Volume 15, Issue 4 (2023)
Iran J War Public Health 2023, 15(4): 323-327 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2023/05/26 | Accepted: 2023/10/9 | Published: 2023/12/19
Received: 2023/05/26 | Accepted: 2023/10/9 | Published: 2023/12/19
How to cite this article
Sherhan A, Saihood H. Role of Antibiotics in Reducing the Days of Hospitalization in Acute Severe Bronchial Asthma Patients. Iran J War Public Health 2023; 15 (4) :323-327
URL: http://ijwph.ir/article-1-1348-en.html
URL: http://ijwph.ir/article-1-1348-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Authors
A.A. Sherhan *1, H.A. Saihood2
1- Department of Medicine, Basrah College of Medicine, Basrah University, Basrah, Iraq
2- Basrah Health Directorate, Basrah, Iraq
2- Basrah Health Directorate, Basrah, Iraq
Full-Text (HTML) (697 Views)
Introduction
Bronchial asthma is a chronic pulmonary disease that has a major impact on people's lives. About three hundred million people worldwide have been affected by asthma, and this is expected to reach four hundred million in 2025 [1]. Bronchial asthma is a chronic inflammatory disorder of the airways associated with airway hyper-responsiveness that leads to recurrent episodes of wheezing, breathlessness, chest tightness, and coughing, particularly at night or in the early morning [2].
Regarding asthma, an exacerbation is defined as an occurrence marked by a change from the patient's previous state. This involves a gradual increase in relevant symptoms and a decline in respiratory function [2]. This decline in respiratory function can be measured through indicators like peak expiratory flow (PEF) and forced expiratory volume in 1 second (FEV1). Compared to the patient's previous or expected values, these measurements reflect the worsening of expiratory airflow, which is the primary physiological effect of an asthma attack. The most common triggers for these exacerbations are exposure to external factors, such as indoor and outdoor allergens [3, 4, 5], air pollutants [6], and respiratory tract infections, with viral infections like human rhinovirus (HRV) being the primary culprits [7, 8]. How these environmental triggers and viruses initiate asthma or exacerbate the condition is still the subject of ongoing research.
Acute severe asthma represents a sudden exacerbation of asthma unresponsive to the standard treatments involving bronchodilators and corticosteroids. These episodes are typically categorized as moderate, severe, or life-threatening based on specific criteria, such as the peak expiratory flow rate (PEFR) falling below 50% of the predicted value and clinical signs, including a pulse rate exceeding 110 beats per minute, a respiratory rate exceeding 25 breaths per minute, and impaired speech, where the patient cannot complete a sentence in one breath. Moreover, these patients have a documented history of bronchial asthma [9].
Such episodes are often characterized by significant, reversible airflow obstruction, necessitating immediate medical attention. Standard emergency treatments include oxygen therapy, beta-agonist bronchodilators, and high hydrocortisone and prednisolone administered upon hospital admission. Continuous monitoring of vital signs, blood gases, and pulse oximetry is essential for patient care. It's important to note that antibiotics are generally not recommended for treating acute asthma attacks, except when there's clear evidence of infection, often linked to viral upper respiratory tract infections [10, 11].
However, emerging evidence suggests that certain antibiotics may contribute to a quicker recovery in severe asthmatic attacks. This suggests that antibiotics may possess beneficial anti-inflammatory effects on the airways and offer anti-infective properties [12].
Clinical trials assessing the effectiveness of antimicrobial treatment against C. pneumoniae and M. pneumoniae in patients with asthma would offer additional evidence regarding the potential role of atypical bacterial infections in this condition [13].
Suitable antibiotic options with activity against atypical bacteria include macrolides (including azithromycin), ketolides like telithromycin, tetracyclines, and fluoroquinolones. In previous clinical trials involving asthma, macrolides and ketolides have been predominantly used due to their well-tolerated and safe profiles and ability to accumulate effectively within cells. Most of these studies have been conducted in individuals with chronic stable asthma, with only one recent study exploring their efficacy in acute asthma exacerbations [13].
The utilization of antibiotics in the management of asthma exacerbations is a common practice. Still, there is limited documentation regarding the specific situations in which treatment is warranted and the advantages it offers. According to the 2018 Global Initiative for Asthma (GINA) guidelines, the routine prescription of antibiotics for asthma exacerbations is discouraged. This recommendation is primarily rooted in the absence of universally accepted criteria for administering antibiotics during acute asthma exacerbations. While infections frequently trigger asthma exacerbations, most infection-related exacerbations are linked to viral pathogens [14].
Much current interest focuses on the role of childhood infections in determining the immune system in early life. It has been suggested that growing up in a relatively non-infective environment may predispose towards an IgE response to allergens (the hygiene hypothesis). Conversely, growing up in an infected environment may prevent the immune system from developing allergic responses. Components of bacteria (e.g., lipo-polysaccharide endotoxin; immune-stimulatory CpG DNA sequences; flagellin), viruses (e.g., SS- and DS-RNA), and fungi (e.g., chiton, a cell wall component) can stimulate up to 10 different toll-like receptors (TLRs) expressed on immune and epithelial cells to direct the immune and inflammatory response away from the allergic (Th2) towards protective (Th1 and T reg) pathways. Th1 immunity is associated with antimicrobial protective immunity, whereas regulatory T cells are strongly implicated in tolerance to allergens [15]. On the other hand, the use of antibiotics in early life has been linked to the development of asthma [16, 17]. Also, delivery via cesarean section is associated with an increased risk of asthma by 20-80%; this increased risk is attributed to the lack of healthy bacterial colonization that the newborn would have acquired from passage through the birth canal [18]. There is a link between asthma and degree of affluence, as less affluent individuals are more liable to bacterial infection [19].
There is increasing evidence that atypical respiratory pathogens such as Chlamydia pneumonia and mycoplasma pneumonia may contribute to the pathogenesis of both stable asthma and asthma exacerbation [20]. It is postulated that these organisms may contribute to inflammation in the airways, possibly by activating inflammatory mechanisms in the respiratory tract [21]. Macrolide antibiotics may play a part in managing asthma by exerting anti-inflammatory effects on the chronically inflamed airways in addition to their anti-infective action [21]. The ketolide antibiotics may also have similar properties. Recent studies on asthmatic patients with evidence of atypical infection suggest that specific antimicrobial treatment macrolides and fluoroquinolones may confer additional advantages compared to standard therapy alone [22]. A considerable amount of data has been describing additional effects associated with macrolide treatment of reduced bronchial hyperresponsiveness and altered cytokine production by decreasing the transcription of m RNA for various cytokines inhibiting interleukin-8 release by eosinophils. These non-antimicrobial effects have been defined as anti-inflammatory activity [23].
This study aimed to show whether using antibiotics to treat acute asthmatic attacks is useful in reducing admission days and rapid recovery of acute asthma attacks.
Instrument & Methods
This cross-sectional study was conducted on acute asthmatic patients admitted from January 2021 to January 2022 in Al-Mawani General Hospital in Basrah, Southern Iraq. Out of the patients, 70 subjects were selected by random sampling according to the Cochrane formula.
Patient’s records were retrieved from AL-Mawani General Hospital after receiving a written consent form from the hospital administration. The research tool was a checklist to register the subjects’ information (duration of asthma, medical treatment, co-morbidities, hospitalization duration, antibiotic therapy, and single/combination medicine). Also, total WBC and neutrophil counts were obtained through the laboratory records of the subjects. The subjects were classified into two groups based on the duration of hospitalization, including 3≥ days and >3 days. The age range of patients was subdivided into four groups; 15-29, 30-44, 45-59, and ≥60 years. The disease durations are subdivided into four groups; 1-5, 6-10, 11-15, and 16 -20 years.
Data were analyzed using the Chi-square test through SPSS 18 software.
Findings
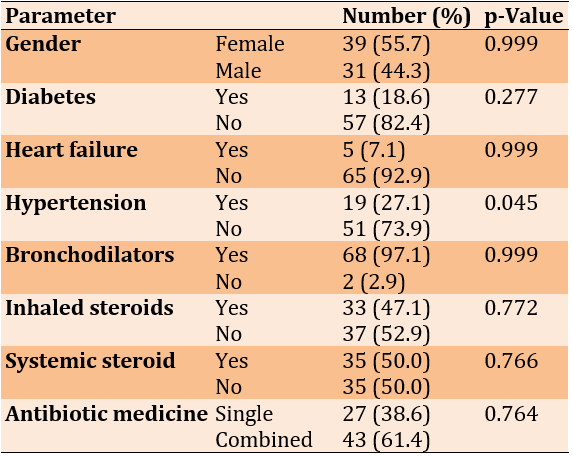
The mean duration of disease and the mean age of the subjects were 8.57±5.01 and 44.46±13.20 years, respectively. There was just a significant difference in the frequency of hypertension in comparing the goodness of fit between the subjects (p=0.045; Table 1).
Table 1. General characteristics of the subjects
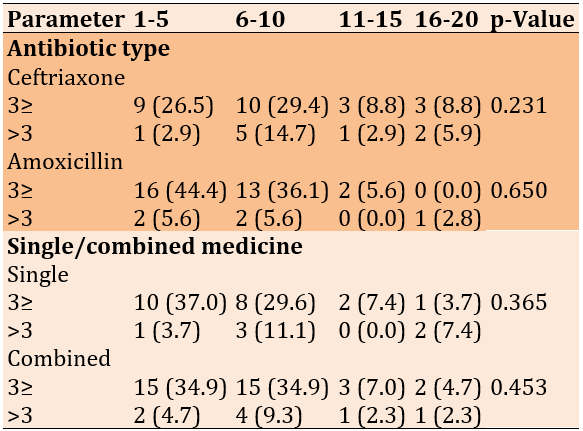
There were no significant associations between the duration of hospitalization with age group (p=0.198) and duration of asthma (p=0.069). No significant association was observed between types of antibiotics and duration of hospitalization (p<0.05). There was an inverse relationship between the duration of hospitalization and single and combined medicine therapy by antibiotic (Table 2).
Table 2. Relationship of age range (year) of the study samples frequency (numbers in parentheses are percentages) with types of antibiotics and single/combined medicine

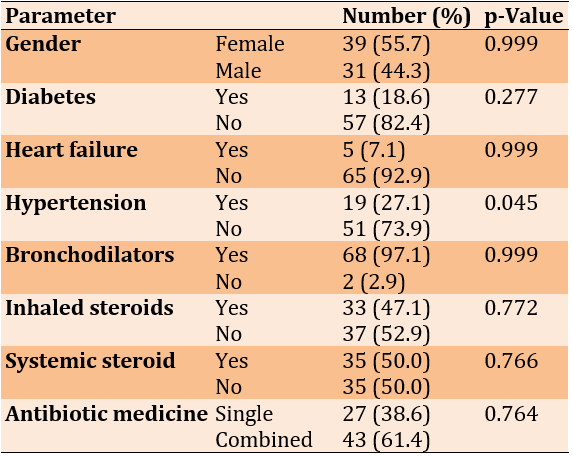
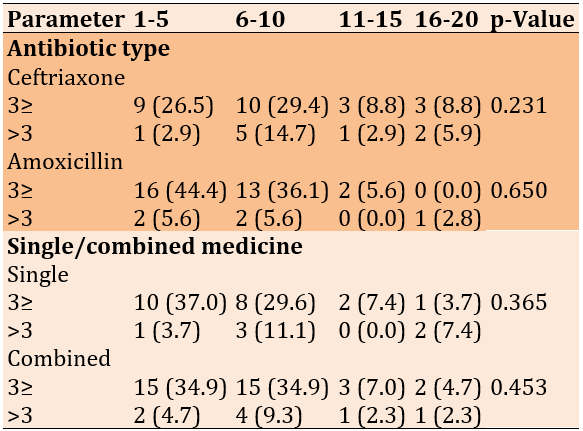
There was no significant association between the duration of asthma and single/combined medicine (Table 3).
Table 3. Relationship of duration of asthma (year) of the study samples frequency (numbers in parentheses are percentages) with types of antibiotics and single/combined medicine
The level of WBC had no significant difference between the 3≥ (8.72±1.96) and >3 (8.87±2.75) groups (p=0.817). Also, the level of neutrophils had no significant difference between the 3≥ (43.72±8.42) and >3 (29.92±6.05) groups (p=0.236).
Discussion
This study aimed to investigate the role of antibiotics in managing acute asthmatic attacks in patients admitted to Al-Mawani General Hospital in Basrah, Iraq. The use of antibiotics in the management of asthma exacerbations is a common practice, although the indications for treatment and the benefits of therapy are not well documented. The findings of this study showed an inverse relationship between hospitalization duration and the use of antibiotics through single or combined medicine. Global Initiative for Asthma (GINA) [14] states that antibiotics should not be routinely prescribed for asthma exacerbations. This recommendation is based on the absence of consensus criteria for using antibiotics during acute worsening of asthma symptoms. Although infection is a common trigger of asthma, most exacerbations from infections are associated with viral pathogens. GINA [15] states that evidence does not support the role of antibiotics in asthma exacerbations unless there is strong evidence of lung infection (e.g., fever and purulent sputum or radiographic evidence of pneumonia). Although Stolbrink et al. [15] do not address the appropriateness nor the necessity of antibiotic prescriptions, their findings support those patients treated with short antibiotic courses usually recovered without needing an additional antibiotic prescription. David & Stemple [14] discussed the appropriate use of antibiotics for acute asthma and found that most patients were treated with either amoxicillin or doxycycline, with a small percentage receiving macrolides. Inconsistent with the findings, Denholm et al. [24], found that antibiotics do not benefit patients hospitalized with an asthma exacerbation and may even lead to worse outcomes, including a longer hospital stay, higher costs, and greater risk of diarrhea.
Amoxicillin and ceftriaxone were the most commonly used antibiotics in this study; the most significantly useful was amoxicillin, which significantly reduced hospitalization duration compared to ceftriaxone. In accordance with these findings, Stolbrink et al. [15] found that the vast majority of patients were treated with either amoxicillin or doxycycline and a small percentage with macrolides. Treatment with amoxicillin was as effective as or more effective than the other agents, as judged by the need for a second course of antibiotics. Denholm et al. [24] found that amoxicillin is one of the most commonly prescribed antibiotics for acute lower respiratory tract infections (ALRTIs) in people with asthma. Co-amoxiclav, a combination of amoxicillin and clavulanic acid, may also treat respiratory infections in people with asthma [24].
Adding a second antibiotic to the treatment regimen further reduced the hospitalization duration and was highly significant when used as a second antibiotic. The findings are consistent with the findings of Sebastian et al. [22], which showed the benefit of using the new ketolides in managing asthma exacerbation.
The matched groups in this study, especially regarding the marker of evidence of infection by the matched WBC counts between two groups showed the exclusion of the role of infection as the cause of difference in the hospital stay. This difference appears in the presence or absence of systemic disease apart from hypertension.
The matched groups in this study, especially regarding the marker of evidence of infection by the matched WBC counts between two groups showed the exclusion of the role of infection as a cause of difference in the hospital stay. This difference appears in the presence or absence of systemic disease apart from hypertension. The duration of asthma in this study showed no significant associations with the period of hospitalization duration.
There was no significant difference between the WBC and paradoxical change in the count of neutrophils in the study's main two groups, which may explain the non-infective role of the antibiotics. However, sputum neutrophil count is superior to serum neutrophil, on which this study depends. The matched characteristics of the variable and matched occurrence of systemic disease like diabetes mellitus apart from systemic hypertension may not be appointed against the study result. Based on the need for direct microbiological diagnosis, isolation of microorganisms, and or serological confirmation of infection, and more recently, investigators have turned to biopsy and polymerase chain reaction (PCR) techniques to more accurately identify the presence of these pathogens.
One of the limitations of the study was the limited sample size. So, the authors suggest studying more sample sizes in different times and areas to evaluate the use of antibiotics to treat acute asthma. Based on the findings, it suggests the use of antibiotics in patients with acute severe asthma.
Conclusion
Amoxicillin and ceftriaxone as an additional treatment to standard therapy of acute severe asthma effectively reduces hospitalization of asthmatic patients.
Acknowledgements: We appreciate to patients participated, hospital medical and administer staff.
Ethical Permission: Research approved by scientific team of medical department.
Conflict of Interests: No Conflict of Interests.
Authors’ Contribution: Sherhan AA (First Author), Introduction Writer/Methodologist/Main Researcher (50%); Saihood HA (Second Author), Assistant Researcher/Statistical Analyst/Discussion Writer (50%)
Funding/Support: Nothing has been reported.
Bronchial asthma is a chronic pulmonary disease that has a major impact on people's lives. About three hundred million people worldwide have been affected by asthma, and this is expected to reach four hundred million in 2025 [1]. Bronchial asthma is a chronic inflammatory disorder of the airways associated with airway hyper-responsiveness that leads to recurrent episodes of wheezing, breathlessness, chest tightness, and coughing, particularly at night or in the early morning [2].
Regarding asthma, an exacerbation is defined as an occurrence marked by a change from the patient's previous state. This involves a gradual increase in relevant symptoms and a decline in respiratory function [2]. This decline in respiratory function can be measured through indicators like peak expiratory flow (PEF) and forced expiratory volume in 1 second (FEV1). Compared to the patient's previous or expected values, these measurements reflect the worsening of expiratory airflow, which is the primary physiological effect of an asthma attack. The most common triggers for these exacerbations are exposure to external factors, such as indoor and outdoor allergens [3, 4, 5], air pollutants [6], and respiratory tract infections, with viral infections like human rhinovirus (HRV) being the primary culprits [7, 8]. How these environmental triggers and viruses initiate asthma or exacerbate the condition is still the subject of ongoing research.
Acute severe asthma represents a sudden exacerbation of asthma unresponsive to the standard treatments involving bronchodilators and corticosteroids. These episodes are typically categorized as moderate, severe, or life-threatening based on specific criteria, such as the peak expiratory flow rate (PEFR) falling below 50% of the predicted value and clinical signs, including a pulse rate exceeding 110 beats per minute, a respiratory rate exceeding 25 breaths per minute, and impaired speech, where the patient cannot complete a sentence in one breath. Moreover, these patients have a documented history of bronchial asthma [9].
Such episodes are often characterized by significant, reversible airflow obstruction, necessitating immediate medical attention. Standard emergency treatments include oxygen therapy, beta-agonist bronchodilators, and high hydrocortisone and prednisolone administered upon hospital admission. Continuous monitoring of vital signs, blood gases, and pulse oximetry is essential for patient care. It's important to note that antibiotics are generally not recommended for treating acute asthma attacks, except when there's clear evidence of infection, often linked to viral upper respiratory tract infections [10, 11].
However, emerging evidence suggests that certain antibiotics may contribute to a quicker recovery in severe asthmatic attacks. This suggests that antibiotics may possess beneficial anti-inflammatory effects on the airways and offer anti-infective properties [12].
Clinical trials assessing the effectiveness of antimicrobial treatment against C. pneumoniae and M. pneumoniae in patients with asthma would offer additional evidence regarding the potential role of atypical bacterial infections in this condition [13].
Suitable antibiotic options with activity against atypical bacteria include macrolides (including azithromycin), ketolides like telithromycin, tetracyclines, and fluoroquinolones. In previous clinical trials involving asthma, macrolides and ketolides have been predominantly used due to their well-tolerated and safe profiles and ability to accumulate effectively within cells. Most of these studies have been conducted in individuals with chronic stable asthma, with only one recent study exploring their efficacy in acute asthma exacerbations [13].
The utilization of antibiotics in the management of asthma exacerbations is a common practice. Still, there is limited documentation regarding the specific situations in which treatment is warranted and the advantages it offers. According to the 2018 Global Initiative for Asthma (GINA) guidelines, the routine prescription of antibiotics for asthma exacerbations is discouraged. This recommendation is primarily rooted in the absence of universally accepted criteria for administering antibiotics during acute asthma exacerbations. While infections frequently trigger asthma exacerbations, most infection-related exacerbations are linked to viral pathogens [14].
Much current interest focuses on the role of childhood infections in determining the immune system in early life. It has been suggested that growing up in a relatively non-infective environment may predispose towards an IgE response to allergens (the hygiene hypothesis). Conversely, growing up in an infected environment may prevent the immune system from developing allergic responses. Components of bacteria (e.g., lipo-polysaccharide endotoxin; immune-stimulatory CpG DNA sequences; flagellin), viruses (e.g., SS- and DS-RNA), and fungi (e.g., chiton, a cell wall component) can stimulate up to 10 different toll-like receptors (TLRs) expressed on immune and epithelial cells to direct the immune and inflammatory response away from the allergic (Th2) towards protective (Th1 and T reg) pathways. Th1 immunity is associated with antimicrobial protective immunity, whereas regulatory T cells are strongly implicated in tolerance to allergens [15]. On the other hand, the use of antibiotics in early life has been linked to the development of asthma [16, 17]. Also, delivery via cesarean section is associated with an increased risk of asthma by 20-80%; this increased risk is attributed to the lack of healthy bacterial colonization that the newborn would have acquired from passage through the birth canal [18]. There is a link between asthma and degree of affluence, as less affluent individuals are more liable to bacterial infection [19].
There is increasing evidence that atypical respiratory pathogens such as Chlamydia pneumonia and mycoplasma pneumonia may contribute to the pathogenesis of both stable asthma and asthma exacerbation [20]. It is postulated that these organisms may contribute to inflammation in the airways, possibly by activating inflammatory mechanisms in the respiratory tract [21]. Macrolide antibiotics may play a part in managing asthma by exerting anti-inflammatory effects on the chronically inflamed airways in addition to their anti-infective action [21]. The ketolide antibiotics may also have similar properties. Recent studies on asthmatic patients with evidence of atypical infection suggest that specific antimicrobial treatment macrolides and fluoroquinolones may confer additional advantages compared to standard therapy alone [22]. A considerable amount of data has been describing additional effects associated with macrolide treatment of reduced bronchial hyperresponsiveness and altered cytokine production by decreasing the transcription of m RNA for various cytokines inhibiting interleukin-8 release by eosinophils. These non-antimicrobial effects have been defined as anti-inflammatory activity [23].
This study aimed to show whether using antibiotics to treat acute asthmatic attacks is useful in reducing admission days and rapid recovery of acute asthma attacks.
Instrument & Methods
This cross-sectional study was conducted on acute asthmatic patients admitted from January 2021 to January 2022 in Al-Mawani General Hospital in Basrah, Southern Iraq. Out of the patients, 70 subjects were selected by random sampling according to the Cochrane formula.
Patient’s records were retrieved from AL-Mawani General Hospital after receiving a written consent form from the hospital administration. The research tool was a checklist to register the subjects’ information (duration of asthma, medical treatment, co-morbidities, hospitalization duration, antibiotic therapy, and single/combination medicine). Also, total WBC and neutrophil counts were obtained through the laboratory records of the subjects. The subjects were classified into two groups based on the duration of hospitalization, including 3≥ days and >3 days. The age range of patients was subdivided into four groups; 15-29, 30-44, 45-59, and ≥60 years. The disease durations are subdivided into four groups; 1-5, 6-10, 11-15, and 16 -20 years.
Data were analyzed using the Chi-square test through SPSS 18 software.
Findings
The mean duration of disease and the mean age of the subjects were 8.57±5.01 and 44.46±13.20 years, respectively. There was just a significant difference in the frequency of hypertension in comparing the goodness of fit between the subjects (p=0.045; Table 1).
Table 1. General characteristics of the subjects
There were no significant associations between the duration of hospitalization with age group (p=0.198) and duration of asthma (p=0.069). No significant association was observed between types of antibiotics and duration of hospitalization (p<0.05). There was an inverse relationship between the duration of hospitalization and single and combined medicine therapy by antibiotic (Table 2).
Table 2. Relationship of age range (year) of the study samples frequency (numbers in parentheses are percentages) with types of antibiotics and single/combined medicine

There was no significant association between the duration of asthma and single/combined medicine (Table 3).
Table 3. Relationship of duration of asthma (year) of the study samples frequency (numbers in parentheses are percentages) with types of antibiotics and single/combined medicine
The level of WBC had no significant difference between the 3≥ (8.72±1.96) and >3 (8.87±2.75) groups (p=0.817). Also, the level of neutrophils had no significant difference between the 3≥ (43.72±8.42) and >3 (29.92±6.05) groups (p=0.236).
Discussion
This study aimed to investigate the role of antibiotics in managing acute asthmatic attacks in patients admitted to Al-Mawani General Hospital in Basrah, Iraq. The use of antibiotics in the management of asthma exacerbations is a common practice, although the indications for treatment and the benefits of therapy are not well documented. The findings of this study showed an inverse relationship between hospitalization duration and the use of antibiotics through single or combined medicine. Global Initiative for Asthma (GINA) [14] states that antibiotics should not be routinely prescribed for asthma exacerbations. This recommendation is based on the absence of consensus criteria for using antibiotics during acute worsening of asthma symptoms. Although infection is a common trigger of asthma, most exacerbations from infections are associated with viral pathogens. GINA [15] states that evidence does not support the role of antibiotics in asthma exacerbations unless there is strong evidence of lung infection (e.g., fever and purulent sputum or radiographic evidence of pneumonia). Although Stolbrink et al. [15] do not address the appropriateness nor the necessity of antibiotic prescriptions, their findings support those patients treated with short antibiotic courses usually recovered without needing an additional antibiotic prescription. David & Stemple [14] discussed the appropriate use of antibiotics for acute asthma and found that most patients were treated with either amoxicillin or doxycycline, with a small percentage receiving macrolides. Inconsistent with the findings, Denholm et al. [24], found that antibiotics do not benefit patients hospitalized with an asthma exacerbation and may even lead to worse outcomes, including a longer hospital stay, higher costs, and greater risk of diarrhea.
Amoxicillin and ceftriaxone were the most commonly used antibiotics in this study; the most significantly useful was amoxicillin, which significantly reduced hospitalization duration compared to ceftriaxone. In accordance with these findings, Stolbrink et al. [15] found that the vast majority of patients were treated with either amoxicillin or doxycycline and a small percentage with macrolides. Treatment with amoxicillin was as effective as or more effective than the other agents, as judged by the need for a second course of antibiotics. Denholm et al. [24] found that amoxicillin is one of the most commonly prescribed antibiotics for acute lower respiratory tract infections (ALRTIs) in people with asthma. Co-amoxiclav, a combination of amoxicillin and clavulanic acid, may also treat respiratory infections in people with asthma [24].
Adding a second antibiotic to the treatment regimen further reduced the hospitalization duration and was highly significant when used as a second antibiotic. The findings are consistent with the findings of Sebastian et al. [22], which showed the benefit of using the new ketolides in managing asthma exacerbation.
The matched groups in this study, especially regarding the marker of evidence of infection by the matched WBC counts between two groups showed the exclusion of the role of infection as the cause of difference in the hospital stay. This difference appears in the presence or absence of systemic disease apart from hypertension.
The matched groups in this study, especially regarding the marker of evidence of infection by the matched WBC counts between two groups showed the exclusion of the role of infection as a cause of difference in the hospital stay. This difference appears in the presence or absence of systemic disease apart from hypertension. The duration of asthma in this study showed no significant associations with the period of hospitalization duration.
There was no significant difference between the WBC and paradoxical change in the count of neutrophils in the study's main two groups, which may explain the non-infective role of the antibiotics. However, sputum neutrophil count is superior to serum neutrophil, on which this study depends. The matched characteristics of the variable and matched occurrence of systemic disease like diabetes mellitus apart from systemic hypertension may not be appointed against the study result. Based on the need for direct microbiological diagnosis, isolation of microorganisms, and or serological confirmation of infection, and more recently, investigators have turned to biopsy and polymerase chain reaction (PCR) techniques to more accurately identify the presence of these pathogens.
One of the limitations of the study was the limited sample size. So, the authors suggest studying more sample sizes in different times and areas to evaluate the use of antibiotics to treat acute asthma. Based on the findings, it suggests the use of antibiotics in patients with acute severe asthma.
Conclusion
Amoxicillin and ceftriaxone as an additional treatment to standard therapy of acute severe asthma effectively reduces hospitalization of asthmatic patients.
Acknowledgements: We appreciate to patients participated, hospital medical and administer staff.
Ethical Permission: Research approved by scientific team of medical department.
Conflict of Interests: No Conflict of Interests.
Authors’ Contribution: Sherhan AA (First Author), Introduction Writer/Methodologist/Main Researcher (50%); Saihood HA (Second Author), Assistant Researcher/Statistical Analyst/Discussion Writer (50%)
Funding/Support: Nothing has been reported.
Keywords:
References
1. Jindal SK, Gupta D, Aggarwal AN, Agarwal R. Guidelines for management of asthma at primary and secondary levels of health care in India (2005). Indian J Chest Dis Allied Sci. 2005;47(4):309-43. [Link]
2. Global Initiative for Asthma (GINA) [Internet]. Global strategy for asthma management and prevention [Cited 2019, 6 August]. Available from: http://search.ebscohost.com/login.aspx?direct=true&db=cin20&A.N.=118972966&site=ehost-live. [Link]
3. Teach SJ, Gill MA, Togias A, Sorkness CA, Arbes SJ, Calatroni A, et al. Preseasonal treatment with either omalizumab or an inhaled corticosteroid boost to prevent fall asthma exacerbations. J Allergy Clin Immunol. 2015;136(6):1476-85. [Link] [DOI:10.1016/j.jaci.2015.09.008]
4. Trasande L, Thurston GD. The role of air pollution in asthma and other pediatric morbidities. J Allergy Clin Immunol. 2005;115(4):689-99. [Link] [DOI:10.1016/j.jaci.2005.01.056]
5. Rosser F, Brehm JM, Forno E, Acosta-Pérez E, Kurland K, Canino G, et al. Proximity to a major road, vitamin D insufficiency, and severe asthma exacerbations in Puerto Rican children. Am J Respir Crit Care Med. 2014;190(10):1190-1193. [Link] [DOI:10.1164/rccm.201408-1568LE]
6. Shmool JLC, Kubzansky LD, Newman OD, Spengler J, Shepard P, Clougherty JE. Social stressors and air pollution across New York City communities: A spatial approach for assessing correlations among multiple exposures. Environ Health. 2014;13(91). [Link] [DOI:10.1186/1476-069X-13-91]
7. Johnston SL, Pattemore PK, Sanderson G, Smith S, Lampe F, Josephs L, et al. Community study of the role of viral infections in exacerbations of asthma in 9-11 year old children. BMJ. 1995;310:1225-1229. [Link] [DOI:10.1136/bmj.310.6989.1225]
8. Jackson DJ, Johnston SL. The role of viruses in acute exacerbations of asthma. J Allergy Clin Immunol. 2010;125(6):1178-87. [Link] [DOI:10.1016/j.jaci.2010.04.021]
9. Shah R, Saltoun CA. Chapter 14: Acute severe asthma (status asthmaticus). Allergy Asthma Proc. 33:147-50. [Link] [DOI:10.2500/aap.2012.33.3547]
10. SIGN (2019). British Guideline on the Management of Asthma. Scotland: SIGN. Available from: https://www.sign.ac.uk/our-guidelines/british-guideline-on-the-management-of-asthma/ [Link]
11. Parsons JP, Hallstrand TS, Mastronarde JG. An official American Thoracic Society clinical practice guideline: exercise-induced bronchoconstriction. Am J Respir Crit Care Med. 187(9):1016-27. [Link] [DOI:10.1164/rccm.201303-0437ST]
12. Jaffe A, Bush A. Anti-inflammatory effects of macrolides in lung disease. Pediatr Pulmonol. 2001;31(6):464-73. [Link] [DOI:10.1002/ppul.1076]
13. David A, Stempel MD. Determining the appropriate use of antibiotics for the treatment of acute asthma. J Allergy Clin Immunol Pract. 2019;7(2):P554-5. [Link] [DOI:10.1016/j.jaip.2018.10.029]
14. Global Initiative for Asthma (2018). GINA report: global strategy for asthma management. Available from: https://ginasthma.org/2018-gina-report-global-strategy-for-asthma-management-and-prevention [Link]
15. Stolbrink M, Bonnett LJ, Blakey JD. Antibiotic choice and duration associate with repeat prescriptions in infective asthma exacerbations. J Allergy Clin Immunol Pract. 2019;7:548-553 [Link] [DOI:10.1016/j.jaip.2018.07.049]
16. Rai SP, Patil AP, Vardhan V, Marwah V, Pethe M, Pandey IM. Best treatment guideline for bronchial asthma. Med J armed force india. 2007;63(3):264-8 [Link] [DOI:10.1016/S0377-1237(07)80151-1]
17. Kumar P, Clark ML. Kumar & Clark's clinical medicine (7th ed). Amsterdam: Elsevier; 2009. [Link]
18. Murk W, Risnes KR, Bracken MB. Prenatal or early life exposure to antibiotics and risk of childhood asthma: a systematic review. Pediatrics. 2011;127(6):1125-38. [Link] [DOI:10.1542/peds.2010-2092]
19. Neu J, Rushing J. Cesarean versus vaginal delivery: long-term infant outcomes and the hygiene hypothesis. Clin Perinatol. 2011;38(2):321-31. [Link] [DOI:10.1016/j.clp.2011.03.008]
20. Richard JM, Monica K, Hong Wei C, Eric AB, Gail HC. A link between chronic asthma and chronic infection. J Allergy Clin Immunol. 2001;107(4):595-601 [Link] [DOI:10.1067/mai.2001.113563]
21. Biscardi S, Mathie L, Elizabeth M, Florence M, Benedicte BF, Claire H, et al. Mycoplasma pneumoniae and asthma in children. Clin Infect Diseases. 2004; 38(10):1341-6. [Link] [DOI:10.1086/392498]
22. Sebastian LJ. Macrolide antibiotics and asthma treatment. J Allergy Clin Immunol. 2006;117(6):1233-6. [Link] [DOI:10.1016/j.jaci.2006.03.035]
23. Amsden GW. Anti-inflammatory effects of macrolides-an underappreciated benefit in the treatment of community-acquired respiratory tract infections and chronic inflammatory pulmonary conditions?. J Antimicrob Chemother. 2005;55(1):10-21. [Link] [DOI:10.1093/jac/dkh519]
24. Denholm R, Vand der Warf ET, Hay AD. Use of antibiotics and asthma medication for acute lower respiratory tract infections in people with and without asthma: retrospective cohort study. Respir Res. 2020;21(4). [Link] [DOI:10.1186/s12931-019-1233-5]