Volume 17, Issue 1 (2025)
Iran J War Public Health 2025, 17(1): 37-42 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2025/01/29 | Accepted: 2025/02/28 | Published: 2025/03/2
Received: 2025/01/29 | Accepted: 2025/02/28 | Published: 2025/03/2
How to cite this article
Muhalla H, Nursalam N, Yusuf A, Bakar A, Kurniawati N, Wahyudi A et al . Effectiveness of a Health Education Program in Managing Diabetes Mellitus and Preventing Renal Complications. Iran J War Public Health 2025; 17 (1) :37-42
URL: http://ijwph.ir/article-1-1548-en.html
URL: http://ijwph.ir/article-1-1548-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Authors
H.I. Muhalla *1, N. Nursalam2, A. Yusuf2, A. Bakar2, N.D. Kurniawati2, A.S. Wahyudi2, A. Ma'ruf3
1- Nursing Doctoral Program, Faculty of Nursing, Airlangga University, Surabaya, Indonesia
2- Department of Advanced Nursing, Faculty of Nursing, Airlangga University, Surabaya, Indonesia
3- Department of Veterinary Medicine, Faculty of Veterinary Medicine, Airlangga University, Surabaya, Indonesia
2- Department of Advanced Nursing, Faculty of Nursing, Airlangga University, Surabaya, Indonesia
3- Department of Veterinary Medicine, Faculty of Veterinary Medicine, Airlangga University, Surabaya, Indonesia
Full-Text (HTML) (374 Views)
Introduction
Diabetes Mellitus (DM) is a chronic disease whose prevalence continues to rise worldwide, especially in Indonesia [1]. According to 2022 International Diabetes Federation (IDF) data, more than 537 million people have diabetes, which is anticipated to rise to 643 million by 2030 [2]. Kind 2 diabetes mellitus, the most common kind of diabetes, is frequently connected with an unhealthy lifestyle, such as an imbalanced diet, lack of physical activity, and obesity [3]. If not appropriately managed, DM can cause various serious complications, one of which is kidney complications (diabetic nephropathy) [4]. Diabetic nephropathy is the major cause of chronic kidney failure that needs kidney replacement therapy, such as dialysis or kidney transplantation [5]. Therefore, DM prevention and management significantly reduce the health burden and medical costs [6].
Health education is an effective intervention in managing Diabetes Mellitus and preventing complications [7]. Health education programs aim to increase patients' knowledge, skills, and motivation in managing their disease. However, the success of health education programs is highly dependent on the readiness and motivation of individuals to adopt healthy behaviors [8]. In this regard, the Transtheoretical Model (TTM), created by Prochaska and DiClemente in 1983, is a helpful theoretical framework for understanding the behavior change process in DM patients [9]. TTM identifies five stages for behavior change: Pre-contemplation, contemplation, preparation, action, and maintenance [10]. Each step necessitates distinct health education tactics and strategies to ease the transition to the next stage [11].
According to TTM, evidence of the success of a health education program can be found in the participants' progression through the stages of behavior modification [12]. For example, in the pre-contemplation stage, patients may not realize the importance of managing diabetes to prevent kidney complications [13]. Next, in the preparation stage, patients begin to plan changes, such as adjusting their diet or starting light exercise [14, 15]. The implementation of healthy behavior characterizes the action stage, while the maintenance stage involves efforts to maintain the behavior in the long term [16].
Previous research has shown that TTM-based health education programs effectively facilitate behavior change in DM patients. For example, research by Settineri et al. [17] found that interventions tailored to the stages of behavior change can improve patient compliance in managing diabetes. Another study [18] showed that a health education program integrating TTM successfully increased patient knowledge and skills in controlling blood sugar levels. In addition, research by Selçuk-Tosun & Zincir [19] found that a TTM-based approach effectively increased physical activity and healthy eating patterns in DM patients. TTM believes that the advancement of participants through the stages of behavior modification demonstrates the success of a health education program.
However, despite the evidence demonstrating the effectiveness of health education programs, their implementation still has challenges. One of the main challenges is patients' lack of awareness and motivation to change their behavior. According to Bandura, motivation and self-confidence (self-efficacy) are key factors in successful behavior change. Therefore, health education programs must be designed to increase patient self-efficacy to manage their disease independently.
This research aimed to examine the impact of health education initiatives in managing Diabetes Mellitus to prevent kidney complications using indicators based on the Transtheoretical Model. Some of the indicators that were measured included changes in behavioral stages (from pre-contemplation to maintenance), increased knowledge about diabetes and its prevention, adoption of healthy behaviors such as a balanced diet, frequent physical activity, and medication adherence, better glycemic control to minimize the risk of diabetic nephropathy, and patient quality of life, demonstrating the program's efficacy in improving physical and emotional well-being. Using the TTM approach, this research provided a comprehensive picture of how the Health Education program for Managing Diabetes Mellitus helped prevent kidney complications, minimizing the associated risks. It is also hoped that the results of this research can serve as a reference for health workers in designing more effective educational programs based on patient needs.
Materials and Methods
This analytic study was conducted from September to November 2024 among diabetes mellitus patients. The sample was determined using area or cluster sampling procedures, randomly assigning groups rather than individuals [20-24]. The sample size was determined through statistical power analysis using G*Power with a significance level (α=0.05), statistical power (1-β=0.8), and effect size (Cohen's f²), as well as the 10-fold rule to ensure sample adequacy. One hundred twenty samples were selected by a simple random sampling method.
Data collection was conducted using a questionnaire consisting of closed questions with a Likert scale, multiple-choice questions, and open questions.
This questionnaire was pre-tested in a pilot study to ensure its reliability and applicability for this research. Validity and reliability tests were conducted with Average Variance Extracted for convergent validity and Fornell-Larcker Criterion and Heterotrait-Monotrait Ratio (HTMT) for discriminant validity. Reliability was tested through Cronbach's Alpha and Composite Reliability.
This study used SEM-PLS software [25-28] to analyze the relationship between variables and test the effectiveness of health education programs in managing Diabetes Mellitus and preventing kidney complications.
Findings
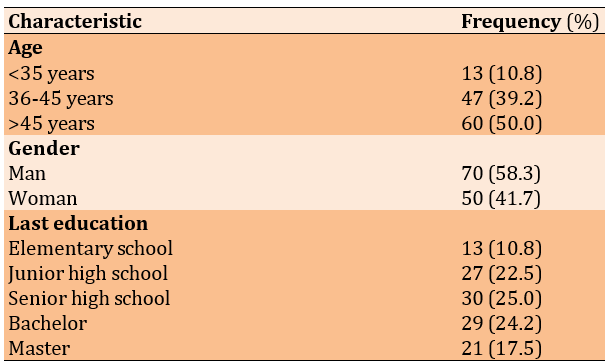
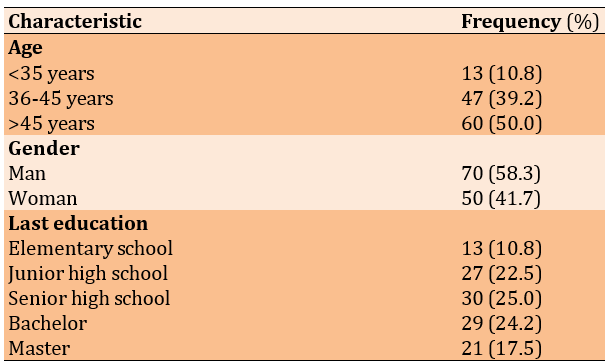
Most respondents were male and over 45 years old (Table 1).
Table 1. Demographic characteristics of diabetes mellitus patients
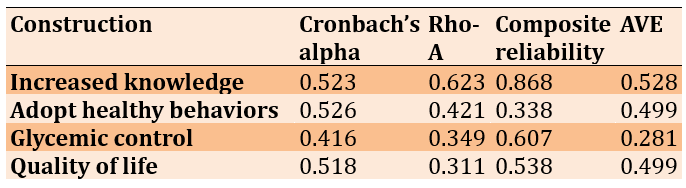
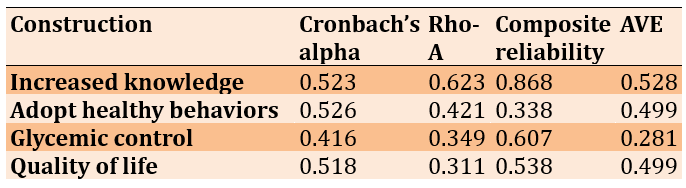
Some constructs, such as increased knowledge, showed adequate reliability and validity, with good levels of internal consistency. However, other constructs, such as health behaviors, glycemic control, and quality of life, showed low levels of reliability (Table 2).
Table 2. The composite reliability, rho-A, Cronbach’s alpha, and average variance extracted (AVE) of parameters
Regression results have shown the effectiveness of health education programs in managing diabetes mellitus to prevent kidney complications (R2=0.945; R2 adjusted=0.927).
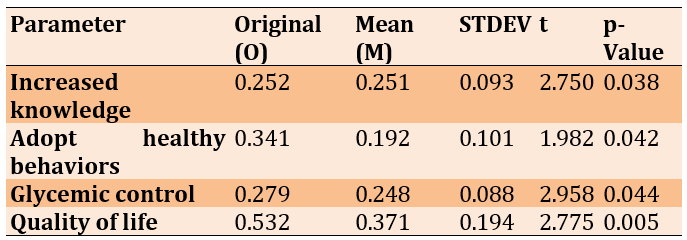
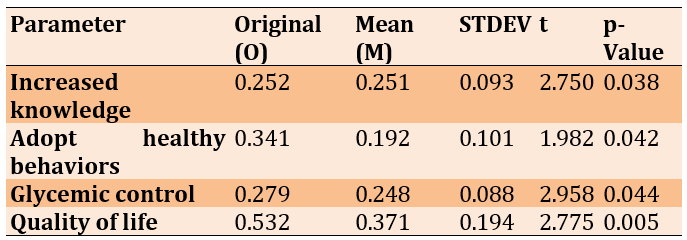
Using the SEM-PLS bootstrapping method showed that all factors significantly influenced the effectiveness of health education programs in managing diabetes mellitus and preventing kidney complications. Increased knowledge, adoption of healthy behaviors, glycemic control, and improved quality of life all contribute significantly to program success. Increased knowledge was shown to improve program effectiveness (p=0.038), followed by the adoption of healthy behaviors (p=0.042) and glycemic control (p=0.044), which also showed significant results. Lastly, improved quality of life was closely related to program success (p=0.005; Table 3).
Table 3. The results of SEM-PLS bootstrapping method
Discussion
Based on the data presented, the health education program effectively increases participants' knowledge regarding managing diabetes mellitus to prevent kidney complications. This can be seen from the p-value of 0.038 (<0.05), which shows that the increase in participants' knowledge is statistically significant. The t-statistics value of 2.750 also indicates that the difference between the original sample and the sample mean is substantial, so the hypothesis is accepted. An increase in knowledge of 0.252 from the initial scale shows that this program has succeeded in providing patients with a better understanding of the importance of increasing DM knowledge to prevent kidney complications. Alrasheeday et al. [29] state that a structured diabetes education program can improve patients' knowledge and skills in managing their disease, thereby reducing the risk of complications such as diabetic nephropathy.
Based on the data presented, health education programs have been proven effective in increasing the adoption of healthy behaviors in diabetes mellitus patients. This is an essential step in preventing kidney complications. The p-value of 0.042 (<0.05) indicates that the increase in the adoption of healthy behavior is statistically significant. Apart from that, the t-statistics value of 1.982 indicates that the difference between the original sample and the sample mean is quite substantial, so the hypothesis is accepted. An increase in healthy behavior adoption of 0.341 from the initial scale shows that this program has encouraged positive behavioral changes in participants, such as healthy eating patterns, regular physical activity, and medication adherence.
Narva et al. [30] support these findings, which state that structured health education interventions can increase the adoption of healthy behavior in DM patients, ultimately reducing the risk of complications such as diabetic nephropathy. This research emphasizes the importance of a sustainable educational approach to sustaining long-term behavior change. In addition, a meta-analysis by Alrasheeday et al. [29] found that health education programs involving social support and a personalized approach can improve patient compliance with diabetes self-management, including diet and physical activity regulation. This is in line with research findings by the American Diabetes Association (ADA) in 2022, which stated that changes in healthy behavior are a key factor in preventing chronic complications of diabetes, including kidney disease [2]. Furthermore, Narva et al. [30] show that health education interventions focusing on preventing kidney complications in DM patients can increase awareness and adoption of healthy behaviors, such as reducing salt intake, controlling blood pressure, and monitoring blood sugar levels regularly. These findings reinforce the importance of health education programs as an integral part of diabetes management.
Thus, it can be concluded that health education programs not only increase knowledge but also encourage the adoption of healthy behavior in diabetes mellitus patients, which ultimately can prevent kidney complications. To improve the health outcomes of DM patients, widespread and sustainable implementation of similar programs is recommended.
Based on the data presented, health education programs are proven effective in improving glycemic control in diabetes mellitus patients, a key factor in preventing kidney complications. The p-value of 0.044 (<0.05) indicates that the improvement in glycemic control is statistically significant. Apart from that, the t-statistics value of 2.958 indicates that the difference between the original sample and the sample mean is quite substantial, so the hypothesis is accepted. An improvement in glycemic control of 0.279 from the initial scale shows that this program is successful in helping participants manage their blood sugar levels, which in turn can reduce the risk of complications such as diabetic nephropathy.
Teshome & Yitayeh [31] support these findings and state that structured health education interventions can improve glycemic control in DM patients through increasing self-management, including monitoring blood sugar levels, managing diet, and compliance with treatment. This study emphasizes that reasonable glycemic control is a significant protective factor against developing renal complications. In addition, a meta-analysis by Rodríguez-Gutiérrez & Montori [32] found that health education programs involving an individualized approach and ongoing support can significantly improve glycemic control in DM patients. This study also shows that maintaining optimum glycemic management can lower the risk of microvascular consequences, including kidney injury. These conclusions are supported by recent studies from American Diabetes [2]; health education programs focusing on diabetes self-management can improve glucose control and prevent long-term consequences, including kidney failure.
Thus, it is possible to conclude that health education programs promote awareness and adoption of healthy behavior while improving glycemic control in diabetes mellitus patients. This is critical for reducing kidney problems and enhancing the patient's quality of life. For improved health results, it is recommended that such programs be implemented widely and sustainably.
Based on the data presented, health education programs have been shown to improve the quality of life of diabetic mellitus patients, which is an important indicator in disease management and the avoidance of renal problems. The p-value of 0.005 (<0.05) indicates that the improvement in quality of life is statistically significant. Apart from that, the t-statistics value of 2.775 indicates that the difference between the original sample and the sample mean is quite substantial, so the hypothesis is accepted. An increase in quality of life of 0.532 from the initial scale shows that this program has positively impacted the patient's physical, mental, and social aspects, which in turn can reduce the risk of complications such as diabetic nephropathy.
A meta-analysis by Alshahrani et al. [33] discovered that health education programs that take a holistic approach, including emotional support and teaching about healthy lifestyles, can dramatically improve the quality of life of DM patients. This study also found that improving quality of life can lower psychological loads and boost patient motivation to treat their disease more effectively. Additionally, Alshayban & Joseph [34] found that health education programs that promote quality of life can reduce the risk of microvascular consequences, including kidney injury, in DM patients.
Thus, it is possible to infer that health education programs not only raise knowledge, adopt healthy behaviors, and improve glycemic control, but also considerably improve the quality of life of diabetes mellitus patients. This is critical in avoiding kidney issues and increasing the patient's well-being. For improved health results, it is recommended that such programs be implemented widely and sustainably.
Practical recommendations for health educators and policymakers include developing and implementing health education programs that are more inclusive and tailored to individual needs, especially for younger age groups and those with lower levels of education. Health educators could consider more interactive and technology-based approaches to improve patient understanding. Policymakers should also support programs that involve cross-sector collaboration, including medical personnel, nutritionists, and psychologists, to strengthen the effectiveness of health education programs. In addition, further research needs to be conducted with more diverse samples and more accurate measurements to evaluate the long-term impact of these health education programs.
Conclusion
Increased knowledge, adoption of healthy behaviors, glycemic control, and quality of life positively influence the effectiveness of the transtheoretical model health education program.
Acknowledgments: The author would like to thank all parties who have supported and contributed to this research, including institutions, fellow researchers, and respondents who have participated.
Ethical Permissions: This study has obtained ethical approval from the Research Ethics Committee of the Faculty of Nursing Health, Airlangga University, Surabaya, Indonesia (NR.011.02/F.XXXII.25/09/2024).
Conflicts of Interests: The authors declare no conflict of interest in this research. The study was conducted objectively and independently, without influence from personal or external interests.
Authors' Contribution: Muhalla HI (First Author), Introduction Writer (15%); Nursalam N (Second Author), Methodologist (15%); Yusuf A (Third Author), Main Researcher (20%); Bakar A (Fourth Author), Discussion Writer (15%); Kurniawati ND (Fifth Author), Statistical Analyst (15%); Wahyudi AS (Sixth Author), Assistant Researcher (10%); Ma'ruf A (Seventh Author), Assistant Researcher (10%)
Funding/Support: This research was supported by the Faculty of Nursing, Airlangga University, Surabaya, Indonesia.
Diabetes Mellitus (DM) is a chronic disease whose prevalence continues to rise worldwide, especially in Indonesia [1]. According to 2022 International Diabetes Federation (IDF) data, more than 537 million people have diabetes, which is anticipated to rise to 643 million by 2030 [2]. Kind 2 diabetes mellitus, the most common kind of diabetes, is frequently connected with an unhealthy lifestyle, such as an imbalanced diet, lack of physical activity, and obesity [3]. If not appropriately managed, DM can cause various serious complications, one of which is kidney complications (diabetic nephropathy) [4]. Diabetic nephropathy is the major cause of chronic kidney failure that needs kidney replacement therapy, such as dialysis or kidney transplantation [5]. Therefore, DM prevention and management significantly reduce the health burden and medical costs [6].
Health education is an effective intervention in managing Diabetes Mellitus and preventing complications [7]. Health education programs aim to increase patients' knowledge, skills, and motivation in managing their disease. However, the success of health education programs is highly dependent on the readiness and motivation of individuals to adopt healthy behaviors [8]. In this regard, the Transtheoretical Model (TTM), created by Prochaska and DiClemente in 1983, is a helpful theoretical framework for understanding the behavior change process in DM patients [9]. TTM identifies five stages for behavior change: Pre-contemplation, contemplation, preparation, action, and maintenance [10]. Each step necessitates distinct health education tactics and strategies to ease the transition to the next stage [11].
According to TTM, evidence of the success of a health education program can be found in the participants' progression through the stages of behavior modification [12]. For example, in the pre-contemplation stage, patients may not realize the importance of managing diabetes to prevent kidney complications [13]. Next, in the preparation stage, patients begin to plan changes, such as adjusting their diet or starting light exercise [14, 15]. The implementation of healthy behavior characterizes the action stage, while the maintenance stage involves efforts to maintain the behavior in the long term [16].
Previous research has shown that TTM-based health education programs effectively facilitate behavior change in DM patients. For example, research by Settineri et al. [17] found that interventions tailored to the stages of behavior change can improve patient compliance in managing diabetes. Another study [18] showed that a health education program integrating TTM successfully increased patient knowledge and skills in controlling blood sugar levels. In addition, research by Selçuk-Tosun & Zincir [19] found that a TTM-based approach effectively increased physical activity and healthy eating patterns in DM patients. TTM believes that the advancement of participants through the stages of behavior modification demonstrates the success of a health education program.
However, despite the evidence demonstrating the effectiveness of health education programs, their implementation still has challenges. One of the main challenges is patients' lack of awareness and motivation to change their behavior. According to Bandura, motivation and self-confidence (self-efficacy) are key factors in successful behavior change. Therefore, health education programs must be designed to increase patient self-efficacy to manage their disease independently.
This research aimed to examine the impact of health education initiatives in managing Diabetes Mellitus to prevent kidney complications using indicators based on the Transtheoretical Model. Some of the indicators that were measured included changes in behavioral stages (from pre-contemplation to maintenance), increased knowledge about diabetes and its prevention, adoption of healthy behaviors such as a balanced diet, frequent physical activity, and medication adherence, better glycemic control to minimize the risk of diabetic nephropathy, and patient quality of life, demonstrating the program's efficacy in improving physical and emotional well-being. Using the TTM approach, this research provided a comprehensive picture of how the Health Education program for Managing Diabetes Mellitus helped prevent kidney complications, minimizing the associated risks. It is also hoped that the results of this research can serve as a reference for health workers in designing more effective educational programs based on patient needs.
Materials and Methods
This analytic study was conducted from September to November 2024 among diabetes mellitus patients. The sample was determined using area or cluster sampling procedures, randomly assigning groups rather than individuals [20-24]. The sample size was determined through statistical power analysis using G*Power with a significance level (α=0.05), statistical power (1-β=0.8), and effect size (Cohen's f²), as well as the 10-fold rule to ensure sample adequacy. One hundred twenty samples were selected by a simple random sampling method.
Data collection was conducted using a questionnaire consisting of closed questions with a Likert scale, multiple-choice questions, and open questions.
This questionnaire was pre-tested in a pilot study to ensure its reliability and applicability for this research. Validity and reliability tests were conducted with Average Variance Extracted for convergent validity and Fornell-Larcker Criterion and Heterotrait-Monotrait Ratio (HTMT) for discriminant validity. Reliability was tested through Cronbach's Alpha and Composite Reliability.
This study used SEM-PLS software [25-28] to analyze the relationship between variables and test the effectiveness of health education programs in managing Diabetes Mellitus and preventing kidney complications.
Findings
Most respondents were male and over 45 years old (Table 1).
Table 1. Demographic characteristics of diabetes mellitus patients
Some constructs, such as increased knowledge, showed adequate reliability and validity, with good levels of internal consistency. However, other constructs, such as health behaviors, glycemic control, and quality of life, showed low levels of reliability (Table 2).
Table 2. The composite reliability, rho-A, Cronbach’s alpha, and average variance extracted (AVE) of parameters
Regression results have shown the effectiveness of health education programs in managing diabetes mellitus to prevent kidney complications (R2=0.945; R2 adjusted=0.927).
Using the SEM-PLS bootstrapping method showed that all factors significantly influenced the effectiveness of health education programs in managing diabetes mellitus and preventing kidney complications. Increased knowledge, adoption of healthy behaviors, glycemic control, and improved quality of life all contribute significantly to program success. Increased knowledge was shown to improve program effectiveness (p=0.038), followed by the adoption of healthy behaviors (p=0.042) and glycemic control (p=0.044), which also showed significant results. Lastly, improved quality of life was closely related to program success (p=0.005; Table 3).
Table 3. The results of SEM-PLS bootstrapping method
Discussion
Based on the data presented, the health education program effectively increases participants' knowledge regarding managing diabetes mellitus to prevent kidney complications. This can be seen from the p-value of 0.038 (<0.05), which shows that the increase in participants' knowledge is statistically significant. The t-statistics value of 2.750 also indicates that the difference between the original sample and the sample mean is substantial, so the hypothesis is accepted. An increase in knowledge of 0.252 from the initial scale shows that this program has succeeded in providing patients with a better understanding of the importance of increasing DM knowledge to prevent kidney complications. Alrasheeday et al. [29] state that a structured diabetes education program can improve patients' knowledge and skills in managing their disease, thereby reducing the risk of complications such as diabetic nephropathy.
Based on the data presented, health education programs have been proven effective in increasing the adoption of healthy behaviors in diabetes mellitus patients. This is an essential step in preventing kidney complications. The p-value of 0.042 (<0.05) indicates that the increase in the adoption of healthy behavior is statistically significant. Apart from that, the t-statistics value of 1.982 indicates that the difference between the original sample and the sample mean is quite substantial, so the hypothesis is accepted. An increase in healthy behavior adoption of 0.341 from the initial scale shows that this program has encouraged positive behavioral changes in participants, such as healthy eating patterns, regular physical activity, and medication adherence.
Narva et al. [30] support these findings, which state that structured health education interventions can increase the adoption of healthy behavior in DM patients, ultimately reducing the risk of complications such as diabetic nephropathy. This research emphasizes the importance of a sustainable educational approach to sustaining long-term behavior change. In addition, a meta-analysis by Alrasheeday et al. [29] found that health education programs involving social support and a personalized approach can improve patient compliance with diabetes self-management, including diet and physical activity regulation. This is in line with research findings by the American Diabetes Association (ADA) in 2022, which stated that changes in healthy behavior are a key factor in preventing chronic complications of diabetes, including kidney disease [2]. Furthermore, Narva et al. [30] show that health education interventions focusing on preventing kidney complications in DM patients can increase awareness and adoption of healthy behaviors, such as reducing salt intake, controlling blood pressure, and monitoring blood sugar levels regularly. These findings reinforce the importance of health education programs as an integral part of diabetes management.
Thus, it can be concluded that health education programs not only increase knowledge but also encourage the adoption of healthy behavior in diabetes mellitus patients, which ultimately can prevent kidney complications. To improve the health outcomes of DM patients, widespread and sustainable implementation of similar programs is recommended.
Based on the data presented, health education programs are proven effective in improving glycemic control in diabetes mellitus patients, a key factor in preventing kidney complications. The p-value of 0.044 (<0.05) indicates that the improvement in glycemic control is statistically significant. Apart from that, the t-statistics value of 2.958 indicates that the difference between the original sample and the sample mean is quite substantial, so the hypothesis is accepted. An improvement in glycemic control of 0.279 from the initial scale shows that this program is successful in helping participants manage their blood sugar levels, which in turn can reduce the risk of complications such as diabetic nephropathy.
Teshome & Yitayeh [31] support these findings and state that structured health education interventions can improve glycemic control in DM patients through increasing self-management, including monitoring blood sugar levels, managing diet, and compliance with treatment. This study emphasizes that reasonable glycemic control is a significant protective factor against developing renal complications. In addition, a meta-analysis by Rodríguez-Gutiérrez & Montori [32] found that health education programs involving an individualized approach and ongoing support can significantly improve glycemic control in DM patients. This study also shows that maintaining optimum glycemic management can lower the risk of microvascular consequences, including kidney injury. These conclusions are supported by recent studies from American Diabetes [2]; health education programs focusing on diabetes self-management can improve glucose control and prevent long-term consequences, including kidney failure.
Thus, it is possible to conclude that health education programs promote awareness and adoption of healthy behavior while improving glycemic control in diabetes mellitus patients. This is critical for reducing kidney problems and enhancing the patient's quality of life. For improved health results, it is recommended that such programs be implemented widely and sustainably.
Based on the data presented, health education programs have been shown to improve the quality of life of diabetic mellitus patients, which is an important indicator in disease management and the avoidance of renal problems. The p-value of 0.005 (<0.05) indicates that the improvement in quality of life is statistically significant. Apart from that, the t-statistics value of 2.775 indicates that the difference between the original sample and the sample mean is quite substantial, so the hypothesis is accepted. An increase in quality of life of 0.532 from the initial scale shows that this program has positively impacted the patient's physical, mental, and social aspects, which in turn can reduce the risk of complications such as diabetic nephropathy.
A meta-analysis by Alshahrani et al. [33] discovered that health education programs that take a holistic approach, including emotional support and teaching about healthy lifestyles, can dramatically improve the quality of life of DM patients. This study also found that improving quality of life can lower psychological loads and boost patient motivation to treat their disease more effectively. Additionally, Alshayban & Joseph [34] found that health education programs that promote quality of life can reduce the risk of microvascular consequences, including kidney injury, in DM patients.
Thus, it is possible to infer that health education programs not only raise knowledge, adopt healthy behaviors, and improve glycemic control, but also considerably improve the quality of life of diabetes mellitus patients. This is critical in avoiding kidney issues and increasing the patient's well-being. For improved health results, it is recommended that such programs be implemented widely and sustainably.
Practical recommendations for health educators and policymakers include developing and implementing health education programs that are more inclusive and tailored to individual needs, especially for younger age groups and those with lower levels of education. Health educators could consider more interactive and technology-based approaches to improve patient understanding. Policymakers should also support programs that involve cross-sector collaboration, including medical personnel, nutritionists, and psychologists, to strengthen the effectiveness of health education programs. In addition, further research needs to be conducted with more diverse samples and more accurate measurements to evaluate the long-term impact of these health education programs.
Conclusion
Increased knowledge, adoption of healthy behaviors, glycemic control, and quality of life positively influence the effectiveness of the transtheoretical model health education program.
Acknowledgments: The author would like to thank all parties who have supported and contributed to this research, including institutions, fellow researchers, and respondents who have participated.
Ethical Permissions: This study has obtained ethical approval from the Research Ethics Committee of the Faculty of Nursing Health, Airlangga University, Surabaya, Indonesia (NR.011.02/F.XXXII.25/09/2024).
Conflicts of Interests: The authors declare no conflict of interest in this research. The study was conducted objectively and independently, without influence from personal or external interests.
Authors' Contribution: Muhalla HI (First Author), Introduction Writer (15%); Nursalam N (Second Author), Methodologist (15%); Yusuf A (Third Author), Main Researcher (20%); Bakar A (Fourth Author), Discussion Writer (15%); Kurniawati ND (Fifth Author), Statistical Analyst (15%); Wahyudi AS (Sixth Author), Assistant Researcher (10%); Ma'ruf A (Seventh Author), Assistant Researcher (10%)
Funding/Support: This research was supported by the Faculty of Nursing, Airlangga University, Surabaya, Indonesia.
Keywords:
References
1. De Boer IH, Khunti K, Sadusky T, Tuttle KR, Neumiller JJ, Rhee CM, et al. Diabetes management in chronic kidney disease: A consensus report by the American Diabetes Association (ADA) and kidney disease: Improving global outcomes (KDIGO). Diabetes Care. 2022;45(12):3075-90. [Link] [DOI:10.2337/dci22-0027]
2. American Diabetes Association. Classification and diagnosis of diabetes: Standards of medical care in diabetes-2022. Diabetes Care. 2022;45(Suppl 1):S17-38. [Link] [DOI:10.2337/dc22-S002]
3. Odgers‐Jewell K, Ball LE, Kelly JT, Isenring EA, Reidlinger DP, Thomas R. Effectiveness of group‐based self‐management education for individuals with Type 2 diabetes: A systematic review with meta‐analyses and meta‐regression. Diabet Med. 2017;34(8):1027-39. [Link] [DOI:10.1111/dme.13340]
4. Ha Dinh TT, Bonner A, Clark R, Ramsbotham J, Hines S. The effectiveness of the teach-back method on adherence and self-management in health education for people with chronic disease: A systematic review. JBI Database Syst Rev Implement Rep. 2016;14(1):210-47. [Link] [DOI:10.11124/jbisrir-2016-2296]
5. Pamungkas R, Chamroonsawasdi K, Vatanasomboon P. A systematic review: Family support integrated with diabetes self-management among uncontrolled type II diabetes mellitus patients. Behav Sci. 2017;7(3):62. [Link] [DOI:10.3390/bs7030062]
6. Shan R, Sarkar S, Martin SS. Digital health technology and mobile devices for the management of diabetes mellitus: State of the art. Diabetologia. 2019;62(6):877-87. [Link] [DOI:10.1007/s00125-019-4864-7]
7. Reach G, Pechtner V, Gentilella R, Corcos A, Ceriello A. Clinical inertia and its impact on treatment intensification in people with type 2 diabetes mellitus. Diabetes Metab. 2017;43(6):501-11. [Link] [DOI:10.1016/j.diabet.2017.06.003]
8. Sinclair AJ, Abdelhafiz A, Dunning T, Izquierdo M, Rodriguez Manas L, Bourdel-Marchasson I, et al. An international position statement on the management of frailty in diabetes mellitus: Summary of recommendations 2017. J Frailty Aging. 2018;7(1):10-20. [Link] [DOI:10.14283/jfa.2017.39]
9. Hashemzadeh M, Rahimi A, Zare-Farashbandi F, Alavi-Naeini A, Daei A. Transtheoretical model of health behavioral change: A systematic review. Iran J Nurs Midwifery Res. 2019;24(2):83-90. [Link] [DOI:10.4103/ijnmr.IJNMR_94_17]
10. Alzeidan R, Shata Z, Hassounah MM, Baghdadi LR, Hersi A, Fayed A, et al. Effectiveness of digital health using the transtheoretical model to prevent or delay type 2 diabetes in impaired glucose tolerance patients: Protocol for a randomized control trial. BMC Public Health. 2019;19(1):1550. [Link] [DOI:10.1186/s12889-019-7921-8]
11. Zare M, Tarighat-Esfanjani A, Rafraf M, Shaghaghi A, Asghari-Jafarabadi M, Shamshiri M. The barriers and facilitators of self-management among adults with type 2 diabetes mellitus: A trans theoretical model (TTM)-based mixed method study in Iran. Diabetes Metab Syndr Obes. 2020;13:2687-99. [Link] [DOI:10.2147/DMSO.S230083]
12. Zare M, Tarighat-Esfanjani A, Rafraf M, Shaghaghi A, Asghari Jafarabadi M, Iranparvar-Alamdari M. Segmentation of Iranian Type 2 diabetes patients based on the transtheoretical model of behavior change. J Biochem TechNOL. 2019;10(2):23-33. [Link]
13. Selçuk‐Tosun A, Zincir H. The effect of a transtheoretical model-based motivational interview on self‐efficacy, metabolic control, and health behaviour in adults with type 2 diabetes mellitus: A randomized controlled trial. Int J Nurs Pract. 2019;25(4):e12742. [Link] [DOI:10.1111/ijn.12742]
14. Bonoto BC, De Araújo VE, Godói IP, De Lemos LLP, Godman B, Bennie M, et al. Efficacy of mobile apps to support the care of patients with diabetes mellitus: A systematic review and meta-analysis of randomized controlled trials. JMIR Mhealth Uhealth. 2017;5(3):e4. [Link] [DOI:10.2196/mhealth.6309]
15. Lee YJ, Shin SJ, Wang RH, Lin KD, Lee YL, Wang YH. Pathways of empowerment perceptions, health literacy, self-efficacy, and self-care behaviors to glycemic control in patients with type 2 diabetes mellitus. Patient Educ Couns. 2016;99(2):287-94. [Link] [DOI:10.1016/j.pec.2015.08.021]
16. Adu MD, Malabu UH, Malau-Aduli AEO, Malau-Aduli BS. Enablers and barriers to effective diabetes self-management: A multi-national investigation. PLoS One. 2019;14(6):e0217771. [Link] [DOI:10.1371/journal.pone.0217771]
17. Settineri S, Frisone F, Merlo EM, Geraci D, Martino G. Compliance, adherence, concordance, empowerment, and self-management: Five words to manifest a relational maladjustment in diabetes. J Multidiscip Healthc. 2019;12:299-314. [Link] [DOI:10.2147/JMDH.S193752]
18. Honda H, Igaki M, Tanaka SI, Ono K, Hirota Y. Impact of self-reported sitting time and transtheoretical model based on exercise behavior change on glycemic and weight control in Japanese adults with type 1 diabetes: A cross-sectional study. Healthcare. 2020;8(2):105. [Link] [DOI:10.3390/healthcare8020105]
19. Selçuk-Tosun A, Zincir H. The effect on health outcomes of post-intervention transtheoretical model-based motivational interview in adults with type 2 diabetes mellitus: Follow up a cross-sectional study. J Caring Sci. 2019;8(1):1-8. [Link] [DOI:10.15171/jcs.2019.001]
20. Amalia RN, Dianingati RS, Annisaa' E. The effect of number of respondents on the results of knowledge and self-medication behavior questionnaire's validity and reliability. Generics J Res Pharm. 2022;2(1):9-15. [Indonesian] [Link] [DOI:10.14710/genres.v2i1.12271]
21. Verd JM. Using a hybrid data collection tool: Analysis of youth labour market trajectories integrating quantitative, qualitative and social network data. Int J Soc Welf. 2023;32(1):9-19. [Link] [DOI:10.1111/ijsw.12528]
22. Elreedy D, Atiya AF. A comprehensive analysis of synthetic minority oversampling technique (SMOTE) for handling class imbalance. Inf Sci. 2019;505:32-64. [Link] [DOI:10.1016/j.ins.2019.07.070]
23. Maguire BJ, O'Meara P, O'Neill BJ, Brightwell R. Violence against emergency medical services personnel: A systematic review of the literature. Am J Ind Med. 2018;61(2):167-80. [Link] [DOI:10.1002/ajim.22797]
24. Berndt AE. Sampling methods. J Hum Lact. 2020;36(2):224-6. [Link] [DOI:10.1177/0890334420906850]
25. Cui F, Zhou Z, Zhou HS. Review-measurement and analysis of cancer biomarkers based on electrochemical biosensors. J Electrochem Soc. 2020;167(3):037525. [Link] [DOI:10.1149/2.0252003JES]
26. Pasquini C. Near infrared spectroscopy: A mature analytical technique with new perspectives-A review. ANALYTICA CHIMICA ACTA. 2018;1026:8-36. [Link] [DOI:10.1016/j.aca.2018.04.004]
27. Hox J, Moerbeek M, Van De Schoot R. Multilevel analysis: Techniques and applications. New York: Routledge; 2017. [Link] [DOI:10.4324/9781315650982]
28. Mohamad NR, Marzuki NHC, Buang NA, Huyop F, Wahab RA. An overview of technologies for immobilization of enzymes and surface analysis techniques for immobilized enzymes. Biotechnol Biotechnol Equip. 2015;29(2):205-20. [Link] [DOI:10.1080/13102818.2015.1008192]
29. Alrasheeday AM, Alshammari HS, Alshammari B, Alkubati SA, Llego JH, Alshammari AD, et al. Perceived barriers to healthy lifestyle adherence and associated factors among patients with type 2 diabetes mellitus: Implications for improved self-care. Patient Prefer Adherence. 2024;18:2425-39. [Link] [DOI:10.2147/PPA.S432806]
30. Narva AS, Norton JM, Boulware LE. Educating patients about CKD: The path to self-management and patient-centered care. Clin J Am Soc Nephrol. 2016;11(4):694-703. [Link] [DOI:10.2215/CJN.07680715]
31. Teshome A, Yitayeh A. The effect of periodontal therapy on glycemic control and fasting plasma glucose level in type 2 diabetic patients: Systematic review and meta-analysis. BMC Oral Health. 2016;17(1):31. [Link] [DOI:10.1186/s12903-016-0249-1]
32. Rodríguez-Gutiérrez R, Montori VM. Glycemic control for patients with type 2 diabetes mellitus: Our evolving faith in the face of evidence. Circ Cardiovasc Qual Outcomes. 2016;9(5):504-12. [Link] [DOI:10.1161/CIRCOUTCOMES.116.002901]
33. Alshahrani SM, Alzahran M, Alakhali K, Vigneshwaran E, Iqbal MJ, Khan NA, et al. Association between diabetes consequences and quality of life among patients with diabetes mellitus in the Aseer province of Saudi Arabia. Maced J Med Sci. 2020;8(E):325-30. [Link] [DOI:10.3889/oamjms.2020.4107]
34. Alshayban D, Joseph R. Health-related quality of life among patients with type 2 diabetes mellitus in Eastern Province, Saudi Arabia: A cross-sectional study. PLoS One. 2020;15(1):e0227573. [Link] [DOI:10.1371/journal.pone.0227573]










