Volume 17, Issue 3 (2025)
Iran J War Public Health 2025, 17(3): 217-222 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2025/05/29 | Accepted: 2025/07/10 | Published: 2025/07/15
Received: 2025/05/29 | Accepted: 2025/07/10 | Published: 2025/07/15
How to cite this article
Balat K, Elywy G. The Mediators of Family Involvement between Home-Based Rehabilitation and Daily Living Activities of Individuals with Disabilities. Iran J War Public Health 2025; 17 (3) :217-222
URL: http://ijwph.ir/article-1-1639-en.html
URL: http://ijwph.ir/article-1-1639-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Authors
K.Z. Balat *1, G.J. Elywy1
1- Department of Community Health Nursing, College of Nursing, University of Thi-Qar, Thi-Qar-Iraq
Full-Text (HTML) (97 Views)
Introduction
Rehabilitation is a cornerstone in restoring purposeful abilities and promoting independence among individuals with disabilities [1]. Among numerous modalities, home-based rehabilitation (HBR) has emerged as a preferred method for long-term care, particularly in community health settings [2]. HBR is an effective approach designed to enhance the involvement of patients and their families in recognizing their needs and delivering essential education [3]. By actively engaging patients in their own care, HBR empowers them to take charge of their health journey, leading to improved adherence to treatment plans. Additionally, this method fosters open communication between healthcare providers and families, ensuring that everyone is aligned in their goals and understanding of the rehabilitation process, which ultimately contributes to better health outcomes. Moreover, the personalized nature of HBR allows for tailored interventions that address specific challenges faced by patients and their families, making the rehabilitation experience more relevant and impactful. The goal of HBR is to preserve and restore patients’ health and independence while minimizing disabilities associated with chronic illnesses [4]. These services are particularly beneficial for addressing the health needs of individuals requiring rehabilitation, offering significant value due to their affordability, practicality, ability to ensure client comfort, reduction of frequent hospital visits, and the facilitation of connections between healthcare facilities and the community.
It offers the benefits of delivering therapy in a familiar environment, facilitating continuity of care, and reducing institutionalization costs [2]. Studies have shown that individuals receiving HBR demonstrate higher adherence to therapy and report greater pride compared to those undergoing facility-based rehabilitation [5, 6]. Jafari et al. showed that HBR not only enhances stroke patients’ adherence to treatment regimens in three key areas—rehabilitation, diet, and medication—but also improves their quality of life (QoL). Consequently, the authors strongly advocate for the implementation of this approach by nursing staff to more effectively engage patients with chronic conditions and their families in the ongoing care process [7].
Family members play a crucial role in providing emotional support and encouragement, which can significantly enhance a patient’s motivation to engage in rehabilitation activities. The success of HBR is not solely dependent on professional offerings; it is heavily influenced by the involvement and support of family members [8, 9]. Additionally, active participation of family in the care process helps ensure that patients adhere to treatment plans and make necessary lifestyle changes, thereby reinforcing the skills and knowledge acquired during rehabilitation. Furthermore, when families are involved, they can facilitate better communication with healthcare providers, leading to more comprehensive care that addresses the holistic needs of the patient.
Family involvement plays an important mediating role in the rehabilitation outcomes of individuals with disabilities. The presence of an engaged and supportive circle of relatives can significantly improve motivation, adherence to rehabilitation plans, and overall psychosocial well-being [10]. Research has documented that family members frequently assist with therapy, monitor progress, and provide emotional encouragement, all of which contribute to improved functional outcomes [11]. In contexts where formal rehabilitation services are limited, family involvement becomes even more vital in assisting with activities of daily living (ADLs), such as dressing, mobility, and hygiene [12, 13]. Family members often take on essential caregiving roles, providing hands-on support that can greatly enhance the quality of care and daily functioning for individuals recovering from injury or illness. Furthermore, their presence not only helps address immediate physical needs but also fosters emotional well-being, as the support of loved ones can alleviate feelings of isolation and promote a sense of stability during the recovery process.
ADLs are essential indicators of a person’s potential to function independently. The goal of successful rehabilitation programs is not only to reduce impairment but also to restore the ability to carry out vital daily responsibilities [14]. The literature indicates that higher levels of family engagement are associated with greater improvements in ADLs, particularly in populations with chronic physical or neurological disabilities [15, 16]. Despite the recognized significance of family involvement, few studies have explicitly tested its mediating role in the relationship between HBR and ADL performance. Bogner et al. assessed how family attendance at inpatient rehabilitation therapy sessions impacts the outcomes of patients with traumatic brain injury (TBI) at discharge and up to nine months afterward. They reported that family involvement in rehabilitation leads to improved outcomes; specifically, participants whose families attend therapy sessions at least 10% of the time demonstrate greater community engagement post-discharge. Additionally, family participation during inpatient rehabilitation may enhance cognitive function and community involvement for up to nine months after discharge [17]. Foster et al. concluded that having the support and involvement of one’s family during rehabilitation after a serious traumatic brain injury can significantly enhance the likelihood of achieving positive outcomes. Rehabilitation services can and should offer families the necessary support to facilitate their engagement in the rehabilitation process. This paper describes the innovative strategies that one rehabilitation service provider has implemented to effectively involve families in the rehabilitation journey, ultimately aiming to improve patient outcomes [18]. Given this gap, the current study aimed to explore the mediating impact of family involvement in the relationship between HBR and ADLs among individuals with disabilities. Understanding this dynamic can inform nursing interventions, policy development, and the design of community rehabilitation programs that emphasize family integration as a central aspect of care. The importance of this study lies in its potential to shift the focus of rehabilitation from a purely clinical approach to one that recognizes the critical role of family support in achieving successful outcomes. By demonstrating how family involvement influences rehabilitation effectiveness, the findings can encourage healthcare providers to adopt more inclusive practices that actively engage family members in the care process. Additionally, this research can serve as a foundation for developing targeted training programs for family caregivers, equipping them with the necessary skills to support their loved ones effectively. Ultimately, the insights gained from this study can contribute to more comprehensive and person-centered rehabilitation strategies, leading to enhanced quality of life for individuals with disabilities.
Materials and Methods
Study design and sample
This descriptive correlational cross-sectional study was conducted between March and June 2025 at selected community-based primary health care centers and rehabilitation facilities in Thi Qar Governorate, Iraq. The sample consisted of adults with physical or neurological disabilities who had been receiving HBR for at least three months.
The cross-sectional approach was chosen due to its suitability for assessing associations among psychosocial and functional prameters at a single point in time, which aligns with the objectives of behavioral research in community health nursing. These locations were chosen based on provider availability, accessibility, and their establishment of HBR programs.
Participants were selected using a systematic random sampling approach, guided by the rehabilitation service data. The sample size was calculated using the single population percentage formula with a 95% confidence level and a 5% margin of error, based on an initial estimate of 384 individuals. To account for potential non-response, the final sample size was adjusted to 422. Inclusion criteria included adults aged 18 years or older, currently receiving HBR, living with their family caregiver, and able to understand Arabic. Individuals with severe psychiatric disorders or those in institutionalized care were excluded.
Research tools
Data collection was conducted using an established interviewer-administered questionnaire comprising four sections. The first section covered demographic and medical factors, such as age, gender, type of disability, and duration of HBR. The second section assessed HBR using the Home-Based Rehabilitation Services Questionnaire (HBRSQ), which was developed in accordance with WHO CBR recommendations and consists of 10 items rated on a five-point Likert scale [19]. The third section evaluated family involvement through the Family Involvement Questionnaire-Rehabilitation Version (FIQ-R), which includes 12 items measuring emotional, physical, and decision-making support provided by family members [20]. The fourth section assessed ADLs using the Barthel Index, a widely used tool that evaluates basic functional tasks, such as mobility, feeding, and personal hygiene [21].
To ensure the quality and cultural appropriateness of the study tools, the questionnaire underwent content validation by a panel of five experts in rehabilitation nursing, public health, and social sciences. Based on their feedback, several items were revised for clarity. A pilot study was conducted with forty-two individuals with disabilities to evaluate the internal consistency, flow, and clarity of the instrument. The pilot responses were excluded from the final data analysis. The reliability coefficients (Cronbach’s alpha) for the primary observation tools were 0.87 for the HBRSQ, 0.88 for the FIQ-R, and 0.90 for the Barthel Index, all indicating strong internal consistency.
Data collection
Data collection was conducted with the assistance of skilled community health nurses through private, face-to-face interviews at primary healthcare centers or participants’ homes, depending on the individual’s mobility status. Each interview session lasted approximately 30 to 40 minutes. All participants provided written informed consent before participation. Confidentiality and the right to withdraw at any stage were explained. Ethical approval for the study was obtained from the Research Ethics Committee at the College of Nursing, University of Thi Qar.
Statistical analysis
Data were analyzed using SPSS 28. Pearson correlation coefficients were used to explore the relationships among parameters. The mediating effect of family involvement was tested using the PROCESS macro (Model-4) for SPSS, with 5,000 bootstrap samples to estimate indirect effects and 95% confidence intervals. A p-value of less than 0.05 was considered statistically significant in all analyses.
Findings
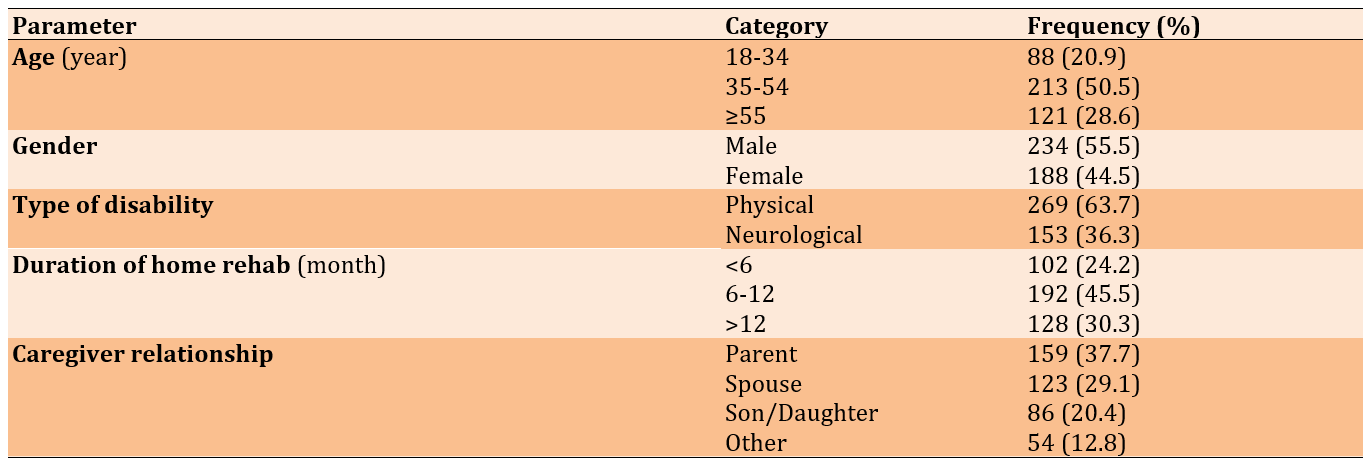
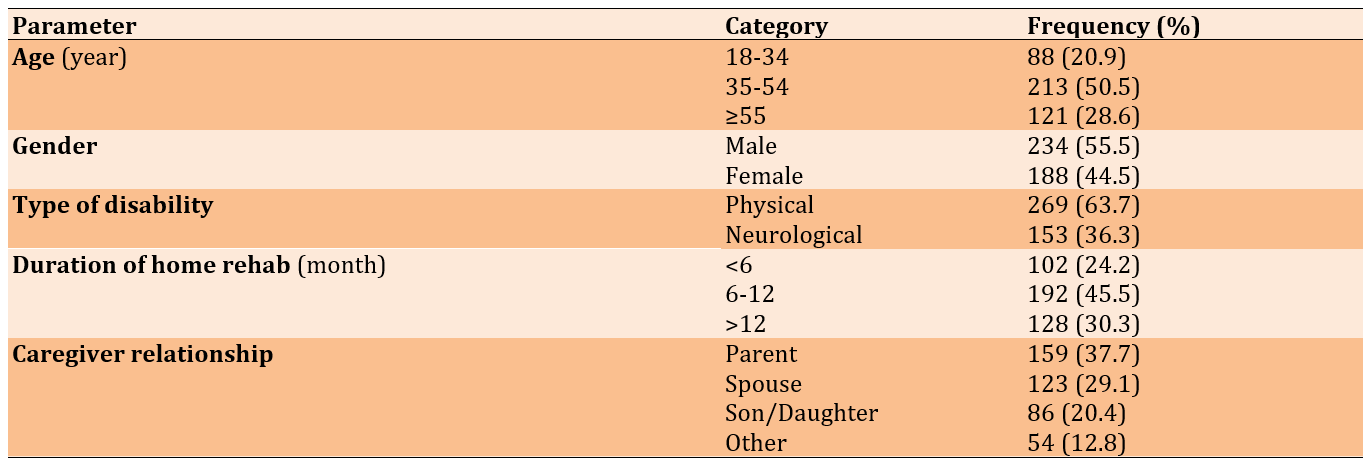
The average age of participants was 47.3±14.6 years, with the majority falling within the 35-54 age range (50.5%). More than half of the sample was male (55.5%). The majority (63.7%) had physical disabilities, while 36.3% had neurological conditions. Participants had received HBR for a median of 8.3 months, with nearly half (45.5%) enrolled in rehabilitation for 6-12 months. Regarding caregiver relationships, 37.7% of caregivers were parents, followed by spouses (29.1%) and sons/daughters (20.4%). The mean duration of home rehabilitation was 8.3±2.9 months (Table 1).
Table 1. Sample characteristics of participants
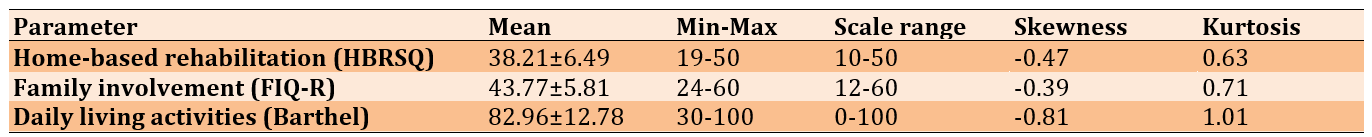
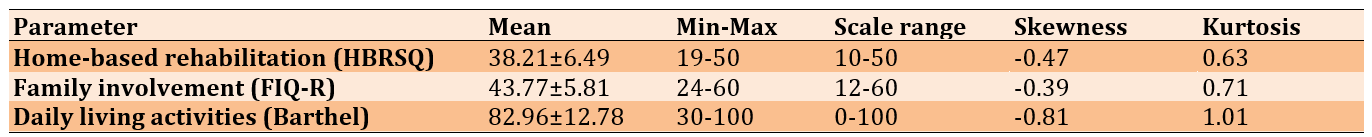
HBR scores with an average of 38.21±6.49, indicated robust engagement in home services. Family involvement scores (FIQ-R) averaged 44.77±5.81, reflecting mild to high family participation. ADLs with a high score of 82.96±12.78, demonstrated excellent functional independence among participants. Skewness and kurtosis values were within acceptable levels (±2), indicating a normal distribution (Table 2).
Table 2. Descriptive statistics and reliability of main variables
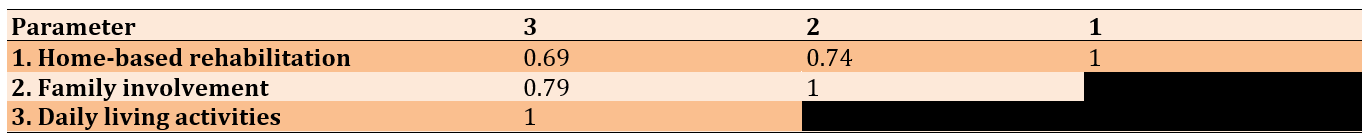
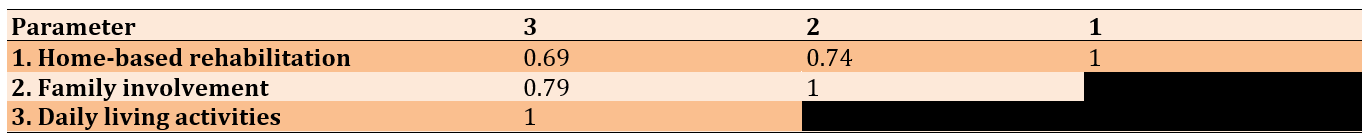
HBR was strongly and positively correlated with family involvement (r=0.74, p<0.001) and ADLs (r=0.69, p<0.001). Family Involvement also exhibited a strong positive correlation with ADLs (r=0.79, p<0.001; Table 3).
Table 3. Correlation matrix among main variables
The relationship between HBR and family involvement was strong and significant (B=0.94, β=0.74, p<0.001). Similarly, family involvement significantly predicted ADLs (B=1.12, β=0.79, p<0.001). The overall effect of HBR on was substantial (B=1.57, β=0.73, p<0.001), and the direct impact remained significant, though smaller (B=0.52, β=0.42, p<0.001; Table 4).
Table 4. Mediation analysis (PROCESS Model 4)
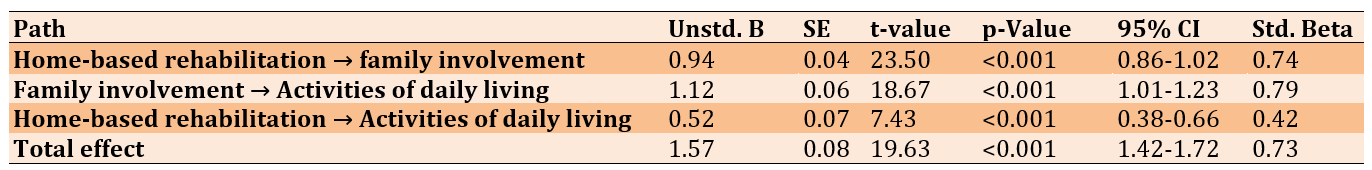
The indirect effect through the home-based rehabilitation → family involvement → activities of daily living pathway was estimated at 1.05 (Boot SE=0.07; 95% CI=0.91-1.19; p-value<0.001). Since the CI does not include zero, this mediation effect was statistically significant.
The overall regression model predicting ADLs yielded an R² of 0.66, indicating that 66% of the variance in ADL performance was explained by HBR and family involvement. The model was statistically significant (F=408.15, df=2, 419; p-value<0.001; R=0.81). The high R² value reflects an excellent model fit, suggesting that these predictors were strong determinants of daily functional outcomes in this population.
Discussion
The present study examined the mediating role of family involvement in the relationship between HBR services and ADLs among individuals with disabilities. There was a significant and positive association among all three parameters, with family involvement emerging as a strong mediator that enhances the effect of rehabilitation services on functional independence. These findings align with a growing body of literature emphasizing the importance of family-centered care in rehabilitation outcomes.
The sample characteristics revealed a diverse group of participants, predominantly middle-aged adults, with a moderate majority being male and primarily experiencing physical disabilities. This demographic profile is consistent with the population typically served by community-based rehabilitation (CBR) programs in low- and middle-income countries. Similar distributions have been observed in research conducted by Makofane et al. in South Africa and Roberto & Savla in the United States, both highlighting the centrality of family caregiving and community services for adults with mobility or neurological impairments [22, 23].
In terms of descriptive statistics, the participants scored distinctly high in ADLs, suggesting that HBR and familial support make a significant contribution to functional potential. This supports a study, reporting that individuals receiving HBR in combination with caregiver training demonstrate marked improvements in Barthel Index scores. Additionally, the high reliability of the tools used in this study indicates robust psychometric consistency, aligning with findings from previous validation studies of the Barthel Index and similar rehabilitation measures [24-26].
The strong correlations found among HBR, family involvement, and ADLs further reinforce the idea that social and environmental supports are crucial in disability recovery. A recent study emphasizes the role of informal caregivers as essential mediators of health outcomes, particularly when formal healthcare resources are limited [27]. Moreover, it is highlighted that increased family involvement leads to better adherence to rehabilitation regimens, improved mental health outcomes, and enhanced physical functioning, consistent with our findings [28].
The mediation analysis, using the PROCESS macro, confirmed that family involvement partially mediated the effect of HBR on ADLs. The indirect effect was statistically significant, and the overall model accounted for 66% of the variance in functional outcomes. These results are consistent with previous studies that have reported that caregiver participation enhances the efficacy of stroke rehabilitation interventions [29, 30]. Similarly, it was found that involving family members in the rehabilitation planning for older adults with disabilities significantly increased patients’ autonomy and reduced their dependency ratings over time [31].
The strength of the mediation model indicates that rehabilitation interventions are more effective when families are actively engaged, not only in physical care but also in emotional support and decision-making. This aligns with the concepts of the World Health Organization’s Community-Based Rehabilitation Matrix, which emphasizes the significance of family and community participation in achieving inclusive development and functional recovery. Furthermore, the standardized coefficients from this study suggest that family involvement is not a peripheral detail but a key mechanism in maximizing rehabilitation outcomes.
This study has several limitations. First, its cross-sectional design limits the ability to establish causality among HBR, family involvement, and ADLs. Second, data were collected through self-reported measures, which may be subject to recall bias or social desirability bias. Third, the study was conducted in a single Iraqi governorate, which may restrict the generalizability of the findings to other areas or countries with different healthcare systems and cultural norms. Lastly, unmeasured variables, such as mental health status or socioeconomic factors, may influence rehabilitation outcomes and have not been controlled for in this analysis.
Strong family support enhanced the effectiveness of rehabilitation programs, leading to improved meaningful independence. Based on these findings, it is recommended that healthcare providers and policymakers incorporate family-centered approaches into rehabilitation programs. Priority should be given to training and supporting family caregivers to ensure sustainable and effective home care. Future research using longitudinal models is also recommended to explore causal relationships and evaluate long-term outcomes.
Conclusion
Family involvement significantly mediates the relationship between home rehabilitation and ADLs for individuals with disabilities.
Acknowledgments: The authors would like to thank all the participants who permitted them to interview them for their cooperation and participation.
Ethical Permissions: The ethical approval was obtained from the Research Ethics Committee of the University of Thi-Qar (date: 06/03/2024, number: 711/3).
Conflicts of Interests: The authors declared no conflicts of interests.
Authors' Contribution: Balat KZ (First Author), Introduction Writer/Main Researcher/Methodologist (50%); Elywy GJ (Second Author), Assistant Researcher/Discussion Writer/Statistical Analyst (50%)
Funding/Support: The present study was not financially supported.
Rehabilitation is a cornerstone in restoring purposeful abilities and promoting independence among individuals with disabilities [1]. Among numerous modalities, home-based rehabilitation (HBR) has emerged as a preferred method for long-term care, particularly in community health settings [2]. HBR is an effective approach designed to enhance the involvement of patients and their families in recognizing their needs and delivering essential education [3]. By actively engaging patients in their own care, HBR empowers them to take charge of their health journey, leading to improved adherence to treatment plans. Additionally, this method fosters open communication between healthcare providers and families, ensuring that everyone is aligned in their goals and understanding of the rehabilitation process, which ultimately contributes to better health outcomes. Moreover, the personalized nature of HBR allows for tailored interventions that address specific challenges faced by patients and their families, making the rehabilitation experience more relevant and impactful. The goal of HBR is to preserve and restore patients’ health and independence while minimizing disabilities associated with chronic illnesses [4]. These services are particularly beneficial for addressing the health needs of individuals requiring rehabilitation, offering significant value due to their affordability, practicality, ability to ensure client comfort, reduction of frequent hospital visits, and the facilitation of connections between healthcare facilities and the community.
It offers the benefits of delivering therapy in a familiar environment, facilitating continuity of care, and reducing institutionalization costs [2]. Studies have shown that individuals receiving HBR demonstrate higher adherence to therapy and report greater pride compared to those undergoing facility-based rehabilitation [5, 6]. Jafari et al. showed that HBR not only enhances stroke patients’ adherence to treatment regimens in three key areas—rehabilitation, diet, and medication—but also improves their quality of life (QoL). Consequently, the authors strongly advocate for the implementation of this approach by nursing staff to more effectively engage patients with chronic conditions and their families in the ongoing care process [7].
Family members play a crucial role in providing emotional support and encouragement, which can significantly enhance a patient’s motivation to engage in rehabilitation activities. The success of HBR is not solely dependent on professional offerings; it is heavily influenced by the involvement and support of family members [8, 9]. Additionally, active participation of family in the care process helps ensure that patients adhere to treatment plans and make necessary lifestyle changes, thereby reinforcing the skills and knowledge acquired during rehabilitation. Furthermore, when families are involved, they can facilitate better communication with healthcare providers, leading to more comprehensive care that addresses the holistic needs of the patient.
Family involvement plays an important mediating role in the rehabilitation outcomes of individuals with disabilities. The presence of an engaged and supportive circle of relatives can significantly improve motivation, adherence to rehabilitation plans, and overall psychosocial well-being [10]. Research has documented that family members frequently assist with therapy, monitor progress, and provide emotional encouragement, all of which contribute to improved functional outcomes [11]. In contexts where formal rehabilitation services are limited, family involvement becomes even more vital in assisting with activities of daily living (ADLs), such as dressing, mobility, and hygiene [12, 13]. Family members often take on essential caregiving roles, providing hands-on support that can greatly enhance the quality of care and daily functioning for individuals recovering from injury or illness. Furthermore, their presence not only helps address immediate physical needs but also fosters emotional well-being, as the support of loved ones can alleviate feelings of isolation and promote a sense of stability during the recovery process.
ADLs are essential indicators of a person’s potential to function independently. The goal of successful rehabilitation programs is not only to reduce impairment but also to restore the ability to carry out vital daily responsibilities [14]. The literature indicates that higher levels of family engagement are associated with greater improvements in ADLs, particularly in populations with chronic physical or neurological disabilities [15, 16]. Despite the recognized significance of family involvement, few studies have explicitly tested its mediating role in the relationship between HBR and ADL performance. Bogner et al. assessed how family attendance at inpatient rehabilitation therapy sessions impacts the outcomes of patients with traumatic brain injury (TBI) at discharge and up to nine months afterward. They reported that family involvement in rehabilitation leads to improved outcomes; specifically, participants whose families attend therapy sessions at least 10% of the time demonstrate greater community engagement post-discharge. Additionally, family participation during inpatient rehabilitation may enhance cognitive function and community involvement for up to nine months after discharge [17]. Foster et al. concluded that having the support and involvement of one’s family during rehabilitation after a serious traumatic brain injury can significantly enhance the likelihood of achieving positive outcomes. Rehabilitation services can and should offer families the necessary support to facilitate their engagement in the rehabilitation process. This paper describes the innovative strategies that one rehabilitation service provider has implemented to effectively involve families in the rehabilitation journey, ultimately aiming to improve patient outcomes [18]. Given this gap, the current study aimed to explore the mediating impact of family involvement in the relationship between HBR and ADLs among individuals with disabilities. Understanding this dynamic can inform nursing interventions, policy development, and the design of community rehabilitation programs that emphasize family integration as a central aspect of care. The importance of this study lies in its potential to shift the focus of rehabilitation from a purely clinical approach to one that recognizes the critical role of family support in achieving successful outcomes. By demonstrating how family involvement influences rehabilitation effectiveness, the findings can encourage healthcare providers to adopt more inclusive practices that actively engage family members in the care process. Additionally, this research can serve as a foundation for developing targeted training programs for family caregivers, equipping them with the necessary skills to support their loved ones effectively. Ultimately, the insights gained from this study can contribute to more comprehensive and person-centered rehabilitation strategies, leading to enhanced quality of life for individuals with disabilities.
Materials and Methods
Study design and sample
This descriptive correlational cross-sectional study was conducted between March and June 2025 at selected community-based primary health care centers and rehabilitation facilities in Thi Qar Governorate, Iraq. The sample consisted of adults with physical or neurological disabilities who had been receiving HBR for at least three months.
The cross-sectional approach was chosen due to its suitability for assessing associations among psychosocial and functional prameters at a single point in time, which aligns with the objectives of behavioral research in community health nursing. These locations were chosen based on provider availability, accessibility, and their establishment of HBR programs.
Participants were selected using a systematic random sampling approach, guided by the rehabilitation service data. The sample size was calculated using the single population percentage formula with a 95% confidence level and a 5% margin of error, based on an initial estimate of 384 individuals. To account for potential non-response, the final sample size was adjusted to 422. Inclusion criteria included adults aged 18 years or older, currently receiving HBR, living with their family caregiver, and able to understand Arabic. Individuals with severe psychiatric disorders or those in institutionalized care were excluded.
Research tools
Data collection was conducted using an established interviewer-administered questionnaire comprising four sections. The first section covered demographic and medical factors, such as age, gender, type of disability, and duration of HBR. The second section assessed HBR using the Home-Based Rehabilitation Services Questionnaire (HBRSQ), which was developed in accordance with WHO CBR recommendations and consists of 10 items rated on a five-point Likert scale [19]. The third section evaluated family involvement through the Family Involvement Questionnaire-Rehabilitation Version (FIQ-R), which includes 12 items measuring emotional, physical, and decision-making support provided by family members [20]. The fourth section assessed ADLs using the Barthel Index, a widely used tool that evaluates basic functional tasks, such as mobility, feeding, and personal hygiene [21].
To ensure the quality and cultural appropriateness of the study tools, the questionnaire underwent content validation by a panel of five experts in rehabilitation nursing, public health, and social sciences. Based on their feedback, several items were revised for clarity. A pilot study was conducted with forty-two individuals with disabilities to evaluate the internal consistency, flow, and clarity of the instrument. The pilot responses were excluded from the final data analysis. The reliability coefficients (Cronbach’s alpha) for the primary observation tools were 0.87 for the HBRSQ, 0.88 for the FIQ-R, and 0.90 for the Barthel Index, all indicating strong internal consistency.
Data collection
Data collection was conducted with the assistance of skilled community health nurses through private, face-to-face interviews at primary healthcare centers or participants’ homes, depending on the individual’s mobility status. Each interview session lasted approximately 30 to 40 minutes. All participants provided written informed consent before participation. Confidentiality and the right to withdraw at any stage were explained. Ethical approval for the study was obtained from the Research Ethics Committee at the College of Nursing, University of Thi Qar.
Statistical analysis
Data were analyzed using SPSS 28. Pearson correlation coefficients were used to explore the relationships among parameters. The mediating effect of family involvement was tested using the PROCESS macro (Model-4) for SPSS, with 5,000 bootstrap samples to estimate indirect effects and 95% confidence intervals. A p-value of less than 0.05 was considered statistically significant in all analyses.
Findings
The average age of participants was 47.3±14.6 years, with the majority falling within the 35-54 age range (50.5%). More than half of the sample was male (55.5%). The majority (63.7%) had physical disabilities, while 36.3% had neurological conditions. Participants had received HBR for a median of 8.3 months, with nearly half (45.5%) enrolled in rehabilitation for 6-12 months. Regarding caregiver relationships, 37.7% of caregivers were parents, followed by spouses (29.1%) and sons/daughters (20.4%). The mean duration of home rehabilitation was 8.3±2.9 months (Table 1).
Table 1. Sample characteristics of participants
HBR scores with an average of 38.21±6.49, indicated robust engagement in home services. Family involvement scores (FIQ-R) averaged 44.77±5.81, reflecting mild to high family participation. ADLs with a high score of 82.96±12.78, demonstrated excellent functional independence among participants. Skewness and kurtosis values were within acceptable levels (±2), indicating a normal distribution (Table 2).
Table 2. Descriptive statistics and reliability of main variables
HBR was strongly and positively correlated with family involvement (r=0.74, p<0.001) and ADLs (r=0.69, p<0.001). Family Involvement also exhibited a strong positive correlation with ADLs (r=0.79, p<0.001; Table 3).
Table 3. Correlation matrix among main variables
The relationship between HBR and family involvement was strong and significant (B=0.94, β=0.74, p<0.001). Similarly, family involvement significantly predicted ADLs (B=1.12, β=0.79, p<0.001). The overall effect of HBR on was substantial (B=1.57, β=0.73, p<0.001), and the direct impact remained significant, though smaller (B=0.52, β=0.42, p<0.001; Table 4).
Table 4. Mediation analysis (PROCESS Model 4)
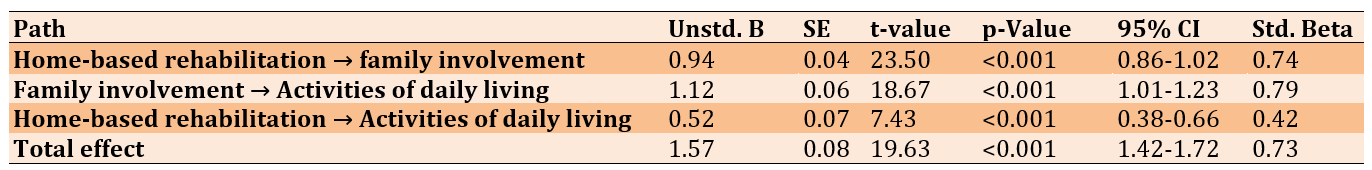
The indirect effect through the home-based rehabilitation → family involvement → activities of daily living pathway was estimated at 1.05 (Boot SE=0.07; 95% CI=0.91-1.19; p-value<0.001). Since the CI does not include zero, this mediation effect was statistically significant.
The overall regression model predicting ADLs yielded an R² of 0.66, indicating that 66% of the variance in ADL performance was explained by HBR and family involvement. The model was statistically significant (F=408.15, df=2, 419; p-value<0.001; R=0.81). The high R² value reflects an excellent model fit, suggesting that these predictors were strong determinants of daily functional outcomes in this population.
Discussion
The present study examined the mediating role of family involvement in the relationship between HBR services and ADLs among individuals with disabilities. There was a significant and positive association among all three parameters, with family involvement emerging as a strong mediator that enhances the effect of rehabilitation services on functional independence. These findings align with a growing body of literature emphasizing the importance of family-centered care in rehabilitation outcomes.
The sample characteristics revealed a diverse group of participants, predominantly middle-aged adults, with a moderate majority being male and primarily experiencing physical disabilities. This demographic profile is consistent with the population typically served by community-based rehabilitation (CBR) programs in low- and middle-income countries. Similar distributions have been observed in research conducted by Makofane et al. in South Africa and Roberto & Savla in the United States, both highlighting the centrality of family caregiving and community services for adults with mobility or neurological impairments [22, 23].
In terms of descriptive statistics, the participants scored distinctly high in ADLs, suggesting that HBR and familial support make a significant contribution to functional potential. This supports a study, reporting that individuals receiving HBR in combination with caregiver training demonstrate marked improvements in Barthel Index scores. Additionally, the high reliability of the tools used in this study indicates robust psychometric consistency, aligning with findings from previous validation studies of the Barthel Index and similar rehabilitation measures [24-26].
The strong correlations found among HBR, family involvement, and ADLs further reinforce the idea that social and environmental supports are crucial in disability recovery. A recent study emphasizes the role of informal caregivers as essential mediators of health outcomes, particularly when formal healthcare resources are limited [27]. Moreover, it is highlighted that increased family involvement leads to better adherence to rehabilitation regimens, improved mental health outcomes, and enhanced physical functioning, consistent with our findings [28].
The mediation analysis, using the PROCESS macro, confirmed that family involvement partially mediated the effect of HBR on ADLs. The indirect effect was statistically significant, and the overall model accounted for 66% of the variance in functional outcomes. These results are consistent with previous studies that have reported that caregiver participation enhances the efficacy of stroke rehabilitation interventions [29, 30]. Similarly, it was found that involving family members in the rehabilitation planning for older adults with disabilities significantly increased patients’ autonomy and reduced their dependency ratings over time [31].
The strength of the mediation model indicates that rehabilitation interventions are more effective when families are actively engaged, not only in physical care but also in emotional support and decision-making. This aligns with the concepts of the World Health Organization’s Community-Based Rehabilitation Matrix, which emphasizes the significance of family and community participation in achieving inclusive development and functional recovery. Furthermore, the standardized coefficients from this study suggest that family involvement is not a peripheral detail but a key mechanism in maximizing rehabilitation outcomes.
This study has several limitations. First, its cross-sectional design limits the ability to establish causality among HBR, family involvement, and ADLs. Second, data were collected through self-reported measures, which may be subject to recall bias or social desirability bias. Third, the study was conducted in a single Iraqi governorate, which may restrict the generalizability of the findings to other areas or countries with different healthcare systems and cultural norms. Lastly, unmeasured variables, such as mental health status or socioeconomic factors, may influence rehabilitation outcomes and have not been controlled for in this analysis.
Strong family support enhanced the effectiveness of rehabilitation programs, leading to improved meaningful independence. Based on these findings, it is recommended that healthcare providers and policymakers incorporate family-centered approaches into rehabilitation programs. Priority should be given to training and supporting family caregivers to ensure sustainable and effective home care. Future research using longitudinal models is also recommended to explore causal relationships and evaluate long-term outcomes.
Conclusion
Family involvement significantly mediates the relationship between home rehabilitation and ADLs for individuals with disabilities.
Acknowledgments: The authors would like to thank all the participants who permitted them to interview them for their cooperation and participation.
Ethical Permissions: The ethical approval was obtained from the Research Ethics Committee of the University of Thi-Qar (date: 06/03/2024, number: 711/3).
Conflicts of Interests: The authors declared no conflicts of interests.
Authors' Contribution: Balat KZ (First Author), Introduction Writer/Main Researcher/Methodologist (50%); Elywy GJ (Second Author), Assistant Researcher/Discussion Writer/Statistical Analyst (50%)
Funding/Support: The present study was not financially supported.
Keywords:
References
1. Radhi MM, Al-Eqabi QA, Hindi NK. Rehabilitation problems of people with motor disabilities at Babylon center for rehabilitation of the disabled. Med J Babylon. 2023;20(4):838-43. [Link] [DOI:10.4103/MJBL.MJBL_674_23]
2. Denham AC, Kistler CE. Home- and community-based care. In: Chronic illness care: Principles and practice. Cham: Springer International Publishing; 2023. p. 269-83. [Link] [DOI:10.1007/978-3-031-29171-5_20]
3. Sanaie N, Nejati S, Zolfaghari M, Alhani F, Kazemnezhad A. The effects of family-based empowerment on family cooperation in following patient treatment regime after coroner arteries bypass surgery. Modern Care J. 11(1): 19-27. [Link]
4. Dehghan Nayeri N, Mohammadi S, Pedram Razi S, Arazi TM, Kazemnejad A. Effectiveness of family empowerment program on level of adherence to treatment regimens in stroke patients; a randomized controlled trial. Evid Based Care. 2015;5(1):57-66. [Link]
5. Gilson A, Gassman M, Dodds D, Lombardo R, Ford JH, Potteiger M. Refining a digital therapeutic platform for home care agencies in dementia care to elicit stakeholder feedback: Focus group study with stakeholders. JMIR Aging. 2022;5(1):e32516. [Link] [DOI:10.2196/32516]
6. Radhi MM, Elywy GJ, Al-Eqabi QAK. Burdens among wives of disabled people in the light of some social variables. Iran Rehabil J. 2023;21(3):473-84. [Link] [DOI:10.32598/irj.21.3.1765.3]
7. Jafari J, Kermansaravi F, Yaghoubinia F. The effect of home-based rehabilitation on adherence to treatment and quality of life of individuals after stroke. Med Surg Nurs J. 2020;9(2): e107716. [Link] [DOI:10.5812/msnj.107716]
8. Radhi MM, Niazy SM, Abed SN. Individual-related factors associated with treatment adherence among hypertensive patients. J Public Health Afr. 2023;14(6):2466. [Link] [DOI:10.4081/jphia.2023.2466]
9. Elywy GJ, Radhi MM, AlEqabi QA. Relationship between social support and self-hardiness among breast cancer women in Nasiriyah, Iraq. J Pak Med Assoc. 2023;73(9):S9-14. [Link] [DOI:10.47391/JPMA.IQ-02]
10. Aliedan MM, Elshaer IA, Zayed MA, Elrayah M, Moustafa MA. Evaluating the role of university disability service support, family support, and friends' support in predicting the quality of life among disabled students in higher education: Physical self-esteem as a mediator. J Disabil Res. 2023;2(3):48-59. [Link] [DOI:10.57197/JDR-2023-0035]
11. Handayani AA. Family involvement in mental health recovery: Systemic barriers and supportive strategies for enhancing treatment adherence and outcomes. JURNAL RISET KUALITATIF DAN PROMOSI KESEHATAN. 2022;1(2):57-71. [Link] [DOI:10.61194/jrkpk.v1i2.656]
12. Zawaly K, Ripat J, Guse L, Katz A, Edwards J, Sibley KM. Re-braiding the strands of life through community rehabilitation, home care, and informal support: A longitudinal collective case study. Can J Aging. 2023;42(1):80-91. [Link] [DOI:10.1017/S0714980822000137]
13. Elywy GJ, Radhi MM, Al-Eqabi QAK. Social support and its association with the quality of life (QoL) of amputees. Iran Rehabil J. 2022;20(2):253-60. [Link] [DOI:10.32598/irj.20.2.1784.1]
14. Cipriani G, Danti S, Picchi L, Nuti A, Fiorino MD. Daily functioning and dementia. Dement Neuropsychol. 2020;14(2):93-102. [Link] [DOI:10.1590/1980-57642020dn14-020001]
15. Balat KZ, Laftah SA, Radhi M. The relationship between psychological distress and quality of life among women undergoing mastectomy in Iraq: A descriptive correlational study. Natl J Community Med. 2025;16(1):20-7. [Link] [DOI:10.55489/njcm.160120254716]
16. Al-Eqabi QA, Niazy SM, Radhi MM. Amputation-related factors influencing activities of daily living among amputees. Iran J War Public Health. 2024;16(2):123-9. [Link]
17. Bogner J, Hade EM, Peng J, Beaulieu CL, Horn SD, Corrigan JD, Hammond FM, Dijkers MP, Montgomery E, Gilchrist K, Giuffrida C. Family involvement in traumatic brain injury inpatient rehabilitation: A propensity score analysis of effects on outcomes during the first year after discharge. Archives of physical medicine and rehabilitation. 2019;100(10):1801-9. [Link] [DOI:10.1016/j.apmr.2019.04.008]
18. Foster AM, Armstrong J, Buckley A, Sherry J, Young T, Foliaki S, James-Hohaia TM, Theadom A, McPherson KM. Encouraging family engagement in the rehabilitation process: a rehabilitation provider's development of support strategies for family members of people with traumatic brain injury. Disability and rehabilitation. 2012;34(22):1855-62. [Link] [DOI:10.3109/09638288.2012.670028]
19. Lee IF, Yau FN, Yim SS, Lee DT. Evaluating the impact of a home-based rehabilitation service on older people and their caregivers: A matched-control quasi-experimental study. Clin Interv Aging. 2018;13:1727-37. [Link] [DOI:10.2147/CIA.S172871]
20. Fantuzzo J, Tighe E, Childs S. Family involvement questionnaire: A multivariate assessment of family participation in early childhood education. J Educ Psychol. 2000;92(2):367-76. [Link] [DOI:10.1037/0022-0663.92.2.367]
21. Collin C, Wade DT, Davies S, Horne V. The Barthel ADL Index: A reliability study. Int Disabil Stud. 1988;10(2):61-3. [Link] [DOI:10.3109/09638288809164103]
22. Makofane K, Berkman LF, Bassett MT, Tchetgen EJ. The effect of family wealth on physical function among older adults in Mpumalanga, South Africa: A causal network analysis. Int J Public Health. 2023;68:1606072. [Link] [DOI:10.3389/ijph.2023.1606072]
23. Roberto KA, Savla J. Extended family caregivers for persons living with dementia. J Fam Nurs. 2022;28(4):396-407. [Link] [DOI:10.1177/10748407221115455]
24. Kaambwa B, Bulamu NB, Mpundu-Kaambwa C, Oppong R. Convergent and discriminant validity of the Barthel Index and the EQ-5D-3L when used on older people in a rehabilitation setting. Int J Environ Res Public Health. 2021;18(19):10314. [Link] [DOI:10.3390/ijerph181910314]
25. Alwatify SS, Radhi MM. Diabetes self-management and its association with medication adherence in diabetic patients. Iran J War Public Health. 2025;17(1):17-22. [Link] [DOI:10.58209/ijwph.17.1.17]
26. Abed Laftah S, Kadhim Abdul-Hameed A, Balat KZ, Radhi MM. Barriers and facilitators in rehabilitative nursing care for clients with disabilities: A mediating roles of nurse-related factors. Iran Rehabil J. 2025;23(2):165-74. [Link] [DOI:10.32598/irj.23.2.1989.4]
27. Vrettos I, Anagnostopoulos F, Voukelatou P, Panayiotou S, Kyvetos A, Nikas A, et al. Factors associated with health‐related quality of life of informal caregivers of older patients and the mediating role of subjective caregivers' burden. Psychogeriatrics. 2023;23(2):286-97. [Link] [DOI:10.1111/psyg.12930]
28. Religioni U, Barrios-Rodríguez R, Requena P, Borowska M, Ostrowski J. Enhancing therapy adherence: Impact on clinical outcomes, healthcare costs, and patient quality of life. Medicina. 2025;61(1):153. [Link] [DOI:10.3390/medicina61010153]
29. Radhi MM, Abd RK, Al Eqabi QA. The body image and its relation to self-esteem among amputation patients at artificial limbs hospital at Kut City, Iraq. J Public Health Afr. 2022;13(4):9. [Link] [DOI:10.4081/jphia.2022.1228]
30. Radhi MM. Degree of disease acceptance and health seeking behaviors for type 2 diabetic patients at diabetic center in Hilla City. Medico Leg Update. 2020;20(2):853-8. [Link] [DOI:10.37506/mlu.v20i2.1347]
31. Barria P, Andrade A, Yelincic A, Córdova B, Covarrubias-Escudero F, Cifuentes C, et al. Impact of a long-term home-based rehabilitation program on quality of life, balance, and autonomy in adults with disabilities. J Funct Morphol Kinesiol. 2025;10(1):24. [Link] [DOI:10.3390/jfmk10010024]









