Volume 13, Issue 2 (2021)
Iran J War Public Health 2021, 13(2): 109-113 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2021/08/20 | Accepted: 2021/08/25 | Published: 2021/09/29
Received: 2021/08/20 | Accepted: 2021/08/25 | Published: 2021/09/29
How to cite this article
Moradinia M, Sameie M, Mohamadebrahimi H, Shahraki S, Dorri S. Factors related to the Hospital Admissions of COVID-19 Patients in the Intensive Care Unit of Selected Iranian Navy Hospitals. Iran J War Public Health 2021; 13 (2) :109-113
URL: http://ijwph.ir/article-1-996-en.html
URL: http://ijwph.ir/article-1-996-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
1- Aerospace and Sub Aquatic Medicine Faculty, AJA University of Medical Sciences, Tehran, Iran, tehran
2- Department of Emergency Medicine, Golestan Hospital, Tehran, Iran
3- Department of Health in Disasters and Emergencies, School of Nursing, AJA University of Medical Sciences, Tehran, Iran
4- Department of Health Services Management, Faculty of Health and Medical Engineering, Tehran Medical Sciences, Islamic Azad University, Tehran, Iran
5- Department of Medical Surgical Nursing, Isfahan University of Medical Sciences, Isfahan, Iran
2- Department of Emergency Medicine, Golestan Hospital, Tehran, Iran
3- Department of Health in Disasters and Emergencies, School of Nursing, AJA University of Medical Sciences, Tehran, Iran
4- Department of Health Services Management, Faculty of Health and Medical Engineering, Tehran Medical Sciences, Islamic Azad University, Tehran, Iran
5- Department of Medical Surgical Nursing, Isfahan University of Medical Sciences, Isfahan, Iran
Full-Text (HTML) (902 Views)
Introduction
Pandemics have a high prevalence of infectious diseases that are normally serious, leading to an increase in morbidity and mortality in a particular region [1]. It is also related to the selection of economic, social, and political disciplines [2]. Possible epidemics and pandemics have existed throughout history, including the Black Death (plague), smallpox, cholera, Spanish flu, SARS, Ebola, and Zika [3]. Between 30 and 50% of the European population died because of the plague outbreak [4]. Since 1817, there have been seven cholera outbreaks, which are ongoing, killing 120,000 people each year [5]. The Spanish flu epidemic of 1918 killed at least 20 million people worldwide [6]. Due to poor nutritional conditions and limited access to medical care, mortality rates in low-income countries are significantly higher than in high-income ones [7].
In West Africa, the Ebola virus outbreak resulted in 28,646 infections and 11,323 deaths [1]. Pandemics can increase morbidity and death in low-income countries [1]. Pandemics have immediate and long-term devastating consequences and indirect effects such as economic and social ramifications that affect communities for years. In 2017, the Zika virus outbreak cost Latin America between $7 and $18 billion [8]. During a flu pandemic, the disease's effects remain on younger people [9]. As a result, the working-age in the countries involved has increased [10]. Microcephaly, for example, induced by the Zika virus, has a significant impact on health [11].
The coronavirus (COVID-19) outbreak began in late December 2019 in Wuhan, China, and rapidly spread worldwide [12].
The disease has gone so far that on March 11, the World Health Organization proclaimed coronary heart disease to be a pandemic [13]. Over 115,000,000 cases and nearly 2,500,000 deaths have been reported thus far, including 221 countries and regions involved (as of March 5, 2021). The coronavirus family is responsible for various well-known human diseases, including the common cold, Mers, SARS, and COVID-19, which cause more severe diseases than seasonal flu [14]. It can not be treated like the flu, so despite the similarities between the two diseases [15], the transmission rate and the virus's characteristics have resulted in more people being exposed to and dying from Covid19 [16].
The coronavirus pandemic's consequences have had far-reaching social, economic, and political consequences around the world. During the COVID-19 outbreak, the significant reduction in insurance coverage for 20 million workers in the United States caused many of them to lose their employer's insurance coverage [17]. Furthermore, accessibility to healthcare services has been significantly reduced.
According to a Lancet magazine study, the number of hospital deliveries has decreased by 43.2%. The effect of coronavirus on mental health differs from other variables [18]. With the actuation of the coronavirus crisis, the mental health consequences, including suicidal behavior, are likely to last longer [19]. Individuals and communities have suffered greatly as a result of quarantine as a means of preventing disease spread. In one study, quarantine has shown the effect of disabilities and increased abdominal obesity on Spanish children [20]. In terms of personal consequences, it is critical to analyze the disease's long-term consequences in terms of personal health, in addition to the disease's short-term consequences.
As a result, to gain awareness, aid treatment, and prevent infection, it is necessary to learn as much as possible about the virus, its characteristics, and the characteristics of the infected. In this regard, important research has been carried out throughout the world. Underlying disease was found in 191 hospitalized patients in Wuhan, with 48% of all patients having an underlying disease that could increase mortality. According to this study, the most common underlying diseases were hypertension, diabetes, and coronary artery disease [21]. Another group of Wuhan researchers discovered that aging has a direct relationship with the likelihood of reported deaths. This study also found that increasing the level of d-dimer by more than 1g/ml is associated with a higher risk of death in patients [21].
According to the findings of the Zheng et al. study, male gender, age over 65, and smoking were all risk factors for disease progression in COVID-19 patients. In patients with severe conditions, the proportion of underlying diseases such as hypertension, diabetes, heart disease, and respiratory disorders was statistically higher than in normal patients. Fever, cough, and dyspnea were all strongly associated with disease severity [22]. Although various other studies are being conducted in this area around the world, the need for study is felt in countries, especially in Iran, because there are still many unknown characteristics.
COVID-19 is still spreading throughout Iran, and all of the country's government and military hospitals are working to control and cure the sickness. The army has Iran's largest military hospital and has fought the COVID-19 with all of its power. The majority of Army hospitals' beds have been allocated to COVID-19 military and civilian patients. The data collected from these patients has not been effectively examined thus far, and it is critical to examine the hidden dimensions and elements influencing the parameters associated with COVID-19 patients' admission in hospital intensive care units.
Investigating factors associated with patient hospitalization in a hospital's intensive care unit can improve the intensive care unit's productivity and play a role in future health management and policy, especially since Winter 2021, no similar study has been conducted. As a result, this study aimed to investigate the factors that contributed to the hospitalization of COVID-19 patients in the intensive care unit of selected Iranian Military Navy Hospitals.
Instrument and Methods
This descriptive study was conducted on all patients with suspected COVID-19 virus symptoms in Iranian military hospitals. During three months, 367 people with COVID-19 were investigated in Naval Hospitals affiliated with the Army of Tehran and Gilan Provinces, Iran (March to May 2020). The study was conducted using a census sampling method, which meant that all subjects who tested positive for COVID-19 were included in the study through continuous sampling. Conscious willingness and consent to participate in the study, definite COVID-19 infection, and hospitalization were all required for inclusion. Incomplete form completion and patient refusal to continue participating in the study were exclusion criteria.
The data collection tool was a checklist created by the researcher, which included demographic data (age, gender, marital status, pregnancy, BMI), disease information underlying such as heart disease, lung disease, immune system deficiency, blood pressure, diabetes, and cancer, and Clinical signs may include fever, cough, sore throat, shortness of breath, chills, headache, muscle aches, and gastrointestinal symptoms. The Kuder Richardson method was used to assess the reliability of this checklist, yielding a score of 0.781 (all checklist questions were "Yes/No"). In addition, the method used in this study to determine the instrument's validity was the content and the face of the validity. Each questionnaire, the degree of clarity and simplicity in each phrase of the tool, was evaluated and examined by ten faculty members, and the checklist was finalized when correct comments were submitted.
In analyzing statistical indicators and describing variables, the central and dispersion indices were used to evaluate the mean differences between variables, chi-square, and t-test. Finally, logistic regression is used to determine the predictor variables. SPSS 23 was used to analyze the data.
Findings
367 military and civil populations in the Golestan Naval Hospital in Tehran and Valiasr in Rasht were examined. The mean±SD age of participants was 57.01±16.25 years. The mean±SD age was 55.16±15.62 years in the inpatient ward and 61.82±16.92 years in the intensive care unit. More than 50% of those admitted to the hospital were employed and retired mainly.
The findings revealed that 180 patients (49.04%) with COVID-19 had no underlying disease, while 187 patients (50.96%) had at least one. High blood pressure, diabetes, and heart disease were the most common underlying diseases. Fever, cough, sore throat, shortness of breath, chills, headache, muscle aches, and digestive problems were among the clinical signs of patients with the COVID-19, and 6 (2.7%) patients with COVID-19 have no clinical symptoms. Shortness of breath, fever, cough, and chills respectively were the most common clinical findings.
Table 1) Results of demographic and clinical characteristics of two groups of patients (hospitalized and ICU patients)
Logistic regression analysis also revealed a significant relationship between patients' age, clinical signs of cough, respiration rate, blood oxygen, and diastolic blood pressure as predictive risk factors associated with intensive care unit admission (Table 2).
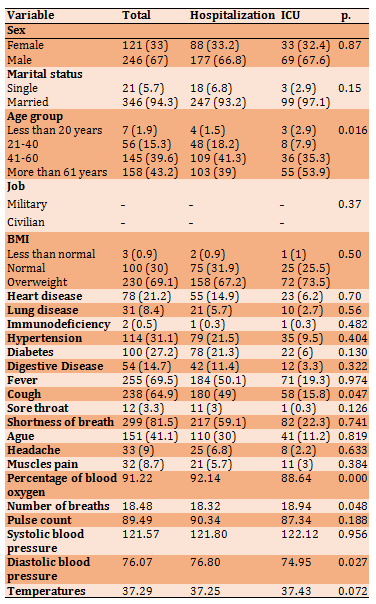
Table 2) Estimation of the odds ratio (OR) with a 95% confidence interval for risk factors associated with hospitalization of patients in selected hospitals' intensive care units.
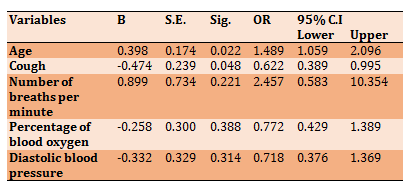
The odds ratios for age (OR=1.48) and the number of breaths per minute (OR=2.45) were the highest.
Discussion
The current study evaluated the factors influencing the hospitalization of patients in the intensive care unit of 367 patients from naval hospitals. The findings revealed that the age of patients with COVID-19 was associated with intensive care unit hospitalization. This result contradicts the findings of Grassley et al., but it is consistent with Sanchez et al.. And the research of Bart et al.. As a significant variable, as a predictor variable, it raises the risk of ICU hospitalization [23-25].
This is due to a chronic inflammatory condition of the immune system in the elderly, which may increase tissue damage caused by infections. Aging is also associated with a high prevalence of comorbidity and reduced vital organ storage capacity, leading to increasing weakness, leading to adverse consequences for older adults, and a higher risk of death from COVID19 infection [26].
The current study's results indicate that the clinical sign of cough is significantly associated with ICU hospitalization, which is consistent with the findings of Ten et al.. However, in the study of Feng Hee et al.., there is no significant relationship between cough and ICU hospitalization, which is unrelated to the current study [27, 28]. Cough has also been identified as one of the predictors of ICU hospitalization based on the findings, consistent with the Suarez et al.. study [29]. Indeed, this symptom can be used in future disease processes as a warning sign of extensive lung involvement.
Respiratory rate was not suggested to be associated with ICU admission and was not determined as a risk factor or predictor variable in this study. However, a significant variable has been suggested for ICU patients' hospitalization, related to the Young et al. study. However, no agreement was found in this study with Hee et al. [28, 30]. In this study, the percentage of blood oxygen is related to ICU hospitalization, but it is not a significant predictor of hospitalization risk for patients in this ward. The current study differs from Bargil et al. [31]. In this regard, but is similar to Petrile et al.. Patients' deterioration and hospitalization in intensive care have a significant relationship with oxygen saturation [32].
Diastolic blood pressure was significantly associated with ICU admission in the current study, which is consistent with Bromheint et al.. but not with the study of Huo et al. [33, 34].
The difference in the number of samples, race and geographical status, and type of nutrition could be the reason for this, given that diastolic blood pressure can be one of the variables of underlying heart disease. However, given that no underlying disease was significantly associated with hospitalization in the ICU, diastolic blood pressure was not predicted as a risk factor in this study.
The limitations of this study are that it only considers Navy Referral Center hospitals, that there is no distinction between the incidence of military patients from different forces, and that it is not possible to compare them. It is also suggested that military and civilian patients be examined more thoroughly. Joint supplementary studies with larger sample sizes between various military forces. Other limitations of the present research are the lack of access to patient data in the form of the confidentiality of the files of military patients and the incompleteness of some patient test findings.
Conclusion
Age may affect COVID-19 disease. Cough, hypoxia, and diastolic blood pressure appear to be clinical signs that will affect hospitalization in the intensive care unit and should be evaluated with good effort and frequency in patients with COVID-19.
Acknowledgments: We are grateful to all of the valuable professors, specialists, and patients who contributed to this study, as well as Abhad Nedaja.
Ethical Permissions: The Ethics Committee in Biomedical Research has also approved this study, which has the code of ethics (IRB) AR.AJAUMS.REC1399.084.
Conflicts of Interests: The current article results from a research project that the Research Council approved of the Vice Chancellor for Research and Technology of AJA University of Medical Sciences under the code of ethics (IRB) 1399.084 AR.AJAUMS.REC.
Authors’ Contribution: moradinia M. (first author), Main Researcher (30%); Sameie M. (Second author), Introduction Writer/Assistant Researcher (15%); Mohamadebrahimi H. (Third author), Assistant Researcher/Statistical Analyst (15%); Shahraki S. (Fourth author), Discussion Writer (10%); Dorri S. (Fifth author), Methodologist/Assistant researcher (30%).
Funding/Support: The authors state that there is no conflict of interest in the present study.
Pandemics have a high prevalence of infectious diseases that are normally serious, leading to an increase in morbidity and mortality in a particular region [1]. It is also related to the selection of economic, social, and political disciplines [2]. Possible epidemics and pandemics have existed throughout history, including the Black Death (plague), smallpox, cholera, Spanish flu, SARS, Ebola, and Zika [3]. Between 30 and 50% of the European population died because of the plague outbreak [4]. Since 1817, there have been seven cholera outbreaks, which are ongoing, killing 120,000 people each year [5]. The Spanish flu epidemic of 1918 killed at least 20 million people worldwide [6]. Due to poor nutritional conditions and limited access to medical care, mortality rates in low-income countries are significantly higher than in high-income ones [7].
In West Africa, the Ebola virus outbreak resulted in 28,646 infections and 11,323 deaths [1]. Pandemics can increase morbidity and death in low-income countries [1]. Pandemics have immediate and long-term devastating consequences and indirect effects such as economic and social ramifications that affect communities for years. In 2017, the Zika virus outbreak cost Latin America between $7 and $18 billion [8]. During a flu pandemic, the disease's effects remain on younger people [9]. As a result, the working-age in the countries involved has increased [10]. Microcephaly, for example, induced by the Zika virus, has a significant impact on health [11].
The coronavirus (COVID-19) outbreak began in late December 2019 in Wuhan, China, and rapidly spread worldwide [12].
The disease has gone so far that on March 11, the World Health Organization proclaimed coronary heart disease to be a pandemic [13]. Over 115,000,000 cases and nearly 2,500,000 deaths have been reported thus far, including 221 countries and regions involved (as of March 5, 2021). The coronavirus family is responsible for various well-known human diseases, including the common cold, Mers, SARS, and COVID-19, which cause more severe diseases than seasonal flu [14]. It can not be treated like the flu, so despite the similarities between the two diseases [15], the transmission rate and the virus's characteristics have resulted in more people being exposed to and dying from Covid19 [16].
The coronavirus pandemic's consequences have had far-reaching social, economic, and political consequences around the world. During the COVID-19 outbreak, the significant reduction in insurance coverage for 20 million workers in the United States caused many of them to lose their employer's insurance coverage [17]. Furthermore, accessibility to healthcare services has been significantly reduced.
According to a Lancet magazine study, the number of hospital deliveries has decreased by 43.2%. The effect of coronavirus on mental health differs from other variables [18]. With the actuation of the coronavirus crisis, the mental health consequences, including suicidal behavior, are likely to last longer [19]. Individuals and communities have suffered greatly as a result of quarantine as a means of preventing disease spread. In one study, quarantine has shown the effect of disabilities and increased abdominal obesity on Spanish children [20]. In terms of personal consequences, it is critical to analyze the disease's long-term consequences in terms of personal health, in addition to the disease's short-term consequences.
As a result, to gain awareness, aid treatment, and prevent infection, it is necessary to learn as much as possible about the virus, its characteristics, and the characteristics of the infected. In this regard, important research has been carried out throughout the world. Underlying disease was found in 191 hospitalized patients in Wuhan, with 48% of all patients having an underlying disease that could increase mortality. According to this study, the most common underlying diseases were hypertension, diabetes, and coronary artery disease [21]. Another group of Wuhan researchers discovered that aging has a direct relationship with the likelihood of reported deaths. This study also found that increasing the level of d-dimer by more than 1g/ml is associated with a higher risk of death in patients [21].
According to the findings of the Zheng et al. study, male gender, age over 65, and smoking were all risk factors for disease progression in COVID-19 patients. In patients with severe conditions, the proportion of underlying diseases such as hypertension, diabetes, heart disease, and respiratory disorders was statistically higher than in normal patients. Fever, cough, and dyspnea were all strongly associated with disease severity [22]. Although various other studies are being conducted in this area around the world, the need for study is felt in countries, especially in Iran, because there are still many unknown characteristics.
COVID-19 is still spreading throughout Iran, and all of the country's government and military hospitals are working to control and cure the sickness. The army has Iran's largest military hospital and has fought the COVID-19 with all of its power. The majority of Army hospitals' beds have been allocated to COVID-19 military and civilian patients. The data collected from these patients has not been effectively examined thus far, and it is critical to examine the hidden dimensions and elements influencing the parameters associated with COVID-19 patients' admission in hospital intensive care units.
Investigating factors associated with patient hospitalization in a hospital's intensive care unit can improve the intensive care unit's productivity and play a role in future health management and policy, especially since Winter 2021, no similar study has been conducted. As a result, this study aimed to investigate the factors that contributed to the hospitalization of COVID-19 patients in the intensive care unit of selected Iranian Military Navy Hospitals.
Instrument and Methods
This descriptive study was conducted on all patients with suspected COVID-19 virus symptoms in Iranian military hospitals. During three months, 367 people with COVID-19 were investigated in Naval Hospitals affiliated with the Army of Tehran and Gilan Provinces, Iran (March to May 2020). The study was conducted using a census sampling method, which meant that all subjects who tested positive for COVID-19 were included in the study through continuous sampling. Conscious willingness and consent to participate in the study, definite COVID-19 infection, and hospitalization were all required for inclusion. Incomplete form completion and patient refusal to continue participating in the study were exclusion criteria.
The data collection tool was a checklist created by the researcher, which included demographic data (age, gender, marital status, pregnancy, BMI), disease information underlying such as heart disease, lung disease, immune system deficiency, blood pressure, diabetes, and cancer, and Clinical signs may include fever, cough, sore throat, shortness of breath, chills, headache, muscle aches, and gastrointestinal symptoms. The Kuder Richardson method was used to assess the reliability of this checklist, yielding a score of 0.781 (all checklist questions were "Yes/No"). In addition, the method used in this study to determine the instrument's validity was the content and the face of the validity. Each questionnaire, the degree of clarity and simplicity in each phrase of the tool, was evaluated and examined by ten faculty members, and the checklist was finalized when correct comments were submitted.
In analyzing statistical indicators and describing variables, the central and dispersion indices were used to evaluate the mean differences between variables, chi-square, and t-test. Finally, logistic regression is used to determine the predictor variables. SPSS 23 was used to analyze the data.
Findings
367 military and civil populations in the Golestan Naval Hospital in Tehran and Valiasr in Rasht were examined. The mean±SD age of participants was 57.01±16.25 years. The mean±SD age was 55.16±15.62 years in the inpatient ward and 61.82±16.92 years in the intensive care unit. More than 50% of those admitted to the hospital were employed and retired mainly.
The findings revealed that 180 patients (49.04%) with COVID-19 had no underlying disease, while 187 patients (50.96%) had at least one. High blood pressure, diabetes, and heart disease were the most common underlying diseases. Fever, cough, sore throat, shortness of breath, chills, headache, muscle aches, and digestive problems were among the clinical signs of patients with the COVID-19, and 6 (2.7%) patients with COVID-19 have no clinical symptoms. Shortness of breath, fever, cough, and chills respectively were the most common clinical findings.
Table 1) Results of demographic and clinical characteristics of two groups of patients (hospitalized and ICU patients)
Logistic regression analysis also revealed a significant relationship between patients' age, clinical signs of cough, respiration rate, blood oxygen, and diastolic blood pressure as predictive risk factors associated with intensive care unit admission (Table 2).
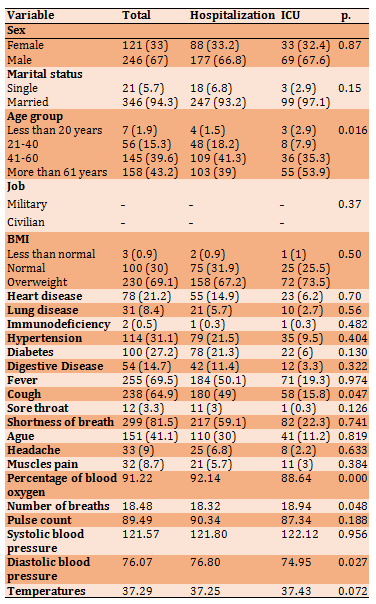
Table 2) Estimation of the odds ratio (OR) with a 95% confidence interval for risk factors associated with hospitalization of patients in selected hospitals' intensive care units.
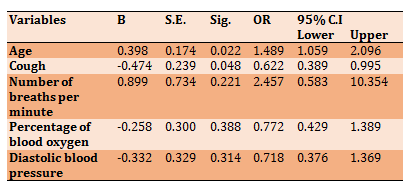
The odds ratios for age (OR=1.48) and the number of breaths per minute (OR=2.45) were the highest.
Discussion
The current study evaluated the factors influencing the hospitalization of patients in the intensive care unit of 367 patients from naval hospitals. The findings revealed that the age of patients with COVID-19 was associated with intensive care unit hospitalization. This result contradicts the findings of Grassley et al., but it is consistent with Sanchez et al.. And the research of Bart et al.. As a significant variable, as a predictor variable, it raises the risk of ICU hospitalization [23-25].
This is due to a chronic inflammatory condition of the immune system in the elderly, which may increase tissue damage caused by infections. Aging is also associated with a high prevalence of comorbidity and reduced vital organ storage capacity, leading to increasing weakness, leading to adverse consequences for older adults, and a higher risk of death from COVID19 infection [26].
The current study's results indicate that the clinical sign of cough is significantly associated with ICU hospitalization, which is consistent with the findings of Ten et al.. However, in the study of Feng Hee et al.., there is no significant relationship between cough and ICU hospitalization, which is unrelated to the current study [27, 28]. Cough has also been identified as one of the predictors of ICU hospitalization based on the findings, consistent with the Suarez et al.. study [29]. Indeed, this symptom can be used in future disease processes as a warning sign of extensive lung involvement.
Respiratory rate was not suggested to be associated with ICU admission and was not determined as a risk factor or predictor variable in this study. However, a significant variable has been suggested for ICU patients' hospitalization, related to the Young et al. study. However, no agreement was found in this study with Hee et al. [28, 30]. In this study, the percentage of blood oxygen is related to ICU hospitalization, but it is not a significant predictor of hospitalization risk for patients in this ward. The current study differs from Bargil et al. [31]. In this regard, but is similar to Petrile et al.. Patients' deterioration and hospitalization in intensive care have a significant relationship with oxygen saturation [32].
Diastolic blood pressure was significantly associated with ICU admission in the current study, which is consistent with Bromheint et al.. but not with the study of Huo et al. [33, 34].
The difference in the number of samples, race and geographical status, and type of nutrition could be the reason for this, given that diastolic blood pressure can be one of the variables of underlying heart disease. However, given that no underlying disease was significantly associated with hospitalization in the ICU, diastolic blood pressure was not predicted as a risk factor in this study.
The limitations of this study are that it only considers Navy Referral Center hospitals, that there is no distinction between the incidence of military patients from different forces, and that it is not possible to compare them. It is also suggested that military and civilian patients be examined more thoroughly. Joint supplementary studies with larger sample sizes between various military forces. Other limitations of the present research are the lack of access to patient data in the form of the confidentiality of the files of military patients and the incompleteness of some patient test findings.
Conclusion
Age may affect COVID-19 disease. Cough, hypoxia, and diastolic blood pressure appear to be clinical signs that will affect hospitalization in the intensive care unit and should be evaluated with good effort and frequency in patients with COVID-19.
Acknowledgments: We are grateful to all of the valuable professors, specialists, and patients who contributed to this study, as well as Abhad Nedaja.
Ethical Permissions: The Ethics Committee in Biomedical Research has also approved this study, which has the code of ethics (IRB) AR.AJAUMS.REC1399.084.
Conflicts of Interests: The current article results from a research project that the Research Council approved of the Vice Chancellor for Research and Technology of AJA University of Medical Sciences under the code of ethics (IRB) 1399.084 AR.AJAUMS.REC.
Authors’ Contribution: moradinia M. (first author), Main Researcher (30%); Sameie M. (Second author), Introduction Writer/Assistant Researcher (15%); Mohamadebrahimi H. (Third author), Assistant Researcher/Statistical Analyst (15%); Shahraki S. (Fourth author), Discussion Writer (10%); Dorri S. (Fifth author), Methodologist/Assistant researcher (30%).
Funding/Support: The authors state that there is no conflict of interest in the present study.
References
1. Madhav N, Oppenheim B, Gallivan M, Mulembakani P, Rubin E, Wolfe N, et al.. Pandemics: Risks, impacts, and mitigation. Washington: The International Bank for Reconstruction and Development; 2017. [Link] [DOI:10.1596/978-1-4648-0527-1_ch17] [PMID]
2. Jones KE, Patel NG, Levy MA, Storeygard A, Balk D, Gittleman JL, et al.. Global trends in emerging infectious diseases. Nature. 2008;451(7181):990-3. [Link] [DOI:10.1038/nature06536] [PMID] [PMCID]
3. Huremovic D. Brief history of pandemics (pandemics throughout history). Psychiatry Pandemics. 2019 May:7-35. [Link] [DOI:10.1007/978-3-030-15346-5_2] [PMCID]
4. DeWitte SN. Mortality risk and survival in the aftermath of the medieval black death. Plos One. 2014;9(5):96513. [Link] [DOI:10.1371/journal.pone.0096513] [PMID] [PMCID]
5. Harris JF, Larocque RC, Qadri F, Ryan ET, Calderwood SB. Cholera. Lancet. 2012;379(9835):2466-76. [Link] [DOI:10.1016/S0140-6736(12)60436-X]
6. Johnson NPAS, Mueller J. Updating the accounts: Global mortality of the 1918-1920 Spanish influenza pandemic. Bull Hist Med. 2002;76(1):105-15. [Link] [DOI:10.1353/bhm.2002.0022] [PMID]
7. Brundage JF, Shanks GD. Deaths from bacterial pneumonia during 1918-19 influenza pandemic. Emerg Infect Dis. 2008;14(8):1193. [Link] [DOI:10.3201/eid1408.071313] [PMID] [PMCID]
8. World health organization. Coronavirus disease (COVID-19) situation reports [Internet]. Geneva: World Health Organization; 2021 [cited 21 May 2021]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports. [Link]
9. Lowe R, Barcellos C, Brasil P, Cruz OG, Honório NA, Kuper H, et al.. The Zika virus epidemic in Brazil: From discovery to future implications. Int J Environ Res Public Health. 2018;15(1):96. [Link] [DOI:10.3390/ijerph15010096] [PMID] [PMCID]
10. Viboud C, Miller M, Olson DR, Osterholm M, Simonsen L. Preliminary estimates of mortality and years of life lost associated with the 2009 A/H1N1 pandemic in the US and comparison with past influenza seasons. Plos Curr. 2010;2:1153. [Link] [DOI:10.1371/currents.RRN1153] [PMID] [PMCID]
11. Riley R. A review of the impacts of the 1918 Spanish flu pandemic [Internet]. Birmingham: University of Birmingham; 2020 [cited May 21 2021]. Available from: https://blog.bham.ac.uk/cityredi/a-review-of-the-impacts-of-the-1918-spanish-flu-pandemic/. [Link]
12. Waggoner JJ, Pinsky BA. Zika virus: Diagnostics for an emerging pandemic threat. J Clin Microbiol. 2016;54(4):860-7. [Link] [DOI:10.1128/JCM.00279-16] [PMID] [PMCID]
13. Bogoch II, Watts A, Thomas-Bachli A, Huber C, Kraemer MUG, Khan K. Potential for global spread of a novel coronavirus from China. J Travel Med. 2020;27(2):11. [Link] [DOI:10.1093/jtm/taaa011] [PMID] [PMCID]
14. World health organization. Coronavirus disease (COVID-19) pandemic [Internet]. Geneva: World Health Organization; 2019 [cited 21 May 2021]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019. [Link]
15. Russell B, Moss C, George G, Santaolalla A, Cope A, Papa S, et al.. Associations between immune-suppressive and stimulating drugs and novel COVID-19-a systematic review of current evidence. Ecancermedicalscience. 2020;14:1022. [Link] [DOI:10.3332/ecancer.2020.1022] [PMID] [PMCID]
16. Hsih WH, Cheng MY, Ho MW, Chou CH, Lin PC, Chi CY, et al.. Featuring COVID-19 cases via screening symptomatic patients with epidemiologic link during flu season in a medical center of central Taiwan. J Microbiol Immunol Infect. 2020;53(3):459-66. [Link] [DOI:10.1016/j.jmii.2020.03.008] [PMID] [PMCID]
17. Zipfel CM, Bansal S. Assessing the interactions between COVID-19 and influenza in the United States. Med Rxiv. 2020 Apr:20047993. [Link]
18. Blumenthal D, Fowler EJ, Abrams M, Collins SR. COVID-19-implications for the health care system. N Engl J Med. 2020;383:1483-8. [Link] [DOI:10.1056/NEJMsb2021088] [PMID]
19. Center for global development. The indirect health effects of COVID-19: The challenges of living through a pandemic [Internet]. Washington: Center for Global Development; 2020 [cited 21 May 2021]. Available from: https://www.cgdev.org/blog/indirect-health-effects-covid-19-challenges-living-through-pandemic. [Link]
20. Sher L. The impact of the COVID-19 pandemic on suicide rates. QJM. 2020;113(10):707-12. [Link] [DOI:10.1093/qjmed/hcaa202] [PMID] [PMCID]
21. Medrano M, Cadenas‐Sanchez C, Oses M, Arenaza L, Amasene M, Labayen I. Changes in lifestyle behaviours during the COVID‐19 confinement in Spanish children: A longitudinal analysis from the MUGI project. Pediatr Obes. 2021;16(4):12731. [Link] [DOI:10.1111/ijpo.12731]
22. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al.. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020;395(10229):1054-62. [Link] [DOI:10.1016/S0140-6736(20)30566-3]
23. Zheng Z, Peng F, Xu B, Zhao J, Liu H, Peng J, et al.. Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis. J Infect. 2020;81(2):16-25. [Link] [DOI:10.1016/j.jinf.2020.04.021] [PMID] [PMCID]
24. Pijls BG, Jolani S, Atherley A, Derckx RT, Dijkstra JI, Franssen GH, et al.. Demographic risk factors for COVID-19 infection, severity, ICU admission and death: A meta-analysis of 59 studies. BMJ Open. 2021;11(1):044640. [Link] [DOI:10.1136/bmjopen-2020-044640] [PMID] [PMCID]
25. Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al.. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. 2020;323(16):1574-81. [Link] [DOI:10.1001/jama.2020.5394] [PMID] [PMCID]
26. Liu W, Tao ZW, Wang L, Yuan ML, Liu K, Zhou L, et al.. Analysis of factors associated with disease outcomes in hospitalized patients with 2019 novel coronavirus disease. Chin Med J. 2020;133(9):1032-8. [Link] [DOI:10.1097/CM9.0000000000000775] [PMID] [PMCID]
27. Shaw AC, Joshi S, Greenwood H, Panda A, Lord JM. Aging of the innate immune system. Curr Opin Immunol. 2010;22(4):507-13. [Link] [DOI:10.1016/j.coi.2010.05.003] [PMID] [PMCID]
28. Tan E, Song J, Deane AM, Plummer MP. Global impact of coronavirus disease 2019 infection requiring admission to the ICU: A systematic review and meta-analysis. Chest. 2021;159(2):524-36. [Link] [DOI:10.1016/j.chest.2020.10.014] [PMID] [PMCID]
29. He F, Quan Y, Lei M, Liu R, Qin S, Zeng J, et al.. Clinical features and risk factors for ICU admission in COVID-19 patients with cardiovascular diseases. Aging Dis. 2020;11(4):763-9. [Link] [DOI:10.14336/AD.2020.0622] [PMID] [PMCID]
30. Soares RCM, Mattos LR, Raposo LM. Risk factors for hospitalization and mortality due to COVID-19 in Espirito Santo State, Brazil. Am J Trop Med Hyg. 2020;103(3):1184-90. [Link] [DOI:10.4269/ajtmh.20-0483] [PMID] [PMCID]
31. Wang Y, Lu X, Li Y, Chen H, Chen T, Su N, et al.. Clinical course and outcomes of 344 intensive care patients with COVID-19. Am J Respir Crit Care Med. 2020;201(11):1430-4. [Link] [DOI:10.1164/rccm.202003-0736LE] [PMID] [PMCID]
32. Kokoszka-Bargiel I, Cyprys P, Rutkowska K, Madowicz J, Knapik P. Intensive care unit admissions during the first 3 months of the COVID-19 pandemic in Poland: A single-center, cross-sectional study. Med Sci Monit. 2020;26:926974. [Link] [DOI:10.12659/MSM.926974] [PMID] [PMCID]
33. Bruminhent J, Ruangsubvilai N, Nabhindhakara J, Ingsathit A, Kiertiburanakul S. Clinical characteristics and risk factors for coronavirus disease 2019 (COVID-19) among patients under investigation in Thailand. Plos One. 2020;15(9):0239250. [Link] [DOI:10.1371/journal.pone.0239250] [PMID] [PMCID]
34. Petrilli CM, Jones SA, Yang J, Rajagopalan H, O'Donnell LF, Chernyak Y, et al.. Factors associated with hospitalization and critical illness among 4,103 patients with COVID-19 disease in New York city. Med Rxiv. 2020 Apr:1-25. [Link] [DOI:10.1101/2020.04.08.20057794]








