Volume 17, Issue 1 (2025)
Iran J War Public Health 2025, 17(1): 83-87 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2025/03/6 | Accepted: 2025/04/9 | Published: 2025/04/12
Received: 2025/03/6 | Accepted: 2025/04/9 | Published: 2025/04/12
How to cite this article
Niazy S, Al-Eqabi Q, Radhi M, AL-Thabhawee G. Nutritional Status in Community-Dwelling Older Adults and Geriatric Home. Iran J War Public Health 2025; 17 (1) :83-87
URL: http://ijwph.ir/article-1-1569-en.html
URL: http://ijwph.ir/article-1-1569-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
1- Department of Community, Medical-Technical Institute, Middle Technical University, Baghdad, Iraq
2- Department of Community Health Techniques, College of Health & Medical Techniques-Kufa, Al-Furat Al-Awsat Technical University, Najaf, Iraq
2- Department of Community Health Techniques, College of Health & Medical Techniques-Kufa, Al-Furat Al-Awsat Technical University, Najaf, Iraq
Full-Text (HTML) (259 Views)
Introduction
Nutritional status is a crucial determinant of health and well-being in public health, particularly among older adults, who are at increased risk of malnutrition due to physiological, psychological, and social factors [1, 2]. Malnutrition in older adults is associated with several adverse outcomes, including increased morbidity, mortality, and healthcare costs [3]. As the global population ages, understanding the nutritional status of older adults in different living environments, such as community-living settings and geriatric homes, is essential for developing targeted interventions to enhance health outcomes [4, 5].
Community-living older adults frequently face challenges, such as limited access to nutritious food, social isolation, and age-related changes in appetite and metabolism [6]. In contrast, older adults living in geriatric homes may have access to structured meal plans and professional care; however, they may also experience geriatric eating patterns and reduced autonomy, which can affect their nutritional status [7, 8]. Comparative research between these populations is critical to uncover disparities and inform policies that promote healthy aging [9].
Malnutrition among older adults varies widely depending on the living environment. Studies have shown that community-dwelling older adults are much less likely to be malnourished compared to those in geriatric homes, where the prevalence of malnutrition may be as high as 50% [10, 11]. However, even among community-dwelling older adults, the risk of malnutrition remains significant, particularly among individuals with chronic diseases, functional limitations, or low socioeconomic status [12]. These findings underscore the need for comprehensive assessments of nutritional status in both settings.
Nutritional assessments generally include anthropometric measurements, biochemical markers, nutritional intake evaluations, and screening tools, such as the mini nutritional assessment (MNA) [13]. These tools help identify individuals at risk of malnutrition and guide interventions tailored to their specific needs. For community-living older adults, interventions may focus on improving access to nutritious food, enhancing social support, and providing education on healthy eating [14]. In geriatric homes, interventions might include modifying meal plans, addressing swallowing difficulties, and promoting a more personalized approach to nutritional care [15].
The comparative examination of nutritional status among community-living older adults and those in geriatric homes provides valuable insights into the unique challenges faced by each population. By identifying the factors that contribute to malnutrition in these settings, healthcare providers and policymakers can develop targeted strategies to improve nutritional outcomes and enhance the quality of life for older adults. This study aimed to contribute to the growing body of evidence in this field, with the ultimate goal of promoting healthy aging and reducing the burden of malnutrition among older adults worldwide.
Instrument and Methods
Study design and setting
This comparative cross-sectional study assessed the nutritional status of community-dwelling older adults and older adults residing in geriatric homes in Babil Governorate, Iraq over two months, from January 5th to March 10th, 2025. The comparative design was selected to identify potential differences in nutritional status between the two groups, providing insights into the effects of living arrangements on the health and well-being of older adults in the community. Babil Governorate was chosen because of its diverse population and the presence of both community-dwelling older adults and geriatric homes, which allowed for a comprehensive comparison of nutritional status between the two groups.
Inclusion/exclusion criteria
The sample consisted of 200 participants, divided into two groups (100 community-dwelling older adults and 100 older adults residing in geriatric homes). Participants were included if they were aged 60 years or older, were willing to participate, and were able to provide informed consent. Exclusion criteria included severe cognitive impairment, terminal illness, or refusal to participate. The sample size was determined to ensure adequate statistical power for detecting significant differences between the groups.
Study tools
Nutritional status was assessed using the MNA tool, a validated and widely used instrument for evaluating malnutrition and the risk of malnutrition among older adults. The MNA consists of questions related to nutritional intake, weight loss, mobility, psychological stress, and anthropometric measurements (e.g., body mass index). Additionally, demographic information such as age, gender, and marital status is collected.
Validity and reliability
The MNA tool has been extensively validated and demonstrates high reliability and validity for assessing nutritional status in older populations. Before data collection, the tool was reviewed by a panel of experts to ensure its cultural appropriateness and relevance to the study context. A pilot study involving 20 participants (ten from each group) was conducted to test the clarity and reliability of the tool, and minor adjustments were made based on feedback.
Data collection
Participants were recruited through purposive sampling. Community-dwelling older adults were identified via local community centers and public health clinics, while older adults in geriatric homes were recruited directly from facilities in Babil Governorate. Trained researchers administered the MNA tool through face-to-face interviews to ensure accurate data collection. Anthropometric measurements were taken using standardized procedures.
Statistical analysis
Data were analyzed using SPSS 25 software. Descriptive statistics, including mean, standard deviations, frequencies, and percentages, were used to summarize demographic and nutritional data. Independent t-tests and chi-square tests were employed to compare continuous and categorical variables, respectively, between the two groups. A p-value of <0.05 was considered statistically significant. Multivariate analysis, including logistic regression analysis, was conducted to identify factors associated with malnutrition or the risk of malnutrition, adjusting for potential confounders.
Findings
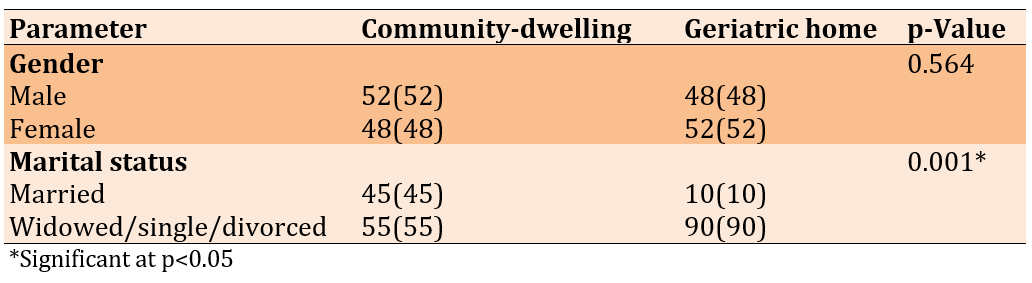
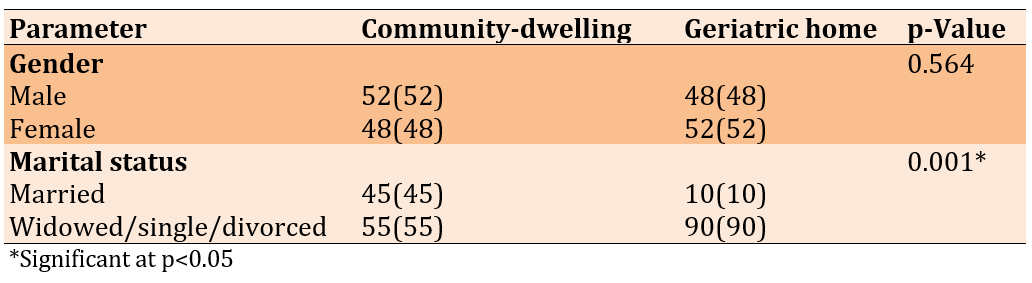
The mean age was significantly higher in the geriatric home group (74.8±7.1 years) compared to the community-dwelling group (72.5±6.4 years; p=0.032), indicating an older population in institutional settings. Gender distribution was nearly equal in both groups, with no significant difference (p=0.564). However, marital status showed a significant difference, as only 10% of geriatric home residents were married compared to 45% of community-dwelling individuals (p<0.001). Conversely, 90% of geriatric home residents were widowed, single, or divorced, which was significantly higher than the 55% in the community-dwelling group (p<0.001; Table 1).
Table 1. Frequency of demographic characteristics of participants
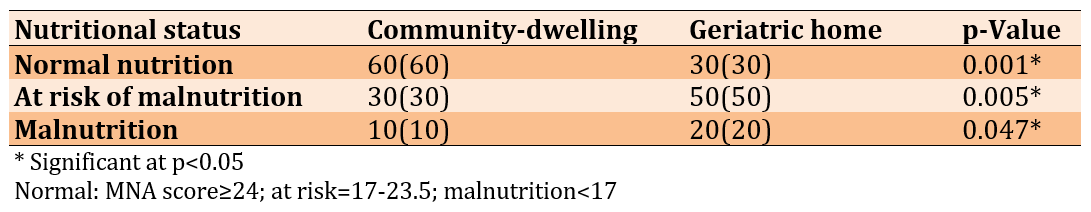
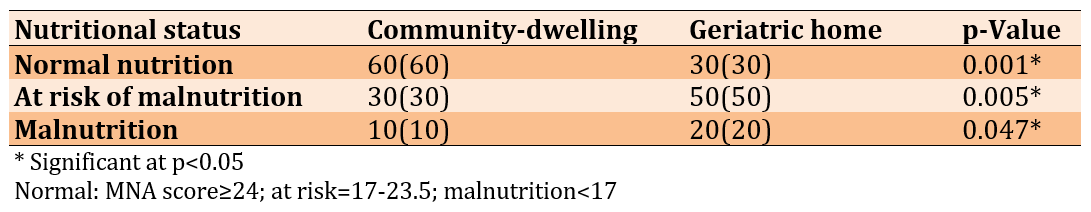
Malnutrition was significantly more prevalent among geriatric home residents. While 60% of community-dwelling individuals had normal nutritional status, only 30% of those in geriatric homes fell into this category (p<0.001). Conversely, the percentage of individuals at risk of malnutrition was higher among geriatric home residents (50%) compared to community-dwelling individuals (30%; p=0.005). Additionally, 20% of geriatric home residents were malnourished, which is double the rate found in the community-dwelling group (10%; p=0.047; Table 2).
Table 2. Nutritional status based on mini nutritional assessment (MNA)
The mean body mass index (BMI) was significantly lower in geriatric home residents (22.8±3.5kg/m2) than in community-dwelling individuals (24.6±3.1kg/m2; p=0.018), suggesting a poorer overall nutritional status. Weight loss in the past three months was significantly greater in geriatric home residents (12.2±3.4) compared to community dwellers (8.5±2.3; p<0.001), indicating greater nutritional deterioration in geriatric individuals. Furthermore, daily food consumption showed a significant decrease in geriatric home residents (2.4±0.6 meals/day) compared to the community-dwelling group (3.1±0.5 meals/day; p<0.001), emphasizing decreased nutritional intake as a potential factor for malnutrition. Additionally, mobility restrictions were significantly higher among geriatric home residents (50(50%)) compared to community-dwelling individuals (25(25%); p=0.002), suggesting that limited mobility may also contribute to poorer nutritional outcomes.
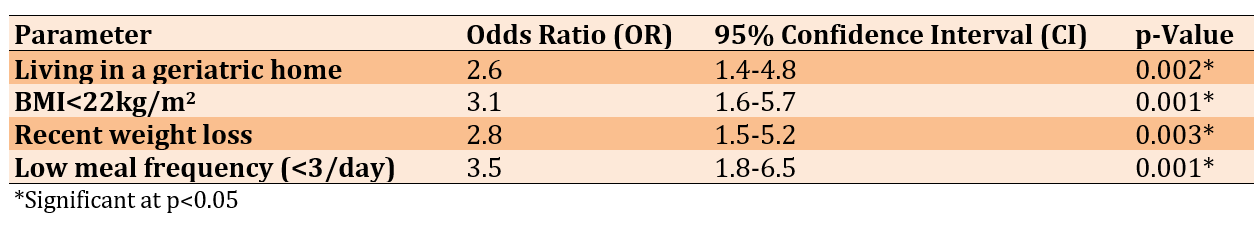
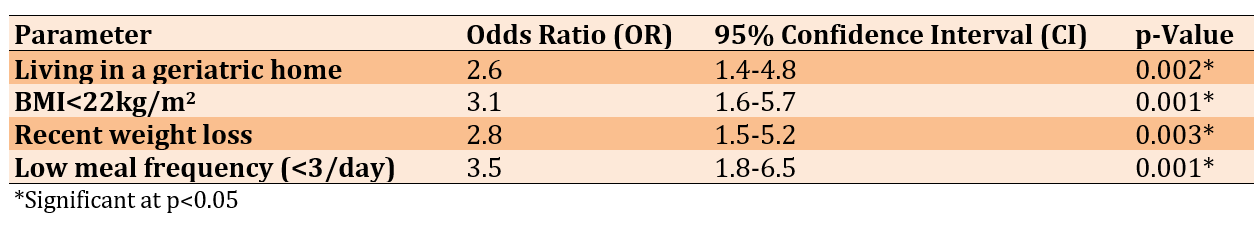
Living in a geriatric home was associated with a 2.6-fold increased risk of malnutrition (p=0.002). A BMI under 22 was a strong predictor, increasing the risk of malnutrition by 3.1 times (p=0.001). Recent weight loss was also a significant predictor, with individuals experiencing weight loss being 2.8 times more likely to be malnourished (p=0.003). Low meal frequency (<3 meals/day) was the strongest predictor, increasing the risk of malnutrition by 3.5 times (p<0.001; Table 3).
Table 3. Multivariate analysis-logistic regression for predictors of malnutrition
Discussion
This study aimed to compare the nutritional status of community-dwelling older adults with those residing in geriatric homes. The findings highlight significant differences in the nutritional status of older adults living in community settings compared to those in geriatric homes. The MNA scores indicated that malnutrition and the risk of malnutrition were notably higher among geriatric home residents. Only 30% of geriatric older adults had normal nutritional status compared to 60% of their community-dwelling counterparts. Furthermore, the percentage of individuals at risk of malnutrition was significantly greater among those in geriatric homes. Additionally, the prevalence of malnutrition in geriatric home residents was twice as high as in community-dwelling individuals. These findings align with previous studies indicating that geriatric older adults are at higher risk of malnutrition due to factors, such as decreased autonomy, dietary restrictions, and limited access to diverse food options [16, 17].
The comparative analysis of nutritional indicators further reinforced these findings. The mean BMI was significantly lower among geriatric home residents compared to community dwellers, indicating a higher prevalence of undernutrition among geriatric individuals. Weight loss over the past three months was significantly more pronounced in geriatric home residents compared to community-living individuals, a trend that can be attributed to inadequate nutritional intake, decreased physical activity, and potential health conditions affecting appetite and metabolism [2]. Moreover, daily meal consumption was substantially lower among geriatric home residents than among those residing in the community. This reduced meal frequency may be a crucial factor in the higher rates of malnutrition observed among geriatric individuals, as inadequate meal consumption has been linked to weight loss and deteriorating health in older adults [18, 19]. Furthermore, mobility restrictions were significantly more common among geriatric home residents (50%) than in community-living older adults, suggesting that physical barriers could contribute to decreased independence in meal choice and consumption, ultimately exacerbating nutritional deficiencies [20, 21].
The logistic regression analysis similarly identified key predictors of malnutrition in older adults. Living in a geriatric home was associated with a 2.6-fold increased risk of malnutrition, supporting previous evidence that geriatric settings may present additional challenges in maintaining adequate nutrition due to dependence on facility-provided food and potential neglect [22, 23]. A BMI below 22 emerged as a strong predictor, increasing the risk of malnutrition by 3.1 times, reinforcing the well-established relationship between low BMI and nutrition risk in older populations [24]. Recent weight loss also significantly predicted malnutrition, with individuals experiencing weight loss being 2.8 times more likely to be malnourished. This finding is consistent with studies showing that unintended weight loss is a major red flag for nutritional decline in geriatric populations [25, 26]. Notably, low meal frequency (<three meals/day) was the strongest predictor, increasing the risk of malnutrition by 3.5 times, emphasizing the critical role of regular and adequate food intake in preventing nutritional deterioration [27, 28].
Overall, these findings underscore the pressing need for targeted nutritional interventions in geriatric homes to mitigate malnutrition risks. Strategies that include individualized nutrition plans, increased meal frequency, and mobility-enhancing programs can be effective in improving the nutritional well-being of geriatric older adults. Future studies should explore interventions tailored to the unique needs of geriatric home residents, considering both nutritional and physical activity components to enhance overall health outcomes.
This study has several limitations that must be taken into consideration. First, the cross-sectional design prevents the establishment of causality between living arrangements and nutritional status. Second, potential selection bias may exist, as participants from community settings may differ in socioeconomic status and health conditions compared to those in geriatric homes. Third, self-reported nutritional intake and weight loss may introduce recall bias. Additionally, factors such as cognitive status, comorbidities, and social support, which can impact nutritional outcomes, were not significantly analyzed. Lastly, the study was conducted in a specific location, which may limit the generalizability of the findings to other populations.
The study highlights significant disparities in nutritional status among community-dwelling older adults and those residing in geriatric homes, with geriatric individuals facing a higher prevalence of malnutrition, decreased meal frequency, and greater weight loss. To address these challenges, targeted interventions are recommended, including personalized meal plans tailored to individual preferences and needs, regular nutrition screenings to identify at-risk individuals, and mobility support programs to enhance physical activity and appetite. Additionally, caregiver training and improved meal support practices in geriatric homes can help ensure adequate food consumption. Policymakers and healthcare providers must collaborate to implement these strategies, fostering a multidisciplinary approach to malnutrition prevention and improving the overall well-being of older adults, particularly those in institutional settings.
Conclusion
Geriatric home residents are at greater risk of malnutrition compared to community-dwelling older adults.
Acknowledgments: The authors would like to thank all the participants who allowed them to interview them for their cooperation and participation.
Ethical Permissions: Ethical approval was obtained from the Research Ethics Committee of the College of Health and Medical Techniques/Kufa, Al-Furat Al-Awsat Technical University (date: 27.09.2024, number: 294/1).
Conflicts of Interests: Nothing declared by the authors.
Authors' Contribution: Niazy SM (First Author), Introduction Writer/Main Researcher (25%); Al-Eqabi QAK (Second Author), Assistant Researcher/Discussion Writer (25%); Radhi MM (Third Author), Methodologist/Statistical Analyst (25%); AL-Thabhawee GDM (Fourth Author), Statistical Analyst (25%)
Funding/Support: The present study was not financially supported.
Nutritional status is a crucial determinant of health and well-being in public health, particularly among older adults, who are at increased risk of malnutrition due to physiological, psychological, and social factors [1, 2]. Malnutrition in older adults is associated with several adverse outcomes, including increased morbidity, mortality, and healthcare costs [3]. As the global population ages, understanding the nutritional status of older adults in different living environments, such as community-living settings and geriatric homes, is essential for developing targeted interventions to enhance health outcomes [4, 5].
Community-living older adults frequently face challenges, such as limited access to nutritious food, social isolation, and age-related changes in appetite and metabolism [6]. In contrast, older adults living in geriatric homes may have access to structured meal plans and professional care; however, they may also experience geriatric eating patterns and reduced autonomy, which can affect their nutritional status [7, 8]. Comparative research between these populations is critical to uncover disparities and inform policies that promote healthy aging [9].
Malnutrition among older adults varies widely depending on the living environment. Studies have shown that community-dwelling older adults are much less likely to be malnourished compared to those in geriatric homes, where the prevalence of malnutrition may be as high as 50% [10, 11]. However, even among community-dwelling older adults, the risk of malnutrition remains significant, particularly among individuals with chronic diseases, functional limitations, or low socioeconomic status [12]. These findings underscore the need for comprehensive assessments of nutritional status in both settings.
Nutritional assessments generally include anthropometric measurements, biochemical markers, nutritional intake evaluations, and screening tools, such as the mini nutritional assessment (MNA) [13]. These tools help identify individuals at risk of malnutrition and guide interventions tailored to their specific needs. For community-living older adults, interventions may focus on improving access to nutritious food, enhancing social support, and providing education on healthy eating [14]. In geriatric homes, interventions might include modifying meal plans, addressing swallowing difficulties, and promoting a more personalized approach to nutritional care [15].
The comparative examination of nutritional status among community-living older adults and those in geriatric homes provides valuable insights into the unique challenges faced by each population. By identifying the factors that contribute to malnutrition in these settings, healthcare providers and policymakers can develop targeted strategies to improve nutritional outcomes and enhance the quality of life for older adults. This study aimed to contribute to the growing body of evidence in this field, with the ultimate goal of promoting healthy aging and reducing the burden of malnutrition among older adults worldwide.
Instrument and Methods
Study design and setting
This comparative cross-sectional study assessed the nutritional status of community-dwelling older adults and older adults residing in geriatric homes in Babil Governorate, Iraq over two months, from January 5th to March 10th, 2025. The comparative design was selected to identify potential differences in nutritional status between the two groups, providing insights into the effects of living arrangements on the health and well-being of older adults in the community. Babil Governorate was chosen because of its diverse population and the presence of both community-dwelling older adults and geriatric homes, which allowed for a comprehensive comparison of nutritional status between the two groups.
Inclusion/exclusion criteria
The sample consisted of 200 participants, divided into two groups (100 community-dwelling older adults and 100 older adults residing in geriatric homes). Participants were included if they were aged 60 years or older, were willing to participate, and were able to provide informed consent. Exclusion criteria included severe cognitive impairment, terminal illness, or refusal to participate. The sample size was determined to ensure adequate statistical power for detecting significant differences between the groups.
Study tools
Nutritional status was assessed using the MNA tool, a validated and widely used instrument for evaluating malnutrition and the risk of malnutrition among older adults. The MNA consists of questions related to nutritional intake, weight loss, mobility, psychological stress, and anthropometric measurements (e.g., body mass index). Additionally, demographic information such as age, gender, and marital status is collected.
Validity and reliability
The MNA tool has been extensively validated and demonstrates high reliability and validity for assessing nutritional status in older populations. Before data collection, the tool was reviewed by a panel of experts to ensure its cultural appropriateness and relevance to the study context. A pilot study involving 20 participants (ten from each group) was conducted to test the clarity and reliability of the tool, and minor adjustments were made based on feedback.
Data collection
Participants were recruited through purposive sampling. Community-dwelling older adults were identified via local community centers and public health clinics, while older adults in geriatric homes were recruited directly from facilities in Babil Governorate. Trained researchers administered the MNA tool through face-to-face interviews to ensure accurate data collection. Anthropometric measurements were taken using standardized procedures.
Statistical analysis
Data were analyzed using SPSS 25 software. Descriptive statistics, including mean, standard deviations, frequencies, and percentages, were used to summarize demographic and nutritional data. Independent t-tests and chi-square tests were employed to compare continuous and categorical variables, respectively, between the two groups. A p-value of <0.05 was considered statistically significant. Multivariate analysis, including logistic regression analysis, was conducted to identify factors associated with malnutrition or the risk of malnutrition, adjusting for potential confounders.
Findings
The mean age was significantly higher in the geriatric home group (74.8±7.1 years) compared to the community-dwelling group (72.5±6.4 years; p=0.032), indicating an older population in institutional settings. Gender distribution was nearly equal in both groups, with no significant difference (p=0.564). However, marital status showed a significant difference, as only 10% of geriatric home residents were married compared to 45% of community-dwelling individuals (p<0.001). Conversely, 90% of geriatric home residents were widowed, single, or divorced, which was significantly higher than the 55% in the community-dwelling group (p<0.001; Table 1).
Table 1. Frequency of demographic characteristics of participants
Malnutrition was significantly more prevalent among geriatric home residents. While 60% of community-dwelling individuals had normal nutritional status, only 30% of those in geriatric homes fell into this category (p<0.001). Conversely, the percentage of individuals at risk of malnutrition was higher among geriatric home residents (50%) compared to community-dwelling individuals (30%; p=0.005). Additionally, 20% of geriatric home residents were malnourished, which is double the rate found in the community-dwelling group (10%; p=0.047; Table 2).
Table 2. Nutritional status based on mini nutritional assessment (MNA)
The mean body mass index (BMI) was significantly lower in geriatric home residents (22.8±3.5kg/m2) than in community-dwelling individuals (24.6±3.1kg/m2; p=0.018), suggesting a poorer overall nutritional status. Weight loss in the past three months was significantly greater in geriatric home residents (12.2±3.4) compared to community dwellers (8.5±2.3; p<0.001), indicating greater nutritional deterioration in geriatric individuals. Furthermore, daily food consumption showed a significant decrease in geriatric home residents (2.4±0.6 meals/day) compared to the community-dwelling group (3.1±0.5 meals/day; p<0.001), emphasizing decreased nutritional intake as a potential factor for malnutrition. Additionally, mobility restrictions were significantly higher among geriatric home residents (50(50%)) compared to community-dwelling individuals (25(25%); p=0.002), suggesting that limited mobility may also contribute to poorer nutritional outcomes.
Living in a geriatric home was associated with a 2.6-fold increased risk of malnutrition (p=0.002). A BMI under 22 was a strong predictor, increasing the risk of malnutrition by 3.1 times (p=0.001). Recent weight loss was also a significant predictor, with individuals experiencing weight loss being 2.8 times more likely to be malnourished (p=0.003). Low meal frequency (<3 meals/day) was the strongest predictor, increasing the risk of malnutrition by 3.5 times (p<0.001; Table 3).
Table 3. Multivariate analysis-logistic regression for predictors of malnutrition
Discussion
This study aimed to compare the nutritional status of community-dwelling older adults with those residing in geriatric homes. The findings highlight significant differences in the nutritional status of older adults living in community settings compared to those in geriatric homes. The MNA scores indicated that malnutrition and the risk of malnutrition were notably higher among geriatric home residents. Only 30% of geriatric older adults had normal nutritional status compared to 60% of their community-dwelling counterparts. Furthermore, the percentage of individuals at risk of malnutrition was significantly greater among those in geriatric homes. Additionally, the prevalence of malnutrition in geriatric home residents was twice as high as in community-dwelling individuals. These findings align with previous studies indicating that geriatric older adults are at higher risk of malnutrition due to factors, such as decreased autonomy, dietary restrictions, and limited access to diverse food options [16, 17].
The comparative analysis of nutritional indicators further reinforced these findings. The mean BMI was significantly lower among geriatric home residents compared to community dwellers, indicating a higher prevalence of undernutrition among geriatric individuals. Weight loss over the past three months was significantly more pronounced in geriatric home residents compared to community-living individuals, a trend that can be attributed to inadequate nutritional intake, decreased physical activity, and potential health conditions affecting appetite and metabolism [2]. Moreover, daily meal consumption was substantially lower among geriatric home residents than among those residing in the community. This reduced meal frequency may be a crucial factor in the higher rates of malnutrition observed among geriatric individuals, as inadequate meal consumption has been linked to weight loss and deteriorating health in older adults [18, 19]. Furthermore, mobility restrictions were significantly more common among geriatric home residents (50%) than in community-living older adults, suggesting that physical barriers could contribute to decreased independence in meal choice and consumption, ultimately exacerbating nutritional deficiencies [20, 21].
The logistic regression analysis similarly identified key predictors of malnutrition in older adults. Living in a geriatric home was associated with a 2.6-fold increased risk of malnutrition, supporting previous evidence that geriatric settings may present additional challenges in maintaining adequate nutrition due to dependence on facility-provided food and potential neglect [22, 23]. A BMI below 22 emerged as a strong predictor, increasing the risk of malnutrition by 3.1 times, reinforcing the well-established relationship between low BMI and nutrition risk in older populations [24]. Recent weight loss also significantly predicted malnutrition, with individuals experiencing weight loss being 2.8 times more likely to be malnourished. This finding is consistent with studies showing that unintended weight loss is a major red flag for nutritional decline in geriatric populations [25, 26]. Notably, low meal frequency (<three meals/day) was the strongest predictor, increasing the risk of malnutrition by 3.5 times, emphasizing the critical role of regular and adequate food intake in preventing nutritional deterioration [27, 28].
Overall, these findings underscore the pressing need for targeted nutritional interventions in geriatric homes to mitigate malnutrition risks. Strategies that include individualized nutrition plans, increased meal frequency, and mobility-enhancing programs can be effective in improving the nutritional well-being of geriatric older adults. Future studies should explore interventions tailored to the unique needs of geriatric home residents, considering both nutritional and physical activity components to enhance overall health outcomes.
This study has several limitations that must be taken into consideration. First, the cross-sectional design prevents the establishment of causality between living arrangements and nutritional status. Second, potential selection bias may exist, as participants from community settings may differ in socioeconomic status and health conditions compared to those in geriatric homes. Third, self-reported nutritional intake and weight loss may introduce recall bias. Additionally, factors such as cognitive status, comorbidities, and social support, which can impact nutritional outcomes, were not significantly analyzed. Lastly, the study was conducted in a specific location, which may limit the generalizability of the findings to other populations.
The study highlights significant disparities in nutritional status among community-dwelling older adults and those residing in geriatric homes, with geriatric individuals facing a higher prevalence of malnutrition, decreased meal frequency, and greater weight loss. To address these challenges, targeted interventions are recommended, including personalized meal plans tailored to individual preferences and needs, regular nutrition screenings to identify at-risk individuals, and mobility support programs to enhance physical activity and appetite. Additionally, caregiver training and improved meal support practices in geriatric homes can help ensure adequate food consumption. Policymakers and healthcare providers must collaborate to implement these strategies, fostering a multidisciplinary approach to malnutrition prevention and improving the overall well-being of older adults, particularly those in institutional settings.
Conclusion
Geriatric home residents are at greater risk of malnutrition compared to community-dwelling older adults.
Acknowledgments: The authors would like to thank all the participants who allowed them to interview them for their cooperation and participation.
Ethical Permissions: Ethical approval was obtained from the Research Ethics Committee of the College of Health and Medical Techniques/Kufa, Al-Furat Al-Awsat Technical University (date: 27.09.2024, number: 294/1).
Conflicts of Interests: Nothing declared by the authors.
Authors' Contribution: Niazy SM (First Author), Introduction Writer/Main Researcher (25%); Al-Eqabi QAK (Second Author), Assistant Researcher/Discussion Writer (25%); Radhi MM (Third Author), Methodologist/Statistical Analyst (25%); AL-Thabhawee GDM (Fourth Author), Statistical Analyst (25%)
Funding/Support: The present study was not financially supported.
Keywords:
References
1. Tek NA, Karaà MÅ. Determinants of health related quality of life in home dwelling elderly population: Appetite and nutritional status. J Nutr Health Aging. 2018;22(8):996-1002. [Link] [DOI:10.1007/s12603-018-1066-9]
2. Ganhão-Arranhado S, Poínhos R, Pinhão S. Determinants of nutritional risk among community-dwelling older adults with social support. Nutrients. 2023;15(11):2506. [Link] [DOI:10.3390/nu15112506]
3. Abugroun A, Nayyar A, Abdel-Rahman M, Patel P. Impact of malnutrition on hospitalization outcomes for older adults admitted for sepsis. Am J Med. 2021;134(2):221-6. [Link] [DOI:10.1016/j.amjmed.2020.06.044]
4. Wei K, Nyunt MS, Gao Q, Wee SL, Yap KB, Ng TP. Association of frailty and malnutrition with long-term functional and mortality outcomes among community-dwelling older adults: Results from the Singapore longitudinal aging study 1. JAMA Netw Open. 2018;1(3):e180650. [Link] [DOI:10.1001/jamanetworkopen.2018.0650]
5. Balat KZ, Laftah SA, Radhi M. The relationship between psychological distress and quality of life among women undergoing mastectomy in Iraq: A descriptive correlational study. Natl J Community Med. 2025;16(1):20-7. [Link] [DOI:10.55489/njcm.160120254716]
6. Scheufele P, Rappl A, Visser M, Kiesswetter E, Volkert D. Characterisation of community-dwelling older adults with poor appetite. Eur J Nutr. 2023;62(5):1991-2000. [Link] [DOI:10.1007/s00394-023-03129-5]
7. Shakil S, Ghosh J, Singh K, Chaudhury SR. Comparative analysis of nutritional status among institutionalised and community-dwelling elderly women and its association with mental health status and cognitive function. J Family Med Prim Care. 2024;13(8):3078-83. [Link] [DOI:10.4103/jfmpc.jfmpc_1932_23]
8. Al-Eqabi QA, Niazy SM, Radhi MM. Effectiveness of digital health interventions in managing glycated haemoglobin: A randomized controlled trial. Natl J Community Med. 2024;15(9):747-53. [Link] [DOI:10.55489/njcm.150920244442]
9. Al-Eqabi QA, Niazy SM, Radhi MM. Amputation-related factors influencing activities of daily living among amputees. Iran J War Public Health. 2024;16(2):123-9. [Link]
10. Corish CA, Bardon LA. Malnutrition in older adults: Screening and determinants. Proc Nutr Soc. 2019;78(3):372-9. [Link] [DOI:10.1017/S0029665118002628]
11. Volkert D, Beck AM, Cederholm T, Cereda E, Cruz-Jentoft A, Goisser S, et al. Management of malnutrition in older patients-current approaches, evidence and open questions. J Clin Med. 2019;8(7):974. [Link] [DOI:10.3390/jcm8070974]
12. Malih Radhi M, Zair Balat K. Health literacy and its association with medication adherence in patients with hypertension: A mediating role of social support. Iran Rehabil J. 2024;22(1):117-28. [Link] [DOI:10.32598/irj.22.1.1989.1]
13. Valentini A, Federici M, Cianfarani MA, Tarantino U, Bertoli A. Frailty and nutritional status in older people: The mini nutritional assessment as a screening tool for the identification of frail subjects. Clin Interv Aging. 2018;13:1237-44. [Link] [DOI:10.2147/CIA.S164174]
14. Radhi MM, Al-Eqabi QA, Hindi NK. Rehabilitation problems of people with motor disabilities at Babylon center for rehabilitation of the disabled. Med J Babylon. 2023;20(4):838-43. [Link] [DOI:10.4103/MJBL.MJBL_674_23]
15. Radhi MM, Elywy GJ, Al-Eqabi QAK. Burdens among wives of disabled people in the light of some social variables. Iran Rehabil J. 2023;21(3):473-84. [Link] [DOI:10.32598/irj.21.3.1765.3]
16. Caso G, Vecchio R. Factors influencing independent older adults (un) healthy food choices: A systematic review and research agenda. Food Res Int. 2022;158:111476. [Link] [DOI:10.1016/j.foodres.2022.111476]
17. Elywy GJ, Radhi MM, Al-Eqabi QA. Relationship between social support and self-hardiness among breast cancer women in Nasiriyah, Iraq. J Pak Med Assoc. 2023;73(9):S9-14. [Link] [DOI:10.47391/JPMA.IQ-02]
18. DeLacey E, Tann C, Groce N, Kett M, Quiring M, Bergman E, et al. The nutritional status of children living within institutionalized care: A systematic review. PeerJ. 2020;8:e8484. [Link] [DOI:10.7717/peerj.8484]
19. Hamza NF, Ewadh RM, Radhi MM, Hindi NK, AL-Jubori RH, Hadi B, et al. Prevalence of measles virus infection among children in Babylon governorate, 2017-2019: A retrospective descriptive data analysis. AIP Conf Proc. 2023;2776(1):020006. [Link] [DOI:10.1063/5.0136194]
20. Burris M, Kihlstrom L, Arce KS, Prendergast K, Dobbins J, McGrath E, et al. Food insecurity, loneliness, and social support among older adults. J Hunger Environ Nutr. 2021;16(1):29-44. [Link] [DOI:10.1080/19320248.2019.1595253]
21. Radhi MM, Niazy SM, Abed SN. Individual-related factors associated with treatment adherence among hypertensive patients. J Public Health Afr. 2023;14(6):2466. [Link] [DOI:10.4081/jphia.2023.2466]
22. Elywy GJ, Radhi MM, Tuama AM. Determination the causes of neonatal mortality during the last 3 years ago in Al-Kut City. Medico Leg Update. 2020;20(3):1412-9. [Link]
23. Radhi MM. Degree of disease acceptance and health seeking behaviors for type 2 diabetic patients at diabetic center in Hilla City. Medico Leg Update. 2020;20(2):853-8. [Link] [DOI:10.37506/mlu.v20i2.1347]
24. Bosch X, Monclús E, Escoda O, Guerra-García M, Moreno P, Guasch N, et al. Unintentional weight loss: Clinical characteristics and outcomes in a prospective cohort of 2677 patients. PLoS One. 2017;12(4):e0175125. [Link] [DOI:10.1371/journal.pone.0175125]
25. Radhi MM, AL-Rubaey NK, AL-Jubori RH, Kadhim Hindi NK. Prevalence of viral hepatitis infections in Babylon province, Iraq, during the interval from 2014 to 2018. Ann Trop Med Public Health. 2019;22(9):S253. [Link] [DOI:10.36295/ASRO.2019.220923]
26. Yasir AA, Elywy GJ, Radhi MM. Assessment the development of social responsibility among sample of (Kut Technical Institute, Iraq) students and its relation to social media network sites. Res J Pharm Technol. 2018;11(10):4426-30. [Link] [DOI:10.5958/0974-360X.2018.00810.7]
27. Souza AC, Vasconcelos AR, Dias DD, Komoni G. The integral role of magnesium in muscle integrity and aging: A comprehensive review. Nutrients. 2023;15(24):5127. [Link] [DOI:10.3390/nu15245127]
28. Badr SH, Abed MT, Faris I. Mother's knowledge concerning preventive measures of their children during the COVID-19 period. Rawal Med J. 2023;48(2):289. [Link] [DOI:10.5455/rmj.20230114031923]