Volume 17, Issue 2 (2025)
Iran J War Public Health 2025, 17(2): 131-137 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2025/03/13 | Accepted: 2025/06/9 | Published: 2025/06/13
Received: 2025/03/13 | Accepted: 2025/06/9 | Published: 2025/06/13
How to cite this article
Faris H, Khanjary M, Badr S, Hussein B. Effect of Pain Management on Quality of Life Mediated by Sleep Quality in Patients with Chronic Musculoskeletal Disorders. Iran J War Public Health 2025; 17 (2) :131-137
URL: http://ijwph.ir/article-1-1550-en.html
URL: http://ijwph.ir/article-1-1550-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
1- Department of Laboratory and Clinical Sciences, Faculty of Pharmacy, Jabir Ibn Hayyan University for Medical and Pharmaceutical Sciences, Najaf, Iraq
2- Department of Adult Nursing, Faculty of Nursing, Al-Ameed University, Karbala, Iraq
3- Department of Pediatric Nursing, Faculty of Nursing, Al-Ameed University, Karbala, Iraq
4- Department of Adult Nursing, Altoosi University College, Najaf, Iraq
2- Department of Adult Nursing, Faculty of Nursing, Al-Ameed University, Karbala, Iraq
3- Department of Pediatric Nursing, Faculty of Nursing, Al-Ameed University, Karbala, Iraq
4- Department of Adult Nursing, Altoosi University College, Najaf, Iraq
Full-Text (HTML) (395 Views)
Introduction
Chronic musculoskeletal disorders (CMDs), which include osteoarthritis, rheumatoid arthritis, and persistent lower back pain, are globally recognized as the leading causes of disability and diminished quality of life (QoL) among adults [1]. These conditions not only affect physical functioning but also contribute significantly to emotional distress, leading to issues such as depression and anxiety. Furthermore, CMDs often result in increased healthcare costs, as patients may require ongoing medical treatment, physical therapy, and pain management interventions. Musculoskeletal conditions affect more than 1.7 billion people worldwide and significantly reduce physical functioning, social participation, and psychological well-being. The widespread prevalence of these disorders highlights the urgent need for effective preventive strategies and comprehensive management plans to alleviate their impact on individuals and healthcare systems alike. Additionally, public health initiatives aimed at raising awareness about CMDs can play a crucial role in promoting early intervention and improving overall health outcomes for affected individuals. Chronic pain is a hallmark of CMDs, and its persistent nature contributes not only to physical discomfort but also to emotional distress, sleep disturbances, and prolonged periods of functional impairment [2]. Consequently, the holistic management of CMDs requires a multidimensional approach, with pain relief as a central goal [3]. This comprehensive strategy not only addresses the physical aspects of pain but also considers psychological, emotional, and social factors that contribute to a patient’s overall health. Effective pain management often involves a combination of pharmacological treatments, physical therapy, lifestyle modifications, and complementary therapies, ensuring that all dimensions of a patient’s well-being are taken into account.
Nurses play a pivotal role in managing chronic pain through various strategies, including pharmacological guidance, patient education, relaxation techniques, encouragement of physical activity, and cognitive-behavioral interventions [4]. By assessing each patient’s unique pain profile and needs, nurses can tailor their approaches to ensure optimal pain relief and support. Additionally, they provide essential education on the proper use of medications, helping patients understand potential side effects and the importance of adherence to prescribed regimens. Furthermore, nurses often facilitate access to complementary therapies, such as massage or acupuncture, which can enhance traditional pain management methods. Previous studies have shown that nurse-led pain management interventions can reduce pain intensity and improve patient-reported outcomes [5]. These interventions often include personalized care plans that address the specific needs and preferences of each patient, which can lead to more effective pain control. Additionally, nurses play a critical role in monitoring patients’ responses to treatment, allowing for timely adjustments to pain management strategies as needed. For example, a randomized controlled trial found that individualized nursing interventions for chronic arthritis patients significantly improved pain levels and daily functioning [6]. Similarly, another study emphasized the impact of nurse-delivered cognitive-behavioral techniques on reducing pain perception and enhancing emotional resilience in patients with chronic musculoskeletal conditions [7].
Importantly, sleep satisfaction has emerged as a vital mediator in the relationship between chronic pain and overall QoL. Sleep disturbances are relatively common among individuals with CMDs, largely due to the intrusive nature of persistent pain that interrupts sleep continuity and reduces sleep depth. Poor sleep has been associated with increased pain sensitivity, decreased coping ability, and diminished QoL [8]. Individuals experiencing chronic pain often struggle with sleep disturbances, which can exacerbate pain perception and lead to a vicious cycle of worsening symptoms and reduced functioning. When patients achieve better sleep satisfaction, they are more likely to report lower pain intensity and improved emotional well-being. Research has shown that effective pain management can lead to improvements in sleep, which in turn affects various dimensions of QoL [9]. When pain is adequately controlled, individuals often experience fewer disruptions during the night, allowing for deeper and more restorative sleep. This improvement in sleep quality can enhance mood, cognitive function, and overall emotional well-being, which are critical components of QoL. Additionally, better sleep can increase energy levels and motivation, enabling individuals to engage more actively in social and recreational activities. Furthermore, improved sleep can bolster the immune system, leading to better physical health and resilience against illness, thereby contributing to a more holistic sense of well-being. It has been found that improvements in sleep mediate the relationship between pain reduction and physical and emotional well-being among older adults with chronic pain [10]. Furthermore, sleep-focused nursing interventions have been shown to enhance both sleep and QoL outcomes, indicating the potential synergistic impact of integrated pain and sleep management strategies [11]. These interventions may include sleep education, relaxation techniques, and cognitive-behavioral approaches designed to improve sleep hygiene and address any underlying sleep disorders. By improving sleep quality, patients often experience reduced pain sensitivity and enhanced emotional resilience, which can further contribute to better overall health and well-being.
Despite the increasing recognition of the association between pain, sleep, and QoL, there remains a gap in knowledge regarding the mediating role of sleep quality in the impact of nurses’ pain management approaches on the QoL of adults with CMDs. This gap is particularly concerning given that CMDs are prevalent conditions that significantly diminish individuals’ overall well-being and functioning. Bridging this gap is critical for developing comprehensive, evidence-based nursing practices and improving patient-centered care. Understanding how sleep quality mediates the relationship between effective pain management and QoL can provide valuable insights into the mechanisms at play, allowing healthcare providers to tailor interventions that address both pain and sleep issues simultaneously. Therefore, this study aimed to investigate the effect of nurses’ pain management on QoL, with a focus on the mediating role of sleep quality in adults with CMDs. By exploring this relationship, the study seeks to highlight the importance of integrating sleep assessments into pain management protocols, ultimately leading to enhanced health outcomes and a better quality of life for patients facing the challenges of chronic pain. Additionally, findings from this research could inform nursing education and training, ensuring that nurses are equipped with the knowledge and skills necessary to effectively address the interconnected issues of pain, sleep, and overall well-being in their patients.
Instrument and Methods
Study design
This cross-sectional study was conducted to investigate the effect of nurses’ pain management strategies on the QoL of adults with CMDs, with sleep quality serving as a mediating factor in 2024. The study aimed to identify relationships between various parameters using standardized questionnaires to obtain quantifiable data from individuals at a single point in time. This design was chosen to assess natural variations in pain management strategies and their association with sleep quality and perceived QoL.
Study sample
The study was conducted at a specialized outpatient rehabilitation and chronic pain center affiliated with a tertiary care hospital, which receives an average of 1,800 patients with CMDs each month. The target population comprised adults aged 18 years and older who were diagnosed with chronic musculoskeletal conditions, such as osteoarthritis, chronic low back pain, fibromyalgia, or rheumatoid arthritis, and who had been under nursing care for at least three months. The sample size was calculated based on a 95% confidence level, an assumed proportion (p) of 0.30 (based on previous literature), and a 0.5 margin of error. The initial sample size was calculated using the following formula:
n₀=(Z²×p×(1-p))/d²,
n₀=(1.96²×0.30×0.70)/0.05²≈323.
Adjusting N=1,800 using the formula:
n=(n₀×N)/(n₀+N-1),
n=(323×1800)/(323+1800-1)≈280.
Hence, a final sample of 280 participants was determined to be sufficient. Participants were selected based on the inclusion criteria, including adults aged ≥18 years, clinically diagnosed with a chronic musculoskeletal disorder for a minimum of six months, receiving nursing care related to pain management, and being able to communicate effectively and provide informed consent. Exclusion criteria included patients with comorbid severe psychiatric illness, cognitive impairments that could hinder questionnaire completion, or recent hospitalization within the last month due to acute exacerbation of their musculoskeletal condition.
Study tools
The study utilized a structured questionnaire comprising four parts.
The first component collected participants’ sociodemographic and medical information, including age, gender, diagnosis, duration of the condition, medication use, and comorbidities.
The second part involved the Pain Management Inventory-Nurse Version (PMI-N), which was adapted from established pain management assessment tools to evaluate the strategies used by nurses in managing chronic musculoskeletal pain. The PMI-N measured both pharmacological and non-pharmacological interventions, including medication adherence, physical therapy recommendations, cognitive-behavioral strategies, and relaxation techniques. This inventory has been used in previous studies assessing pain management in clinical nursing contexts [12].
The third part of the questionnaire utilized the Pittsburgh Sleep Quality Index (PSQI) to assess the sleep satisfaction of participants over the past month. The PSQI includes 19 self-rated questions grouped into seven components: subjective sleep quality, sleep latency, sleep duration, overall sleep efficiency, sleep disturbances, use of sleeping medications, and daytime dysfunction. Each component yields a score ranging from zero to three, with higher global scores indicating poorer sleep. The PSQI is a well-validated and reliable tool in both clinical and research settings [13].
The fourth part employed the World Health Organization Quality of Life-Brief Version (WHOQOL-BREF), a 26-item instrument designed to measure four domains of QoL, namely physical health, psychological well-being, social relationships, and environmental health. The WHOQOL-BREF has demonstrated excellent cross-cultural validity and is frequently used in studies involving patients with chronic conditions, including musculoskeletal disorders [14].
Validity and reliability
To ensure the content validity of the tool, the complete questionnaire was reviewed by a panel of five nursing and rehabilitation experts. Modifications were made based on expert feedback to enhance readability and cultural relevance. A pilot study was conducted with 10% of the target sample (28 individuals), and data from the pilot were excluded from the final analysis. The reliability of the tools was assessed using Cronbach’s alpha; the PMI-N showed a reliability coefficient of 0.87, the PSQI 0.83, and the WHOQOL-BREF 0.89, indicating high internal consistency. All tools used have been previously validated in similar populations and are suitable for use in clinical research settings involving chronic pain and QoL assessments.
Data collection
Data were collected through direct, face-to-face interviews and the use of the standardized questionnaire. Trained research nurses conducted the interviews in designated quiet areas within the hospital to ensure privacy and minimize distractions. Each consultation lasted approximately 30-40 minutes. Before participation, verbal and written informed consent was obtained from each participant, and the study protocol was approved by the institutional review board. Participants were assured of the confidentiality and anonymity of their responses and were informed of their right to withdraw at any time without any impact on their hospital treatment.
Statistical analysis
All statistical analyses were conducted using SPSS version 26.0. Descriptive statistics, including frequencies, percentages, means, and standard deviations, were used to summarize demographic and medical characteristics. The normality of the data distribution was assessed using the Kolmogorov-Smirnov and Shapiro-Wilk tests. To explore the relationships between several primary observed variables (nurses’ pain management strategies, sleep quality, and satisfaction with QoL), Pearson’s correlation coefficients were computed. Mediation analysis was conducted using the PROCESS macro for SPSS (Model 4) to test the indirect effect of pain management strategies on QoL through sleep. A bootstrapping method with 5,000 samples was employed to determine the significance of the indirect effect, and a p-value <0.05 was considered statistically significant during the analysis.
Findings
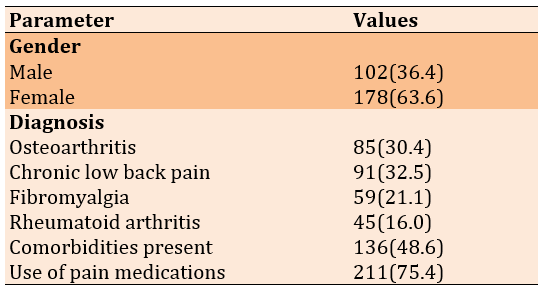
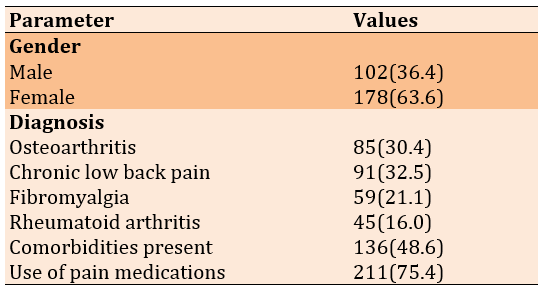
A total of 280 participants were enrolled, who had a mean age of 52.4±11.6 years, with a higher percentage being female (63.6%). Diagnostically, participants were primarily affected by chronic low back pain (32.5%) and osteoarthritis (30.4%), followed by fibromyalgia (21.1%) and rheumatoid arthritis (60%). On average, participants had been living with their musculoskeletal condition for over three years (38.5±19.2 months). About 75% had used pain medications, and nearly half had additional comorbidities, indicating a clinically complex population with multifactorial health burdens (Table 1).
Table 1. Frequency of sociodemographic and clinical characteristics of participants (n=280)
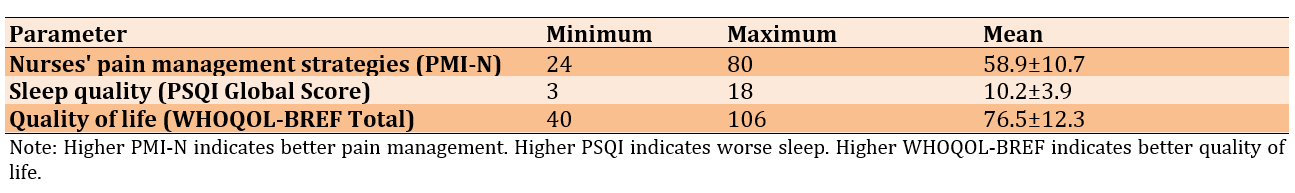
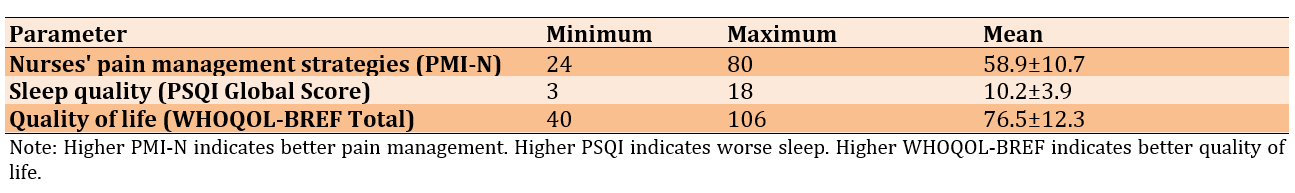
Participants reported mild exposure to nurse-led pain management strategies, generally poor sleep quality, and a relatively high perceived QoL (Table 2).
Table 2. Descriptive statistics of main study parameters
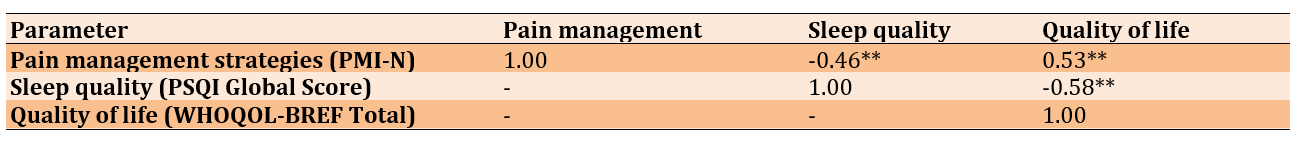
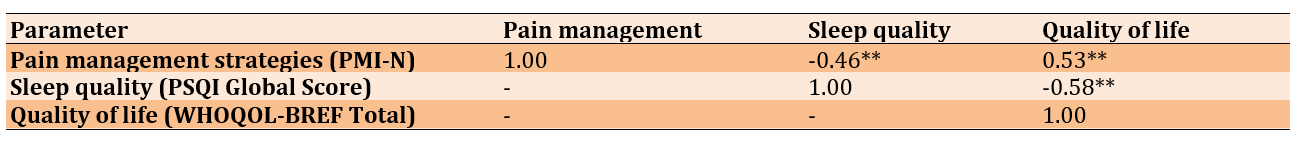
There was a statistically significant correlation between nurses’ pain management strategies and participants’ QoL (r=0.53, p<0.01), suggesting that more effective nursing interventions are associated with better perceived well-being. A moderate negative correlation was found between pain management and sleep quality (r=-0.46, p<0.01), indicating that higher levels of pain management are associated with improved sleep (lower PSQI scores). Sleep quality was also negatively correlated with QoL (r=-0.58, p<0.01), indicating that poor sleep was significantly associated with decreased satisfaction with QoL (Table 3).
Table 3. Pearson’s correlation matrix among key study parameters
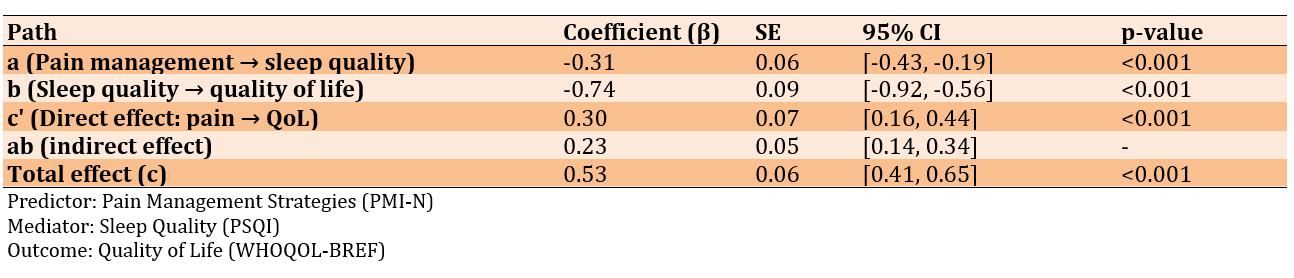
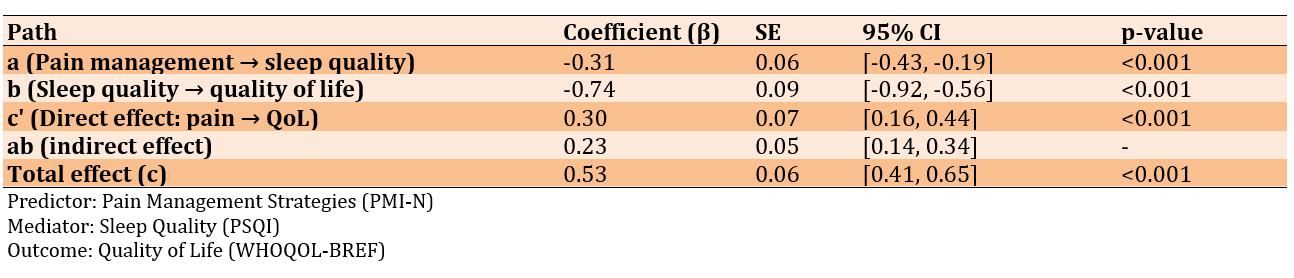
The direct path from pain management to sleep quality (path a) was significantly negative, indicating that improved pain management decreased sleep disturbances. The path from sleep quality to QoL (path b) was also significantly negative, showing that poorer sleep was associated with a lower QoL. The indirect effect (ab=0.23) was statistically significant, as the 95% confidence interval did not include 0, confirming that sleep quality partially mediates the relationship. Additionally, the direct effect (c’) remained significant, indicating partial rather than full mediation (Table 4).
Table 4. Mediation analysis using PROCESS Macro (Model 4)
Discussion
This study aimed to investigate the effect of nurses’ pain management on QoL, with a focus on the mediating role of sleep quality in adults with CMDs. The findings provide significant insights into how nurses’ pain management strategies impact the QoL in adults suffering from CMDs, with sleep acting as a partial mediator. The demographic profile indicated a predominance of middle-aged and older female adults, a trend widely documented in musculoskeletal epidemiology. According to Overstreet et al., women, particularly postmenopausal, are more vulnerable to chronic musculoskeletal conditions, such as osteoarthritis and fibromyalgia, largely due to hormonal, anatomical, and behavioral factors [15]. The chronicity and severity of their conditions, along with common comorbidities, reflect the multidimensional burden faced by this population and underscore the need for holistic nursing approaches [16].
The descriptive analysis demonstrated moderate engagement in nurse-led pain management strategies and generally poor sleep among participants. This aligns with previous research, including studies by Buonanno et al. and Balat et al., emphasizing that despite the availability of pharmacological and non-pharmacological interventions, pain in chronic musculoskeletal patients is often under-managed, leading to poor outcomes in sleep and overall life satisfaction [17, 18]. Notably, the high reliability ratings of the measurement tools confirm the robustness of the data and lend credibility to the findings.
Effective pain management by nurses was positively related to higher QoL, reinforcing the vital role nurses play in chronic pain care. This is supported by evidence from Ibrahim et al. and Malih Radhi & Zair Balat, highlighting that tailored nursing interventions, including patient education, emotional support, and self-management training, significantly improve health outcomes in chronic pain patients [19, 20]. Furthermore, better pain management was moderately associated with improved sleep, and in turn, higher sleep quality was strongly associated with better QoL. These findings are consistent with those of Herrero Babiloni et al. and Radhi et al., suggesting that sleep disturbances contribute to chronic pain, creating a cycle that exacerbates functional limitations and emotional distress [21, 22].
The mediation analysis provided nuanced insights into the mechanisms, by which nursing care affects the patient’s well-being. Sleep quality was found to partially mediate the relationship between pain management strategies and QoL, suggesting that while pain management has a direct impact, its effects are also mediated by its ability to improve sleep. This finding resonates with the biopsychosocial model of chronic pain, which posits that psychological and behavioral factors, such as sleep, play an essential role in modulating the effects of physical symptoms on QoL [21, 22]. The persistence of a significant direct effect even after accounting for sleep implies that nurses’ strategies provide multidimensional benefits beyond merely enhancing sleep—potentially by improving patient autonomy, reducing anxiety, and promoting adherence to treatment regimens [23-28].
Overall, these results underscore the importance of incorporating comprehensive, evidence-based pain management strategies within nursing care plans to address both the physical and psychosocial aspects of chronic musculoskeletal issues. The mediating role of sleep quality also highlights the value of integrating sleep-focused interventions (such as sleep hygiene education and relaxation techniques) into chronic pain management protocols. Future longitudinal research is recommended to explore causality and examine additional mediators, such as emotional regulation or social support.
This study had several limitations. Its cross-sectional design restricts the ability to establish causal relationships among pain management, sleep quality, and QoL. Self-reported measures can be subject to recall bias or response bias. Additionally, the examination was conducted in a single tertiary care facility, which may affect the generalizability of the findings to other populations or healthcare settings. Lastly, unmeasured confounding factors, such as mental distress or socioeconomic status, may have influenced the outcomes.
The study highlights that pain management techniques provided by nurses significantly impact the QoL of adults with CMDs, with restful sleep being a key factor. Participants who received better levels of pain management from nurses reported improved sleep quality and, consequently, a better sense of their QoL. These findings emphasize the critical role of effective, multidimensional pain management (which includes both pharmacological and non-pharmacological interventions) in improving health outcomes for chronic pain patients. It is recommended that healthcare institutions prioritize incorporating comprehensive pain management training into nursing practices, promote periodic assessments of sleep quality in chronic pain patients, and implement evidence-based nursing protocols tailored to individual pain patterns.
Conclusion
Effective nurse-led pain management improves the quality of life in patients with chronic musculoskeletal disorders, in part due to enhanced sleep quality.
Acknowledgments: The authors would like to thank all the participants who permitted them to interview them for their cooperation and participation.
Ethical Permissions: Ethical approval was obtained from the Research Ethics Committee of Jabir Ibn Hayyan Medical University (date: 05/02/2025, number: 372/2).
Conflicts of Interests: Nothing declared by the authors.
Authors’ Contribution: Faris HI (First Author), Introduction Writer/Main Researcher (25%); Khanjary MO (Second Author), Assistant Researcher/Discussion Writer (25%); Badr SH (Third Author), Methodologist (25%); Hussein BH (Fourth Author), Methodologist/Data Analysis (25%)
Funding/Support: The present study was not financially supported.
Chronic musculoskeletal disorders (CMDs), which include osteoarthritis, rheumatoid arthritis, and persistent lower back pain, are globally recognized as the leading causes of disability and diminished quality of life (QoL) among adults [1]. These conditions not only affect physical functioning but also contribute significantly to emotional distress, leading to issues such as depression and anxiety. Furthermore, CMDs often result in increased healthcare costs, as patients may require ongoing medical treatment, physical therapy, and pain management interventions. Musculoskeletal conditions affect more than 1.7 billion people worldwide and significantly reduce physical functioning, social participation, and psychological well-being. The widespread prevalence of these disorders highlights the urgent need for effective preventive strategies and comprehensive management plans to alleviate their impact on individuals and healthcare systems alike. Additionally, public health initiatives aimed at raising awareness about CMDs can play a crucial role in promoting early intervention and improving overall health outcomes for affected individuals. Chronic pain is a hallmark of CMDs, and its persistent nature contributes not only to physical discomfort but also to emotional distress, sleep disturbances, and prolonged periods of functional impairment [2]. Consequently, the holistic management of CMDs requires a multidimensional approach, with pain relief as a central goal [3]. This comprehensive strategy not only addresses the physical aspects of pain but also considers psychological, emotional, and social factors that contribute to a patient’s overall health. Effective pain management often involves a combination of pharmacological treatments, physical therapy, lifestyle modifications, and complementary therapies, ensuring that all dimensions of a patient’s well-being are taken into account.
Nurses play a pivotal role in managing chronic pain through various strategies, including pharmacological guidance, patient education, relaxation techniques, encouragement of physical activity, and cognitive-behavioral interventions [4]. By assessing each patient’s unique pain profile and needs, nurses can tailor their approaches to ensure optimal pain relief and support. Additionally, they provide essential education on the proper use of medications, helping patients understand potential side effects and the importance of adherence to prescribed regimens. Furthermore, nurses often facilitate access to complementary therapies, such as massage or acupuncture, which can enhance traditional pain management methods. Previous studies have shown that nurse-led pain management interventions can reduce pain intensity and improve patient-reported outcomes [5]. These interventions often include personalized care plans that address the specific needs and preferences of each patient, which can lead to more effective pain control. Additionally, nurses play a critical role in monitoring patients’ responses to treatment, allowing for timely adjustments to pain management strategies as needed. For example, a randomized controlled trial found that individualized nursing interventions for chronic arthritis patients significantly improved pain levels and daily functioning [6]. Similarly, another study emphasized the impact of nurse-delivered cognitive-behavioral techniques on reducing pain perception and enhancing emotional resilience in patients with chronic musculoskeletal conditions [7].
Importantly, sleep satisfaction has emerged as a vital mediator in the relationship between chronic pain and overall QoL. Sleep disturbances are relatively common among individuals with CMDs, largely due to the intrusive nature of persistent pain that interrupts sleep continuity and reduces sleep depth. Poor sleep has been associated with increased pain sensitivity, decreased coping ability, and diminished QoL [8]. Individuals experiencing chronic pain often struggle with sleep disturbances, which can exacerbate pain perception and lead to a vicious cycle of worsening symptoms and reduced functioning. When patients achieve better sleep satisfaction, they are more likely to report lower pain intensity and improved emotional well-being. Research has shown that effective pain management can lead to improvements in sleep, which in turn affects various dimensions of QoL [9]. When pain is adequately controlled, individuals often experience fewer disruptions during the night, allowing for deeper and more restorative sleep. This improvement in sleep quality can enhance mood, cognitive function, and overall emotional well-being, which are critical components of QoL. Additionally, better sleep can increase energy levels and motivation, enabling individuals to engage more actively in social and recreational activities. Furthermore, improved sleep can bolster the immune system, leading to better physical health and resilience against illness, thereby contributing to a more holistic sense of well-being. It has been found that improvements in sleep mediate the relationship between pain reduction and physical and emotional well-being among older adults with chronic pain [10]. Furthermore, sleep-focused nursing interventions have been shown to enhance both sleep and QoL outcomes, indicating the potential synergistic impact of integrated pain and sleep management strategies [11]. These interventions may include sleep education, relaxation techniques, and cognitive-behavioral approaches designed to improve sleep hygiene and address any underlying sleep disorders. By improving sleep quality, patients often experience reduced pain sensitivity and enhanced emotional resilience, which can further contribute to better overall health and well-being.
Despite the increasing recognition of the association between pain, sleep, and QoL, there remains a gap in knowledge regarding the mediating role of sleep quality in the impact of nurses’ pain management approaches on the QoL of adults with CMDs. This gap is particularly concerning given that CMDs are prevalent conditions that significantly diminish individuals’ overall well-being and functioning. Bridging this gap is critical for developing comprehensive, evidence-based nursing practices and improving patient-centered care. Understanding how sleep quality mediates the relationship between effective pain management and QoL can provide valuable insights into the mechanisms at play, allowing healthcare providers to tailor interventions that address both pain and sleep issues simultaneously. Therefore, this study aimed to investigate the effect of nurses’ pain management on QoL, with a focus on the mediating role of sleep quality in adults with CMDs. By exploring this relationship, the study seeks to highlight the importance of integrating sleep assessments into pain management protocols, ultimately leading to enhanced health outcomes and a better quality of life for patients facing the challenges of chronic pain. Additionally, findings from this research could inform nursing education and training, ensuring that nurses are equipped with the knowledge and skills necessary to effectively address the interconnected issues of pain, sleep, and overall well-being in their patients.
Instrument and Methods
Study design
This cross-sectional study was conducted to investigate the effect of nurses’ pain management strategies on the QoL of adults with CMDs, with sleep quality serving as a mediating factor in 2024. The study aimed to identify relationships between various parameters using standardized questionnaires to obtain quantifiable data from individuals at a single point in time. This design was chosen to assess natural variations in pain management strategies and their association with sleep quality and perceived QoL.
Study sample
The study was conducted at a specialized outpatient rehabilitation and chronic pain center affiliated with a tertiary care hospital, which receives an average of 1,800 patients with CMDs each month. The target population comprised adults aged 18 years and older who were diagnosed with chronic musculoskeletal conditions, such as osteoarthritis, chronic low back pain, fibromyalgia, or rheumatoid arthritis, and who had been under nursing care for at least three months. The sample size was calculated based on a 95% confidence level, an assumed proportion (p) of 0.30 (based on previous literature), and a 0.5 margin of error. The initial sample size was calculated using the following formula:
n₀=(Z²×p×(1-p))/d²,
n₀=(1.96²×0.30×0.70)/0.05²≈323.
Adjusting N=1,800 using the formula:
n=(n₀×N)/(n₀+N-1),
n=(323×1800)/(323+1800-1)≈280.
Hence, a final sample of 280 participants was determined to be sufficient. Participants were selected based on the inclusion criteria, including adults aged ≥18 years, clinically diagnosed with a chronic musculoskeletal disorder for a minimum of six months, receiving nursing care related to pain management, and being able to communicate effectively and provide informed consent. Exclusion criteria included patients with comorbid severe psychiatric illness, cognitive impairments that could hinder questionnaire completion, or recent hospitalization within the last month due to acute exacerbation of their musculoskeletal condition.
Study tools
The study utilized a structured questionnaire comprising four parts.
The first component collected participants’ sociodemographic and medical information, including age, gender, diagnosis, duration of the condition, medication use, and comorbidities.
The second part involved the Pain Management Inventory-Nurse Version (PMI-N), which was adapted from established pain management assessment tools to evaluate the strategies used by nurses in managing chronic musculoskeletal pain. The PMI-N measured both pharmacological and non-pharmacological interventions, including medication adherence, physical therapy recommendations, cognitive-behavioral strategies, and relaxation techniques. This inventory has been used in previous studies assessing pain management in clinical nursing contexts [12].
The third part of the questionnaire utilized the Pittsburgh Sleep Quality Index (PSQI) to assess the sleep satisfaction of participants over the past month. The PSQI includes 19 self-rated questions grouped into seven components: subjective sleep quality, sleep latency, sleep duration, overall sleep efficiency, sleep disturbances, use of sleeping medications, and daytime dysfunction. Each component yields a score ranging from zero to three, with higher global scores indicating poorer sleep. The PSQI is a well-validated and reliable tool in both clinical and research settings [13].
The fourth part employed the World Health Organization Quality of Life-Brief Version (WHOQOL-BREF), a 26-item instrument designed to measure four domains of QoL, namely physical health, psychological well-being, social relationships, and environmental health. The WHOQOL-BREF has demonstrated excellent cross-cultural validity and is frequently used in studies involving patients with chronic conditions, including musculoskeletal disorders [14].
Validity and reliability
To ensure the content validity of the tool, the complete questionnaire was reviewed by a panel of five nursing and rehabilitation experts. Modifications were made based on expert feedback to enhance readability and cultural relevance. A pilot study was conducted with 10% of the target sample (28 individuals), and data from the pilot were excluded from the final analysis. The reliability of the tools was assessed using Cronbach’s alpha; the PMI-N showed a reliability coefficient of 0.87, the PSQI 0.83, and the WHOQOL-BREF 0.89, indicating high internal consistency. All tools used have been previously validated in similar populations and are suitable for use in clinical research settings involving chronic pain and QoL assessments.
Data collection
Data were collected through direct, face-to-face interviews and the use of the standardized questionnaire. Trained research nurses conducted the interviews in designated quiet areas within the hospital to ensure privacy and minimize distractions. Each consultation lasted approximately 30-40 minutes. Before participation, verbal and written informed consent was obtained from each participant, and the study protocol was approved by the institutional review board. Participants were assured of the confidentiality and anonymity of their responses and were informed of their right to withdraw at any time without any impact on their hospital treatment.
Statistical analysis
All statistical analyses were conducted using SPSS version 26.0. Descriptive statistics, including frequencies, percentages, means, and standard deviations, were used to summarize demographic and medical characteristics. The normality of the data distribution was assessed using the Kolmogorov-Smirnov and Shapiro-Wilk tests. To explore the relationships between several primary observed variables (nurses’ pain management strategies, sleep quality, and satisfaction with QoL), Pearson’s correlation coefficients were computed. Mediation analysis was conducted using the PROCESS macro for SPSS (Model 4) to test the indirect effect of pain management strategies on QoL through sleep. A bootstrapping method with 5,000 samples was employed to determine the significance of the indirect effect, and a p-value <0.05 was considered statistically significant during the analysis.
Findings
A total of 280 participants were enrolled, who had a mean age of 52.4±11.6 years, with a higher percentage being female (63.6%). Diagnostically, participants were primarily affected by chronic low back pain (32.5%) and osteoarthritis (30.4%), followed by fibromyalgia (21.1%) and rheumatoid arthritis (60%). On average, participants had been living with their musculoskeletal condition for over three years (38.5±19.2 months). About 75% had used pain medications, and nearly half had additional comorbidities, indicating a clinically complex population with multifactorial health burdens (Table 1).
Table 1. Frequency of sociodemographic and clinical characteristics of participants (n=280)
Participants reported mild exposure to nurse-led pain management strategies, generally poor sleep quality, and a relatively high perceived QoL (Table 2).
Table 2. Descriptive statistics of main study parameters
There was a statistically significant correlation between nurses’ pain management strategies and participants’ QoL (r=0.53, p<0.01), suggesting that more effective nursing interventions are associated with better perceived well-being. A moderate negative correlation was found between pain management and sleep quality (r=-0.46, p<0.01), indicating that higher levels of pain management are associated with improved sleep (lower PSQI scores). Sleep quality was also negatively correlated with QoL (r=-0.58, p<0.01), indicating that poor sleep was significantly associated with decreased satisfaction with QoL (Table 3).
Table 3. Pearson’s correlation matrix among key study parameters
The direct path from pain management to sleep quality (path a) was significantly negative, indicating that improved pain management decreased sleep disturbances. The path from sleep quality to QoL (path b) was also significantly negative, showing that poorer sleep was associated with a lower QoL. The indirect effect (ab=0.23) was statistically significant, as the 95% confidence interval did not include 0, confirming that sleep quality partially mediates the relationship. Additionally, the direct effect (c’) remained significant, indicating partial rather than full mediation (Table 4).
Table 4. Mediation analysis using PROCESS Macro (Model 4)
Discussion
This study aimed to investigate the effect of nurses’ pain management on QoL, with a focus on the mediating role of sleep quality in adults with CMDs. The findings provide significant insights into how nurses’ pain management strategies impact the QoL in adults suffering from CMDs, with sleep acting as a partial mediator. The demographic profile indicated a predominance of middle-aged and older female adults, a trend widely documented in musculoskeletal epidemiology. According to Overstreet et al., women, particularly postmenopausal, are more vulnerable to chronic musculoskeletal conditions, such as osteoarthritis and fibromyalgia, largely due to hormonal, anatomical, and behavioral factors [15]. The chronicity and severity of their conditions, along with common comorbidities, reflect the multidimensional burden faced by this population and underscore the need for holistic nursing approaches [16].
The descriptive analysis demonstrated moderate engagement in nurse-led pain management strategies and generally poor sleep among participants. This aligns with previous research, including studies by Buonanno et al. and Balat et al., emphasizing that despite the availability of pharmacological and non-pharmacological interventions, pain in chronic musculoskeletal patients is often under-managed, leading to poor outcomes in sleep and overall life satisfaction [17, 18]. Notably, the high reliability ratings of the measurement tools confirm the robustness of the data and lend credibility to the findings.
Effective pain management by nurses was positively related to higher QoL, reinforcing the vital role nurses play in chronic pain care. This is supported by evidence from Ibrahim et al. and Malih Radhi & Zair Balat, highlighting that tailored nursing interventions, including patient education, emotional support, and self-management training, significantly improve health outcomes in chronic pain patients [19, 20]. Furthermore, better pain management was moderately associated with improved sleep, and in turn, higher sleep quality was strongly associated with better QoL. These findings are consistent with those of Herrero Babiloni et al. and Radhi et al., suggesting that sleep disturbances contribute to chronic pain, creating a cycle that exacerbates functional limitations and emotional distress [21, 22].
The mediation analysis provided nuanced insights into the mechanisms, by which nursing care affects the patient’s well-being. Sleep quality was found to partially mediate the relationship between pain management strategies and QoL, suggesting that while pain management has a direct impact, its effects are also mediated by its ability to improve sleep. This finding resonates with the biopsychosocial model of chronic pain, which posits that psychological and behavioral factors, such as sleep, play an essential role in modulating the effects of physical symptoms on QoL [21, 22]. The persistence of a significant direct effect even after accounting for sleep implies that nurses’ strategies provide multidimensional benefits beyond merely enhancing sleep—potentially by improving patient autonomy, reducing anxiety, and promoting adherence to treatment regimens [23-28].
Overall, these results underscore the importance of incorporating comprehensive, evidence-based pain management strategies within nursing care plans to address both the physical and psychosocial aspects of chronic musculoskeletal issues. The mediating role of sleep quality also highlights the value of integrating sleep-focused interventions (such as sleep hygiene education and relaxation techniques) into chronic pain management protocols. Future longitudinal research is recommended to explore causality and examine additional mediators, such as emotional regulation or social support.
This study had several limitations. Its cross-sectional design restricts the ability to establish causal relationships among pain management, sleep quality, and QoL. Self-reported measures can be subject to recall bias or response bias. Additionally, the examination was conducted in a single tertiary care facility, which may affect the generalizability of the findings to other populations or healthcare settings. Lastly, unmeasured confounding factors, such as mental distress or socioeconomic status, may have influenced the outcomes.
The study highlights that pain management techniques provided by nurses significantly impact the QoL of adults with CMDs, with restful sleep being a key factor. Participants who received better levels of pain management from nurses reported improved sleep quality and, consequently, a better sense of their QoL. These findings emphasize the critical role of effective, multidimensional pain management (which includes both pharmacological and non-pharmacological interventions) in improving health outcomes for chronic pain patients. It is recommended that healthcare institutions prioritize incorporating comprehensive pain management training into nursing practices, promote periodic assessments of sleep quality in chronic pain patients, and implement evidence-based nursing protocols tailored to individual pain patterns.
Conclusion
Effective nurse-led pain management improves the quality of life in patients with chronic musculoskeletal disorders, in part due to enhanced sleep quality.
Acknowledgments: The authors would like to thank all the participants who permitted them to interview them for their cooperation and participation.
Ethical Permissions: Ethical approval was obtained from the Research Ethics Committee of Jabir Ibn Hayyan Medical University (date: 05/02/2025, number: 372/2).
Conflicts of Interests: Nothing declared by the authors.
Authors’ Contribution: Faris HI (First Author), Introduction Writer/Main Researcher (25%); Khanjary MO (Second Author), Assistant Researcher/Discussion Writer (25%); Badr SH (Third Author), Methodologist (25%); Hussein BH (Fourth Author), Methodologist/Data Analysis (25%)
Funding/Support: The present study was not financially supported.
Keywords:
References
1. Tushingham S, Cottle J, Adesokan M, Ogwumike OO, Ojagbemi A, Stubbs B, et al. The prevalence and pattern of comorbid long-term conditions with low back pain and osteoarthritis in low-and middle-income countries: A systematic review and meta-analysis. Int J Health Promot Educ. 2024;1:1-25. [Link] [DOI:10.1080/14635240.2024.2332911]
2. Chen N, Fong DY, Wong JY. Health and economic outcomes associated with musculoskeletal disorders attributable to high body mass index in 192 countries and territories in 2019. JAMA Netw Open. 2023;6(1):e2250674. [Link] [DOI:10.1001/jamanetworkopen.2022.50674]
3. Alwatify SS, Radhi MM. Diabetes self-management and its association with medication adherence in diabetic patients. Iran J War Public Health. 2025;17(1):17-22. [Link]
4. Alruwaili MO, Alruwaili FO, Mohammed SH, Alruwaili H, Alanazi AM, Alruwaili AR. Pain management in nursing care: Effective strategies and techniques. Gland Surg. 2024;9(2):316-23. [Link]
5. Faris HI, Badr SH, Hussein BH. Independence level as a mediators between physical activity and activities of daily living in lower limb amputation. Iran Rehabil J. 2025;23(1):77-86. [Link] [DOI:10.32598/irj.23.1.1989.2]
6. Al-Eqabi QA, Niazy SM, Radhi MM. Effectiveness of digital health interventions in managing glycated haemoglobin: A randomized controlled trial. Natl J Community Med. 2024;15(9):747-53. [Link] [DOI:10.55489/njcm.150920244442]
7. Al-Eqabi QA, Niazy SM, Radhi MM. Amputation-related factors influencing activities of daily living among amputees. Iran J War Public Health. 2024;16(2):123-9. [Link]
8. Jain SV, Panjeton GD, Martins YC. Relationship between sleep disturbances and chronic pain: A narrative review. Clin Pract. 2024;14(6):2650-60. [Link] [DOI:10.3390/clinpract14060209]
9. Skúladóttir H, Sveinsdottir H, Holden JE, Gunnarsdóttir TJ, Halldorsdottir S, Björnsdottir A. Pain, sleep, and health-related quality of life after multidisciplinary intervention for chronic pain. Int J Environ Res Public Health. 2021;18(19):10233. [Link] [DOI:10.3390/ijerph181910233]
10. Elywy GJ, Radhi MM, AlEqabi QA. Relationship between social support and self-hardiness among breast cancer women in Nasiriyah, Iraq. J Pak Med Assoc. 2023;73(9):S9-14. [Link] [DOI:10.47391/JPMA.IQ-02]
11. Radhi MM, Al-Eqabi QA, Hindi NK. Rehabilitation problems of people with motor disabilities at Babylon center for rehabilitation of the disabled. Med J Babylon. 2023;20(4):838-43. [Link] [DOI:10.4103/MJBL.MJBL_674_23]
12. Watt‐Watson J, Stevens B, Garfinkel P, Streiner D, Gallop R. Relationship between nurses' pain knowledge and pain management outcomes for their postoperative cardiac patients. J Adv Nurs. 2001;36(4):535-45. [Link] [DOI:10.1046/j.1365-2648.2001.02006.x]
13. Buysse DJ, Reynolds III CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193-213. [Link] [DOI:10.1016/0165-1781(89)90047-4]
14. WHOQOL Group. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol Med. 1998;28(3):551-8. [Link] [DOI:10.1017/S0033291798006667]
15. Overstreet DS, Strath LJ, Jordan M, Jordan IA, Hobson JM, Owens MA, et al. A brief overview: Sex differences in prevalent chronic musculoskeletal conditions. Int J Environ Res Public Health. 2023;20(5):4521. [Link] [DOI:10.3390/ijerph20054521]
16. Malih Radhi M, Elywy GJ, Khyoosh Al-Eqabi QA. Burdens among wives of disabled people in the light of some social variables. Iran Rehabil J. 2023;21(3):473-84. [Link] [DOI:10.32598/irj.21.3.1765.3]
17. Buonanno P, Marra A, Iacovazzo C, Vargas M, Nappi S, Squillacioti F, et al. The PATIENT approach: A new bundle for the management of chronic pain. J Pers Med. 2023;13(11):1551. [Link] [DOI:10.3390/jpm13111551]
18. Balat KZ, Laftah SA, Radhi M. The relationship between psychological distress and quality of life among women undergoing mastectomy in Iraq: A descriptive correlational study. Natl J Community Med. 2025;16(1):20-7. [Link] [DOI:10.55489/njcm.160120254716]
19. Ibrahim AM, Gano FA, Abdel-Aziz HR, Elneblawi NH, Zaghamir DE, Negm LM, et al. Tailoring nursing interventions to empower patients: Personal coping strategies and self-management in type 2 diabetes care. BMC Nurs. 2024;23(1):926. [Link] [DOI:10.1186/s12912-024-02573-w]
20. Malih Radhi M, Zair Balat K. Health literacy and its association with medication adherence in patients with hypertension: A mediating role of social support. Iran Rehabil J. 2024;22(1):117-28. [Link] [DOI:10.32598/irj.22.1.1989.1]
21. Herrero Babiloni A, De Koninck BP, Beetz G, De Beaumont L, Martel MO, Lavigne GJ. Sleep and pain: Recent insights, mechanisms, and future directions in the investigation of this relationship. J Neural Transm. 2020;127(4):647-60. [Link] [DOI:10.1007/s00702-019-02067-z]
22. Radhi MM, Niazy SM, Abed SN. Individual-related factors associated with treatment adherence among hypertensive patients. J Public Health Afr. 2023;14(6):2466. [Link] [DOI:10.4081/jphia.2023.2466]
23. De Sonis AM. Combining modern pharmacology with integrative medicine: A biopsychosocial model for comprehensive pain care. In: Pain management-from acute to chronic and beyond. London: IntechOpen; 2023. [Link]
24. Nijs J, Mairesse O, Tang NK. The importance of sleep in the paradigm shift from a tissue-and disease-based pain management approach towards multimodal lifestyle interventions for chronic pain. Braz J Phys Ther. 2024;28(1):100594. [Link] [DOI:10.1016/j.bjpt.2024.100594]
25. Elywy GJ, Radhi MM, Khyoosh Al-Eqabi QA. Social support and its association with the quality of life (QoL) of amputees. Iran Rehabil J. 2022;20(2):253-60. [Link] [DOI:10.32598/irj.20.2.1784.1]
26. Radhi MM. Degree of disease acceptance and health seeking behaviors for type 2 diabetic patients at diabetic center in Hilla City. Medico Leg Update. 2020;20(2):853-8. [Link] [DOI:10.37506/mlu.v20i2.1347]
27. Yasir AA, Qassim WJ, Radhi MM. Assessment the feeling of psychological loneliness among wives of martyrs in the light of some social variables in Babylon Governorate/Iraq. J Pharm Sci Res. 2018;10(1):40-4. [Link]
28. Qassim WJ, Yasir AA, Radhi MM. Assessment of self hardness and its relationship to treatment acceptance for patients with diabetes mellitus at diabetic center in Hilla City/Iraq. J Pharm Sci Res. 2018;10(1):142-5. [Link]