Volume 14, Issue 2 (2022)
Iran J War Public Health 2022, 14(2): 119-123 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2022/03/11 | Accepted: 2022/04/1 | Published: 2022/05/30
Received: 2022/03/11 | Accepted: 2022/04/1 | Published: 2022/05/30
How to cite this article
Oleiwi S, Al-Taie A, Al-Hilali K. Risk Factors for Diabetic Nephropathy in Diabetic Patients. Iran J War Public Health 2022; 14 (2) :119-123
URL: http://ijwph.ir/article-1-1126-en.html
URL: http://ijwph.ir/article-1-1126-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
1- Department of Nursing, Alsafwa University College, Karbala, Iraq
Full-Text (HTML) (661 Views)
Introduction
Diabetes Mellitus (DM) a group of metabolic diseases characterized by chronic hyperglycemia resulting from defects in insulin secretion, insulin action, or both. Metabolic abnormalities in carbohydrates, lipids, and proteins result from the importance of insulin as an anabolic hormone. Low levels of insulin to achieve adequate response and/or insulin resistance of target tissues, mainly skeletal muscles, adipose tissue, and to a lesser extent, liver, at the level of insulin receptors, signal transduction system, and/or effector enzymes or genes are responsible for these metabolic abnormalities. The severity of symptoms is due to the type and duration of diabetes [1-3].
Diabetes mellitus prevalence is increasing around the world. It is estimated to affect 8-10% of the global population [4]. By 2035, the number of diabetics is expected to increase to 550 million [5].
Of the long-term complications of diabetes, Chronic Kidney Disease (CKD) imposes the highest burden, both in terms of financial cost and the effects on daily life. The presence and severity of CKD identify individuals who are at increased risk for adverse health outcomes, including frailty, reduced quality of life, End-Stage Renal Disease (ESRD), progressive end-organ damage at other sites and premature mortality. Indeed, excess mortality associated with type 1 diabetes and type 2 diabetes is largely confined to those with CKD [6-9]. Consequently, preventing and managing CKD in patients with diabetes is a key aim of their overall management.
Approximately half of all patients with type 2 diabetes and one-third with type 1 diabetes will develop CKD, which is clinically defined by the presence of impaired renal function or elevated urinary albumin excretion or both [10, 11].
Diabetic Kidney Disease (DKD) or Diabetic Nephropathy (DN) can occur in both forms of DM (1 and 2), although type 2 has a lower rate of progression to End Stage Kidney Disease (ESKD) and End Stage Renal Failure (ESRF), because of higher prevalence of type 2 DM [12]. Not all patients with DM develop kidney disease, which leads to kidney failure, although up to 10-50% of them develop DN, which leads to ESRF and hemodialysis or kidney transplantation [12, 13].
Diabetic kidney disease is a common cause of ESKD in the western world [14]. Diabetic nephropathy (DN) is a clinical disease characterized by a persistent increase in urinary albumin excretion, increased arterial blood pressure, a progressive decline in Glomerular Filtration Rate (GFR), and a significant risk of cardiovascular morbidity and death [15].
In general, well-known risk factors for DKD (or DN) include: age, male sex, hyperglycemia, hypertension, hypovitaminosis D, obesity, chronicity, insulin resistance and some other factors [16].
As previously stated, not all diabetics experience complications. The evolution of DN and those who have it vary according to the influence of risk factors.
DN histopathology starts with a gradual thickening of the glomerular membrane base, which progresses faster or slower depending on the severity of the risk factors for mesangial matrix deposition and podocyte loss, and ends to Kimmelsteil-Wilson nodules and glomerular sclerosis with increased urinary albumin excretion, ending into ESRF or ESKD [15].
DN is now thought to be caused by genetic and environmental factors [17]. Poor glycemic control results in to liberation of glycation products, this with other metabolites and hemodynamic factors have toxic effects on the glomerulus causing their damage.
Diabetic nephropathy is not an uncommon complication of DM among geriatric population [14], and the incidence of DN and ESRD as a result of DM increases with age [4]. Some reports indicate an increase in the incidence of DN in men compared to women [4]. Other reports suggested that type 2 diabetes and DN are more common in women (1 in 4) than men (1 in 5) [18].
Racial, genetics and familial predisposition may play a marked role in the epidemiology of DKD [17, 19-22].
Obesity with type 2 diabetes affects the rate and progression of kidney disease (CKD) and End-Stage Renal Disease (ESRD). However, obesity may increase the risk of renal disease even if type 2 diabetes is not present [23, 24].
Diabetic kidney disease is uncommon in diabetes with a duration shorter than a decade; after which the incidence increases by about 3% to per year [16].
Diabetic nephropathy can be stopped or reduced by continuously monitoring patients, especially in the early stages, detecting risk factors, and treating modifiable factors, such as hyperglycemia, hypertension, obesity, smoking, and hyperlipidemia [25].
Screening should start after five years of diagnosis of type 1 DM and immediately after diagnosis of type 2 DM.
Estimation of urinary albumin and urinary creatinine excretion, as well as albumin creatinine ratio, are all part of routine screening. Other tests may be needed, for example renal function test, GFR and renal biopsy [13].
Angiotensin Converting Enzyme Inhibitors (ACEIs) and angiotensin receptor blockers can help reduce or stop diabetic nephropathy [26].
The aim of this study was to identify the risk factors for diabetic nephropathy in diabetic patients.
Instruments and Methods
In this cross-sectional descriptive research, 121 patients (66 women and 55 men) with T2 DM referred to the Diabetic Clinic of the Medical City of Al-Hussein Teaching Hospital, Karbala Holy City, Iraq, were studied from October 2019 to April 2021.
Initially, written consent was obtained from patients stating their willingness to participate in the study in accordance with human rights guidelines.
In the first stage, a complete history of the patients was taken and then a physical examination was performed. For this purpose, Blood Pressure (BP) was checked twice while sitting. If the blood pressure was above 140/90 mm Hg, high blood pressure was considered.
Then the patient's weight and height were assessed using Physician Balance Beam Scale. Body Mass Index (BMI) was calculated based on the following formula:
BMI (kg/m2) = Weight in kg / (Height in meters)2
where BMI = 18-24.9 kg/m2 is normal, BMI = 25-29.9 kg/m2 is overweight and BMI ≥30 kg/m2 is obese.
After that, 5 ml of aspirated blood and 100 ml of urine were collected from each patient and both were sent to the laboratory for biochemical tests and urinalysis. Urine albumin from urine sample was measured in mg/dl turbid metric point method by 1-chroma instrument and urine creatinine was measured by spectrophotometer in g/dl. The Albumin-to-Creatinine Ratio (ACR) was then calculated as follows:
ACR = 0-29 is normal, ACR=30-300 is microalbumiurea, and ACR >300 is macroalbuminurea.
Finally, the collected data were statistically analyzed using SPSS 22 software and Chi-square test.
Findings
A total of 121 patients (66 women and 55 men) participated in the study. The mean age of patients was 54±2.1 years in the range of 30-80 years.
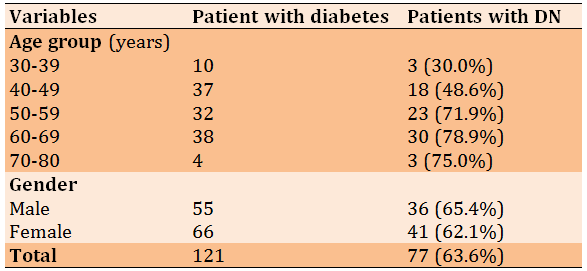
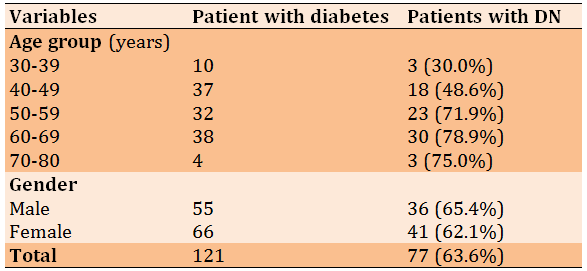
There was a significant relationship between age and DN (p<0.05). The incidence of DN was also higher in men than women (Table 1).
Table 1) Relationship between age and gender with Diabetes Nephropathy (DN)
Persistent hyperglycemia represented by HbA1c and Random Blood Sugar (RBS) showed a significant relationship with DN represented by ACR (p<0.01; Table 2).
The relationship between obesity represented by BMI with ACR was also significant (p<0.05; Table 3).
Table 4 shows the relationship between duration of DM and DN and as you can see, the incidence of diabetic nephropathy increased with the duration of diabetes (p<0.05).
Table 2) Relationship between HbA1c and RBS with ACR
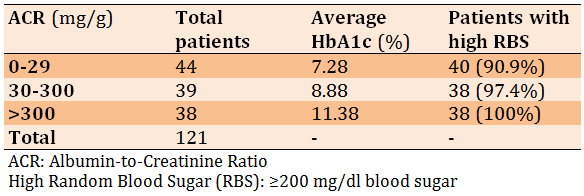
Table 3) Relationship between BMI and ACR

Table 4) Relationship between chronicity of DM (duration in years) and ACR

Discussion
In developed and developing countries, diabetes mellitus (DM) is the most common cause of chronic kidney failure (CKF) [27]. In Malaysia, between 2009 and 2011, DM was the predominant cause of ESRD in about 60% of patients, while in Russia, Singapore, South Korea, Hong Kong, Israel, Taiwan, the Philippines, Japan, the United States and New Zealand, 40-50% of patients with DM develop ESRD [15].
Diabetic Nephropathy (DN) is the most common cause of ESRD in the United States [28] and Australia, as well as many other countries [4]. DN affects about one-third of people with type 1 and type 2 diabetes in the United States [16].
The aim of this study was to identify the role of age, sex, glycemic control, obesity and duration of diabetes on diabetic nephropathy (DN).
The aim of this study was to identify the role of age, sex, glycemic control, obesity and duration of diabetes on diabetic nephropathy (DN).
As people get older, they are more likely to develop DN and ESRD as a result of diabetes. It is also more common in the elderly who have had type 2 diabetes for a long time. Although the role of age in the development of DKD is unknown, the average age of patients with ESRD is about 60 years [29].
According to the National Health and Nutrition Examination Survey results from 1999 to 2004, the incidence of chronic kidney disease increases dramatically with age, so that more than a third of people aged 70 and older with moderate or severe CKD are diagnosed, which is defined as the estimated Glomerular Filtration Rate (eGFR) of less than 60 ml/minutes [30].
Our results in Table 1 show an increase in the incidence of DN with increasing age and are consistent with this concept.
In the present study, the incidence of nephropathy was higher in men than women, which is consistent with the results of Lim study [4], but in other reports, the prevalence of DN was higher in women [18]. According to Yu et al.’s study, women with diabetes showed a higher prevalence of advanced DKD and common risk factors for DKD than men, and these differences were more pronounced among the elderly [31].
Hyperglycemia is a known risk factor for DN because high blood sugar continuously causes damage to glomeruli through its toxic metabolite or glycation product. In the present study, persistent hyperglycemia represented by HbA1c and Random Blood Sugar (RBS) showed a significant relationship with DN represented by ACR. This finding is consistent with the results of previous studies [16, 18, 27, 32].
Obesity is an important risk factor for diabetes and kidney disease. Obesity may increase the risk of kidney damage even if you do not have type 2 diabetes [33].
This study showed a significant association between obesity as a risk factor and DN. There are studies from various parts of the world that try to link racial, ethical, genetics, and familial profile to DN; for example Mooyaart et al. in a meta-analysis found 24 genetic variants associated with diabetic nephropathy [17, 22]. Satko et al. [19]. In a study, Pettitt et al. investigated the familial predisposition to renal disease in two generations of Pima Indians with type 2 (non-insulin-dependent) diabetes mellitus and conclouded that the asymptomatic elevations in urinary albumin excretion and serum creatinine levels are frequently present in diabetic sibs of African American individuals with overt type 2 DN [20]. In addition, a longitudinal cohort study was conducted by Young et al. on veterans with diabetes and racial minority groups were analyzed for baseline differences in prevalence of early diabetic nephropathy, diabetic End-Stage Renal Disease (ESRD), and longitudinal risk of mortality compared with Caucasians [21]. Native Americans, Hispanics, and African Americans have also been shown to be significantly more likely to develop ESRD than non-Hispanic whites with type 2 diabetes. Therefore, these factors may play a marked role in the epidemiology of diabetic kidney disease (DKD) [34].
Finally, our results showed a significant association between the duration of DM and the development of DN. Diabetic nephropathy does not occur early in type 1 diabetes and is uncommon in diabetes with a duration shorter than a decade; after that, the incidence rate increases by about 3% per year [5]. On the other hand, DN may be detected shortly after the diagnosis of type 2 diabetes, especially if it is ignored and not controlled, and especially in the presence of other risk factors.
Conclusion
Age, persistent hyperglycemia, obesity and duration of diabetes are involved in the development of diabetic nephropathy in diabetic patients.
Acknowledgments: None declared.
Ethical Permissions: None declared.
Conflicts of Interests: None declared.
Authors’ Contributions: Oleiwi SR (First Author), Introduction Writer/Main Researcher (40%); Al-Taie AM (Second Author), Assistant Researcher /Discussion Writer (30%); Al-Hilali KA (Third Author), Methodologist (30%)
Funding/Support: None declared.
Diabetes Mellitus (DM) a group of metabolic diseases characterized by chronic hyperglycemia resulting from defects in insulin secretion, insulin action, or both. Metabolic abnormalities in carbohydrates, lipids, and proteins result from the importance of insulin as an anabolic hormone. Low levels of insulin to achieve adequate response and/or insulin resistance of target tissues, mainly skeletal muscles, adipose tissue, and to a lesser extent, liver, at the level of insulin receptors, signal transduction system, and/or effector enzymes or genes are responsible for these metabolic abnormalities. The severity of symptoms is due to the type and duration of diabetes [1-3].
Diabetes mellitus prevalence is increasing around the world. It is estimated to affect 8-10% of the global population [4]. By 2035, the number of diabetics is expected to increase to 550 million [5].
Of the long-term complications of diabetes, Chronic Kidney Disease (CKD) imposes the highest burden, both in terms of financial cost and the effects on daily life. The presence and severity of CKD identify individuals who are at increased risk for adverse health outcomes, including frailty, reduced quality of life, End-Stage Renal Disease (ESRD), progressive end-organ damage at other sites and premature mortality. Indeed, excess mortality associated with type 1 diabetes and type 2 diabetes is largely confined to those with CKD [6-9]. Consequently, preventing and managing CKD in patients with diabetes is a key aim of their overall management.
Approximately half of all patients with type 2 diabetes and one-third with type 1 diabetes will develop CKD, which is clinically defined by the presence of impaired renal function or elevated urinary albumin excretion or both [10, 11].
Diabetic Kidney Disease (DKD) or Diabetic Nephropathy (DN) can occur in both forms of DM (1 and 2), although type 2 has a lower rate of progression to End Stage Kidney Disease (ESKD) and End Stage Renal Failure (ESRF), because of higher prevalence of type 2 DM [12]. Not all patients with DM develop kidney disease, which leads to kidney failure, although up to 10-50% of them develop DN, which leads to ESRF and hemodialysis or kidney transplantation [12, 13].
Diabetic kidney disease is a common cause of ESKD in the western world [14]. Diabetic nephropathy (DN) is a clinical disease characterized by a persistent increase in urinary albumin excretion, increased arterial blood pressure, a progressive decline in Glomerular Filtration Rate (GFR), and a significant risk of cardiovascular morbidity and death [15].
In general, well-known risk factors for DKD (or DN) include: age, male sex, hyperglycemia, hypertension, hypovitaminosis D, obesity, chronicity, insulin resistance and some other factors [16].
As previously stated, not all diabetics experience complications. The evolution of DN and those who have it vary according to the influence of risk factors.
DN histopathology starts with a gradual thickening of the glomerular membrane base, which progresses faster or slower depending on the severity of the risk factors for mesangial matrix deposition and podocyte loss, and ends to Kimmelsteil-Wilson nodules and glomerular sclerosis with increased urinary albumin excretion, ending into ESRF or ESKD [15].
DN is now thought to be caused by genetic and environmental factors [17]. Poor glycemic control results in to liberation of glycation products, this with other metabolites and hemodynamic factors have toxic effects on the glomerulus causing their damage.
Diabetic nephropathy is not an uncommon complication of DM among geriatric population [14], and the incidence of DN and ESRD as a result of DM increases with age [4]. Some reports indicate an increase in the incidence of DN in men compared to women [4]. Other reports suggested that type 2 diabetes and DN are more common in women (1 in 4) than men (1 in 5) [18].
Racial, genetics and familial predisposition may play a marked role in the epidemiology of DKD [17, 19-22].
Obesity with type 2 diabetes affects the rate and progression of kidney disease (CKD) and End-Stage Renal Disease (ESRD). However, obesity may increase the risk of renal disease even if type 2 diabetes is not present [23, 24].
Diabetic kidney disease is uncommon in diabetes with a duration shorter than a decade; after which the incidence increases by about 3% to per year [16].
Diabetic nephropathy can be stopped or reduced by continuously monitoring patients, especially in the early stages, detecting risk factors, and treating modifiable factors, such as hyperglycemia, hypertension, obesity, smoking, and hyperlipidemia [25].
Screening should start after five years of diagnosis of type 1 DM and immediately after diagnosis of type 2 DM.
Estimation of urinary albumin and urinary creatinine excretion, as well as albumin creatinine ratio, are all part of routine screening. Other tests may be needed, for example renal function test, GFR and renal biopsy [13].
Angiotensin Converting Enzyme Inhibitors (ACEIs) and angiotensin receptor blockers can help reduce or stop diabetic nephropathy [26].
The aim of this study was to identify the risk factors for diabetic nephropathy in diabetic patients.
Instruments and Methods
In this cross-sectional descriptive research, 121 patients (66 women and 55 men) with T2 DM referred to the Diabetic Clinic of the Medical City of Al-Hussein Teaching Hospital, Karbala Holy City, Iraq, were studied from October 2019 to April 2021.
Initially, written consent was obtained from patients stating their willingness to participate in the study in accordance with human rights guidelines.
In the first stage, a complete history of the patients was taken and then a physical examination was performed. For this purpose, Blood Pressure (BP) was checked twice while sitting. If the blood pressure was above 140/90 mm Hg, high blood pressure was considered.
Then the patient's weight and height were assessed using Physician Balance Beam Scale. Body Mass Index (BMI) was calculated based on the following formula:
BMI (kg/m2) = Weight in kg / (Height in meters)2
where BMI = 18-24.9 kg/m2 is normal, BMI = 25-29.9 kg/m2 is overweight and BMI ≥30 kg/m2 is obese.
After that, 5 ml of aspirated blood and 100 ml of urine were collected from each patient and both were sent to the laboratory for biochemical tests and urinalysis. Urine albumin from urine sample was measured in mg/dl turbid metric point method by 1-chroma instrument and urine creatinine was measured by spectrophotometer in g/dl. The Albumin-to-Creatinine Ratio (ACR) was then calculated as follows:
ACR = 0-29 is normal, ACR=30-300 is microalbumiurea, and ACR >300 is macroalbuminurea.
Finally, the collected data were statistically analyzed using SPSS 22 software and Chi-square test.
Findings
A total of 121 patients (66 women and 55 men) participated in the study. The mean age of patients was 54±2.1 years in the range of 30-80 years.
There was a significant relationship between age and DN (p<0.05). The incidence of DN was also higher in men than women (Table 1).
Table 1) Relationship between age and gender with Diabetes Nephropathy (DN)
Persistent hyperglycemia represented by HbA1c and Random Blood Sugar (RBS) showed a significant relationship with DN represented by ACR (p<0.01; Table 2).
The relationship between obesity represented by BMI with ACR was also significant (p<0.05; Table 3).
Table 4 shows the relationship between duration of DM and DN and as you can see, the incidence of diabetic nephropathy increased with the duration of diabetes (p<0.05).
Table 2) Relationship between HbA1c and RBS with ACR
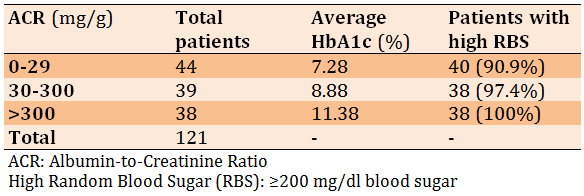
Table 3) Relationship between BMI and ACR

Table 4) Relationship between chronicity of DM (duration in years) and ACR

Discussion
In developed and developing countries, diabetes mellitus (DM) is the most common cause of chronic kidney failure (CKF) [27]. In Malaysia, between 2009 and 2011, DM was the predominant cause of ESRD in about 60% of patients, while in Russia, Singapore, South Korea, Hong Kong, Israel, Taiwan, the Philippines, Japan, the United States and New Zealand, 40-50% of patients with DM develop ESRD [15].
Diabetic Nephropathy (DN) is the most common cause of ESRD in the United States [28] and Australia, as well as many other countries [4]. DN affects about one-third of people with type 1 and type 2 diabetes in the United States [16].
The aim of this study was to identify the role of age, sex, glycemic control, obesity and duration of diabetes on diabetic nephropathy (DN).
The aim of this study was to identify the role of age, sex, glycemic control, obesity and duration of diabetes on diabetic nephropathy (DN).
As people get older, they are more likely to develop DN and ESRD as a result of diabetes. It is also more common in the elderly who have had type 2 diabetes for a long time. Although the role of age in the development of DKD is unknown, the average age of patients with ESRD is about 60 years [29].
According to the National Health and Nutrition Examination Survey results from 1999 to 2004, the incidence of chronic kidney disease increases dramatically with age, so that more than a third of people aged 70 and older with moderate or severe CKD are diagnosed, which is defined as the estimated Glomerular Filtration Rate (eGFR) of less than 60 ml/minutes [30].
Our results in Table 1 show an increase in the incidence of DN with increasing age and are consistent with this concept.
In the present study, the incidence of nephropathy was higher in men than women, which is consistent with the results of Lim study [4], but in other reports, the prevalence of DN was higher in women [18]. According to Yu et al.’s study, women with diabetes showed a higher prevalence of advanced DKD and common risk factors for DKD than men, and these differences were more pronounced among the elderly [31].
Hyperglycemia is a known risk factor for DN because high blood sugar continuously causes damage to glomeruli through its toxic metabolite or glycation product. In the present study, persistent hyperglycemia represented by HbA1c and Random Blood Sugar (RBS) showed a significant relationship with DN represented by ACR. This finding is consistent with the results of previous studies [16, 18, 27, 32].
Obesity is an important risk factor for diabetes and kidney disease. Obesity may increase the risk of kidney damage even if you do not have type 2 diabetes [33].
This study showed a significant association between obesity as a risk factor and DN. There are studies from various parts of the world that try to link racial, ethical, genetics, and familial profile to DN; for example Mooyaart et al. in a meta-analysis found 24 genetic variants associated with diabetic nephropathy [17, 22]. Satko et al. [19]. In a study, Pettitt et al. investigated the familial predisposition to renal disease in two generations of Pima Indians with type 2 (non-insulin-dependent) diabetes mellitus and conclouded that the asymptomatic elevations in urinary albumin excretion and serum creatinine levels are frequently present in diabetic sibs of African American individuals with overt type 2 DN [20]. In addition, a longitudinal cohort study was conducted by Young et al. on veterans with diabetes and racial minority groups were analyzed for baseline differences in prevalence of early diabetic nephropathy, diabetic End-Stage Renal Disease (ESRD), and longitudinal risk of mortality compared with Caucasians [21]. Native Americans, Hispanics, and African Americans have also been shown to be significantly more likely to develop ESRD than non-Hispanic whites with type 2 diabetes. Therefore, these factors may play a marked role in the epidemiology of diabetic kidney disease (DKD) [34].
Finally, our results showed a significant association between the duration of DM and the development of DN. Diabetic nephropathy does not occur early in type 1 diabetes and is uncommon in diabetes with a duration shorter than a decade; after that, the incidence rate increases by about 3% per year [5]. On the other hand, DN may be detected shortly after the diagnosis of type 2 diabetes, especially if it is ignored and not controlled, and especially in the presence of other risk factors.
Conclusion
Age, persistent hyperglycemia, obesity and duration of diabetes are involved in the development of diabetic nephropathy in diabetic patients.
Acknowledgments: None declared.
Ethical Permissions: None declared.
Conflicts of Interests: None declared.
Authors’ Contributions: Oleiwi SR (First Author), Introduction Writer/Main Researcher (40%); Al-Taie AM (Second Author), Assistant Researcher /Discussion Writer (30%); Al-Hilali KA (Third Author), Methodologist (30%)
Funding/Support: None declared.
Keywords:
References
1. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014;37 Suppl 1:S81-90. [Link] [DOI:10.2337/dc14-S081]
2. Craig ME, Hattersley A, Donaghue KC. Definition, epidemiology and classification of diabetes in children and adolescents. Pediatr Diabetes. 2009;10 Suppl 12:3-12. [Link] [DOI:10.1111/j.1399-5448.2009.00568.x]
3. Galtier F. Definition, epidemiology, risk factors. Diabetes Metab. 2010;36(6 Pt 2):628-51. [Link] [DOI:10.1016/j.diabet.2010.11.014]
4. Lim AK. Diabetic nephropathy - complications and treatment. Int J Nephrol Renovasc Dis. 2014;7:361-81. [Link] [DOI:10.2147/IJNRD.S40172]
5. Anderson AR, Christian sen JS, Anderson JK, Kreiner S, Deckert T. Diabetic nephropathy in Type 1 (insulin-dependent) diabetes: an epidemiological study. Diabetologia. 1983;25(6):496-501. [Link] [DOI:10.1007/BF00284458]
6. Groop PH, Thomas MC, Moran JL, Wadèn J, Thorn LM, et al. The presence and severity of chronic kidney disease predicts all-cause mortality in type 1 diabetes. Diabetes. 2009;58(7):1651-8. [Link] [DOI:10.2337/db08-1543]
7. Orchard TJ, Secrest AM, Miller RG, Costacou T. In the absence of renal disease, 20 year mortality risk in type 1 diabetes is comparable to that of the general population: a report from the Pittsburgh Epidemiology of Diabetes Complications Study. Diabetologia. 2010;53(11):2312-9. [Link] [DOI:10.1007/s00125-010-1860-3]
8. Bruno G, Merletti F, Bargero G, Novelli G, Melis D, et al. Estimated glomerular filtration rate, albuminuria and mortality in type 2 diabetes: the Casale Monferrato study. Diabetologia. 2007;50(5):941-8. [Link] [DOI:10.1007/s00125-007-0616-1]
9. Afkarian M, Sachs MC, Kestenbaum B, Hirsch IB, Tuttle KR, et al. Kidney disease and increased mortality risk in type 2 diabetes. J Am Soc Nephrol. 2013;24(2):302-8. [Link] [DOI:10.1681/ASN.2012070718]
10. Thomas MC, Weekes AJ, Broadley OJ, Cooper ME, Mathew TH. The burden of chronic kidney disease in Australian patients with type 2 diabetes (the NEFRON study). Med J Aust. 2006;185(3):140-4. [Link] [DOI:10.5694/j.1326-5377.2006.tb00499.x]
11. Dwyer JP, Parving HH, Hunsicker LG, Ravid M, Remuzzi G, Lewis JB. Renal dysfunction in the presence of normoalbuminuria in type 2 diabetes: results from the DEMAND study. Cardiorenal Med. 2012;2(1):1-10. [Link] [DOI:10.1159/000333249]
12. American Diabetes Association. Nephropathy in diabetes. Diabetes Care. 2004;27:S79-83. [Link] [DOI:10.2337/diacare.27.2007.S79]
13. Myo Clinic. Diabetic nephropathy (kidney disease) [Internet]. Scottsdale, Arizona: Myo Clinic; 2020 [cited 2021 Apr 1]. Available from: https://www.mayoclinic.org/diseases-conditions/diabetic-nephropathy/symptoms-causes/syc-20354556 [Link]
14. Rabkin R. Diabetic nephropathy. Clin Cornerstone. 2003;5(2): 1-11. [Link] [DOI:10.1016/S1098-3597(03)90014-7]
15. Cooper ME. Pathogenesis, prevention, and treatment of diabetic nephropathy. Lancet. 1998;352(9123):213-9. [Link] [DOI:10.1016/S0140-6736(98)01346-4]
16. Gheith O, Farouk N, Nampoory N, Halim MA, Al- Otaibi T. Diabetic kidney disease: world wide difference of prevalence and risk factors. J Nephropharmacol. 2015;5(1):49-56. [Link]
17. Mooyaart AL, Valk EJJ, Van Es LA, Bruijn JA, de Heer E, et al. Genetic associations in diabetic nephropathy: a meta-analysis. Diabetologia. 2011;54(3):544-53. [Link] [DOI:10.1007/s00125-010-1996-1]
18. MyDr. Diabetic nephropathy [Internet]. MyDr; 2020 [cited 2021 Apr 1]. Available from: https://www.mydr.com.au/diabetic-nephropathy/ [Link]
19. Satko SG, Longefeld CD, Daeihagh P, Bowden DW, Rich SS, Freeman BI. Nephropathy in siblings of African Americans with overt type 2 diabetic nephropathy. Am J Kidney Dis. 2002;40(3):489-94. [Link] [DOI:10.1053/ajkd.2002.34888]
20. Pettitt DJ, Saad MF, Bennett PH, Nelson RG, knowler WC. Familial predisposition to renal disease in two generations of Pima Indians with type 2 (non-insulin-dependent) diabetes mellitus. Diabtologia. 1990,33(7):438-43. [Link] [DOI:10.1007/BF00404096]
21. Young BA, Maynard C, Boyko EJ. Racial differences in diabetic nephropathy, cardiovascular disease, and mortality in a national population of veterans.Diabetes Care. 2003;26(8):2392-9. [Link] [DOI:10.2337/diacare.26.8.2392]
22. Mooyarrt AL. Genetic associations in diabetic nephropathy. Clin Exp Nephrol. 2014;18(2):197-200. [Link] [DOI:10.1007/s10157-013-0874-9]
23. Marric Bilkan C. Obesity and diabetic kidney disease. Med Clin North Am. 2013;97(1):59-74. [Link] [DOI:10.1016/j.mcna.2012.10.010]
24. Eknoyan G. Obesity, diabetes, and chronic kidney disease. Curr Diab Rep. 2007;7(6):449-53. [Link] [DOI:10.1007/s11892-007-0076-5]
25. Parving HH, Smith UM, Hammel E, Mathiesen ER, Rossing P, Nielsen F, Gall MA. Effective antihypertensive treatment postpones renal insufficiency in diabetic nephropathy. Am J Kidney Dis. 1993;22(1):188-95. [Link] [DOI:10.1016/S0272-6386(12)70185-3]
26. Parving HH, Andersen S, Jacobsen P, Christensen PK, Rossing K, et al. Angiotensin receptor blockers in diabetic nephropathy: renal and cardiovascular end points. Semin Nephrol. 2004;24(2):147-57. [Link] [DOI:10.1016/j.semnephrol.2003.11.003]
27. Kanwar YS, Wada J, Sun L, Xie P, Wallner EI, et al. Diabetic nephropathy: mechanisms of renal disease progression. Exp Biol Med (Maywood). 2008;233(1):4-11. [Link] [DOI:10.3181/0705-MR-134]
28. Weatherspoon D, Seymour T. Diabetic nephropathy or kidney disease [Internet]. Cheltenham: Medical News Today; 2019 [cited 2021 May 9]. Available from: https://www.medicalnewstoday.com/articles/319686. [Link]
29. Batuman V. What is the age distribution for diabetic nephropathy? [Internet]. New York: Medscape; 2021 cited 2021 May 9]. Available from: https://www.medscape.com/answers/238946-42544/what-is-the-age-distribution-for-diabetic-nephropathy. [Link]
30. Prakash S, O' Hare AM. Interaction of aging and chronic kidney disease. Semin Nephrol. 2009;29(5):497-503. [Link] [DOI:10.1016/j.semnephrol.2009.06.006]
31. Yu MK, Lyles CR, Bent-Shaw LA, Young BA. Risk factor, age and sex differences in chronic kidney disease prevalence in a diabetic cohort: the pathways study. Am J Nephrol. 2012;36(3):245-51. [Link] [DOI:10.1159/000342210]
32. Thomas MC, Tikellis C, Burns WM, Bialkowski K, Cao Z, et al. Interactions between renin angiotensin system and advanced glycation in the kidney. J Am Soc Nephrol. 2005;16(10):2976-84. [Link] [DOI:10.1681/ASN.2005010013]
33. Hall JE, Crook ED, Jones DW, Wofford MR, Dubbert PM. Mechanisms of obesity-associated cardiovascular and renal disease. Am J Med Sci. 2002;324(3):127-37. [Link] [DOI:10.1097/00000441-200209000-00003]
34. de Bore, DCCT/EDIC Research Group. Kidney disease and related findings in the diabetes control and complications trial/epidemiology of diabetes interventions and complications study. Diabetes Care. 2014;37(1):24-30. [Link] [DOI:10.2337/dc13-2113]