness for HazMat and CBRN incidents [5, 31, 33, 34, 39, 42, 43, 47, 50, 52].
Mortelmans et al.'s studies showed that financial resource shortages were a major barrier to achieving hospital staff preparedness in responding to CBRN incidents; Therefore, it is essential to allocate appropriate physical and human resources to handle such incidents [59]. Budgetary strategies for preparedness should be prioritized and logically reviewed [60].
The results of the evaluation study of the preparedness of 93 hospital EDs in the Netherlands to cope with CBRN incidents showed that only 40% of them had decontamination facilities and 32% had appropriate PPE [40]. Therefore, facilities for staff to work in HazMat and CBRN incident conditions, such as access to vaccination, PPE, childcare, etc., should be considered.
The presence of a Hospital Incident Command System (HICS) based on HazMat and CBRN incidents was one of the derived factors in this study. HICS leads to a systematic approach to preparedness and response to incidents in hospitals. It also enables unified and integrated command in dealing with HazMat and CBRN incidents and provides a structure that improves coordination, control and supervision of staff, operations, planning, support and other essential functions for incident management. The hospital incident command system clearly defines responsibilities to ensure an appropriate response to incidents [2, 26, 61]. Anbari et al. point out in their study that the use of HICS is part of an appropriate response to CBRN incidents in confirmation of this, the NATO guidelines also mention the importance of a joint incident command system and incident organizational structure in increasing the readiness of first responders in CBRN incidents [52, 62]. In a study by Sharififar et al., participants identified HICS as an effective factor in responding to biological incidents [38].
Different levels of concern and risk perception will affect the willingness of ED staff to cooperate during HazMat and CBRN incidents [45]. Due to fear and unfamiliarity with nuclear/radiological incidents and emerging infectious disease epidemics, risk perception for emergency responders in Australia varied with the nature of the incident [63]. The study of Sharififar et al. shows that risk perception is highly effective in enhancing hospital staff's preparedness for infectious disasters [26], As Farhat et al.'s study in Saudi Arabia showed, all responding physicians and nurses were highly concerned about responding to a Crimean Congo Hemorrhagic Fever (CCHF), hence adhering to strict infection control measures [53]. Nurses' attitudes toward risk perception are influenced by individual and organizational factors such as gender, past experiences and exposure to colleague violence [64]. Employment region also affects ED staff's risk perception [34]. Transparent communication to increase risk perception and communication are effective factors in ED staff preparedness during HazMat and CBRN incidents [10, 38]. During such incidents, communications and information are the most important risk management tools in the healthcare system. Effective communication reduces response time during emergencies [26] and having a process for verifying news from the emergency operations center and announcing new disease or incident cases will be effective in increasing ED staff preparedness [25].
Recently, a study supported the impact of artificial intelligence in increasing the level of preparedness of staff against nuclear accidents. Virtual learning environments based on artificial intelligence, including virtual and augmented reality, are excellent learning environments because they help simulate an unexpected modeled situation with minimal cost and no risk [53].
According to study results, hospital management's commitment to prioritizing the safety and health of employees and creating a dynamic and capable environment in the hospital setting is particularly important in ED staff preparedness [44]. Maintaining a healthy and high-quality workforce in hospitals through continuous training in safety principles, continuous monitoring of employees' physical and mental health, financial incentives, providing suitable spaces for rest and meals for employees, and providing appropriate PPE against HazMat and CBRN incidents are good management practices aimed at increasing ED staff preparedness [65]. The results of this study showed that approximately 20% of the articles emphasized the importance of this category in ED staff preparedness.
Several studies have emphasized the importance of effective decontamination in emergencies [5, 16, 35, 41, 42]. HazMat and CBRN incidents often result in multiple casualties, so the possibility of contamination of ED staff is always a concern [5]. When providing services to patients exposed to HazMat and CBRN agents, the first priority is to protect the staff. Secondary contamination can have immediate or long-term health effects on first responders, potentially incapacitating them from direct patient care immediately after the incident or even leading to delayed effects [66]. Li et al. and Mortelmans et al. said decontamination in mass casualty incidents is less prioritized, but decontamination in HazMat and CBRN incidents differs from normal conditions. In biological incidents, implementing individual and mass quarantine is of paramount importance to prevent hospital staff contamination and protect their health [40, 67]. When victims of nuclear/radiological incidents are transferred to hospitals, decontamination infrastructure must be established in the ED to prevent secondary contamination of ED staff. Decontamination of victims should commence promptly [16, 68]. A study in EDs of 138 Belgian hospitals showed that only 11% of hospitals have decontamination facilities for CBRN casualties at the ED entrance [59]. Standard operational procedures for decontaminating casualties, disposing of contaminated clothing and preventing entry of contaminated wastewater from washing casualties into municipal sewage should be in place, but unfortunately, such standard operational procedures are sometimes lacking [5].
The Japan Tsunami and Hurricane Katrina demonstrated the necessity of infection control measures to prevent the spread of secondary diseases after disasters [50]. Strategic and preventive infection control measures and programs such as hand hygiene, appropriate PPE use and environmental disinfection can improve ED staff preparedness in response to biological disasters [10, 50]. Access to various drugs and vaccines will enhance the safety, health and preparedness of ED staff [38, 40]. However, hospitals usually do not stock essential drugs and antibiotics due to high costs and risk assessment results indicating the low probability of HazMat and CBRN incidents [59].
The casualty management category, determined by content analysis of articles, includes the subcategory of rapid diagnosis and intervention for patients/victims [5, 10, 38, 40, 41, 43, 50]. The ability to quickly diagnose CBRN agents and promptly intervene with patients/victims in these incidents is crucial for preventing further disease development and maintaining the health of both responders and patients [69]. A study showed that emergency nurses' willingness to promptly intervene with patients/victims of HazMat and CBRN incidents largely depends on their clinical competency [10].
Our study's limitations include the lack of uniform methodology among similar studies. The majority of the data used in this study was retrospective event-based data which can be considered to jeopardise the scientific quality and validity of findings. Additionally, excluding articles published before 2005 the failure to review articles in languages (other than Persian and English) and the inability to access the full text of some articles may have resulted in an incomplete and restricted review. Potential biases may also have been introduced during thematic coding. This study was designed and conducted solely to investigate the factors influencing the preparedness of ED Staff in response to HazMat and CBRN incidents. The researchers recommend that, in the future, a tool be developed to assess the preparedness of hospital emergency personnel for such incidents. A systematic review of studies published after 2024 should also be conducted, incorporating articles published in languages (other than English/Persian). ED staff play a vital role in responding to HazMat and CBRN incidents. Therefore, policies, programs, coordination efforts, budgets, and other necessary measures are strongly recommended to increase ED staff preparedness against HazMat and CBRN incidents. Financial resources and budget allocation significantly increase ED preparedness in response to HazMat and CBRN incidents. These incidents pose challenges for developing countries and necessitate international assistance, as seen in the COVID-19 pandemic with vaccine and PPE aid. By fostering a positive attitude and increasing ED staff confidence through planning and training, ED staff's preparedness to respond to such incidents improves. In addition to known challenges, ED staff preparedness faces obstacles, uncertainties, and inconsistencies that require attention.
Conclusion
The preparedness of emergency department staff to respond to HazMat and Chemical, Biological, Radiological, and Nuclear incidents is limited. Each of the nine identified categories and their subcategories requires careful implementation and upgrading in alignment.
Acknowledgments: We would like to thank all researchers whose articles were reviewed in this study.
Ethical Permissions: This article is approved with ethical permission code of IR.AJAUMS.REC.1402.139
Conflicts of Interests: The authors declare that there are no conflicts of interest regarding the publication of this manuscript.
Authors' Contribution: Ghaffari F (First Author), Introduction Writer/Main Researcher/Discussion Writer (35%); Pishgooie SAH (Second Author), Methodologist/Main Researcher (30%); Zareiyan A (Third Author), Assistant Researcher (10%); Sharififar S (Fourth Author), Assistant Researcher/Statistical Analyst (15%); Azarmi S (Fifth Author), Assistant Researcher (10%)
Funding/Support: No financial support was received for this study.
In recent years, the world has witnessed numerous disasters and calamities. With advancements in technology, the risk of non-natural disasters such as Chemical, Biological, Radiological, and Nuclear (CBRN) incidents has increased, leaving fatal consequences both in terms of human lives and financial costs over several decades. Hazardous Materials (HazMat) and CBRN incidents occur either accidentally or intentionally. These incidents are often unpredictable and invisible, causing fear and anxiety, disrupting social well-being and mental health, and impairing the delivery of healthcare services in the community. Diagnosing symptoms related to CBRN agents is challenging due to the rarity of these incidents and the similarity of their symptoms to other diseases [1-3]. There are national and international concerns regarding CBRN incidents, primarily due to the unexpected nature of these events and the resulting consequences caused by a lack of awareness, resources, planning, and preparedness [4]. Whether intentional or accidental, CBRN incidents are significant from economic, political, social, security, and medical perspectives [5]. The primary concern for people during such incidents is health; Hence, hospitals and healthcare system staff, especially Emergency Departments (ED), are heavily involved [4, 6]. Hospitals bear the brunt of admissions and treatment of affected individuals, and ED serves as the "first gateway" for those needing care [7]. ED staff, referred to as first receivers include doctors, nurses, healthcare specialists, and non-clinical staff [2].
A 2020 study among 308 nurses from selected hospitals in Tehran found that the highest willingness and ability were related to participation in natural disasters like floods and earthquakes, while the lowest willingness and ability were reported for participation in CBRN incidents [8]. Additionally, another study indicated a low likelihood of nurses responding to nuclear/radiological disasters [9].
The potential consequences and costs of unpreparedness for HazMat and CBRN incidents can be immense [10]. Quick and appropriate responses to CBRN incidents can significantly reduce the harmful effects on physical health, decrease mortality, and mitigate the psychological impacts, all of which depend on the preparedness of hospital ED staff [11, 12]. Lack of preparedness can lead to ineffective crisis management, increased fear and anxiety among the public and hospital staff, and potentially inadequate care for the injured, setting the stage for a larger socio-psychological crisis [13]. Preparedness is a significant part of the disaster management cycle. The World Health Organization has identified it as a critical component of sustainable development, emphasizing prior planning and implementation of necessary activities. They have noted that many hospitals are still not adequately prepared for such incidents and face various challenges due to the differing pathophysiology of these events [10, 14]. Hospitals can appropriately respond to nuclear incidents with trained staff [14]. Those responding to these incidents face highly stressful situations that impact their physical and mental health. However, prior planning can minimize these effects and facilitate decision-making [15]. ED staff must prevent contamination by using PPE. Training ED staff about radiation hazards enables them to provide safe care to patients [16]. Despite recognizing the need for emergency preparedness training and programs in the healthcare sector, preparedness levels vary across countries, as does the level of understanding and training among ED staff [17]. Even though hospitals have developed response plans and regularly conduct exercises for HazMat and CBRN incidents in Hong Kong, studies have shown that clinical staff, such as nurses, do not feel adequately prepared and need further training [18]. The role of emergency physicians in preparing for and responding to CBRN and HazMat incidents is crucial worldwide [19].
A report from a medical institute indicated that EDs are better prepared for such incidents than before but still have a long way to go [7, 20]. One challenge for ED staff is the ambiguity in diagnosing the type of contaminant when a patient or victim arrives at the triage area. Another challenge is patient decontamination, which is related to the use of PPE. These are examples of the challenges faced by ED staff in responding to HazMat and CBRN incidents. Training is the only means to enhance the ED's response preparedness for HazMat and CBRN incidents, but it faces obstacles such as staff shortages and frequent relocation of trained staff [2]. Various studies in Iran and worldwide have evaluated hospital preparedness for CBRN incidents, yet differing information exists. Each study has highlighted certain factors affecting hospital staff preparedness, and no comprehensive scoping reviews were found that examined all aspects of ED preparedness for CBRN and HAZMAT incidents. Therefore, the researcher conducted a comprehensive and targeted study to determine the factors that affected the preparedness of ED for HazMat and CBRN incidents. This study employed the scoping review method, utilizing the findings of studies conducted worldwide.
Information and Methods
This article is the result of a scoping review study. The study utilized all five stages proposed by Arksey & O'Malley [21]. Levac et al. recommendations were considered during data charting [22].
Stage 1: Identifying and stating the research questions
This study aimed to determine the factors influencing the preparedness of ED staff in HazMat and CBRN incidents. The following research questions were adopted to guide the review:
1. What factors influence the preparedness of ED staff and their components in facing HazMat and CBRN incidents?
2. What methods can enhance the preparedness of ED staff in facing HazMat and CBRN incidents?
Stage 2: Identifying relevant studies
The search components were preparedness, emergency departments, HazMat, and CBRN incidents. The term "staff" was removed from the search process after consulting the research team to maximize the number of articles retrieved. Additionally, after an initial internet search to identify relevant keywords and subject phrases, the Medical Subject Heading (MeSH) website and consultation with relevant specialists were used to determine keywords in Persian and English. The literature search was conducted using Persian and international databases, including Scopus, PubMed, Cochrane Library, Web of Science, ProQuest, and Magiran, from January 1, 2005, to April 1, 2024 (Table 1).
Table 1. Keywords and search strategies
Stage 3: Study selection
In this stage, an overview of the selected articles and sources for the review was provided. After identifying the relevant studies, they were screened for duplicates and assessed for relevance according to the inclusion and exclusion criteria. Inclusion criteria included research results in all countries from January 2005 to April 2024, all research methods, and relevance to the study topic and research question. Exclusion criteria included articles in languages other than English and Persian (due to the researcher's lack of knowledge of languages other than these two), abstracts of seminar and conference articles, articles that assessed the preparedness of emergency and hospital staff other than HazMat and CBRN incidents, and articles that did not meet the required quality according to the statement of Strobe and COREQ. After excluding all articles that did not meet the inclusion criteria, the full texts of all articles that met the criteria were obtained and reviewed. It is important to note that no articles were excluded due to a lack of full-text access to ensure comprehensive coverage of all countries.
Out of the 361 articles and documents gathered during the search, 154 were found to be relevant, and 34 articles were ultimately included in the study. The overall study selection process is illustrated in the PRISMA diagram (Figure 1).
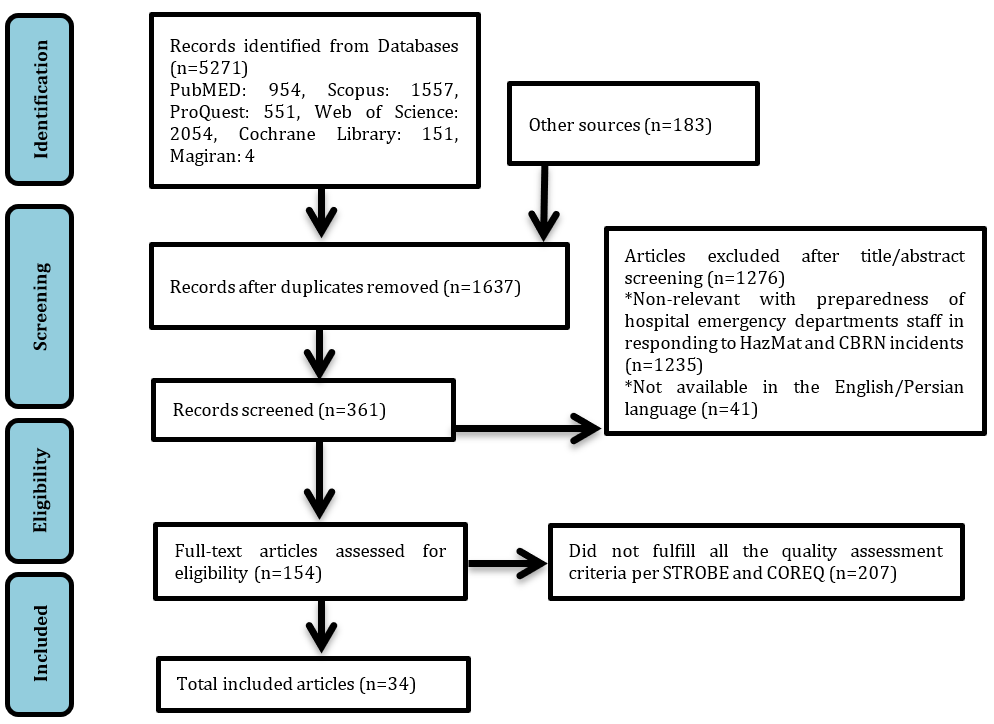
Figure 1. Diagram of the selection process of related articles based on the PRISMA method
Findings
Stage 4: Data charting and synthesis (content analysis)
Quality assessment of studies
The tools for reviewing and assessing the quality of studies and selecting articles eligible for inclusion in the study were evaluated using the STROBE statement and COREQ criteria [23, 24]. Following the quality assessment of articles using these checklists, articles that did not meet the minimum quality standards were excluded from the study. STROBE checklist consisted of 22 items for critiquing observational studies, with the first item on the checklist relating to the title and abstract and the second and third items on the introduction. Items 4-12 related to methodology, items 13-17 related to results, items 18-21 related to discussion, and item 22 related to funding sources. The COREQ checklist consisted of 32 items in three dimensions: Research team and interaction with research units, study design and implementation, data analysis, and results.
At the end of the search, and after omitting duplicates, 2 research team members screened articles and documents according to their titles and abstracts, considering the inclusion and exclusion criteria. In case of any disagreement, a third author was consulted. In this study, an inter-rater reliability score of 75% was considered. Finally, details of the selected articles, including the first author, year of publication, article title, country, study type, number of participants, and relevant results according to the research objective (factors influencing the preparedness of ED staff in facing HazMat and CBRN incidents) were extracted (Table 2). After completing this form, the results obtained from the review of the articles (content analysis) were summarized and reported.
Table 2. Summary of reviewed studies results
Description of studies
Most of the reviewed articles were cross-sectional research studies. Eighteen articles (53%) were conducted in Asian hospitals, eight articles (23%) in European hospitals, four articles (12%) in hospitals in the Americas, one article (3%) in an African hospital and three articles (9%) involved hospitals across more than one continent. Of the total studies, 79% were research or original articles, 15% were review articles and 6% were guidelines and protocols (Table 3).
Table 3. Number of articles encoded by world region and type of documents
Stage 5: Summarizing and reporting the results
To extract and synthesize data, based on the review, the articles were carefully read several times and the most important points were extracted and summarized and utilizing content analysis, the meaningful units related to the research questions were categorized into 24 subcategories. Categories were defined emergently. These subcategories were then grouped based on similarities and differences into 9 main categories: Resources, training and exercise, contamination control and treatment, coordination, assessment and planning and classification and guidelines, casualty management, communications and information systems, structure, and hospital management (Table 4).
Table 4. Theme and sub-themes
Discussion
Training and exercise are crucial factors in enhancing the preparedness of ED staff for HazMat and CBRN incidents. Recent studies emphasize the importance of well-trained ED staff responding appropriately to HazMat and CBRN events. Without effective training and exercise, ED staff lack the capacity for an adequate response [1, 54]. Physicians, nurses, and ED support staff are the three main groups that require training. Updated training guides are essential for enabling ED staff to respond appropriately to disasters [55]. Educational deficiencies in responding to nuclear/radiological disasters among emergency medical staff in the USA and the UK, as well as during the Ebola epidemic in East Africa, were evident [1, 56]. On the other hand, 66% of emergency physicians in Hong Kong reported having participated in CBRNE incident training, most of which was received within the past five years [33]. O'Sullivan et al. study on Canadian nurses shows that additional training and information are needed to enhance the preparedness of frontline healthcare workers, who are critical in responding to CBRN incidents. This study is consistent with Williams et al. study of British emergency room nurses [34, 35]. The reviewed articles and documents showed that more than 60% of articles addressed this topic, highlighting its importance and frequency as a factor affecting the preparedness of ED staff for HazMat and CBRN incidents [5, 16, 25, 27, 28, 31, 32, 34, 36-38, 40, 41, 43-45, 48, 50-53].
Coordination is one of the main challenges in disasters, especially in CBRN incidents. Hospital EDs must coordinate the mobilization of hospital resources during CBRN incidents [30]. HazMat and CBRN incidents are complex and successful management of this complexity results from the coordination of various functions both within and outside the hospital [38]. Sharififar et al. identified coordination as one of the key factors influencing hospital response to biological disasters, and Teymouri et al. emphasized coordination and communication as key challenges in HazMat and CBRN incidents [30, 38]. Regarding coordination, the Iranian healthcare system and hospitals scored an average rating in response to the COVID-19 pandemic [57]. Coordination with external organizations (responders and supporters) and establishing memorandums of understanding and cooperation plans with other hospitals and local and national centers can improve the management of HazMat and CBRN incidents. These incidents require the coordination of many aspects, such as PPE and decontamination.
Full-scale coordination may sometimes be challenging and disruptive for the hospital ED. To address this, emergency preparedness planning for major incidents should focus on key areas [58].
Evaluation, planning, classification of actions and the presence of specific guidelines are other key elements that influence the preparedness of ED staff in responding to HazMat and CBRN incidents. According to study results, only 31% of nuclear EDs in Japan had predicted and assessed nuclear/radiological incidents [39]. Without risk assessment, prioritizing risk reduction measures can lead to resource loss and parallel efforts [38].
In Razak et al.'s studies and NATO guidelines, was mentioned that without planning, the emergency response of departments to HazMat and CBRN incidents will be limited. Planning for HazMat and CBRN response preparedness, as well as training programs, should be considered at three organizational, technological and individual levels, as well as in short, medium and long-term durations [2, 52].
Physicians and nurses in the EDs of hospitals in three US states identified the lack of specific guidelines for nuclear/radiological threats as a significant factor in reducing preparedness to respond to such incidents [7]. Also, classification and division of actions against CBRN incidents into different phases will enhance staff preparedness for an effective response [28]. This study showed that more than 50% of the studies emphasized the need for assessment, planning, classification, and guidelines in preparing ED staff.
Based on the data analysis results, human resources, physical resources, financial resources, and appropriate capacity for CBRN disasters were subsets under the category of resources [2, 5, 10, 16, 25, 29-37, 40, 42-44, 50, 52]. The presence of essential competencies in ED staff, such as the ability to creatively solve and flexibly address incident problems, documentation skills, and forensic medical analysis results, as well as marital status, age, education, skills, and gender of ED staff, are effective in their preparedness for HazMat and CBRN incidents [5, 31, 33, 34, 39, 42, 43, 47, 50, 52].
Mortelmans et al.'s studies showed that financial resource shortages were a major barrier to achieving hospital staff preparedness in responding to CBRN incidents; Therefore, it is essential to allocate appropriate physical and human resources to handle such incidents [59]. Budgetary strategies for preparedness should be prioritized and logically reviewed [60].
The results of the evaluation study of the preparedness of 93 hospital EDs in the Netherlands to cope with CBRN incidents showed that only 40% of them had decontamination facilities and 32% had appropriate PPE [40]. Therefore, facilities for staff to work in HazMat and CBRN incident conditions, such as access to vaccination, PPE, childcare, etc., should be considered.
The presence of a Hospital Incident Command System (HICS) based on HazMat and CBRN incidents was one of the derived factors in this study. HICS leads to a systematic approach to preparedness and response to incidents in hospitals. It also enables unified and integrated command in dealing with HazMat and CBRN incidents and provides a structure that improves coordination, control and supervision of staff, operations, planning, support and other essential functions for incident management. The hospital incident command system clearly defines responsibilities to ensure an appropriate response to incidents [2, 26, 61]. Anbari et al. point out in their study that the use of HICS is part of an appropriate response to CBRN incidents in confirmation of this, the NATO guidelines also mention the importance of a joint incident command system and incident organizational structure in increasing the readiness of first responders in CBRN incidents [52, 62]. In a study by Sharififar et al., participants identified HICS as an effective factor in responding to biological incidents [38].
Different levels of concern and risk perception will affect the willingness of ED staff to cooperate during HazMat and CBRN incidents [45]. Due to fear and unfamiliarity with nuclear/radiological incidents and emerging infectious disease epidemics, risk perception for emergency responders in Australia varied with the nature of the incident [63]. The study of Sharififar et al. shows that risk perception is highly effective in enhancing hospital staff's preparedness for infectious disasters [26], As Farhat et al.'s study in Saudi Arabia showed, all responding physicians and nurses were highly concerned about responding to a Crimean Congo Hemorrhagic Fever (CCHF), hence adhering to strict infection control measures [53]. Nurses' attitudes toward risk perception are influenced by individual and organizational factors such as gender, past experiences and exposure to colleague violence [64]. Employment region also affects ED staff's risk perception [34]. Transparent communication to increase risk perception and communication are effective factors in ED staff preparedness during HazMat and CBRN incidents [10, 38]. During such incidents, communications and information are the most important risk management tools in the healthcare system. Effective communication reduces response time during emergencies [26] and having a process for verifying news from the emergency operations center and announcing new disease or incident cases will be effective in increasing ED staff preparedness [25].
Recently, a study supported the impact of artificial intelligence in increasing the level of preparedness of staff against nuclear accidents. Virtual learning environments based on artificial intelligence, including virtual and augmented reality, are excellent learning environments because they help simulate an unexpected modeled situation with minimal cost and no risk [53].
According to study results, hospital management's commitment to prioritizing the safety and health of employees and creating a dynamic and capable environment in the hospital setting is particularly important in ED staff preparedness [44]. Maintaining a healthy and high-quality workforce in hospitals through continuous training in safety principles, continuous monitoring of employees' physical and mental health, financial incentives, providing suitable spaces for rest and meals for employees, and providing appropriate PPE against HazMat and CBRN incidents are good management practices aimed at increasing ED staff preparedness [65]. The results of this study showed that approximately 20% of the articles emphasized the importance of this category in ED staff preparedness.
Several studies have emphasized the importance of effective decontamination in emergencies [5, 16, 35, 41, 42]. HazMat and CBRN incidents often result in multiple casualties, so the possibility of contamination of ED staff is always a concern [5]. When providing services to patients exposed to HazMat and CBRN agents, the first priority is to protect the staff. Secondary contamination can have immediate or long-term health effects on first responders, potentially incapacitating them from direct patient care immediately after the incident or even leading to delayed effects [66]. Li et al. and Mortelmans et al. said decontamination in mass casualty incidents is less prioritized, but decontamination in HazMat and CBRN incidents differs from normal conditions. In biological incidents, implementing individual and mass quarantine is of paramount importance to prevent hospital staff contamination and protect their health [40, 67]. When victims of nuclear/radiological incidents are transferred to hospitals, decontamination infrastructure must be established in the ED to prevent secondary contamination of ED staff. Decontamination of victims should commence promptly [16, 68]. A study in EDs of 138 Belgian hospitals showed that only 11% of hospitals have decontamination facilities for CBRN casualties at the ED entrance [59]. Standard operational procedures for decontaminating casualties, disposing of contaminated clothing and preventing entry of contaminated wastewater from washing casualties into municipal sewage should be in place, but unfortunately, such standard operational procedures are sometimes lacking [5].
The Japan Tsunami and Hurricane Katrina demonstrated the necessity of infection control measures to prevent the spread of secondary diseases after disasters [50]. Strategic and preventive infection control measures and programs such as hand hygiene, appropriate PPE use and environmental disinfection can improve ED staff preparedness in response to biological disasters [10, 50]. Access to various drugs and vaccines will enhance the safety, health and preparedness of ED staff [38, 40]. However, hospitals usually do not stock essential drugs and antibiotics due to high costs and risk assessment results indicating the low probability of HazMat and CBRN incidents [59].
The casualty management category, determined by content analysis of articles, includes the subcategory of rapid diagnosis and intervention for patients/victims [5, 10, 38, 40, 41, 43, 50]. The ability to quickly diagnose CBRN agents and promptly intervene with patients/victims in these incidents is crucial for preventing further disease development and maintaining the health of both responders and patients [69]. A study showed that emergency nurses' willingness to promptly intervene with patients/victims of HazMat and CBRN incidents largely depends on their clinical competency [10].
Our study's limitations include the lack of uniform methodology among similar studies. The majority of the data used in this study was retrospective event-based data which can be considered to jeopardise the scientific quality and validity of findings. Additionally, excluding articles published before 2005 the failure to review articles in languages (other than Persian and English) and the inability to access the full text of some articles may have resulted in an incomplete and restricted review. Potential biases may also have been introduced during thematic coding. This study was designed and conducted solely to investigate the factors influencing the preparedness of ED Staff in response to HazMat and CBRN incidents. The researchers recommend that, in the future, a tool be developed to assess the preparedness of hospital emergency personnel for such incidents. A systematic review of studies published after 2024 should also be conducted, incorporating articles published in languages (other than English/Persian). ED staff play a vital role in responding to HazMat and CBRN incidents. Therefore, policies, programs, coordination efforts, budgets, and other necessary measures are strongly recommended to increase ED staff preparedness against HazMat and CBRN incidents. Financial resources and budget allocation significantly increase ED preparedness in response to HazMat and CBRN incidents. These incidents pose challenges for developing countries and necessitate international assistance, as seen in the COVID-19 pandemic with vaccine and PPE aid. By fostering a positive attitude and increasing ED staff confidence through planning and training, ED staff's preparedness to respond to such incidents improves. In addition to known challenges, ED staff preparedness faces obstacles, uncertainties, and inconsistencies that require attention.
Conclusion
The preparedness of emergency department staff to respond to HazMat and Chemical, Biological, Radiological, and Nuclear incidents is limited. Each of the nine identified categories and their subcategories requires careful implementation and upgrading in alignment.
Acknowledgments: We would like to thank all researchers whose articles were reviewed in this study.
Ethical Permissions: This article is approved with ethical permission code of IR.AJAUMS.REC.1402.139
Conflicts of Interests: The authors declare that there are no conflicts of interest regarding the publication of this manuscript.
Authors' Contribution: Ghaffari F (First Author), Introduction Writer/Main Researcher/Discussion Writer (35%); Pishgooie SAH (Second Author), Methodologist/Main Researcher (30%); Zareiyan A (Third Author), Assistant Researcher (10%); Sharififar S (Fourth Author), Assistant Researcher/Statistical Analyst (15%); Azarmi S (Fifth Author), Assistant Researcher (10%)
Funding/Support: No financial support was received for this study.
Keywords:
References
1. Farhat H, Alinier G, Gangaram P, El Aifa K, Khenissi MC, Bounouh S, et al. Exploring pre‐hospital healthcare workers' readiness for chemical, biological, radiological, and nuclear threats in the State of Qatar: A cross‐sectional study. Health Sci Rep. 2022;5(5):e803. [Link]
2. Razak S, Hignett S, Barnes J. Emergency department response to chemical, biological, radiological, nuclear, and explosive events: A systematic review. Prehosp Disaster Med. 2018;33(5):543-9. [Link] [DOI:10.1017/S1049023X18000900]
3. Carter H, Drury J, Amlot R. Recommendations for improving public engagement with pre-incident information materials for initial response to a chemical, biological, radiological or nuclear (CBRN) incident: A systematic review. Int J Disaster Risk Reduct. 2020;51:101796. [Link] [DOI:10.1016/j.ijdrr.2020.101796]
4. Yarmohammadian MH, Nasr-Isfahani M, Anbari E. Assessment of preparedness and response of teaching hospitals of Isfahan, Iran, to chemical, biological, radiological, and nuclear incidents. Health Inf Manag. 2016;12(6):777-84. [Persian] [Link]
5. Teymouri F, Zareiyan A, Pishgooie A, Bagheri H. Hospital preparedness challenges in chemical incidents: A qualitative study. Iran J War Public Health. 2022;14(4):377-84. [Link]
6. Khanke HR. Hospital preparedness in accidents and disasters. Tehran: University of Social Welfare and Rehabilitation Science; 2012. [Persian] [Link]
7. Becker SM, Middleton SA. Improving hospital preparedness for radiological terrorism: Perspectives from emergency department physicians and nurses. Disaster Med Public Health Prep. 2008;2(3):174-84. [Link] [DOI:10.1097/DMP.0b013e31817dcd9a]
8. Sharififar S, Shokouh S, Moradi M. Evaluating the willingness and ability of nurses in response to disaster events: A cross-sectional study. Med J Tabriz Univ Med Sci. 2022;44(4):331-42. [Persian] [Link]
9. Veenema TG, Lavin RP, Bender A, Thornton CP, Schneider-Firestone S. National nurse readiness for radiation emergencies and nuclear events: A systematic review of the literature. Nurs Outlook. 2019;67(1):54-88. [Link] [DOI:10.1016/j.outlook.2018.10.005]
10. Aminizadeh M, Farrokhi M, Ebadi A, Masoumi G, Kolivand P, Khankeh H. Hospital preparedness challenges in biological disasters: A qualitative study. Disaster Med Public Health Prep. 2022;16(3):956-60. [Link] [DOI:10.1017/dmp.2020.434]
11. Aminizadeh M, Farrokhi M, Ebadi A, Masoumi GR, Kolivand P, Khankeh HR. Hospital management preparedness tools in biological events: A scoping review. J Educ Health Promot. 2019;8:234. [Link] [DOI:10.4103/jehp.jehp_473_19]
12. Latif M, Abbasi M, Momenian S. The effect of educating confronting accidents and disasters on the improvement of nurses' professional competence in response to the crisis. Health Emerg Disasters. 2019;4(3):147-56. [Link] [DOI:10.32598/hdq.4.3.147]
13. Hoseini A, Musareszaie A, Eslamian J. Awareness of radiological accidents and how to deal with it: A study of nurses and nursing faculties of Isfahan university of medical sciences. Iran J Med Educ. 2014;14(1):78-86. [Persian] [Link]
14. Davari F, Zahed A. A management plan for hospitals and medical centers facing radiation incidents. J Res Med Sci. 2015;20(9):871-8. [Link] [DOI:10.4103/1735-1995.170615]
15. Hick JL, Weinstock DM, Coleman CN, Hanfling D, Cantrill S, Redlener I, et al. Health care system planning for and response to a nuclear detonation. Disaster Med Public Health Prep. 2011;5(Suppl 1):S73-88. [Link]
16. Marzaleh MA, Rezaee R, Rezaianzadeh A, Rakhshan M, Haddadi G, Peyravi M. Developing a model for hospitals' emergency department preparedness in radiation and nuclear incidents and nuclear terrorism in Iran. Bull Emerg Trauma. 2019;7(3):300-6. [Persian] [Link]
17. Wong K, Turner PS, Boppana A, Nugent Z, Coltman T, Cosker TD, et al. Preparation for the next major incident: Are we ready?. Emerg Med J. 2006;23(9):709-12. [Link] [DOI:10.1136/emj.2005.034025]
18. Fung OW, Loke AY, Lai CK. Disaster preparedness among Hong Kong nurses. J Adv Nurs. 2008;62(6):698-703. [Link] [DOI:10.1111/j.1365-2648.2008.04655.x]
19. Rega PP. Doctors and bioterrorism. Lancet. 2005;365(9462):844. [Link] [DOI:10.1016/S0140-6736(05)71036-9]
20. Institute of Medicine. Hospital-based emergency care: At the breaking point. Washington, DC: The National Academies Press; 2007. [Link]
21. Arksey H, O'malley L. Scoping studies: Towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19-32. [Link] [DOI:10.1080/1364557032000119616]
22. Levac D, Colquhoun H, O'brien KK. Scoping studies: Advancing the methodology. Implement Sci. 2010;5:69. [Link] [DOI:10.1186/1748-5908-5-69]
23. Vandenbroucke JP, Von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): Explanation and elaboration. Int J Surg. 2014;12(12):1500-24. [Link] [DOI:10.1016/j.ijsu.2014.07.014]
24. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349-57. [Link] [DOI:10.1093/intqhc/mzm042]
25. Heidaranlu E, Tavan A, Aminizadeh M. Investigating the level of functional preparedness of selected Tehran hospitals in the face of biological events: A focus on COVID-19. Int J Disaster Resil Built Environ. 2022;13(2):150-62. [Link] [DOI:10.1108/IJDRBE-08-2021-0088]
26. Sharififar S, Jahangiri K, Khoshvaghti A. The current state of infectious disasters preparedness around the world: A qualitative systematic review (2007-2019). Disaster Med Public Health Prep. 2022;16(2):753-62. [Link] [DOI:10.1017/dmp.2020.258]
27. Jahangiri K, Sohrabizadeh S, Sadighi J, Tavousi M, Rostami R. Assessing hospital preparedness for nuclear and radiological events: Development a valid and reliable instrument. PAYESH. 2016;15(6):619-27. [Persian] [Link]
28. Bajow N, Alkhalil S, Maghraby N, Alesa S, Najjar AA, Aloraifi S. Assessment of the effectiveness of a course in major chemical incidents for front line health care providers: A pilot study from Saudi Arabia. BMC Med Educ. 2022;22(1):350. [Link] [DOI:10.1186/s12909-022-03427-2]
29. Razak S, Hignett S, Barnes J, Hancox G. The standardization of the emergency department response to chemical, biological, radiological, and nuclear (CBRN) events: Human factors/ergonomics approach. Disaster Med Public Health Prep. 2023;17:e487. [Link]
30. Teymouri F, Zareiyan A, Pishgooie AH, Bagheri H. Hospital preparedness assessment instruments in chemical incidents: A systematic literature review. Asia Pac J Health Manag. 2022;17(3):160-72. [Link] [DOI:10.24083/apjhm.v17i3.1779]
31. Erickson TB, Harvin D, Schmid A, Loevinsohn G, Poriechna A, Martyshyn O, et al. Evaluation of chemical, biological, radiological, nuclear, explosives (CBRNE) knowledge change and skills confidence among frontline-line providers during the Russia-Ukraine war. Disaster Med Public Health Prep. 2023;17:e387. [Link]
32. Asadi M, Mohammadian M, Shahriary A, Mesri M. Multi-purpose model of general emergency of hospitals in CBRN conditions: Narrative review. J Mil Med. 2023;25(1):1660-74. [Persian] [Link]
33. Hung K, Lam E, Wong M, Wong T, Chan E, Graham C. Emergency physicians' preparedness for CBRNE incidents in Hong Kong. Hong Kong J Emerg Med. 2013;20(2):90-7. [Link] [DOI:10.1177/102490791302000204]
34. O'Sullivan TL, Dow D, Turner MC, Lemyre L, Corneil W, Krewski D, et al. Disaster and emergency management: Canadian nurses' perceptions of preparedness on hospital front lines. Prehosp Disaster Med. 2008;23(3):s11-8. [Link]
35. Williams J, Walter D, Challen K. Preparedness of emergency departments in northwest England for managing chemical incidents: A structured interview survey. BMC Emerg Med. 2007;7:20. [Link] [DOI:10.1186/1471-227X-7-20]
36. Azeem AR, Sharif MW, Akhtar A, Sohail CS, Dar AA, Khan M, et al. Perception of preparedness of health care professionals in case of a nuclear, chemical, biological attack/emergency in a tertiary care hospital. Cureus. 2019;11(5):e4657. [Link]
37. Houser R. Evaluating Nebraska EMS providers' ability and willingness to respond to emergencies resulting from bioterrorist attacks. Disaster Med Public Health Prep. 2022;17:e215. [Link]
38. Sharififar S, Jahangiri K, Zareiyan A, Khoshvaghti A. Factors affecting hospital response in biological disasters: A qualitative study. Med J Islam Repub Iran. 2020;34:21. [Link] [DOI:10.47176/mjiri.34.21]
39. Nagata T, Arishima T, Yamaguchi Y, Hirohashi N, Hasegawa A, Hanada H, et al. Radiation emergency medical preparedness in Japan: A survey of nuclear emergency core hospitals. Disaster Med Public Health Prep. 2022;17:e78. [Link]
40. Mortelmans LJ, Gaakeer MI, Dieltiens G, Anseeuw K, Sabbe MB. Are Dutch hospitals prepared for chemical, biological, or radionuclear incidents? A survey study. Prehosp Disaster Med. 2017;32(5):483-91. [Link] [DOI:10.1017/S1049023X17006513]
41. Jama TJ, Kuisma MJ. Preparedness of Finnish emergency medical services for chemical emergencies. Prehosp Disaster Med. 2016;31(4):392-6. [Link] [DOI:10.1017/S1049023X16000546]
42. Chilcott RP, Larner J, Matar H. UK's initial operational response and specialist operational response to CBRN and HazMat incidents: A primer on decontamination protocols for healthcare professionals. Emerg Med J. 2019;36(2):117-23. [Link] [DOI:10.1136/emermed-2018-207562]
43. Sajjadi SL, Gorbannejad S, Feizollahzadeh H, Shabanloei R. Preparedness, knowledge, and attitude of emergency nurses dealing with the crisis of unnatural disasters. Nurs Midwifery J. 2023;21(2):89-97. [Persian] [Link]
44. Amponsah‐Tawiah K, Anuka BE. Pressure for health service delivery and its implications on safety behaviour of health care practitioners. J Nurs Manag. 2018;26(7):802-9. [Link] [DOI:10.1111/jonm.12588]
45. Balicer RD, Catlett CL, Barnett DJ, Thompson CB, Hsu EB, Morton MJ, et al. Characterizing hospital workers' willingness to respond to a radiological event. PLoS One. 2011;6(10):e25327. [Link]
46. Sultan MAS, Løwe Sørensen J, Carlström E, Mortelmans L, Khorram-Manesh A. Emergency healthcare providers' perceptions of preparedness and willingness to work during disasters and public health emergencies. Healthcare. 2020;8(4):442. [Link] [DOI:10.3390/healthcare8040442]
47. Al-Hunaishi W, Hoe VC, Chinna K. Factors associated with healthcare workers willingness to participate in disasters: A cross-sectional study in Sana'a, Yemen. BMJ Open. 2019;9(10). [Link]
48. Siman-Tov M, Davidson B, Adini B. Maintaining preparedness to severe though infrequent threats-can it be done?. Int J Environ Res Public Health. 2020;17(7):2385. [Link] [DOI:10.3390/ijerph17072385]
49. Min YS, Kim SY, Choi SK, Ahn YS. The effect of prior mental health on persistent physical symptoms after exposure to a chemical disaster. Healthcare. 2023;11(7):1004. [Link] [DOI:10.3390/healthcare11071004]
50. Rebmann T, Mohr LB. Missouri nurses' bioterrorism preparedness. Biosecur Bioterror. 2008;6(3):243-51. [Link] [DOI:10.1089/bsp.2008.0022]
51. Farhat H, Laughton J, Gangaram P, El Aifa K, Khenissi MC, Zaghouani O, et al. Hazardous material and chemical, biological, radiological, and nuclear incident readiness among prehospital care professionals in the State of Qatar. Glob Secur Health Sci Policy. 2022;7(1):24-36. [Link] [DOI:10.1080/23779497.2022.2069142]
52. NATO. Minimum standards and non-binding guidelines for first responders regarding planning, training, procedure and equipment for chemical, biological, radiological and nuclear (CBRN) incidents. Brussels: The North Atlantic Treaty Organization; 2014. [Link]
53. Farhat H, Alinier G, Helou M, Galatas I, Josse D, Campbell C, et al. Exploring attitudes towards health preparedness in the Middle East and North Africa against chemical, biological, radiological, and nuclear threats: A qualitative study. J Conting Crisis Manag. 2024;32(1):e12509. [Link]
54. Djalali A, Della Corte F, Segond F, Metzger MH, Gabilly L, Grieger F, et al. TIER competency-based training course for the first receivers of CBRN casualties: A European perspective. Eur J Emerg Med. 2017;24(5):371-6. [Link] [DOI:10.1097/MEJ.0000000000000383]
55. Reilly M, Markenson DS. Education and training of hospital workers: Who are essential personnel during a disaster?. Prehosp Disaster Med. 2009;24(3):239-45. [Link] [DOI:10.1017/S1049023X00006877]
56. Kratochvil CJ, Evans L, Ribner BS, Lowe JJ, Harvey MC, Hunt RC, et al. The national Ebola training and education center: Preparing the United States for Ebola and other special pathogens. Health Secur. 2017;15(3):253-60. [Link] [DOI:10.1089/hs.2017.0005]
57. Yari A, Yousefi Khoshsabegheh H, Zarezadeh Y, Amraei M, Soufi Boubakran M, Motlagh ME. Iranian primary healthcare system's response to the COVID-19 pandemic using the healthcare incident command system. PLoS One. 2023;18(8):e0290273. [Link]
58. Jasper E, Miller M, Sweeney B, Berg D, Feuer E, Reganato D. Preparedness of hospitals to respond to a radiological terrorism event as assessed by a full-scale exercise. J Public Health Manag Pract. 2005;11:S11-6. [Link]
59. Mortelmans LJ, Van Boxstael S, De Cauwer HG, Sabbe MB. Preparedness of Belgian civil hospitals for chemical, biological, radiation, and nuclear incidents: Are we there yet?. Eur J Emerg Med. 2014;21(4):296-300. [Link] [DOI:10.1097/MEJ.0000000000000072]
60. Keeble TA. Bioterrorism preparedness at a hospital level in the Southwest region of the United States-A systematic review [dissertation]. Texas: The University of Texas School of Public Health; 2010. [Link]
61. Schoonover H, Haydon K. Incident command structure using a daily management system and the centers for disease control and prevention's patient notification toolkit drives effective response to an infection control breach. J Healthc Risk Manag. 2018;38(2):19-26. [Link] [DOI:10.1002/jhrm.21323]
62. Anbari E, Yarmohammadian MH, Isfahani MN. From investigation of hospital protocols and guidelines to designing a generic protocol for responding to chemical, biological, radiological, and nuclear incidents. Int J Health Syst Disaster Manag. 2015;3(4):195. [Link] [DOI:10.4103/2347-9019.162553]
63. Smith EC, Burkle FM, Archer FL. Fear, familiarity, and the perception of risk: a quantitative analysis of disaster-specific concerns of paramedics. Disaster Med Public Health Prep. 2011;5(1):46-53. [Link] [DOI:10.1001/dmp.10-v4n2-hre10008]
64. Gülen S, Baykal Ü, Göktepe N. Factors affecting nurses' attitudes towards risks in the work environment: A cross‐sectional study. J Nurs Manag. 2022;30(7):3264-72. [Link] [DOI:10.1111/jonm.13759]
65. Beyramijam M, Rasouli-Ghahfarokhi SM, Fathollahzadeh A, Rahimzadeh A, Shahabirabori MA, Aminizadeh M. The effect of education and implementation of "National Hospital Disaster Preparedness Plan" on an Iranian hospital preparedness: An interventional study. J Educ Health Promot. 2019;8:215. [Link] [DOI:10.4103/jehp.jehp_208_19]
66. Koenig KL, Boatright CJ, Hancock JA, Denny FJ, Teeter DS, Kahn CA, et al. Health care facilities' "war on terrorism": A deliberate process for recommending personal protective equipment. Am J Emerg Med. 2007;25(2):185-95. [Link] [DOI:10.1016/j.ajem.2006.06.012]
67. Li Y, Hsu EB, Links JM. Healthcare system cost evaluation of antiviral stockpiling for pandemic influenza preparedness. Biosecur Bioterror. 2010;8(2):119-28. [Link] [DOI:10.1089/bsp.2009.0050]
68. Belsky JB, Klausner HA, Karson J, Dunne RB. Survey of emergency department chemical hazard preparedness in Michigan, USA: A seven year comparison. Prehosp Disaster Med. 2016;31(2):224-7. [Link] [DOI:10.1017/S1049023X16000108]
69. Grundmann O. The current state of bioterrorist attack surveillance and preparedness in the US. Risk Manag Healthc Policy. 2014;7:177-87. [Link] [DOI:10.2147/RMHP.S56047]










