Volume 17, Issue 2 (2025)
Iran J War Public Health 2025, 17(2): 123-129 |
Back to browse issues page
Article Type:
Subject:
Ethics code: INTI-FHLS-03-01-2021
History
Received: 2025/03/3 | Accepted: 2025/04/13 | Published: 2025/04/21
Received: 2025/03/3 | Accepted: 2025/04/13 | Published: 2025/04/21
How to cite this article
Vasanthi R, Subramaniam A, Asoghan K, Muthusamy S, Chinnusamy S, Purushothaman V. Impact of Face Masks on Cardiopulmonary Efficiency During Exercise in Older Adults. Iran J War Public Health 2025; 17 (2) :123-129
URL: http://ijwph.ir/article-1-1564-en.html
URL: http://ijwph.ir/article-1-1564-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Authors
R.K. Vasanthi1, A. Subramaniam *2, K. Asoghan1, S. Muthusamy3, S. Chinnusamy4, V.K. Purushothaman1
1- Faculty of Health and Life Sciences, INTI International University, Nilai, Malaysia
2- Department of Physiotherapy, M. Kandiah Faculty of Medical and Health Sciences, Tunku Abdul Rahman University, Petaling Jaya, Malaysia
3- Centre for Advance Lung diseases and Lung transplant, Kovai Medical Center and Hospitals, Coimbatore, India
4- Department of Physiotherapy, PPG College of Physiotherapy, The Tamil Nadu Dr. M.G.R. Medical University, Chennai, India
2- Department of Physiotherapy, M. Kandiah Faculty of Medical and Health Sciences, Tunku Abdul Rahman University, Petaling Jaya, Malaysia
3- Centre for Advance Lung diseases and Lung transplant, Kovai Medical Center and Hospitals, Coimbatore, India
4- Department of Physiotherapy, PPG College of Physiotherapy, The Tamil Nadu Dr. M.G.R. Medical University, Chennai, India
Full-Text (HTML) (247 Views)
Introduction
Face masks have progressively become a fundamental aspect of our new-normal existence as part of the public health and social measures implemented during the coronavirus disease pandemic [1]. Wearing surgical and KN95/N95 masks was rigorously mandated in public settings. National and global officials have suggested modifying FFP3 masks for enhanced protection in light of emerging variants of the severe acute respiratory syndrome coronavirus-2 [2]. In recent years, the use of face masks has been adopted more broadly to prevent various infectious respiratory diseases [3]. The transmission risk of infections may also increase during exercise due to heavy breathing, especially indoors, such as in sports and fitness centers [4]. The global health and fitness landscape of the early 2020s was radically transformed with the widespread adoption of face masks as a primary public health measure for mitigating the transmission of respiratory viruses, most notably SARS-CoV-2 [5].
While critical for restricting viral transmission, the widespread adoption of face masks has permeated numerous aspects of daily life, including physical activity. A higher rate of viral transmission has been observed among the elderly, identifying them as the most vulnerable group [6]. Although the efficacy of face masks in attenuating the transmission of infectious diseases is well documented, potential physiological impacts, including cardiopulmonary function, should be thoroughly investigated, particularly among at-risk populations such as elderly individuals [7]. Wearing a surgical mask does not significantly influence breathlessness, respiratory rate, heart rate, or oxygen saturation during submaximal exercise in healthy individuals [8]. Nevertheless, wearing a surgical mask increases the rate of dyspnea when compared to individuals without a mask, but it does not affect the results of a 6-minute walk test in a normally healthy population [9].
Although we are unable to reverse the biological process of aging, frequent engagement in sports and physical activities may mitigate the physiological changes associated with aging and enhance overall health and well-being [10]. Consistent physical activity provides significant health advantages for healthy aging, and these benefits are thoroughly documented [10]. Physical activity among older adults has been recommended at below 150 minutes per week [11]. Being physically active has shown a significant association with maintaining mental health, emotional and psychological well-being, and cognitive function [12]. However, the widespread adoption of facemask usage to curb the spread of respiratory diseases has also been linked to an increasing trend in physical inactivity [6, 13]. Additionally, wearing facemasks during exercise has raised concerns about potential impacts on the cardiopulmonary system, including increased work of breathing (Wb), altered pulmonary gas exchange, and heightened dyspnea [14].
Wearing masks may affect human physiological systems, particularly cardiopulmonary function, causing augmented airway resistance, hypoxia, carbon dioxide retention, and alterations in lung function that may result in increased cardiac workload [15]. In contrast, a previous study indicated that the use of face masks does not have harmful effects [16]. To address this issue, numerous studies on the physiological effects of wearing facemasks have been conducted in recent times [14, 16-24]. Furthermore, a systematic and narrative review on the effect of wearing a face mask during exercise reported that the use of a face mask during exercise exerts a negligible effect on performance and physiological parameters [14, 16]. Elderly individuals have lower physiological reserves and are more vulnerable to the impact of external stressors, such as the respiratory burden caused by wearing a face mask, making this group a critical focus for further study [25]. Nevertheless, the use of facemasks among the elderly during exercise is still scarce, and the physiological effects remain unclear [14].
Significant changes to the structures of the respiratory system are associated with healthy aging, resulting in a progressive decline in pulmonary function and an increased ventilatory response to exercise [26]. Therefore, older individuals experience greater levels of mechanical ventilatory constraint during exercise compared to younger individuals, as indicated by an increased risk of expiratory flow limitation, higher operating lung capacities, and more work of breathing [27]. Despite such alterations in the cardiopulmonary system due to aging and declines in physical performance, sedentary living becomes more prevalent, and participation in formal exercise programs decreases with advancing age in older adults [28].
An earlier study examined the effect of wearing cloth and surgical masks on pulmonary and vital sign parameters and reported that neither cloth masks nor surgical masks produced significant changes in cardiorespiratory fitness at rest or after performing the 6-minute walk test (6MWT) in older adults. The potential effect of face masks on cardiopulmonary function during exercise relates to respiratory mechanics and modifications in gas exchange. Face masks inherently create added resistance to breathing during both inspiration and expiration [29]. These changes may have more profound effects on the older population. Age-related changes, such as decreased elasticity of the lungs, reduced strength of the respiratory muscles, and decreased ventilatory response to hypoxia and hypercapnia can contribute to the physiological burden of mask-wearing while exercising [30].
Thus, the objective of the current study was to examine the physiological effects of facemasks on cardiopulmonary efficiency and exercise performance among the elderly. The study hypothesized that wearing a facemask will reduce exercise performance, as the facemask causes a reduction in oxygen uptake, leading to decreased blood and muscle oxygenation, increased carbon dioxide rebreathing, and resistance during breathing efforts. This crossover study design will provide a comprehensive assessment of the influence of face masks on significant cardiopulmonary parameters, such as oxygen saturation, heart rate, blood pressure, and rating of perceived exertion, during exercise in older adults. The findings will provide valuable information regarding the physiological effects of exercising with a facemask in this specific group of individuals, thereby assisting in the establishment of exercise recommendations and safe physical activity participation.
Instrument and Methods
Study design
This experimental study employed a repeated measures approach. A total of 26 healthy elderly individuals who met the inclusion and exclusion criteria were recruited from three elderly care homes (n=14 males and n=12 females) using convenience sampling. The participants were non-smoking, healthy elderly individuals aged 60 to 70 who engaged in recreational aerobic activities such as jogging, running, or cycling on a regular basis. Individuals with orthopedic, cardiac, pulmonary, or inflammatory diseases, or any other medical contraindications (such as uncontrolled diabetes mellitus), were excluded from the current study.
Regarding ethical considerations, the first author informed the participants about the study’s methods. Before the experiment began, the subjects provided their written informed consent. The research was conducted in accordance with the ethics committee of INTI International University (INTI-FHLS-03-01-2021).
Parameters and procedure
Oxygen saturation (SPO2), blood pressure, heart rate, respiratory rate, distance walked in 6 minutes, forced vital capacity (FVC) [L], forced expiratory volume in 1 second (FEV1) [L], the FEV1/FVC ratio, peak expiratory flow (L/s), vital capacity [L], and maximum voluntary ventilation (MVV) [L] were examined.
The study objectives were examined under no mask (NM), disposable 3-ply surgical mask (SM; Novid PPE Sdn Bhd, Malaysia), disposable N95 mask (N95; 3M’s proprietary filter media, 3M™ Advanced Electret Media, Malaysia), and cloth mask (CM; PROXMASK™ 90V-LITE, Malaysia) conditions.
The participants’ pulmonary function was measured using the UBREATH® Pro Spirometer System PF680 (e-LinkCare Meditech Co., Ltd, Manchester, UK). Three expiratory maneuvers with one-minute intervals were recorded for each of the four conditions (NM, SM, N95, and CM), utilizing the best results from each pulmonary function test. The levels of SPO2 and heart rate were measured using a pulse oximeter, while blood pressure was recorded with a digital blood pressure monitor. The baseline assessment was conducted before the test commenced.
Participants completed the 6-minute walk test (6MWT) after the evaluation to assess their level of exercise endurance. They underwent the 6MWT while wearing an SM, N95, CM, and NM. The sequence in which the masks were worn varied from person to person based on random allocation. Without running, participants were encouraged to cover as much distance as possible in six minutes.
To avoid the impact of anticipation bias, tests were administered at the same time of day, separated by at least 24 hours, and participants were blinded to their own test results. Immediately following the 6MWT, one assessor was assigned to examine cardiopulmonary function, while another assessor was responsible for measuring the distance covered by the participants. Data were collected and subsequently analyzed.
Statistical analysis
SPSS 24 software was used to analyze the data after it was transferred from Microsoft Excel. The normality of the data was evaluated using the Kolmogorov-Smirnov test, which indicated that all of the data were normally distributed. The values of each variable are presented using the mean and standard deviation. For statistical analysis, the differences between each condition (NM, SM, N95, and CM) concerning SPO2, blood pressure, heart rate, respiratory rate, distance walked in 6 minutes, FVC [L], FEV1 [L], the FEV1/FVC ratio, peak expiratory flow (L/s), vital capacity [L], and MVV [L] were assessed using one-way repeated measures ANOVA. The significance level was set at 0.05 with a 95.0% confidence level for all analyses.
Findings
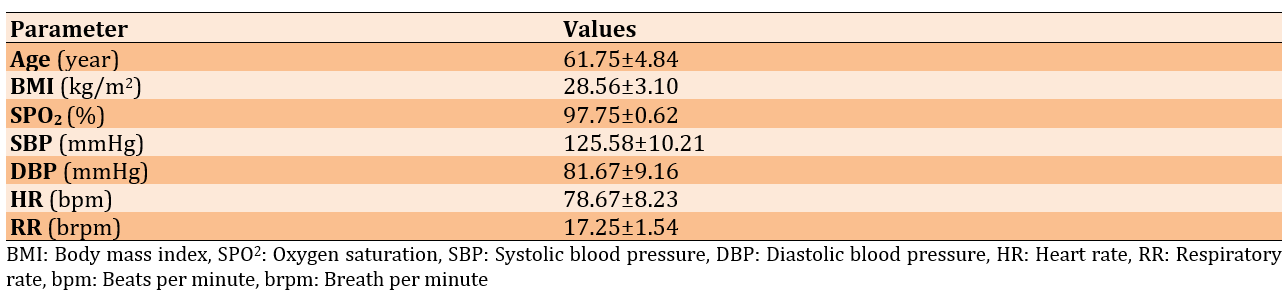
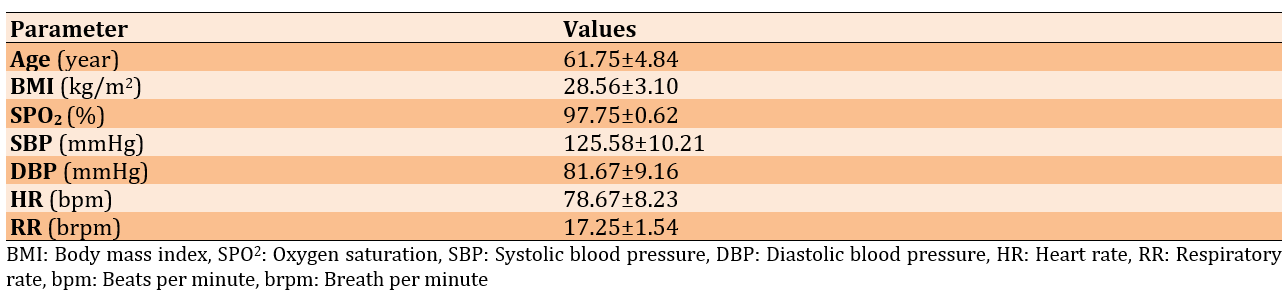
A total of 26 volunteers with a mean age of 61.75±4.84, ranging from 60 to 70 years, were enlisted. The subjects’ mean body mass index (BMI) was 28.56±3.10kg/m2 (Table 1).
Table 1. Mean values of demographic characteristics of the participants (n=26)
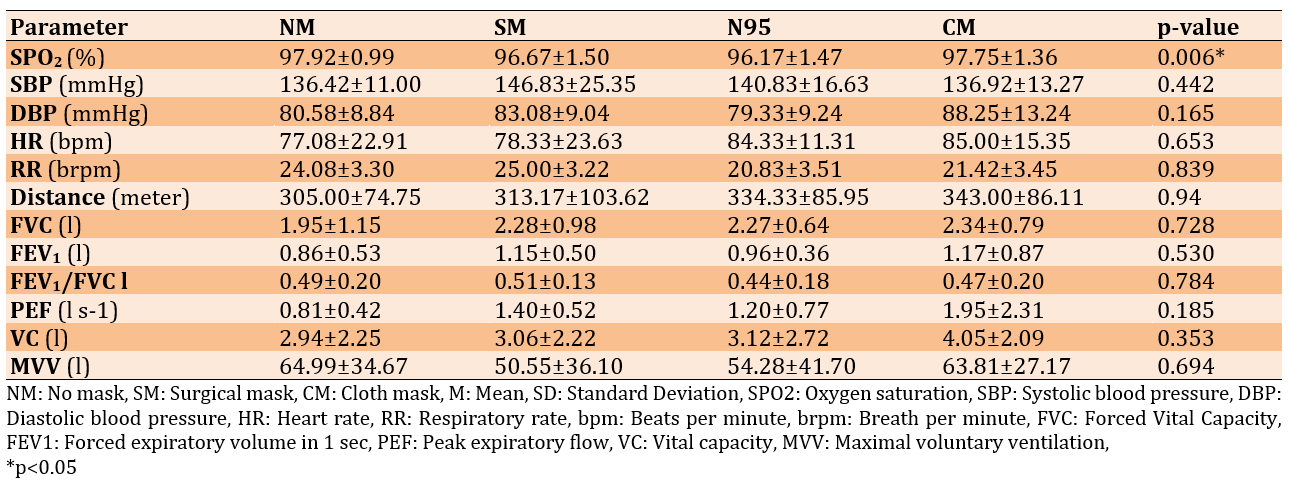
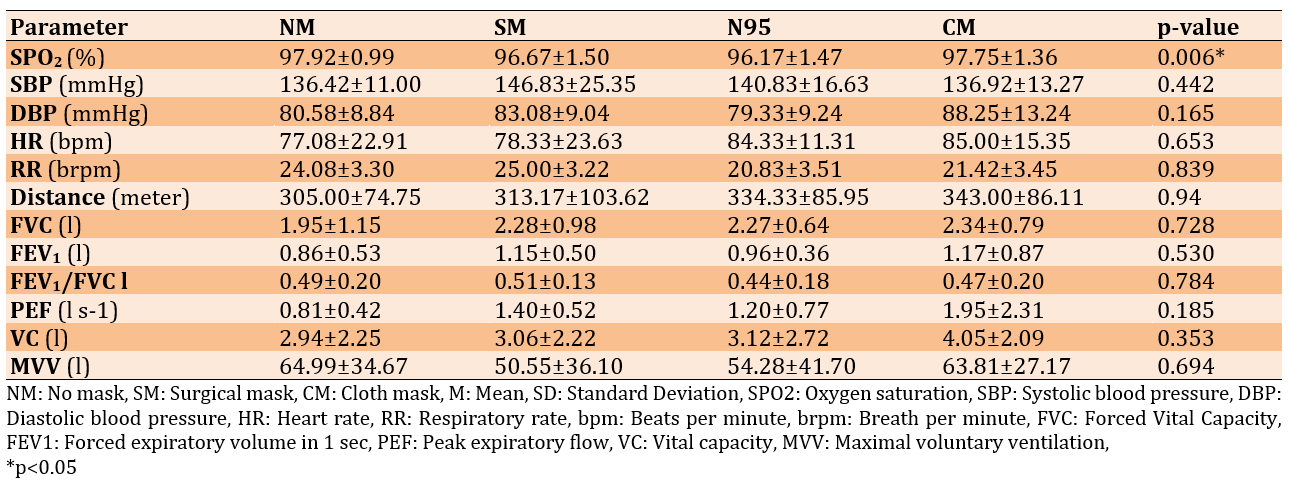
There were no significant differences in any of the parameters except for the SPO2 levels (p<0.05; Table 2).
Table 2. Mean values of the assessed parameters after a 6-minute walk test using four mask-wearing conditions
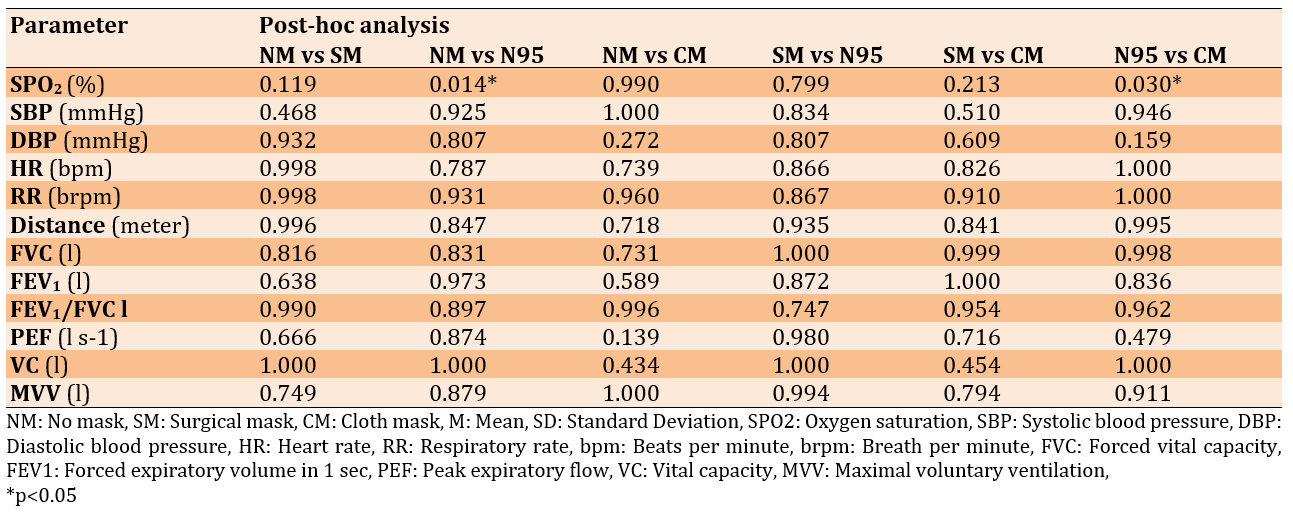
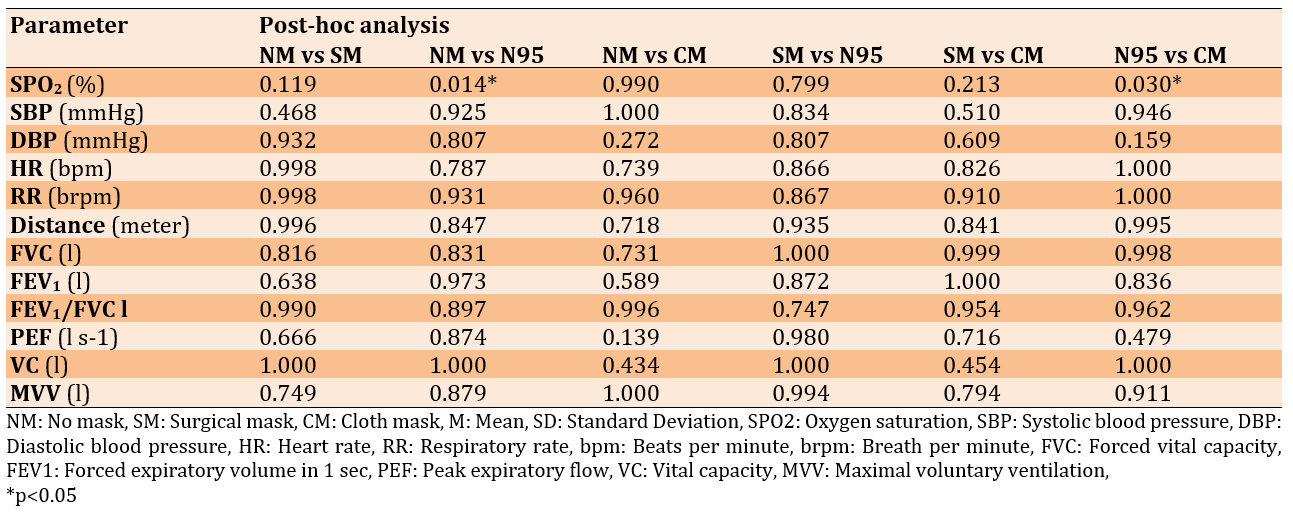
Furthermore, the post-hoc analysis of the SPO2 levels revealed significant differences between NM and N95 (p=0.014). There was also a significant difference between N95 and CM usage (p=0.030) regarding the SPO2 level (Table 3).
Table 3. Post-hoc analysis of the assessed parameters between four mask-wearing conditions after a 6-minute walk test
Discussion
The current study aimed to examine the physiological effects of different face masks on older adults’ cardiopulmonary efficiency during exercise. The use of SM, N95, or CM facemasks during a 6-minute walk test did not significantly affect blood pressure, heart rate, respiration rate, distance covered, or lung function assessments of older individuals compared to not wearing a mask. Previous research conducted on a sample of healthy young individuals has yielded comparable results to the present study [13, 31].
Specifically, the findings indicated that the utilization of surgical masks or N95 respirators during physical exercise was both safe and feasible. Furthermore, these masks were shown to have a low and statistically insignificant influence on several physiological indicators, such as blood pressure, heart rate, and respiratory rate during exercise [13, 31]. While some research suggests that masks have minimal impact on exercise performance and physiological parameters [13, 32], others report significant effects on cardiopulmonary function [33, 34]. Masks were found to be safe and feasible for short-term, moderate-to-strenuous exercise in healthy individuals [13]. However, they may lead to increased end-tidal CO2 levels [13, 32], decreased oxygen uptake, and reduced ventilation efficacy [33]. Overall, while masks appear to be tolerable during exercise, they may have varying effects on physiological parameters and subjective experiences.
Significant differences were found in the SPO2 levels with the use of the N95 mask. Previous studies have also reported a similar trend [31, 35]. The N95 mask offers the most protection and has the highest level of resistance compared to other masks [13, 14]. Nonetheless, even at a ventilation rate of >100L. min⁻¹, breathing simulation studies have demonstrated that the resistance exerted by the N95 mask is <2cm H2O. L⁻¹. s⁻¹ and it remains low even after extended simulation usage [13]. Conversely, another study involving eight participants has shown a reduction in oxygen levels of up to 3.2% and an increase in carbon dioxide of up to 20%, which may cause discomfort for elderly individuals [36]. Significant decreases in SpO2 are observed after prolonged N95 mask wear, lasting from 4 to 6 hours [37-40]. The reductions, while statistically significant, are generally small in magnitude. For instance, Kumar et al. have reported a decrease from 98.7% to 98.3% after 6 hours. Alongside changes in SpO2, increases in heart rate have also been noted [37, 39].
From a different research perspective, wearing a mask (surgical or N95) while walking for brief distances (5-6 minutes) may aid in the development of respiratory muscles [9, 31]. The initial use of masks has demonstrated a decrease in performance. While masks increased ratings of perceived exertion and dyspnea [32], they do not significantly alter arterial oxygen saturation, muscle oxygenation, or primary cardiovascular responses during submaximal or maximal exercise [16, 41]. However, as time progresses, individuals will inevitably acclimate to the practice of wearing a mask. Prolonged use of masks for weeks or even months may potentially enhance the strength and capacity of the respiratory muscles. The study additionally indicated that upon discontinuation of mask usage, the lungs will have an augmented oxygen intake, thereby potentially enhancing exercise performance [31, 36].
The emergence of SARS-CoV-2 and its impact on respiratory function have heightened concerns regarding the physiological effects of face masks, particularly during physical exertion in older adults [42]. However, the results of the present research were consistent with those published in a prior study involving 14 healthy individuals, finding no differences in blood and muscle oxygenation, perceived exertion, or heart rate during peak exercise performance, regardless of whether face masks were worn [16]. Despite the respiratory resistance associated with the use of masks, particularly N95 masks, research findings indicate that such resistance does not have a discernible impact on the dyspnea experienced during moderate-intensity exercise among older individuals [14, 26]. Thus, older adults may wear masks while exercising during outdoor activities or in busy areas without concern for negative impacts on performance, decreases in lung function capacity, increases in carbon dioxide rebreathing, or compromised oxygen consumption leading to lower arterial oxygen saturation of hemoglobin.
Several noteworthy limitations were observed in the present investigation, namely the relatively small sample size and the inclusion of only healthy older participants. Moreover, it is important to note that the findings of this investigation lack generalizability to exercises of higher intensity. It is recommended that future research encompasses a larger sample size, particularly focusing on older individuals with lung and heart diseases. Additionally, continuous monitoring of pulmonary function during the testing session is strongly advised.
While the use of N95 masks may result in a decrease in SpO2 levels, it is important to note that this does not have any adverse effects on the health of elderly adults. Moreover, it is recommended that older individuals with heart or lung conditions undergo a thorough assessment before engaging in physical activity while wearing a mask.
Conclusion
The use of different masks during moderate-intensity physical activity among older individuals does not exhibit any detrimental effects on blood pressure, heart rate, six-minute walking distance, or pulmonary function.
Acknowledgments: The authors express their sincere gratitude to all the volunteers who participated in this study.
Ethical Permissions: The research was approved by the INTI International University Ethical Committee (No: INTI-FHLS-03-01-2021). Informed consent was obtained from all subjects involved in the study.
Conflicts of Interests: None declared.
Authors' Contribution: Vasanthi RK (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (20%); Subramaniam A (Second Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (20%); Asoghan K (Third Author), Methodologist/Assistant Researcher/Discussion Writer (15%); Muthusamy S (Fourth Author), Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (15%); Chinnusamy S (Fifth Author), Assistant Researcher/Discussion Writer/Statistical Analyst (15%); Purushothaman VK (Sixth Author), Introduction Writer/Assistant Researcher/Discussion Writer/Statistical Analyst (15%)
Funding/Support: This research was supported by INTI International University [INTI IU Research Seed Grant 2021: INTI-FHLS-03-01-2021].
Face masks have progressively become a fundamental aspect of our new-normal existence as part of the public health and social measures implemented during the coronavirus disease pandemic [1]. Wearing surgical and KN95/N95 masks was rigorously mandated in public settings. National and global officials have suggested modifying FFP3 masks for enhanced protection in light of emerging variants of the severe acute respiratory syndrome coronavirus-2 [2]. In recent years, the use of face masks has been adopted more broadly to prevent various infectious respiratory diseases [3]. The transmission risk of infections may also increase during exercise due to heavy breathing, especially indoors, such as in sports and fitness centers [4]. The global health and fitness landscape of the early 2020s was radically transformed with the widespread adoption of face masks as a primary public health measure for mitigating the transmission of respiratory viruses, most notably SARS-CoV-2 [5].
While critical for restricting viral transmission, the widespread adoption of face masks has permeated numerous aspects of daily life, including physical activity. A higher rate of viral transmission has been observed among the elderly, identifying them as the most vulnerable group [6]. Although the efficacy of face masks in attenuating the transmission of infectious diseases is well documented, potential physiological impacts, including cardiopulmonary function, should be thoroughly investigated, particularly among at-risk populations such as elderly individuals [7]. Wearing a surgical mask does not significantly influence breathlessness, respiratory rate, heart rate, or oxygen saturation during submaximal exercise in healthy individuals [8]. Nevertheless, wearing a surgical mask increases the rate of dyspnea when compared to individuals without a mask, but it does not affect the results of a 6-minute walk test in a normally healthy population [9].
Although we are unable to reverse the biological process of aging, frequent engagement in sports and physical activities may mitigate the physiological changes associated with aging and enhance overall health and well-being [10]. Consistent physical activity provides significant health advantages for healthy aging, and these benefits are thoroughly documented [10]. Physical activity among older adults has been recommended at below 150 minutes per week [11]. Being physically active has shown a significant association with maintaining mental health, emotional and psychological well-being, and cognitive function [12]. However, the widespread adoption of facemask usage to curb the spread of respiratory diseases has also been linked to an increasing trend in physical inactivity [6, 13]. Additionally, wearing facemasks during exercise has raised concerns about potential impacts on the cardiopulmonary system, including increased work of breathing (Wb), altered pulmonary gas exchange, and heightened dyspnea [14].
Wearing masks may affect human physiological systems, particularly cardiopulmonary function, causing augmented airway resistance, hypoxia, carbon dioxide retention, and alterations in lung function that may result in increased cardiac workload [15]. In contrast, a previous study indicated that the use of face masks does not have harmful effects [16]. To address this issue, numerous studies on the physiological effects of wearing facemasks have been conducted in recent times [14, 16-24]. Furthermore, a systematic and narrative review on the effect of wearing a face mask during exercise reported that the use of a face mask during exercise exerts a negligible effect on performance and physiological parameters [14, 16]. Elderly individuals have lower physiological reserves and are more vulnerable to the impact of external stressors, such as the respiratory burden caused by wearing a face mask, making this group a critical focus for further study [25]. Nevertheless, the use of facemasks among the elderly during exercise is still scarce, and the physiological effects remain unclear [14].
Significant changes to the structures of the respiratory system are associated with healthy aging, resulting in a progressive decline in pulmonary function and an increased ventilatory response to exercise [26]. Therefore, older individuals experience greater levels of mechanical ventilatory constraint during exercise compared to younger individuals, as indicated by an increased risk of expiratory flow limitation, higher operating lung capacities, and more work of breathing [27]. Despite such alterations in the cardiopulmonary system due to aging and declines in physical performance, sedentary living becomes more prevalent, and participation in formal exercise programs decreases with advancing age in older adults [28].
An earlier study examined the effect of wearing cloth and surgical masks on pulmonary and vital sign parameters and reported that neither cloth masks nor surgical masks produced significant changes in cardiorespiratory fitness at rest or after performing the 6-minute walk test (6MWT) in older adults. The potential effect of face masks on cardiopulmonary function during exercise relates to respiratory mechanics and modifications in gas exchange. Face masks inherently create added resistance to breathing during both inspiration and expiration [29]. These changes may have more profound effects on the older population. Age-related changes, such as decreased elasticity of the lungs, reduced strength of the respiratory muscles, and decreased ventilatory response to hypoxia and hypercapnia can contribute to the physiological burden of mask-wearing while exercising [30].
Thus, the objective of the current study was to examine the physiological effects of facemasks on cardiopulmonary efficiency and exercise performance among the elderly. The study hypothesized that wearing a facemask will reduce exercise performance, as the facemask causes a reduction in oxygen uptake, leading to decreased blood and muscle oxygenation, increased carbon dioxide rebreathing, and resistance during breathing efforts. This crossover study design will provide a comprehensive assessment of the influence of face masks on significant cardiopulmonary parameters, such as oxygen saturation, heart rate, blood pressure, and rating of perceived exertion, during exercise in older adults. The findings will provide valuable information regarding the physiological effects of exercising with a facemask in this specific group of individuals, thereby assisting in the establishment of exercise recommendations and safe physical activity participation.
Instrument and Methods
Study design
This experimental study employed a repeated measures approach. A total of 26 healthy elderly individuals who met the inclusion and exclusion criteria were recruited from three elderly care homes (n=14 males and n=12 females) using convenience sampling. The participants were non-smoking, healthy elderly individuals aged 60 to 70 who engaged in recreational aerobic activities such as jogging, running, or cycling on a regular basis. Individuals with orthopedic, cardiac, pulmonary, or inflammatory diseases, or any other medical contraindications (such as uncontrolled diabetes mellitus), were excluded from the current study.
Regarding ethical considerations, the first author informed the participants about the study’s methods. Before the experiment began, the subjects provided their written informed consent. The research was conducted in accordance with the ethics committee of INTI International University (INTI-FHLS-03-01-2021).
Parameters and procedure
Oxygen saturation (SPO2), blood pressure, heart rate, respiratory rate, distance walked in 6 minutes, forced vital capacity (FVC) [L], forced expiratory volume in 1 second (FEV1) [L], the FEV1/FVC ratio, peak expiratory flow (L/s), vital capacity [L], and maximum voluntary ventilation (MVV) [L] were examined.
The study objectives were examined under no mask (NM), disposable 3-ply surgical mask (SM; Novid PPE Sdn Bhd, Malaysia), disposable N95 mask (N95; 3M’s proprietary filter media, 3M™ Advanced Electret Media, Malaysia), and cloth mask (CM; PROXMASK™ 90V-LITE, Malaysia) conditions.
The participants’ pulmonary function was measured using the UBREATH® Pro Spirometer System PF680 (e-LinkCare Meditech Co., Ltd, Manchester, UK). Three expiratory maneuvers with one-minute intervals were recorded for each of the four conditions (NM, SM, N95, and CM), utilizing the best results from each pulmonary function test. The levels of SPO2 and heart rate were measured using a pulse oximeter, while blood pressure was recorded with a digital blood pressure monitor. The baseline assessment was conducted before the test commenced.
Participants completed the 6-minute walk test (6MWT) after the evaluation to assess their level of exercise endurance. They underwent the 6MWT while wearing an SM, N95, CM, and NM. The sequence in which the masks were worn varied from person to person based on random allocation. Without running, participants were encouraged to cover as much distance as possible in six minutes.
To avoid the impact of anticipation bias, tests were administered at the same time of day, separated by at least 24 hours, and participants were blinded to their own test results. Immediately following the 6MWT, one assessor was assigned to examine cardiopulmonary function, while another assessor was responsible for measuring the distance covered by the participants. Data were collected and subsequently analyzed.
Statistical analysis
SPSS 24 software was used to analyze the data after it was transferred from Microsoft Excel. The normality of the data was evaluated using the Kolmogorov-Smirnov test, which indicated that all of the data were normally distributed. The values of each variable are presented using the mean and standard deviation. For statistical analysis, the differences between each condition (NM, SM, N95, and CM) concerning SPO2, blood pressure, heart rate, respiratory rate, distance walked in 6 minutes, FVC [L], FEV1 [L], the FEV1/FVC ratio, peak expiratory flow (L/s), vital capacity [L], and MVV [L] were assessed using one-way repeated measures ANOVA. The significance level was set at 0.05 with a 95.0% confidence level for all analyses.
Findings
A total of 26 volunteers with a mean age of 61.75±4.84, ranging from 60 to 70 years, were enlisted. The subjects’ mean body mass index (BMI) was 28.56±3.10kg/m2 (Table 1).
Table 1. Mean values of demographic characteristics of the participants (n=26)
There were no significant differences in any of the parameters except for the SPO2 levels (p<0.05; Table 2).
Table 2. Mean values of the assessed parameters after a 6-minute walk test using four mask-wearing conditions
Furthermore, the post-hoc analysis of the SPO2 levels revealed significant differences between NM and N95 (p=0.014). There was also a significant difference between N95 and CM usage (p=0.030) regarding the SPO2 level (Table 3).
Table 3. Post-hoc analysis of the assessed parameters between four mask-wearing conditions after a 6-minute walk test
Discussion
The current study aimed to examine the physiological effects of different face masks on older adults’ cardiopulmonary efficiency during exercise. The use of SM, N95, or CM facemasks during a 6-minute walk test did not significantly affect blood pressure, heart rate, respiration rate, distance covered, or lung function assessments of older individuals compared to not wearing a mask. Previous research conducted on a sample of healthy young individuals has yielded comparable results to the present study [13, 31].
Specifically, the findings indicated that the utilization of surgical masks or N95 respirators during physical exercise was both safe and feasible. Furthermore, these masks were shown to have a low and statistically insignificant influence on several physiological indicators, such as blood pressure, heart rate, and respiratory rate during exercise [13, 31]. While some research suggests that masks have minimal impact on exercise performance and physiological parameters [13, 32], others report significant effects on cardiopulmonary function [33, 34]. Masks were found to be safe and feasible for short-term, moderate-to-strenuous exercise in healthy individuals [13]. However, they may lead to increased end-tidal CO2 levels [13, 32], decreased oxygen uptake, and reduced ventilation efficacy [33]. Overall, while masks appear to be tolerable during exercise, they may have varying effects on physiological parameters and subjective experiences.
Significant differences were found in the SPO2 levels with the use of the N95 mask. Previous studies have also reported a similar trend [31, 35]. The N95 mask offers the most protection and has the highest level of resistance compared to other masks [13, 14]. Nonetheless, even at a ventilation rate of >100L. min⁻¹, breathing simulation studies have demonstrated that the resistance exerted by the N95 mask is <2cm H2O. L⁻¹. s⁻¹ and it remains low even after extended simulation usage [13]. Conversely, another study involving eight participants has shown a reduction in oxygen levels of up to 3.2% and an increase in carbon dioxide of up to 20%, which may cause discomfort for elderly individuals [36]. Significant decreases in SpO2 are observed after prolonged N95 mask wear, lasting from 4 to 6 hours [37-40]. The reductions, while statistically significant, are generally small in magnitude. For instance, Kumar et al. have reported a decrease from 98.7% to 98.3% after 6 hours. Alongside changes in SpO2, increases in heart rate have also been noted [37, 39].
From a different research perspective, wearing a mask (surgical or N95) while walking for brief distances (5-6 minutes) may aid in the development of respiratory muscles [9, 31]. The initial use of masks has demonstrated a decrease in performance. While masks increased ratings of perceived exertion and dyspnea [32], they do not significantly alter arterial oxygen saturation, muscle oxygenation, or primary cardiovascular responses during submaximal or maximal exercise [16, 41]. However, as time progresses, individuals will inevitably acclimate to the practice of wearing a mask. Prolonged use of masks for weeks or even months may potentially enhance the strength and capacity of the respiratory muscles. The study additionally indicated that upon discontinuation of mask usage, the lungs will have an augmented oxygen intake, thereby potentially enhancing exercise performance [31, 36].
The emergence of SARS-CoV-2 and its impact on respiratory function have heightened concerns regarding the physiological effects of face masks, particularly during physical exertion in older adults [42]. However, the results of the present research were consistent with those published in a prior study involving 14 healthy individuals, finding no differences in blood and muscle oxygenation, perceived exertion, or heart rate during peak exercise performance, regardless of whether face masks were worn [16]. Despite the respiratory resistance associated with the use of masks, particularly N95 masks, research findings indicate that such resistance does not have a discernible impact on the dyspnea experienced during moderate-intensity exercise among older individuals [14, 26]. Thus, older adults may wear masks while exercising during outdoor activities or in busy areas without concern for negative impacts on performance, decreases in lung function capacity, increases in carbon dioxide rebreathing, or compromised oxygen consumption leading to lower arterial oxygen saturation of hemoglobin.
Several noteworthy limitations were observed in the present investigation, namely the relatively small sample size and the inclusion of only healthy older participants. Moreover, it is important to note that the findings of this investigation lack generalizability to exercises of higher intensity. It is recommended that future research encompasses a larger sample size, particularly focusing on older individuals with lung and heart diseases. Additionally, continuous monitoring of pulmonary function during the testing session is strongly advised.
While the use of N95 masks may result in a decrease in SpO2 levels, it is important to note that this does not have any adverse effects on the health of elderly adults. Moreover, it is recommended that older individuals with heart or lung conditions undergo a thorough assessment before engaging in physical activity while wearing a mask.
Conclusion
The use of different masks during moderate-intensity physical activity among older individuals does not exhibit any detrimental effects on blood pressure, heart rate, six-minute walking distance, or pulmonary function.
Acknowledgments: The authors express their sincere gratitude to all the volunteers who participated in this study.
Ethical Permissions: The research was approved by the INTI International University Ethical Committee (No: INTI-FHLS-03-01-2021). Informed consent was obtained from all subjects involved in the study.
Conflicts of Interests: None declared.
Authors' Contribution: Vasanthi RK (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (20%); Subramaniam A (Second Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (20%); Asoghan K (Third Author), Methodologist/Assistant Researcher/Discussion Writer (15%); Muthusamy S (Fourth Author), Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (15%); Chinnusamy S (Fifth Author), Assistant Researcher/Discussion Writer/Statistical Analyst (15%); Purushothaman VK (Sixth Author), Introduction Writer/Assistant Researcher/Discussion Writer/Statistical Analyst (15%)
Funding/Support: This research was supported by INTI International University [INTI IU Research Seed Grant 2021: INTI-FHLS-03-01-2021].
Keywords:
COVID-19 [MeSH], Physical Activity [MeSH], Pulmonary Function Test [MeSH], Elderly [MeSH], Public Health [MeSH]
References
1. Kwon S, Joshi AD, Lo CH, Drew DA, Nguyen LH, Guo CG, et al. Association of social distancing and face mask use with risk of COVID-19. Nat Commun. 2021;12:3737. [Link] [DOI:10.1038/s41467-021-24115-7]
2. Howard J, Huang A, Li Z, Tufekci Z, Zdimal V, Van Der Westhuizen HM, et al. An evidence review of face masks against COVID-19. Proc Natl Acad Sci U S A. 2021;118(4):e2014564118. [Link] [DOI:10.1073/pnas.2014564118]
3. Shen B, Liu Y, Quan V, Wen X. Supplying masks to combat respiratory diseases: Safety index, welfare and government involvement. Int J Prod Res. 2023;61(8):2636-52. [Link] [DOI:10.1080/00207543.2021.1943036]
4. Lendacki FR, Teran RA, Gretsch S, Fricchione MJ, Kerins JL. COVID-19 outbreak among attendees of an exercise facility-Chicago, Illinois, August-September 2020. MMWR Morb Mortal Wkly Rep. 2021;70(9):321-5. [Link] [DOI:10.15585/mmwr.mm7009e2]
5. World Health Organization [Internet]. COVID-19 Public Health Emergency of International Concern (PHEIC) global research and innovation forum. Geneva: World Health Organization; 2020 [cited 2020 February 12]. Available from: https://cir.nii.ac.jp/crid/1380017282242895885 [Link]
6. Mustaffa N, Lee SY, Mohd Nawi SN, Che Rahim MJ, Chee YC, Muhd Besari A, et al. COVID-19 in the elderly: A Malaysian perspective. J Glob Health. 2020;10(2):020370. [Link] [DOI:10.7189/jogh.10.020370]
7. Ireri AM, Mwangi CN, Arhin V, Oigo M, Mugo S, Munanu RN. Development and initial validation of the attitudes toward face mask use scale (ATFMUS). Heliyon. 2022;8(12):e12349. [Link] [DOI:10.1016/j.heliyon.2022.e12349]
8. Reychler G, Straeten CV, Schalkwijk A, Poncin W. Effects of surgical and cloth facemasks during a submaximal exercise test in healthy adults. Respir Med. 2021;186:106530. [Link] [DOI:10.1016/j.rmed.2021.106530]
9. Person E, Lemercier C, Royer A, Reychler G. Effect of a surgical mask on six minute walking distance. Rev Mal Respir. 2018;35(3):264-8. [French] [Link] [DOI:10.1016/j.rmr.2017.01.010]
10. Teh CH, Lim KK, Chan YY, Lim KH, Azahadi O, Hamizatul Akmar AH, et al. The prevalence of physical activity and its associated factors among Malaysian adults: Findings from the National Health and Morbidity Survey 2011. Public Health. 2014;128(5):416-23. [Link] [DOI:10.1016/j.puhe.2013.10.008]
11. Boulton ER, Horne M, Todd C. Multiple influences on participating in physical activity in older age: Developing a social ecological approach. Health Expect. 2018;21(1):239-48. [Link] [DOI:10.1111/hex.12608]
12. Langhammer B, Bergland A, Rydwik E. The importance of physical activity exercise among older people. Biomed Res Int. 2018;2018:7856823. [Link] [DOI:10.1155/2018/7856823]
13. Epstein D, Korytny A, Isenberg Y, Marcusohn E, Zukermann R, Bishop B, et al. Return to training in the COVID-19 era: The physiological effects of face masks during exercise. Scand J Med Sci Sports. 2021;31(1):70-5. [Link] [DOI:10.1111/sms.13832]
14. Hopkins SR, Dominelli PB, Davis CK, Guenette JA, Luks AM, Molgat-Seon Y, et al. Face masks and the cardiorespiratory response to physical activity in health and disease. Ann Am Thorac Soc. 2021;18(3):399-407. [Link] [DOI:10.1513/AnnalsATS.202008-990CME]
15. Chandrasekaran B, Fernandes S. "Exercise with facemask; Are we handling a devil's sword?"-A physiological hypothesis. Med Hypotheses. 2020;144:110002. [Link] [DOI:10.1016/j.mehy.2020.110002]
16. Shaw K, Butcher S, Ko J, Zello GA, Chilibeck PD. Wearing of cloth or disposable surgical face masks has no effect on vigorous exercise performance in healthy individuals. Int J Environ Res Public Health. 2020;17(21):8110. [Link] [DOI:10.3390/ijerph17218110]
17. Li Y, Tokura H, Guo YP, Wong AS, Wong T, Chung J, et al. Effects of wearing N95 and surgical facemasks on heart rate, thermal stress and subjective sensations. Int Arch Occup Environ Health. 2005;78(6):501-9. [Link] [DOI:10.1007/s00420-004-0584-4]
18. Georgi C, Haase-Fielitz A, Meretz D, Gäsert L, Butter C. The impact of commonly-worn face masks on physiological parameters and on discomfort during standard work-related physical effort. DEUTSCHES ÄRZTEBLATT. 2020;117(40):674-5. [Link] [DOI:10.3238/arztebl.2020.0674]
19. Otsuka A, Komagata J, Sakamoto Y. Wearing a surgical mask does not affect the anaerobic threshold during pedaling exercise. J Hum Sport Exerc. 2020;17(1):22-8. [Link] [DOI:10.14198/jhse.2022.171.03]
20. Barbeito-Caamaño C, Bouzas-Mosquera A, Peteiro J, López-Vázquez D, Quintas-Guzmán M, Varela-Cancelo A, et al. Exercise testing in COVID-19 era: Clinical profile, results and feasibility wearing a facemask. Eur J Clin Invest. 2021;51(4):e13509. [Link] [DOI:10.1111/eci.13509]
21. Lässing J, Falz R, Pökel C, Fikenzer S, Laufs U, Schulze A, et al. Effects of surgical face masks on cardiopulmonary parameters during steady state exercise. Sci Rep. 2020;10:22363. [Link] [DOI:10.1038/s41598-020-78643-1]
22. Wong AY, Ling SK, Louie LH, Law GY, So RC, Lee DC, et al. Impact of the COVID-19 pandemic on sports and exercise. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2020;22:39-44. [Link] [DOI:10.1016/j.asmart.2020.07.006]
23. Morris NB, Piil JF, Christiansen L, Flouris AD, Nybo L. Prolonged facemask use in the heat worsens dyspnea without compromising motor-cognitive performance. Temperature. 2020;8(2):160-5. [Link] [DOI:10.1080/23328940.2020.1826840]
24. Yzaguirre Maura Id, Gen'ıs JT, Zabala DD, Monaco M, Garcia JS, Vielba FR, et al. COVID-19: Analysis of cavitary air inspired through a mask, in competitive adolescent athletes. Apunt Sport Med. 2021;56(210):100349. [Link] [DOI:10.1016/j.apunsm.2021.100349]
25. Kim JH, Benson SM, Roberge RJ. Pulmonary and heart rate responses to wearing N95 filtering facepiece respirators. Am J Infect Control. 2013;41(1):24-7. [Link] [DOI:10.1016/j.ajic.2012.02.037]
26. Molgat-Seon Y, Ramsook AH, Peters CM, Schaeffer MR, Dominelli PB, Romer LM, et al. Manipulation of mechanical ventilatory constraint during moderate intensity exercise does not influence dyspnoea in healthy older men and women. J Physiol. 2019;597(5):1383-99. [Link] [DOI:10.1113/JP277476]
27. Molgat-Seon Y, Dominelli PB, Ramsook AH, Schaeffer MR, Molgat Sereacki S, Foster GE, et al. The effects of age and sex on mechanical ventilatory constraint and dyspnea during exercise in healthy humans. J Appl Physiol. 2018;124(4):1092-106. [Link] [DOI:10.1152/japplphysiol.00608.2017]
28. Craighead DH, Heinbockel TC, Hamilton MN, Bailey EF, MacDonald MJ, Gibala MJ, et al. Time-efficient physical training for enhancing cardiovascular function in midlife and older adults: Promise and current research gaps. J Appl Physiol. 2019;127(5):1427-40. [Link] [DOI:10.1152/japplphysiol.00381.2019]
29. Roberge RJ, Coca A, Williams WJ, Powell JB, Palmiero AJ. Physiological impact of the N95 filtering facepiece respirator on healthcare workers. Respir Care. 2010;55(5):569-77. [Link]
30. Amann M. Pulmonary system limitations to endurance exercise performance in humans. Exp Physiol. 2012;97(3):311-8. [Link] [DOI:10.1113/expphysiol.2011.058800]
31. Akgul MS, Ozcan N, Uzun ME, Gurses VV, Baydil B. Physiological impact of wearing a surgical face mask during walking in the COVID-19 pandemic. Pedagog Phys Cult Sport. 2021;25(4):202-7. [Link] [DOI:10.15561/26649837.2021.0401]
32. Shaw KA, Zello GA, Butcher SJ, Ko JB, Bertrand L, Chilibeck PD. The impact of face masks on performance and physiological outcomes during exercise: A systematic review and meta-analysis. Appl Physiol Nutr Metab. 2021;46(7):693-703. [Link] [DOI:10.1139/apnm-2021-0143]
33. Shui L, Yang B, Tang H, Luo Y, Hu S, Zhong X, et al. Physiological effects of surgical and N95 masks during exercise in the COVID-19 era. Am J Med Sci. 2022;363(5):411-9. [Link] [DOI:10.1016/j.amjms.2022.02.006]
34. Hassabi M, Salehi S, Yekta AHA, Qutbi M, Hakakzadeh A, Poursaeid Esfahani M, et al. Effect of surgical and N95 facial masks on exercise tolerance, heart rate, respiratory rate and blood oxygen saturation. Russ Open Med J. 2022;11(2):201. [Link] [DOI:10.15275/rusomj.2022.0201]
35. Santos-Silva PR, Greve JMD, Pedrinelli A. During the coronavirus (COVID-19) pandemic, does wearing a mask improve or worsen physical performance?. REVISTA BRASILEIRA DE MEDICINA DO ESPORTE. 2020;26(4):281-4. [Link] [DOI:10.1590/1517-869220202604esp001]
36. Pifarré F, Zabala DD, Grazioli G, Maura IDY. COVID-19 and mask in sports. Apunt Sport Med. 2020;55(208):143-5. [Link] [DOI:10.1016/j.apunsm.2020.06.002]
37. Kumar P, Nath K, Prasad A, Tiwari LK, Chowdhry BK, Sinha AK, et al. Effects of the use of N95 masks on the vital signs of healthy healthcare workers during the COVID-19 pandemic: A hospital-based cross-sectional study. Cureus. 2023;15(6):e40622. [Link] [DOI:10.7759/cureus.40622]
38. Gaikwad RP, Banodkar AB, Nandgaonkar VP, Fernandes LC, Awasare PG, Awad MS, et al. Respiratory consequences of N95 mask during Covid-19 pandemic-an observational study. Int J Health Sci Res. 2021;11(4):55-61. [Link] [DOI:10.52403/ijhsr.20210407]
39. Bayoumi A, Shawki M, Abdulaziz A, Allam M, Mosleh M. Blood oxygen level with long-term use of N95 face mask in dental practice during coronavirus pandemic "Covid-19". Adv Med Pharm Dent Res. 2022;2(1):15-21. [Link] [DOI:10.21622/ampdr.2022.02.1.015]
40. Saccomanno S, Manenti RJ, Giancaspro S, Paskay LC, Katzenmaier CS, Mastrapasqua RF, et al. Evaluation of the effects on SpO2 of N95 mask (FFP2) on dental health care providers: A cross-sectional observational study. BMC Health Serv Res. 2022;22(1):248. [Link] [DOI:10.1186/s12913-022-07648-5]
41. Ade CJ, Turpin VG, Parr SK, Hammond ST, White Z, Weber RE, et al. Does wearing a facemask decrease arterial blood oxygenation and impair exercise tolerance?. Respir Physiol Neurobiol. 2021;294:103765. [Link] [DOI:10.1016/j.resp.2021.103765]
42. Narayanan DKL, Djearamane S, Ramalingam V, Kayarohanam S, Rajagopal S, Pandian S, et al. Potential COVID-19 therapeutics in clinical trials-a brief review. J Exp Biol Agric Sci. 2022;10(4):737-42. [Link] [DOI:10.18006/2022.10(4).737.742]