Volume 17, Issue 1 (2025)
Iran J War Public Health 2025, 17(1): 89-101 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2025/02/1 | Accepted: 2025/03/19 | Published: 2025/03/25
Received: 2025/02/1 | Accepted: 2025/03/19 | Published: 2025/03/25
How to cite this article
Rahmat M, Aini Q. Bibliometric Analysis of Hospital and Intensive Care Unit Management. Iran J War Public Health 2025; 17 (1) :89-101
URL: http://ijwph.ir/article-1-1545-en.html
URL: http://ijwph.ir/article-1-1545-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
1- Muhammadiyah University Yogyakarta, Yogyakarta, Indonesia
Full-Text (HTML) (639 Views)
Introduction
Hospital management is a very important and complex field within the health system, particularly due to its functions that include planning, resource management, and effective delivery of health services [1]. A hospital is a highly structured organization, where each component has a specific role in supporting the overall functioning of the institution [2]. Among the various hospital units, the intensive care unit (ICU) is particularly crucial, as it handles critically ill patients who require continuous monitoring and specialized medical care [3]. ICU management, as a part of hospital management, faces increasing challenges in maintaining optimal service availability and quality of care. The demand for ICU services is soaring due to demographic shifts, the increasing number of patients with chronic diseases, and global health crises, such as pandemics [4]. The high need for intensive care necessitates that hospital management carefully plan and make decisions regarding ICU operations [5]. Limited ICU capacity, both in terms of rooms and skilled medical personnel, presents a significant challenge [6]. Substantial investment is required to expand ICU facilities, as each ICU must be equipped with advanced medical technology such as ventilators, dialysis machines, vital monitors, and other devices that ensure patient safety. Additionally, staff training and continuous skill improvement are necessary to keep pace with evolving medical protocols and technological advancements.
Advances in healthcare technology have also brought about significant changes in ICU management [7]. Today, a variety of medical equipment with increasingly precise monitoring and intervention capabilities is available to help manage patients in ICUs. Medical personnel can monitor patients’ vital signs in real time and receive early warnings in case of dangerous changes in their conditions. In addition, more advanced communication technologies enable medical teams in ICUs to collaborate more effectively with specialists in other fields, resulting in faster and more accurate decision-making [8]. However, the implementation of these technologies requires significant investment and ongoing maintenance [9]. Therefore, hospital management needs to develop a rigorous maintenance and supervision system, as well as provide technical training for staff to ensure that they can operate and maintain the equipment properly. Additionally, this technology needs to be calibrated regularly to maintain its accuracy, which adds to the operational burden of hospital management in the ICU [10]. Given these challenges, hospitals must allocate sufficient budgets and resources to sustain technological advancements while ensuring their effective utilization in patient care.
Communication and collaboration systems among medical personnel are essential for effective ICU management, as decision-making in ICUs often involves collaboration among various medical specialties, including cardiology, pulmonology, anesthesiology, and nutrition. Every action taken in the ICU must be clearly communicated to the entire medical team to avoid mistakes and ensure that each intervention is carried out appropriately. Effective communication can reduce the risk of miscommunication and ensure that all team members understand the patient’s condition and needs [11]. This requires a structured and efficient communication system, facilitated by accurate medical documentation and supporting technologies such as electronic medical records that provide access to information. Furthermore, establishing clear protocols and holding regular interdisciplinary meetings can enhance coordination among healthcare professionals. On the other hand, ICUs also face challenges in terms of financing, given the high costs associated with intensive care. ICU operational costs include not only medical equipment and facilities but also the salaries of highly skilled workers, equipment maintenance, and the procurement of specialized medications needed by critically ill patients [12]. Hospital management must possess the ability to create a financial system that can cover the operational costs of ICUs without compromising the quality of services provided [13]. In situations like these, hospitals should develop sustainable financing models that can work in conjunction with health insurance, government assistance, or other sources of funding to alleviate the costs incurred by patients and families. Establishing public-private partnerships and leveraging innovative financial mechanisms can also contribute to the long-term sustainability of ICU operations [14].
Previous bibliometric research has been widely conducted in various fields of health, such as epidemiology, patient safety, and health policy; however, it remains limited in the context of hospital and ICU management. Several studies have analyzed publication trends in the health system at large but have not specifically mapped the development of research in the field of hospital and ICU management. For instance, a study by Pierre et al. [15] discusses the impact of the “To Err Is Human” report 20 years after its publication, providing a bibliometric analysis of the report’s influence on research in patient safety. The findings of this study suggest that while the “To Err Is Human” report has significantly increased attention to patient safety, there is a need to expand research approaches and practices in this area to include a wider range of perspectives and methodologies. Additionally, another research discusses a bibliometric analysis of strategic management articles in healthcare management literature, examining the past, present, and future. The results offer insights into the development of strategic management research in the context of health management and identify potential areas for future research [16].
Research on hospital and ICU management spans various topics, including operational efficiency, patient care models, staff workload, and cost-effectiveness [17]. Hospital management primarily addresses broader aspects, such as governance, financial sustainability, and quality control, to enhance institutional healthcare delivery [17]. In contrast, ICU management focuses on specific challenges, such as patient monitoring, critical care protocols, and the integration of advanced medical technology [18]. While both fields emphasize efficiency and quality care, ICU management prioritizes rapid decision-making, intensive resource utilization, and teamwork across disciplines [19]. Methodologically, studies on hospital management often employ qualitative approaches, including case studies and policy analysis, to evaluate administration and organizational culture [20]. Meanwhile, ICU management research relies more on quantitative methods, such as clinical trials and statistical modeling, to assess patient outcomes and medical interventions [21]. Despite these differences, both fields are increasingly incorporating technology, data analytics, and artificial intelligence to enhance decision-making and optimize services.
Although research on hospital and ICU management is expanding, bibliometric analysis in these areas remains limited. A major gap is the lack of studies examining the link between hospital-wide policies and ICU-specific practices. Most bibliometric research focuses on one of these areas rather than analyzing their interaction in improving healthcare efficiency. Another gap is the insufficient identification of emerging trends and future research needs. Hospital management studies often explore financial models and healthcare policies, while ICU research concentrates on clinical improvements and patient-centered care. However, few bibliometric analyses integrate these topics for a comprehensive perspective. Additionally, research is predominantly focused on developed nations, leaving gaps in understanding hospital and ICU management in lower-income countries.
The impact of digital health technologies, including artificial intelligence, machine learning, and electronic health records, is also underexplored in bibliometric studies. While these innovations are reshaping hospital and ICU operations, there is limited research tracking their implementation and long-term outcomes. A more thorough bibliometric analysis could provide healthcare policymakers, administrators, and researchers with valuable insights to enhance ICU services and hospital management.
However, studies on research trends in the fields of hospital and ICU management are still not widely explored, despite the critical role these areas play in healthcare systems worldwide [12]. The complexity of ICU management, which involves resource allocation, patient care optimization, and advanced medical technologies, makes it essential to understand emerging research trends and innovations. Therefore, this study aimed to fill these gaps by analyzing the development of scientific publications, identifying key trends, and providing insights into the future direction of research. By employing bibliometric analysis, this study will help uncover research patterns and provide a comprehensive picture of how hospital and ICU management have evolved over the past decade. Understanding these trends is crucial for policymakers, hospital administrators, and researchers to formulate evidence-based strategies that improve ICU services and overall hospital management efficiency. Additionally, by recognizing the most influential authors, institutions, and research topics, this study will contribute to ongoing efforts to enhance hospital operations, improve patient outcomes, and optimize healthcare policies [22].
Information and Methods
This study employed a qualitative methodology, utilizing a literature review approach with a focus on bibliometric analysis. Bibliometric analysis is a method used to identify and highlight significant insights derived from annual scientific literature contributed by researchers in different countries worldwide [23]. This method utilizes bibliographic data, including citations, publication counts, and journal information, to uncover trends, patterns, and frameworks in the creation and dissemination of scientific knowledge [24-26]. Bibliometric studies aim to develop and map specific areas of research [27]. They provide several benefits, including identifying areas of knowledge that require deeper exploration and highlighting the most prominent research topics within a particular field. To facilitate the analysis and visualization of research data, the author employs the Vosviewer application. The data consisted of articles published over the past decade, from 2014 to 2023, sourced from journals indexed in the Scopus database. Scopus was chosen as the primary source because it includes a wide range of multidisciplinary scientific literature, covering fields, such as medicine and social sciences that are relevant to this research. Although databases, like PubMed, focus more on the biomedical field, and the Web of Science has a broad historical scope, using additional databases can result in variations in the number of articles found as well as a more diverse coverage of topics.
Articles included in this analysis met the following inclusion criteria: published in Scopus-indexed journals, focused on hospital and ICU management, written in English, classified within the fields of medical and social sciences, and available in open or limited access. Meanwhile, excluded articles are those that are not journal articles, such as editorials, conference proceedings, or brief reviews, irrelevant to the main topic, and not available in full text.
The bibliometric analysis also included an evaluation of citation metrics, such as the total number of citations for each article, the impact factor of the journal in which the article was published, and the h-index of the lead author. This metric is used to identify publications that have a significant influence in the field of hospital management and intensive care [28]. To refine the data for this study, the authors applied a specific formula to narrow the results, ultimately selecting 203 articles from a total of 663 scientific papers (Figure 1). These articles were identified using the keywords “hospital management” and “Intensive Care Unit.” The data reduction process was carried out using the search and filtering capabilities of the Scopus database: (Title-Abs-Key (“Hospital Management”) And Title-Abs-Key (“Intensive Care Unit”)) And Pubyear > 2014 And Pubyear < 2023 And (Limit To (Doctype, “Ar”)) And (Limit To (Pubstage, “Final”)) And (Limit To (Srctype, “J”)) And (Limit To (Language, “English”)) And (Limit To (Oa, “All”)) And (Limit To (Subjarea, “Medi”) Or Limit To (Subjarea, “Soci”)).
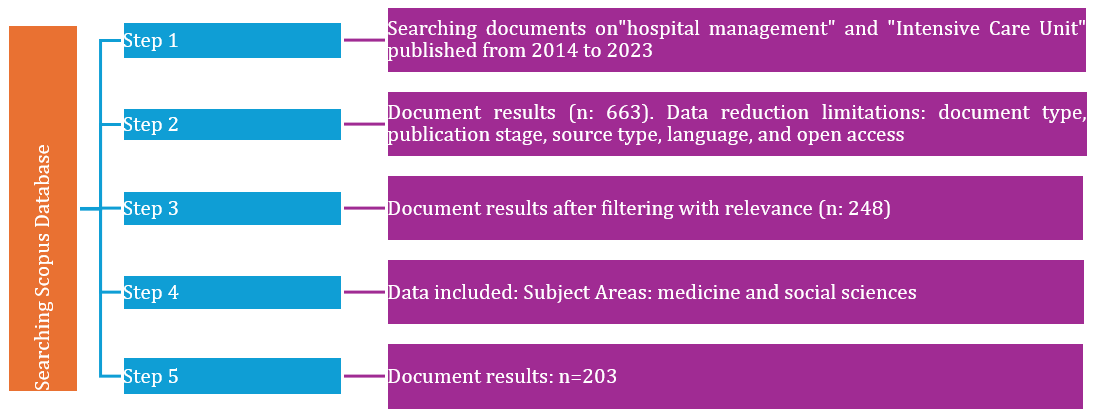
Figure 1. The PRISMA flow diagram used to identify, screen, and include papers for our bibliometric review (2025)
Findings
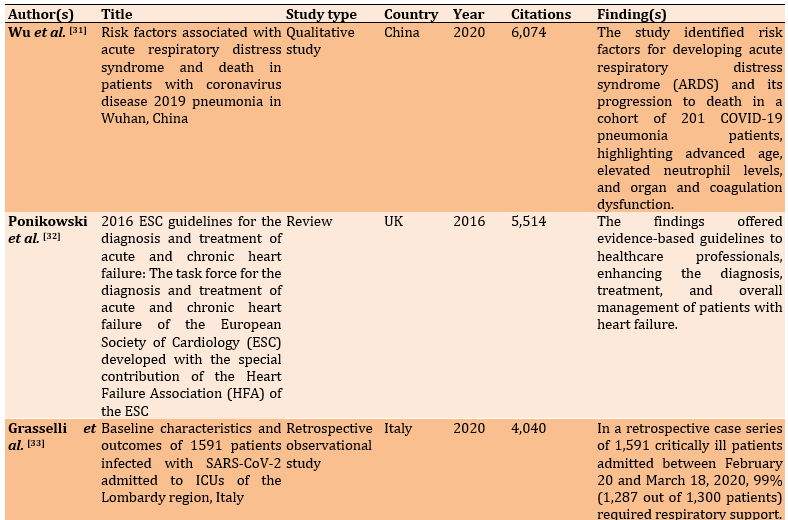
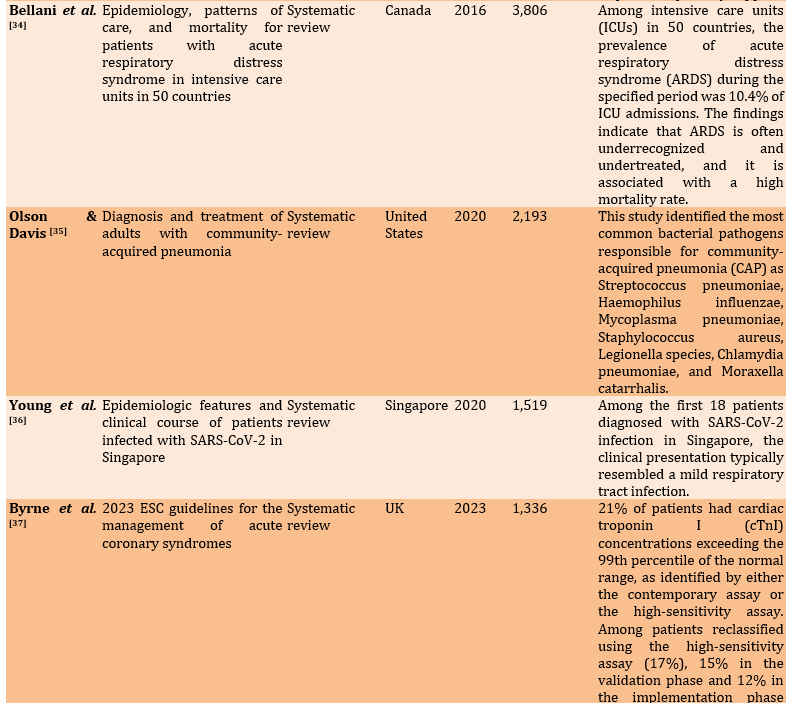
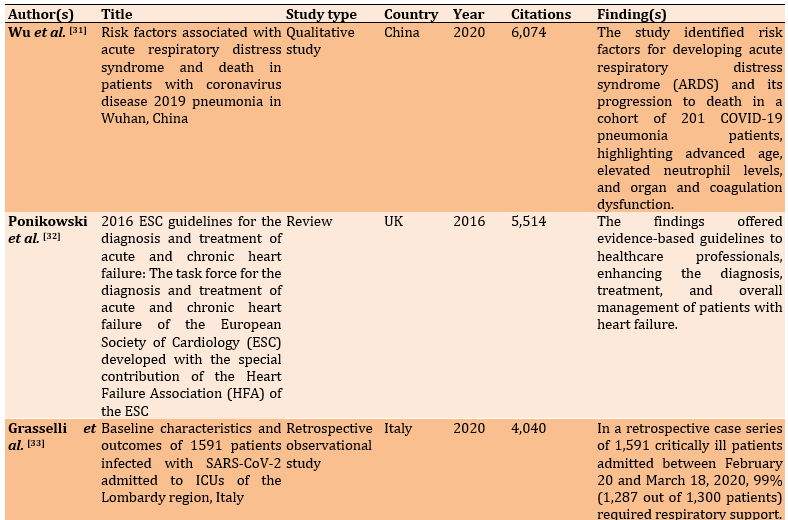
It is very important to present the results to the public in the context of hospital and ICU management. This process is crucial for gaining a comprehensive understanding of research trends, advancements, and future opportunities in the field of hospital and ICU management. By systematically analyzing the literature, it becomes possible to identify key insights, emerging themes, and areas that require further exploration, ultimately contributing to the advancement of knowledge and practices in this critical domain [29]. This condition aligns with the vital role of hospital and ICU management in maintaining the quality of health services; this analysis serves as an important foundation for researchers, hospital managers, and policymakers. A key finding was revealing the main trends, and focusing on hospital and ICU management. Bibliometric analysis illustrates how specific topics, such as management technology, resource efficiency, patient safety, and decision-making systems, evolve [30]. A total of 203 articles were selected for evaluation. The top ten countries identified were the United States (48%), the United Kingdom (17%), China (12%), Italy (11%), and Canada (10%; Table 1).
Table 1. Characteristics of research conducted on hospital and intensive care unit management
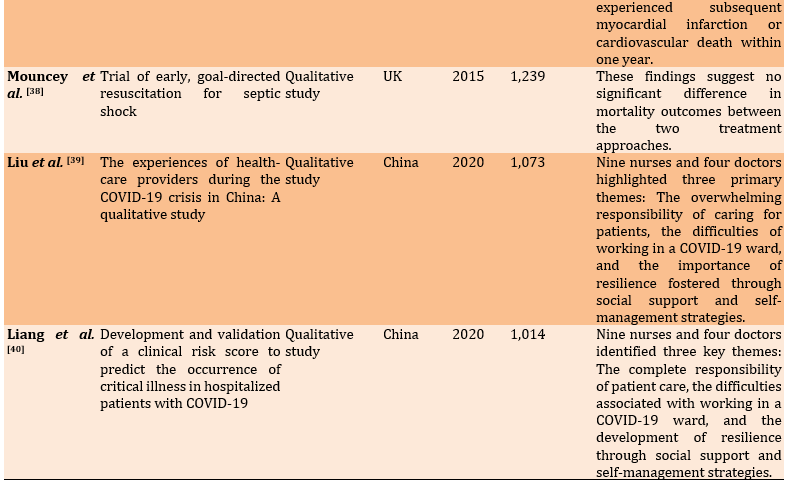
Improvement, severe care, assessment, recommendations, challenges, and healthcare providers were among the factors identified as related to integrated hospital and ICU management (Table 2).
Table 2. Factors related to the integrated hospital and intensive care unit management
Maintaining and enhancing various factors in hospital management and the ICU ensures the delivery of optimal care to hospital patients. These factors are critical for improving service quality, patient outcomes, and overall operational efficiency in healthcare settings. Hospital services can follow developments in facilities and hospital management systems that prioritize the efficiency and effectiveness of services in the ICU. This broad research perspective focuses on past, present, and emerging trends. In greater depth, the author analyzed and mapped the big data results from Scopus with relevant themes from 2014 to 2023.
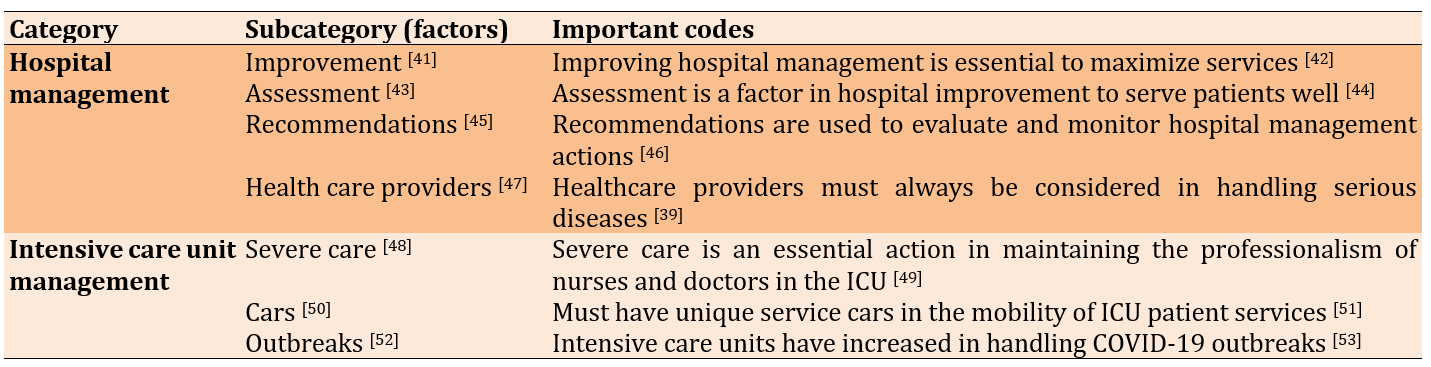
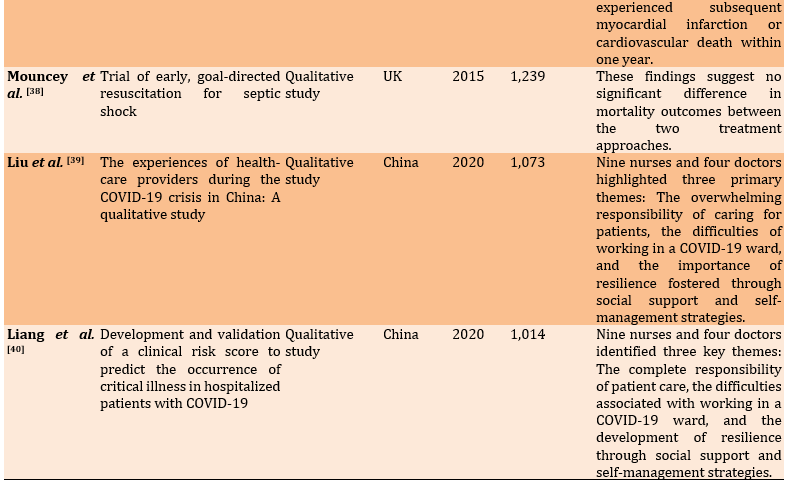
The data revealed a consistent and significant rise in the number of publications in recent years, reflecting growing research activity and interest in the field (Figure 2). This underscores the increasingly relevant theme of hospital and ICU management. The following visualization presents the progress of the study of hospital and ICU management over the last ten years. There have been significant fluctuations in the number of publications per year, with some years showing notable increases while others experienced decreases. At the beginning of the period, specifically in 2014 and 2015, the number of publications was relatively low, at seven. In 2016, there was a slight increase to 11 publications, but this declined back to seven in 2017. The following year, 2018, also saw a further decline to ten publications. Starting in 2019, there was a more pronounced upward trend, with the number of publications rising to 17, and then to 18 in 2020. In 2021, there was a significant jump, reaching 46 publications, which is the highest number during the period shown. This surge may be related to the COVID-19 pandemic, which has made the topic of hospital and ICU management even more critical, thereby attracting greater research interest. The conditions that arose worldwide in 2021 were a direct impact of the COVID-19 pandemic, leading to a crisis in ICU capacity, including the availability of ICU beds, ventilators, and medical resources. As a result, hospital management moved more swiftly to develop new treatment protocols for COVID-19 patients, including the management of critical patients, the use of PPE, and measures to prevent transmission in healthcare facilities.
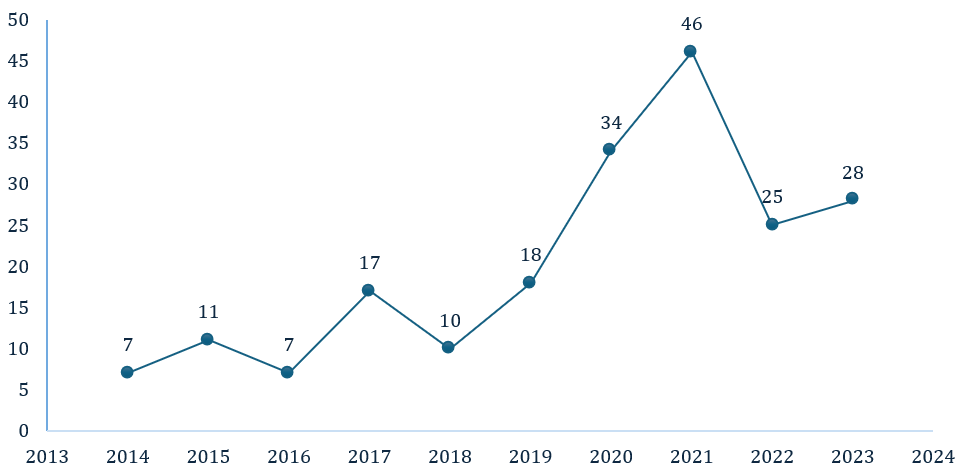
Figure 2. Publication by year (2012-2024)
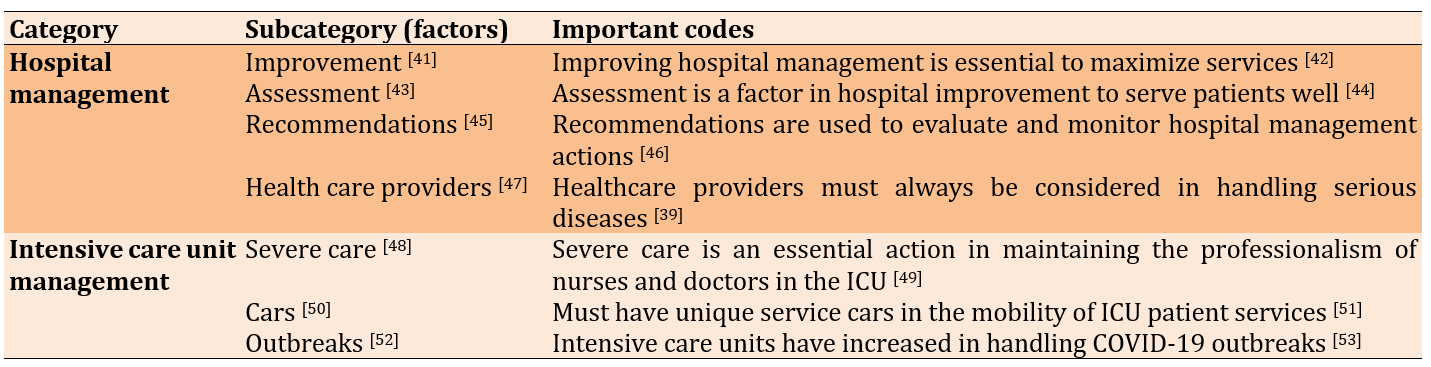
However, after its peak in 2021, there was a decline in the number of publications in 2022, with the figure dropping to 25. In 2023, there was a slight increase back to 28 publications, although this was still well below the high number reached in 2021. Overall, publication trends show a fluctuating increase in interest in this topic, with a sharp rise during the pandemic. This reflects how urgent global conditions, such as the pandemic, can affect the focus of research in the health sector. The increase in 2023, although small, indicates that this topic still holds relevance and attracts attention in research among academics and healthcare practitioners. Our findings map countries that are significantly concerned with hospital and ICU management in detail (Figure 3).
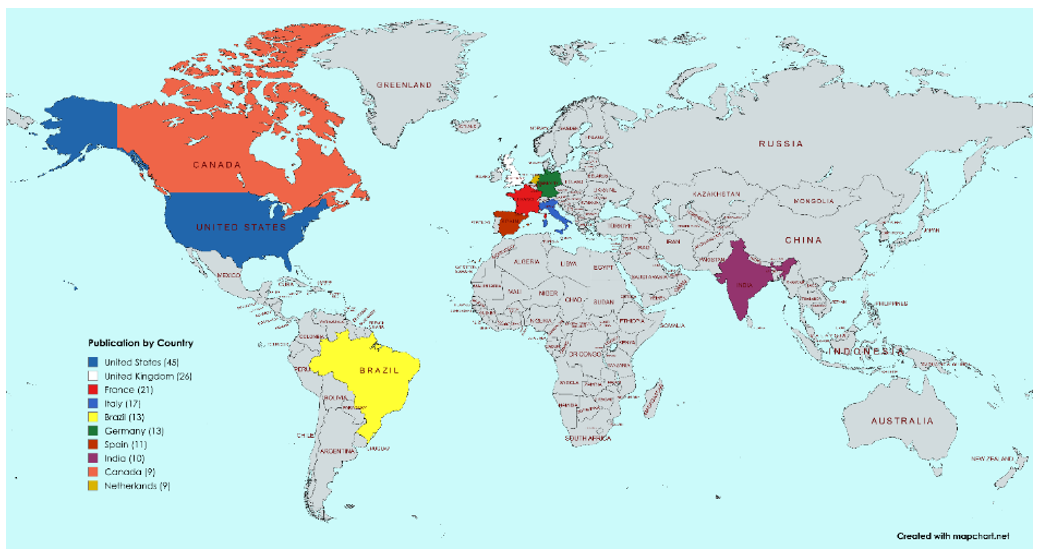
Figure 3. Academic production by country, from 2014-2023 (Software Mapchart)
The United States was among the countries with the highest concentration of research activity in the world, highlighting its prominent role and contributions in the field being studied. The United States showed a strong interest in developing health services, infrastructure, and its well-developed healthcare system. This situation is relevant because the United States has also become a center for global health research; thus, it is unsurprising that this country has the highest concentration of efforts to encourage progress in hospital management and ICU health services. The United States has prioritized technological sophistication in addressing health problems to promote competitive hospital services, including those aimed at treating elderly individuals with disabilities [54].
In second place was England, with 26 publications. In its efforts to enhance health management services in hospitals and ICU settings, the UK emphasized communication strategies, patient self-monitoring, and remote patient tracking as key priorities. These approaches aim to improve care quality, patient engagement, and operational efficiency in healthcare delivery [55]. Meanwhile, the Netherlands ranked tenth in the world with a research focus on hospital and ICU management, examining trends and future research. The management of hospital and ICU health services is crucial for addressing diseases that have impacted the global community; the Netherlands prioritizes collaboration in hospital services to consolidate the innovative results of various experts [56]. One of the large-scale collaborations undertaken in the Netherlands involves managing COVID-19, which is an international challenge [57]. Overall, both developed and developing countries with substantial health infrastructure and populations were demonstrating significant interest in this research topic. Furthermore, the author analyzes the mapping of hospital management in greater depth, highlighting important points and network relationships within this research issue (Figure 4).
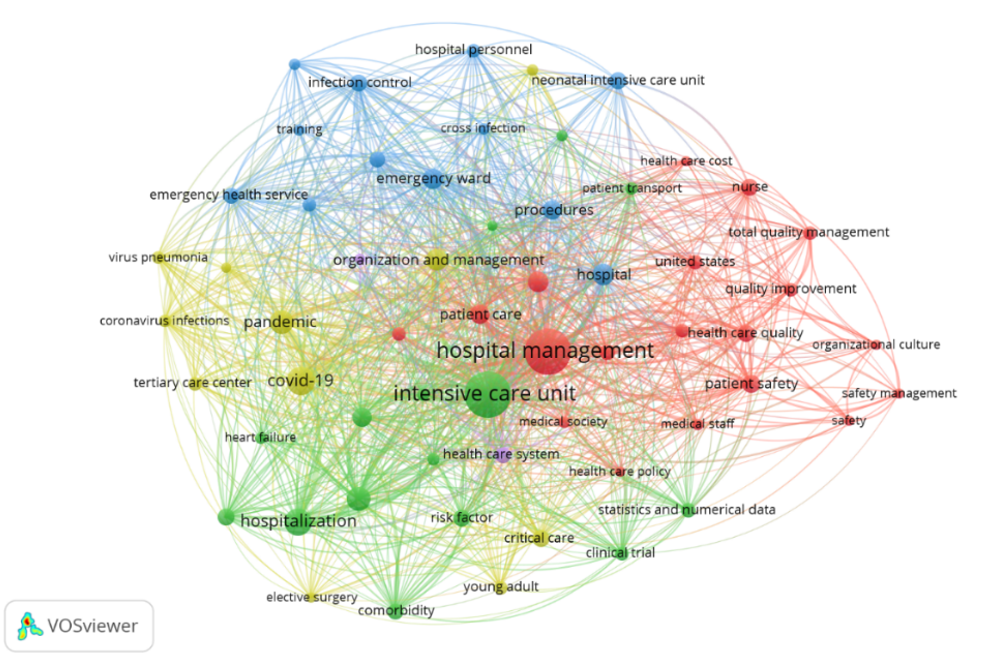
Figure 4. Hospital and intensive care unit management research trends (2014-2023)
Hospital management was the main focus, and there was a close relationship with the ICU. One of the most highlighted issues is related to nurse fatigue in providing medical services to patients, particularly on the African continent, where Ghana had a fatigue score reaching 76.43±27.80 out of 124 [58]. These findings underscore the importance of issues related to emergency health services, safety management in hospitals, and critical care to promote quality hospital and ICU management in the future [59].
Next, the colors in this visualization indicated the publication timeline or popularity of the themes from 2018 to 2021, with a color gradient ranging from blue (2018) to yellow (2021). Themes, such as infection control, cross-infection, health care cost, organizational culture, and patient safety, represented the initial focus in the literature on hospital and ICU management, particularly concerning infection prevention and cost control. In 2019, the focus began to shift toward emergency care and risk management, especially in relation to tertiary care and service quality improvement. The light green color highlights the surge in research in 2020 related to the COVID-19 pandemic. These keywords suggest that the pandemic is drastically changing priorities in hospital management and increasing the focus on how hospitals handle patient surges, particularly concerning intensive care and viral infections. In 2021, attention shifted to the overall management of hospitals and ICUs, with an emphasis on optimal patient care, total quality management, and effective health policies. The themes that appear in different colors and years reflected the evolution of research focus in the field of hospital and ICU management.
On the other hand, training, infection control, risk factor critical care, health care cost, and nurse and safety management tended to appear on the outermost side of the visualization, suggesting that these terms have not been widely researched or have less relevance to the main terms. Specifically, this indicates that the area was still open for further research. Future studies can explore the relationships and interactions between each of these keywords and Hospital and ICU management. By deeply understanding these interactions, subsequent research can identify new strategies to improve patient safety, enhance service standards, and increase the efficiency of information management in the ICU environment. Therefore, further research in this field will not only expand our understanding of effective hospital management but can also provide a foundation for the improvement of the public health system.
The yellow color in Figure 5 indicated the most frequently discussed topics. The denser the keywords surrounded by yellow, the more research has focused on this perspective. Conversely, if the yellow color is not concentrated around a keyword, it suggests that the topic has not been widely discussed in the research. Therefore, these keywords can be used as a novelty in future studies. Hospital management, ICU, pandemic, COVID-19, hospitalization, patient care, patient safety, and organization management formed a dense group, indicating that these terms are frequently associated or addressed together in the literature under analysis. This suggested a strong thematic connection or recurring focus on these concepts within the research being examined. Meanwhile, keywords, such as training, infection control, risk factor critical care, health care cost, nurse, and safety management, tended to appear on the outer side of the visualization, suggesting that these terms have not been widely researched or have less relevance to the main terms. Specifically, this indicates that the area is still open for further research. Further studies in this area hold the potential to offer new insights and deepen our understanding of the connections between various aspects of nurse resilience and related concepts in Public Health and health management. Such research could enhance strategies for supporting healthcare professionals and improving overall health systems.
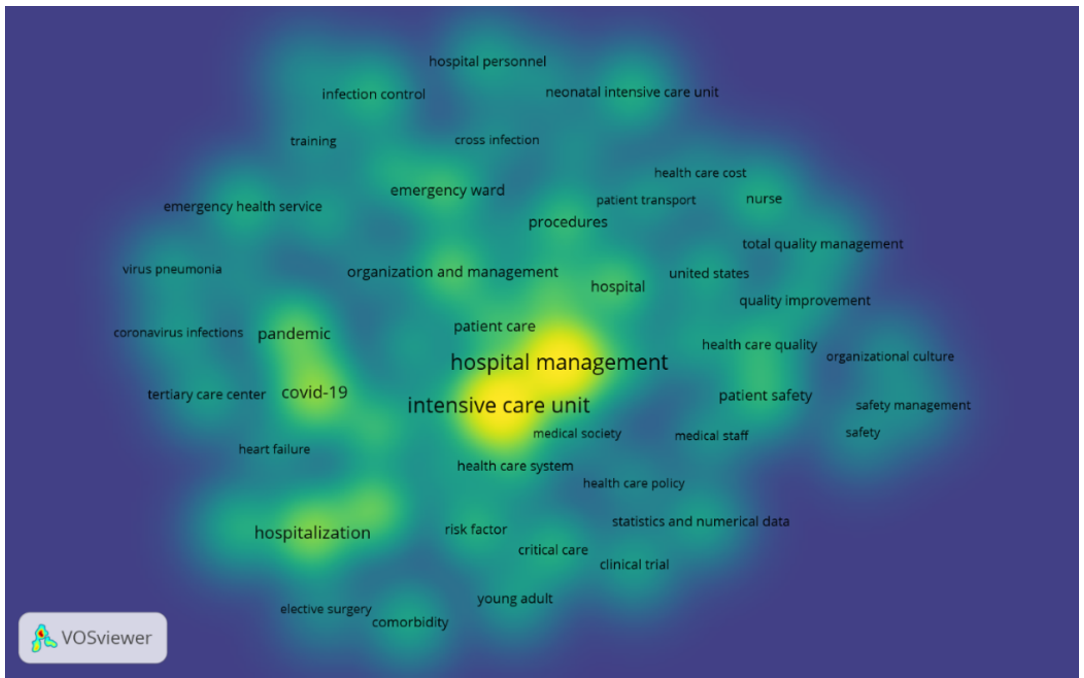
Figure 5. Research agenda and future research of nurse resilience (2014-2023)
Furthermore, keywords, such as patient care, health care system, health care policy, medical staff, patient safety, COVID-19, hospitalization, and emergency ward [60], had the highest occurrence and showed the most vital relationship with research on hospital and ICU management. Patient care, along with the topics of hospital and ICU management, was intertwined because the main focus of hospital management is to ensure the best quality of care for each patient, especially in the ICU [61]. The ICUs aim to provide intensive monitoring and care for critical patients; therefore, effective management is needed to ensure that the needs of each patient are met optimally [4]. The Health Care System is interrelated with hospital and ICU management because an effective health system serves as the foundation for the overall management and operation of the hospital [1]. The management of ICUs requires strong support from the health system regarding resource procurement, procedural arrangements, and coordination between departments to ensure a rapid response and high quality of care. Health care policy is interconnected with the topics of hospital and ICU management because health policy establishes the standards, regulations, and guidelines that must be adhered to in hospital management, including in the ICU [62].
These policies govern various aspects, such as staff qualifications, safety standards, and treatment procedures, which directly impact how ICU management is implemented to achieve optimal treatment outcomes [63]. Medical staff members are interrelated with hospital and ICU management because medical personnel are the core of ICU operations and are responsible for treating patients in critical condition. Effective management must ensure adequate staffing, appropriate qualifications, clearly defined tasks, and specialized training so that medical personnel can carry out their duties efficiently and safely in a stressful environment such as the ICU. Patient safety, hospital management, and ICUs are interconnected because patient safety is a top priority in hospital operations, especially in ICUs that handle high-risk patients. Hospital management is responsible for implementing safety protocols and standards of care to reduce the risk of medical errors, infections, or other complications that can harm patients; thus, maintaining patient safety is the main focus of ICU management [64].
Discussion
This study aimed to analyze the trends and developments in the field of hospital and intensive care unit management based on bibliometric data from 2014 to 2023. In recent years, research on hospital and ICU management has become significant, as the ICU is a crucial factor in hospital management. During the period from 2014 to 2023, there was a significant increasing trend in the number of publications indexed by Scopus on hospital and ICU management, with a notable rise from 2019 to 2021. In 2019, researchers reviewed hospital and ICU management in terms of patient safety [65] and health information technology (IT) [66]. These findings illustrate that patient safety and health IT play important roles in supporting hospital and ICU management. Patient safety is a fundamental aspect of providing high-quality healthcare and reducing the risk of injury or medical errors, especially in critical environments such as ICUs. The use of health IT, such as electronic medical records, real-time patient monitoring systems, and data analysis tools, helps reduce errors, accelerate clinical responses, and improve medical team coordination. The combination of a focus on patient safety and the implementation of health IT enables hospital management to be more efficient in managing resources, optimizing workflows, and improving data-driven clinical decision-making [67, 68].
In 2020, researchers studied hospital and ICU management in terms of critical care costs and the COVID-19 pandemic [69], illustrating that critical care costs and the COVID-19 pandemic are closely related in the context of hospital and ICU Management. The COVID-19 pandemic has led to a surge in the need for critical care services worldwide, which, in turn, has a direct impact on critical care costs. ICUs must operate under high pressure to care for a large number of patients with severe symptoms, necessitating the use of ventilators, specialized medications, and other medical resources. These increased costs include expenditures on medical equipment, PPE, the need for additional healthcare workers, and the costs associated with maintaining intensive care facilities, all of which continue to rise. The relationship between critical care costs and the COVID-19 pandemic also highlights the need for hospital management to have a preparedness strategy for dealing with crisis situations.
Finally, in 2021, researchers frequently reviewed hospital and ICU management in terms of risk factors [70] and medical staff [71], illustrating that risk factors and medical staff are important links in hospital and ICU management. Risk factors refer to elements that can increase the likelihood of complications or the worsening of a patient’s condition in intensive care. In the context of hospital management, the relationship between risk factors and medical staff underscores the importance of ongoing training, meeting the needs of healthcare workers, and providing optimal resource support. These steps are essential for improving patient care and ensuring the well-being of the medical team [72]. Hospitals need to ensure that medical staff have access to effective monitoring technologies and tools to help manage risk proactively. Countries have made significant contributions to hospital and ICU management. The United States leads in the number of publications on this topic, with a total of 45 publications recorded. This highlights the significant contribution and active involvement in research in this area [73]. It indicates that the United States has a strong interest and focus on the topic of hospital and ICU management. As a country with a diverse population and complex health challenges, such as high rates of obesity, chronic diseases, and elevated hospitalization rates, the United States requires a robust hospital and intensive care management system. This situation has been further amplified by the COVID-19 pandemic, which has increased the need for a responsive and adaptive health system. The challenges arising from the pandemic have prompted researchers and medical practitioners in the United States to focus more on finding new ways to improve the efficiency of ICU care, optimize hospital resources, and enhance workflows within the health system. This study suggests that there is an urgency to continue developing and improving the health system, especially regarding hospital and ICU management [74]. Research on hospital and ICU management often involves the development and implementation of new technologies, such as artificial intelligence-based patient monitoring systems, telemedicine devices, and advanced health data management systems [75].
The study has strengths and weaknesses that must be considered. By leveraging only the Scopus database, which consists of leading journals that have undergone a rigorous peer-review process, and by applying bibliometric techniques, this study provides a versatile, reasonable, and insightful analysis that allows for a quick understanding of research trends and opportunities for novelty [76]. This study has several theoretical contributions. First, it offers a comprehensive review of Hospital Management and ICUs, which are often underexplored. Second, the findings are supported by empirical data demonstrating improvements in the quality of health care through increased awareness of ICU management practices. Finally, this study provides insights that encourage wider adoption of ICU management in the realm of hospital management [77].
Research on hospital and ICU management is important due to its crucial role in improving healthcare efficiency, optimizing resources, and ensuring patient safety in high-risk environments. The trend of increasing publications over the past decade indicates that this issue is becoming increasingly relevant, especially in light of global challenges, such as the COVID-19 pandemic, limited medical personnel, and the need for the application of more sophisticated health technologies. However, there are still gaps in existing research. Most studies focus on specific aspects, such as patient safety, health information technology, and the cost of critical care, but there is still limited exploration of the effectiveness of data-driven management strategies, the impact of health policies on ICUs, and the influence of socio-economic factors in intensive care. Future research may lead to a deeper analysis of how evidence-based management strategies can improve hospital efficiency and how data-driven prediction systems can help optimize resource allocation. For future bibliometric studies, it is recommended to incorporate machine learning techniques in the analysis of research trends. This method can help identify hidden patterns, relationships between topics, and predict the direction of future research more accurately.
Although this study successfully explained the research development map in hospital and ICU management, it has limitations regarding data sources. The analyzed data were drawn from only one database. Further studies need to include other databases, such as Web of Science, Dimension, Connected Papers, Open Knowledge Maps, and PubMed [78]. Bibliometric studies also have other limitations, including self-citation bias, where some authors or institutions repeatedly cite their own work, which can affect the results of citation trend analysis. In addition, the database used (Scopus) may not include all relevant articles from unindexed journals, potentially leading to limitations in the generalization of findings.
The research has important implications for a wide range of stakeholders in the health sector, including hospital administrators, medical researchers, and policymakers. For hospital administrators, the identified research trends can serve as a basis for the planning and management of ICUs. For example, the increasing focus on patient health and safety information technology indicates the need to invest in real-time patient monitoring systems and electronic medical records to improve efficiency and reduce medical errors. Additionally, understanding the patterns of critical care costs and the impact of the pandemic on ICU capacity can help hospitals allocate resources more effectively, both in normal situations and during health crises.
For medical researchers, the results of this study identified gaps in research that could present opportunities for further exploration. Some areas that remain underexplored include the analysis of the effectiveness of data-driven management strategies in ICUs, the influence of health policies on hospital efficiency, and the impact of socio-economic factors on intensive care. By understanding research trends, researchers can develop studies that are more relevant to current and future needs, as well as generate innovations in critical care systems.
For policymakers, the findings of this study can be used as a foundation for formulating health policies, particularly in the allocation of funding. Given research trends indicating that patient safety and health technology play important roles in ICU management, policymakers can consider increasing funding for research and the implementation of technologies that can support the efficiency and quality of critical care. Furthermore, the increased attention to the cost of critical care during the pandemic demonstrates the need for a more flexible and responsive healthcare financing strategy for emergency situations. By understanding existing research trends and gaps, all stakeholders can contribute to improving the quality of ICU services in terms of management, research, and public policy.
Conclusion
Bibliometric analysis reveals a significant increase in the number of publications from 2019 to a peak in 2021, reflecting how global conditions, such as the pandemic, have influenced research focus.
Acknowledgments: The authors appreciate all the assistance they received in developing and revising this work.
Ethical Permissions: Not applicable, as the researcher uses secondary data that has been anonymized and is publicly available. There is no direct interaction with the research participants; thus, additional ethical clearance is not required.
Conflicts of Interests: The authors declared no conflicts of interests.
Authors' Contribution: Rahmat M (First Author), Introduction Writer/Methodologist/Statistical Analyst (70%); Aini O (Second Author), Statistical Analyst/Discussion Writer (30%)
Funding/Support: This research received no external funding.
Hospital management is a very important and complex field within the health system, particularly due to its functions that include planning, resource management, and effective delivery of health services [1]. A hospital is a highly structured organization, where each component has a specific role in supporting the overall functioning of the institution [2]. Among the various hospital units, the intensive care unit (ICU) is particularly crucial, as it handles critically ill patients who require continuous monitoring and specialized medical care [3]. ICU management, as a part of hospital management, faces increasing challenges in maintaining optimal service availability and quality of care. The demand for ICU services is soaring due to demographic shifts, the increasing number of patients with chronic diseases, and global health crises, such as pandemics [4]. The high need for intensive care necessitates that hospital management carefully plan and make decisions regarding ICU operations [5]. Limited ICU capacity, both in terms of rooms and skilled medical personnel, presents a significant challenge [6]. Substantial investment is required to expand ICU facilities, as each ICU must be equipped with advanced medical technology such as ventilators, dialysis machines, vital monitors, and other devices that ensure patient safety. Additionally, staff training and continuous skill improvement are necessary to keep pace with evolving medical protocols and technological advancements.
Advances in healthcare technology have also brought about significant changes in ICU management [7]. Today, a variety of medical equipment with increasingly precise monitoring and intervention capabilities is available to help manage patients in ICUs. Medical personnel can monitor patients’ vital signs in real time and receive early warnings in case of dangerous changes in their conditions. In addition, more advanced communication technologies enable medical teams in ICUs to collaborate more effectively with specialists in other fields, resulting in faster and more accurate decision-making [8]. However, the implementation of these technologies requires significant investment and ongoing maintenance [9]. Therefore, hospital management needs to develop a rigorous maintenance and supervision system, as well as provide technical training for staff to ensure that they can operate and maintain the equipment properly. Additionally, this technology needs to be calibrated regularly to maintain its accuracy, which adds to the operational burden of hospital management in the ICU [10]. Given these challenges, hospitals must allocate sufficient budgets and resources to sustain technological advancements while ensuring their effective utilization in patient care.
Communication and collaboration systems among medical personnel are essential for effective ICU management, as decision-making in ICUs often involves collaboration among various medical specialties, including cardiology, pulmonology, anesthesiology, and nutrition. Every action taken in the ICU must be clearly communicated to the entire medical team to avoid mistakes and ensure that each intervention is carried out appropriately. Effective communication can reduce the risk of miscommunication and ensure that all team members understand the patient’s condition and needs [11]. This requires a structured and efficient communication system, facilitated by accurate medical documentation and supporting technologies such as electronic medical records that provide access to information. Furthermore, establishing clear protocols and holding regular interdisciplinary meetings can enhance coordination among healthcare professionals. On the other hand, ICUs also face challenges in terms of financing, given the high costs associated with intensive care. ICU operational costs include not only medical equipment and facilities but also the salaries of highly skilled workers, equipment maintenance, and the procurement of specialized medications needed by critically ill patients [12]. Hospital management must possess the ability to create a financial system that can cover the operational costs of ICUs without compromising the quality of services provided [13]. In situations like these, hospitals should develop sustainable financing models that can work in conjunction with health insurance, government assistance, or other sources of funding to alleviate the costs incurred by patients and families. Establishing public-private partnerships and leveraging innovative financial mechanisms can also contribute to the long-term sustainability of ICU operations [14].
Previous bibliometric research has been widely conducted in various fields of health, such as epidemiology, patient safety, and health policy; however, it remains limited in the context of hospital and ICU management. Several studies have analyzed publication trends in the health system at large but have not specifically mapped the development of research in the field of hospital and ICU management. For instance, a study by Pierre et al. [15] discusses the impact of the “To Err Is Human” report 20 years after its publication, providing a bibliometric analysis of the report’s influence on research in patient safety. The findings of this study suggest that while the “To Err Is Human” report has significantly increased attention to patient safety, there is a need to expand research approaches and practices in this area to include a wider range of perspectives and methodologies. Additionally, another research discusses a bibliometric analysis of strategic management articles in healthcare management literature, examining the past, present, and future. The results offer insights into the development of strategic management research in the context of health management and identify potential areas for future research [16].
Research on hospital and ICU management spans various topics, including operational efficiency, patient care models, staff workload, and cost-effectiveness [17]. Hospital management primarily addresses broader aspects, such as governance, financial sustainability, and quality control, to enhance institutional healthcare delivery [17]. In contrast, ICU management focuses on specific challenges, such as patient monitoring, critical care protocols, and the integration of advanced medical technology [18]. While both fields emphasize efficiency and quality care, ICU management prioritizes rapid decision-making, intensive resource utilization, and teamwork across disciplines [19]. Methodologically, studies on hospital management often employ qualitative approaches, including case studies and policy analysis, to evaluate administration and organizational culture [20]. Meanwhile, ICU management research relies more on quantitative methods, such as clinical trials and statistical modeling, to assess patient outcomes and medical interventions [21]. Despite these differences, both fields are increasingly incorporating technology, data analytics, and artificial intelligence to enhance decision-making and optimize services.
Although research on hospital and ICU management is expanding, bibliometric analysis in these areas remains limited. A major gap is the lack of studies examining the link between hospital-wide policies and ICU-specific practices. Most bibliometric research focuses on one of these areas rather than analyzing their interaction in improving healthcare efficiency. Another gap is the insufficient identification of emerging trends and future research needs. Hospital management studies often explore financial models and healthcare policies, while ICU research concentrates on clinical improvements and patient-centered care. However, few bibliometric analyses integrate these topics for a comprehensive perspective. Additionally, research is predominantly focused on developed nations, leaving gaps in understanding hospital and ICU management in lower-income countries.
The impact of digital health technologies, including artificial intelligence, machine learning, and electronic health records, is also underexplored in bibliometric studies. While these innovations are reshaping hospital and ICU operations, there is limited research tracking their implementation and long-term outcomes. A more thorough bibliometric analysis could provide healthcare policymakers, administrators, and researchers with valuable insights to enhance ICU services and hospital management.
However, studies on research trends in the fields of hospital and ICU management are still not widely explored, despite the critical role these areas play in healthcare systems worldwide [12]. The complexity of ICU management, which involves resource allocation, patient care optimization, and advanced medical technologies, makes it essential to understand emerging research trends and innovations. Therefore, this study aimed to fill these gaps by analyzing the development of scientific publications, identifying key trends, and providing insights into the future direction of research. By employing bibliometric analysis, this study will help uncover research patterns and provide a comprehensive picture of how hospital and ICU management have evolved over the past decade. Understanding these trends is crucial for policymakers, hospital administrators, and researchers to formulate evidence-based strategies that improve ICU services and overall hospital management efficiency. Additionally, by recognizing the most influential authors, institutions, and research topics, this study will contribute to ongoing efforts to enhance hospital operations, improve patient outcomes, and optimize healthcare policies [22].
Information and Methods
This study employed a qualitative methodology, utilizing a literature review approach with a focus on bibliometric analysis. Bibliometric analysis is a method used to identify and highlight significant insights derived from annual scientific literature contributed by researchers in different countries worldwide [23]. This method utilizes bibliographic data, including citations, publication counts, and journal information, to uncover trends, patterns, and frameworks in the creation and dissemination of scientific knowledge [24-26]. Bibliometric studies aim to develop and map specific areas of research [27]. They provide several benefits, including identifying areas of knowledge that require deeper exploration and highlighting the most prominent research topics within a particular field. To facilitate the analysis and visualization of research data, the author employs the Vosviewer application. The data consisted of articles published over the past decade, from 2014 to 2023, sourced from journals indexed in the Scopus database. Scopus was chosen as the primary source because it includes a wide range of multidisciplinary scientific literature, covering fields, such as medicine and social sciences that are relevant to this research. Although databases, like PubMed, focus more on the biomedical field, and the Web of Science has a broad historical scope, using additional databases can result in variations in the number of articles found as well as a more diverse coverage of topics.
Articles included in this analysis met the following inclusion criteria: published in Scopus-indexed journals, focused on hospital and ICU management, written in English, classified within the fields of medical and social sciences, and available in open or limited access. Meanwhile, excluded articles are those that are not journal articles, such as editorials, conference proceedings, or brief reviews, irrelevant to the main topic, and not available in full text.
The bibliometric analysis also included an evaluation of citation metrics, such as the total number of citations for each article, the impact factor of the journal in which the article was published, and the h-index of the lead author. This metric is used to identify publications that have a significant influence in the field of hospital management and intensive care [28]. To refine the data for this study, the authors applied a specific formula to narrow the results, ultimately selecting 203 articles from a total of 663 scientific papers (Figure 1). These articles were identified using the keywords “hospital management” and “Intensive Care Unit.” The data reduction process was carried out using the search and filtering capabilities of the Scopus database: (Title-Abs-Key (“Hospital Management”) And Title-Abs-Key (“Intensive Care Unit”)) And Pubyear > 2014 And Pubyear < 2023 And (Limit To (Doctype, “Ar”)) And (Limit To (Pubstage, “Final”)) And (Limit To (Srctype, “J”)) And (Limit To (Language, “English”)) And (Limit To (Oa, “All”)) And (Limit To (Subjarea, “Medi”) Or Limit To (Subjarea, “Soci”)).
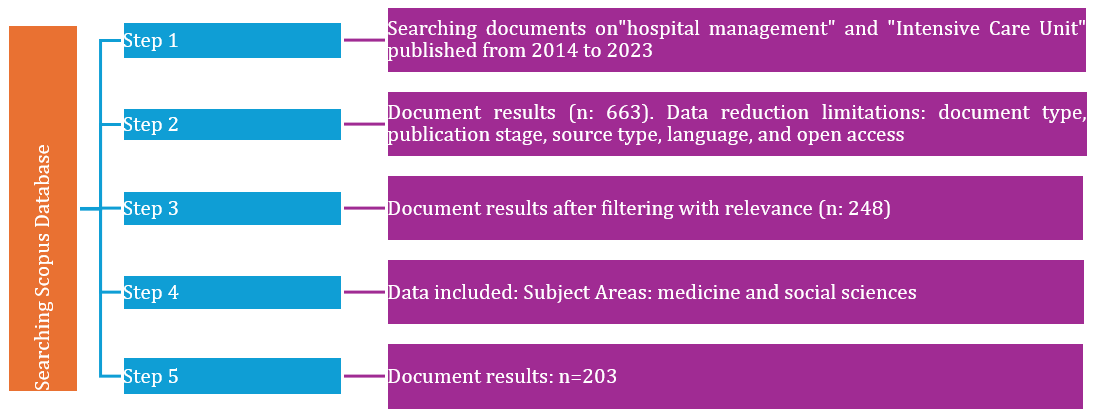
Figure 1. The PRISMA flow diagram used to identify, screen, and include papers for our bibliometric review (2025)
Findings
It is very important to present the results to the public in the context of hospital and ICU management. This process is crucial for gaining a comprehensive understanding of research trends, advancements, and future opportunities in the field of hospital and ICU management. By systematically analyzing the literature, it becomes possible to identify key insights, emerging themes, and areas that require further exploration, ultimately contributing to the advancement of knowledge and practices in this critical domain [29]. This condition aligns with the vital role of hospital and ICU management in maintaining the quality of health services; this analysis serves as an important foundation for researchers, hospital managers, and policymakers. A key finding was revealing the main trends, and focusing on hospital and ICU management. Bibliometric analysis illustrates how specific topics, such as management technology, resource efficiency, patient safety, and decision-making systems, evolve [30]. A total of 203 articles were selected for evaluation. The top ten countries identified were the United States (48%), the United Kingdom (17%), China (12%), Italy (11%), and Canada (10%; Table 1).
Table 1. Characteristics of research conducted on hospital and intensive care unit management
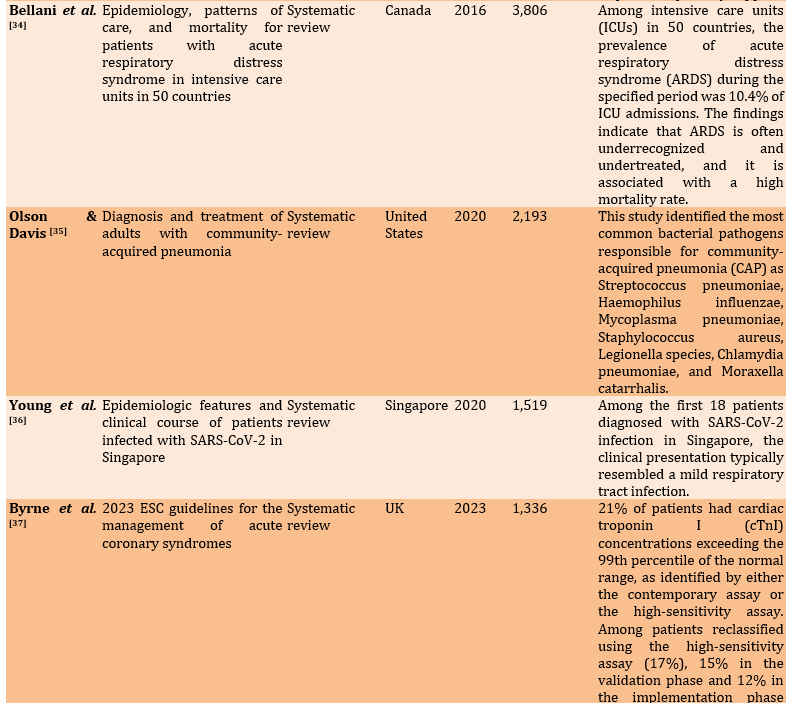
Improvement, severe care, assessment, recommendations, challenges, and healthcare providers were among the factors identified as related to integrated hospital and ICU management (Table 2).
Table 2. Factors related to the integrated hospital and intensive care unit management
Maintaining and enhancing various factors in hospital management and the ICU ensures the delivery of optimal care to hospital patients. These factors are critical for improving service quality, patient outcomes, and overall operational efficiency in healthcare settings. Hospital services can follow developments in facilities and hospital management systems that prioritize the efficiency and effectiveness of services in the ICU. This broad research perspective focuses on past, present, and emerging trends. In greater depth, the author analyzed and mapped the big data results from Scopus with relevant themes from 2014 to 2023.
The data revealed a consistent and significant rise in the number of publications in recent years, reflecting growing research activity and interest in the field (Figure 2). This underscores the increasingly relevant theme of hospital and ICU management. The following visualization presents the progress of the study of hospital and ICU management over the last ten years. There have been significant fluctuations in the number of publications per year, with some years showing notable increases while others experienced decreases. At the beginning of the period, specifically in 2014 and 2015, the number of publications was relatively low, at seven. In 2016, there was a slight increase to 11 publications, but this declined back to seven in 2017. The following year, 2018, also saw a further decline to ten publications. Starting in 2019, there was a more pronounced upward trend, with the number of publications rising to 17, and then to 18 in 2020. In 2021, there was a significant jump, reaching 46 publications, which is the highest number during the period shown. This surge may be related to the COVID-19 pandemic, which has made the topic of hospital and ICU management even more critical, thereby attracting greater research interest. The conditions that arose worldwide in 2021 were a direct impact of the COVID-19 pandemic, leading to a crisis in ICU capacity, including the availability of ICU beds, ventilators, and medical resources. As a result, hospital management moved more swiftly to develop new treatment protocols for COVID-19 patients, including the management of critical patients, the use of PPE, and measures to prevent transmission in healthcare facilities.
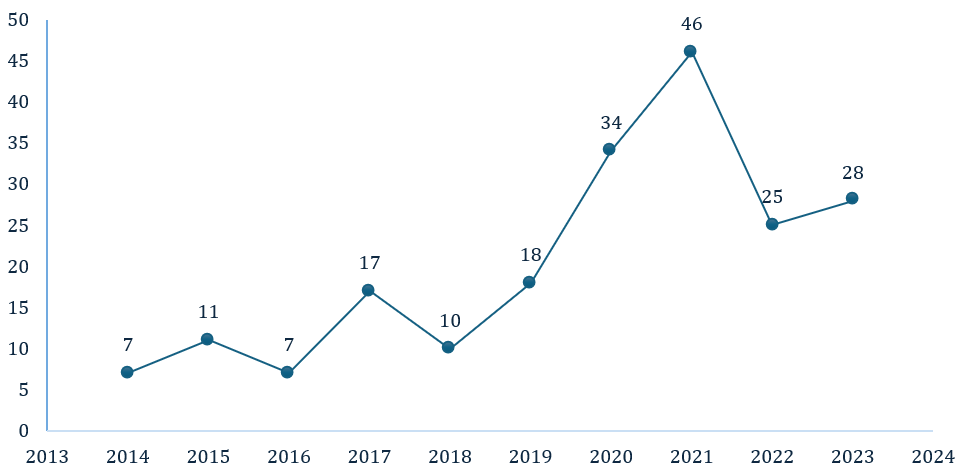
Figure 2. Publication by year (2012-2024)
However, after its peak in 2021, there was a decline in the number of publications in 2022, with the figure dropping to 25. In 2023, there was a slight increase back to 28 publications, although this was still well below the high number reached in 2021. Overall, publication trends show a fluctuating increase in interest in this topic, with a sharp rise during the pandemic. This reflects how urgent global conditions, such as the pandemic, can affect the focus of research in the health sector. The increase in 2023, although small, indicates that this topic still holds relevance and attracts attention in research among academics and healthcare practitioners. Our findings map countries that are significantly concerned with hospital and ICU management in detail (Figure 3).
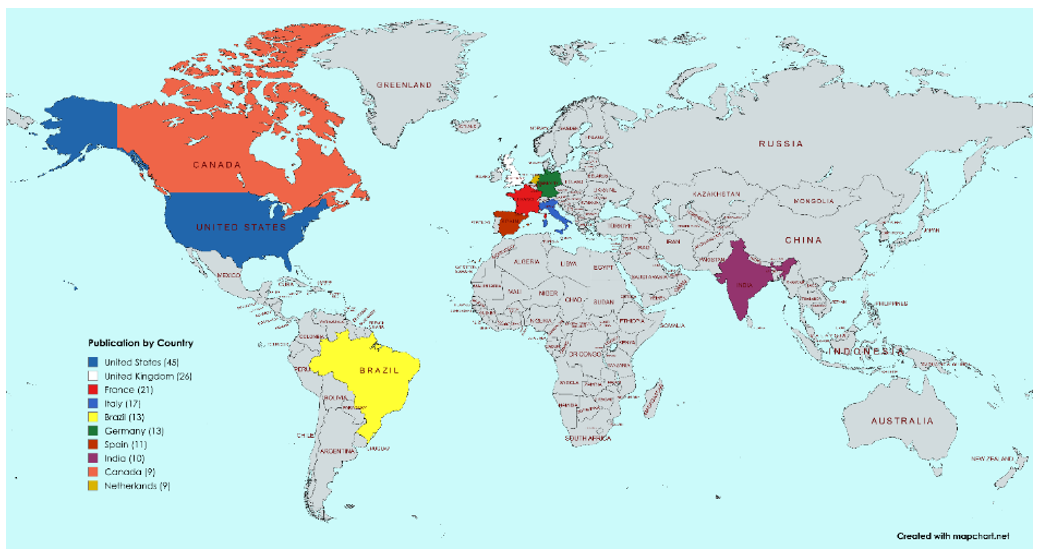
Figure 3. Academic production by country, from 2014-2023 (Software Mapchart)
The United States was among the countries with the highest concentration of research activity in the world, highlighting its prominent role and contributions in the field being studied. The United States showed a strong interest in developing health services, infrastructure, and its well-developed healthcare system. This situation is relevant because the United States has also become a center for global health research; thus, it is unsurprising that this country has the highest concentration of efforts to encourage progress in hospital management and ICU health services. The United States has prioritized technological sophistication in addressing health problems to promote competitive hospital services, including those aimed at treating elderly individuals with disabilities [54].
In second place was England, with 26 publications. In its efforts to enhance health management services in hospitals and ICU settings, the UK emphasized communication strategies, patient self-monitoring, and remote patient tracking as key priorities. These approaches aim to improve care quality, patient engagement, and operational efficiency in healthcare delivery [55]. Meanwhile, the Netherlands ranked tenth in the world with a research focus on hospital and ICU management, examining trends and future research. The management of hospital and ICU health services is crucial for addressing diseases that have impacted the global community; the Netherlands prioritizes collaboration in hospital services to consolidate the innovative results of various experts [56]. One of the large-scale collaborations undertaken in the Netherlands involves managing COVID-19, which is an international challenge [57]. Overall, both developed and developing countries with substantial health infrastructure and populations were demonstrating significant interest in this research topic. Furthermore, the author analyzes the mapping of hospital management in greater depth, highlighting important points and network relationships within this research issue (Figure 4).
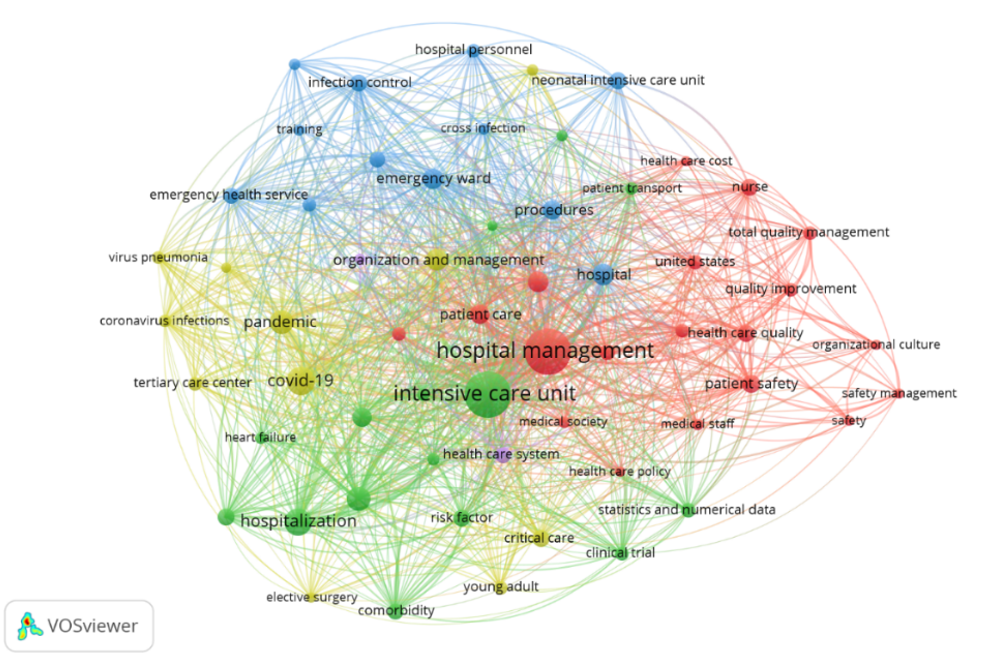
Figure 4. Hospital and intensive care unit management research trends (2014-2023)
Hospital management was the main focus, and there was a close relationship with the ICU. One of the most highlighted issues is related to nurse fatigue in providing medical services to patients, particularly on the African continent, where Ghana had a fatigue score reaching 76.43±27.80 out of 124 [58]. These findings underscore the importance of issues related to emergency health services, safety management in hospitals, and critical care to promote quality hospital and ICU management in the future [59].
Next, the colors in this visualization indicated the publication timeline or popularity of the themes from 2018 to 2021, with a color gradient ranging from blue (2018) to yellow (2021). Themes, such as infection control, cross-infection, health care cost, organizational culture, and patient safety, represented the initial focus in the literature on hospital and ICU management, particularly concerning infection prevention and cost control. In 2019, the focus began to shift toward emergency care and risk management, especially in relation to tertiary care and service quality improvement. The light green color highlights the surge in research in 2020 related to the COVID-19 pandemic. These keywords suggest that the pandemic is drastically changing priorities in hospital management and increasing the focus on how hospitals handle patient surges, particularly concerning intensive care and viral infections. In 2021, attention shifted to the overall management of hospitals and ICUs, with an emphasis on optimal patient care, total quality management, and effective health policies. The themes that appear in different colors and years reflected the evolution of research focus in the field of hospital and ICU management.
On the other hand, training, infection control, risk factor critical care, health care cost, and nurse and safety management tended to appear on the outermost side of the visualization, suggesting that these terms have not been widely researched or have less relevance to the main terms. Specifically, this indicates that the area was still open for further research. Future studies can explore the relationships and interactions between each of these keywords and Hospital and ICU management. By deeply understanding these interactions, subsequent research can identify new strategies to improve patient safety, enhance service standards, and increase the efficiency of information management in the ICU environment. Therefore, further research in this field will not only expand our understanding of effective hospital management but can also provide a foundation for the improvement of the public health system.
The yellow color in Figure 5 indicated the most frequently discussed topics. The denser the keywords surrounded by yellow, the more research has focused on this perspective. Conversely, if the yellow color is not concentrated around a keyword, it suggests that the topic has not been widely discussed in the research. Therefore, these keywords can be used as a novelty in future studies. Hospital management, ICU, pandemic, COVID-19, hospitalization, patient care, patient safety, and organization management formed a dense group, indicating that these terms are frequently associated or addressed together in the literature under analysis. This suggested a strong thematic connection or recurring focus on these concepts within the research being examined. Meanwhile, keywords, such as training, infection control, risk factor critical care, health care cost, nurse, and safety management, tended to appear on the outer side of the visualization, suggesting that these terms have not been widely researched or have less relevance to the main terms. Specifically, this indicates that the area is still open for further research. Further studies in this area hold the potential to offer new insights and deepen our understanding of the connections between various aspects of nurse resilience and related concepts in Public Health and health management. Such research could enhance strategies for supporting healthcare professionals and improving overall health systems.
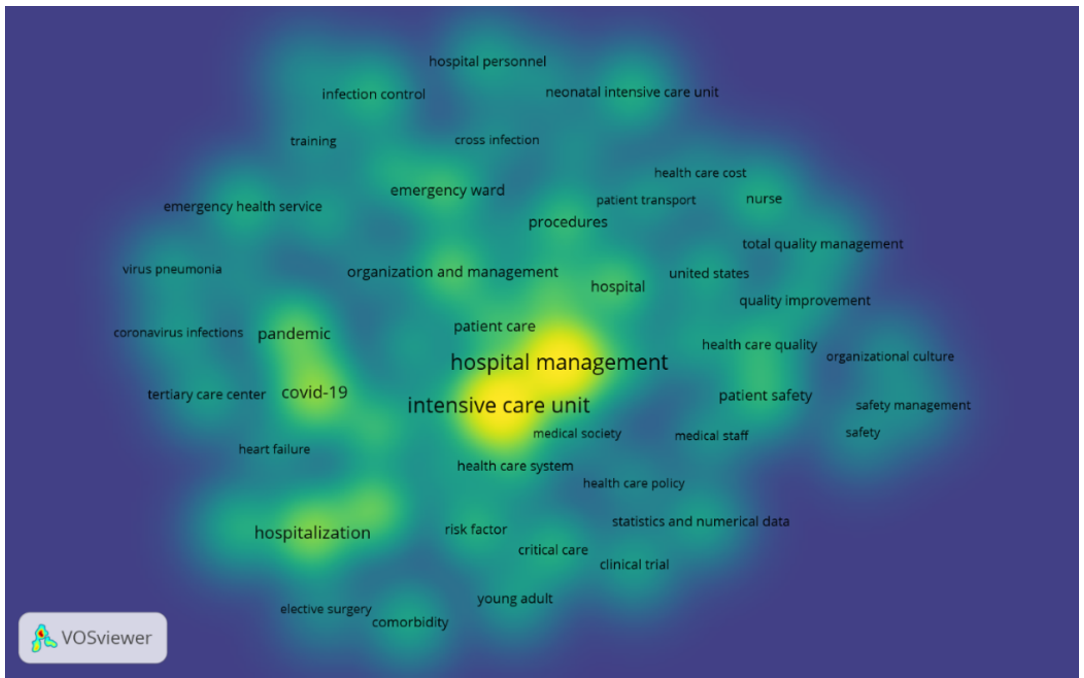
Figure 5. Research agenda and future research of nurse resilience (2014-2023)
Furthermore, keywords, such as patient care, health care system, health care policy, medical staff, patient safety, COVID-19, hospitalization, and emergency ward [60], had the highest occurrence and showed the most vital relationship with research on hospital and ICU management. Patient care, along with the topics of hospital and ICU management, was intertwined because the main focus of hospital management is to ensure the best quality of care for each patient, especially in the ICU [61]. The ICUs aim to provide intensive monitoring and care for critical patients; therefore, effective management is needed to ensure that the needs of each patient are met optimally [4]. The Health Care System is interrelated with hospital and ICU management because an effective health system serves as the foundation for the overall management and operation of the hospital [1]. The management of ICUs requires strong support from the health system regarding resource procurement, procedural arrangements, and coordination between departments to ensure a rapid response and high quality of care. Health care policy is interconnected with the topics of hospital and ICU management because health policy establishes the standards, regulations, and guidelines that must be adhered to in hospital management, including in the ICU [62].
These policies govern various aspects, such as staff qualifications, safety standards, and treatment procedures, which directly impact how ICU management is implemented to achieve optimal treatment outcomes [63]. Medical staff members are interrelated with hospital and ICU management because medical personnel are the core of ICU operations and are responsible for treating patients in critical condition. Effective management must ensure adequate staffing, appropriate qualifications, clearly defined tasks, and specialized training so that medical personnel can carry out their duties efficiently and safely in a stressful environment such as the ICU. Patient safety, hospital management, and ICUs are interconnected because patient safety is a top priority in hospital operations, especially in ICUs that handle high-risk patients. Hospital management is responsible for implementing safety protocols and standards of care to reduce the risk of medical errors, infections, or other complications that can harm patients; thus, maintaining patient safety is the main focus of ICU management [64].
Discussion
This study aimed to analyze the trends and developments in the field of hospital and intensive care unit management based on bibliometric data from 2014 to 2023. In recent years, research on hospital and ICU management has become significant, as the ICU is a crucial factor in hospital management. During the period from 2014 to 2023, there was a significant increasing trend in the number of publications indexed by Scopus on hospital and ICU management, with a notable rise from 2019 to 2021. In 2019, researchers reviewed hospital and ICU management in terms of patient safety [65] and health information technology (IT) [66]. These findings illustrate that patient safety and health IT play important roles in supporting hospital and ICU management. Patient safety is a fundamental aspect of providing high-quality healthcare and reducing the risk of injury or medical errors, especially in critical environments such as ICUs. The use of health IT, such as electronic medical records, real-time patient monitoring systems, and data analysis tools, helps reduce errors, accelerate clinical responses, and improve medical team coordination. The combination of a focus on patient safety and the implementation of health IT enables hospital management to be more efficient in managing resources, optimizing workflows, and improving data-driven clinical decision-making [67, 68].
In 2020, researchers studied hospital and ICU management in terms of critical care costs and the COVID-19 pandemic [69], illustrating that critical care costs and the COVID-19 pandemic are closely related in the context of hospital and ICU Management. The COVID-19 pandemic has led to a surge in the need for critical care services worldwide, which, in turn, has a direct impact on critical care costs. ICUs must operate under high pressure to care for a large number of patients with severe symptoms, necessitating the use of ventilators, specialized medications, and other medical resources. These increased costs include expenditures on medical equipment, PPE, the need for additional healthcare workers, and the costs associated with maintaining intensive care facilities, all of which continue to rise. The relationship between critical care costs and the COVID-19 pandemic also highlights the need for hospital management to have a preparedness strategy for dealing with crisis situations.
Finally, in 2021, researchers frequently reviewed hospital and ICU management in terms of risk factors [70] and medical staff [71], illustrating that risk factors and medical staff are important links in hospital and ICU management. Risk factors refer to elements that can increase the likelihood of complications or the worsening of a patient’s condition in intensive care. In the context of hospital management, the relationship between risk factors and medical staff underscores the importance of ongoing training, meeting the needs of healthcare workers, and providing optimal resource support. These steps are essential for improving patient care and ensuring the well-being of the medical team [72]. Hospitals need to ensure that medical staff have access to effective monitoring technologies and tools to help manage risk proactively. Countries have made significant contributions to hospital and ICU management. The United States leads in the number of publications on this topic, with a total of 45 publications recorded. This highlights the significant contribution and active involvement in research in this area [73]. It indicates that the United States has a strong interest and focus on the topic of hospital and ICU management. As a country with a diverse population and complex health challenges, such as high rates of obesity, chronic diseases, and elevated hospitalization rates, the United States requires a robust hospital and intensive care management system. This situation has been further amplified by the COVID-19 pandemic, which has increased the need for a responsive and adaptive health system. The challenges arising from the pandemic have prompted researchers and medical practitioners in the United States to focus more on finding new ways to improve the efficiency of ICU care, optimize hospital resources, and enhance workflows within the health system. This study suggests that there is an urgency to continue developing and improving the health system, especially regarding hospital and ICU management [74]. Research on hospital and ICU management often involves the development and implementation of new technologies, such as artificial intelligence-based patient monitoring systems, telemedicine devices, and advanced health data management systems [75].
The study has strengths and weaknesses that must be considered. By leveraging only the Scopus database, which consists of leading journals that have undergone a rigorous peer-review process, and by applying bibliometric techniques, this study provides a versatile, reasonable, and insightful analysis that allows for a quick understanding of research trends and opportunities for novelty [76]. This study has several theoretical contributions. First, it offers a comprehensive review of Hospital Management and ICUs, which are often underexplored. Second, the findings are supported by empirical data demonstrating improvements in the quality of health care through increased awareness of ICU management practices. Finally, this study provides insights that encourage wider adoption of ICU management in the realm of hospital management [77].
Research on hospital and ICU management is important due to its crucial role in improving healthcare efficiency, optimizing resources, and ensuring patient safety in high-risk environments. The trend of increasing publications over the past decade indicates that this issue is becoming increasingly relevant, especially in light of global challenges, such as the COVID-19 pandemic, limited medical personnel, and the need for the application of more sophisticated health technologies. However, there are still gaps in existing research. Most studies focus on specific aspects, such as patient safety, health information technology, and the cost of critical care, but there is still limited exploration of the effectiveness of data-driven management strategies, the impact of health policies on ICUs, and the influence of socio-economic factors in intensive care. Future research may lead to a deeper analysis of how evidence-based management strategies can improve hospital efficiency and how data-driven prediction systems can help optimize resource allocation. For future bibliometric studies, it is recommended to incorporate machine learning techniques in the analysis of research trends. This method can help identify hidden patterns, relationships between topics, and predict the direction of future research more accurately.
Although this study successfully explained the research development map in hospital and ICU management, it has limitations regarding data sources. The analyzed data were drawn from only one database. Further studies need to include other databases, such as Web of Science, Dimension, Connected Papers, Open Knowledge Maps, and PubMed [78]. Bibliometric studies also have other limitations, including self-citation bias, where some authors or institutions repeatedly cite their own work, which can affect the results of citation trend analysis. In addition, the database used (Scopus) may not include all relevant articles from unindexed journals, potentially leading to limitations in the generalization of findings.
The research has important implications for a wide range of stakeholders in the health sector, including hospital administrators, medical researchers, and policymakers. For hospital administrators, the identified research trends can serve as a basis for the planning and management of ICUs. For example, the increasing focus on patient health and safety information technology indicates the need to invest in real-time patient monitoring systems and electronic medical records to improve efficiency and reduce medical errors. Additionally, understanding the patterns of critical care costs and the impact of the pandemic on ICU capacity can help hospitals allocate resources more effectively, both in normal situations and during health crises.
For medical researchers, the results of this study identified gaps in research that could present opportunities for further exploration. Some areas that remain underexplored include the analysis of the effectiveness of data-driven management strategies in ICUs, the influence of health policies on hospital efficiency, and the impact of socio-economic factors on intensive care. By understanding research trends, researchers can develop studies that are more relevant to current and future needs, as well as generate innovations in critical care systems.
For policymakers, the findings of this study can be used as a foundation for formulating health policies, particularly in the allocation of funding. Given research trends indicating that patient safety and health technology play important roles in ICU management, policymakers can consider increasing funding for research and the implementation of technologies that can support the efficiency and quality of critical care. Furthermore, the increased attention to the cost of critical care during the pandemic demonstrates the need for a more flexible and responsive healthcare financing strategy for emergency situations. By understanding existing research trends and gaps, all stakeholders can contribute to improving the quality of ICU services in terms of management, research, and public policy.
Conclusion
Bibliometric analysis reveals a significant increase in the number of publications from 2019 to a peak in 2021, reflecting how global conditions, such as the pandemic, have influenced research focus.
Acknowledgments: The authors appreciate all the assistance they received in developing and revising this work.
Ethical Permissions: Not applicable, as the researcher uses secondary data that has been anonymized and is publicly available. There is no direct interaction with the research participants; thus, additional ethical clearance is not required.
Conflicts of Interests: The authors declared no conflicts of interests.
Authors' Contribution: Rahmat M (First Author), Introduction Writer/Methodologist/Statistical Analyst (70%); Aini O (Second Author), Statistical Analyst/Discussion Writer (30%)
Funding/Support: This research received no external funding.
Keywords:
References
1. Ginter PM, Duncan WJ, Swayne LE. The strategic management of health care organizations. Canada: John Wiley & Sons; 2018. [Link]
2. Zingg W, Holmes A, Dettenkofer M, Goetting T, Secci F, Clack L, et al. Hospital organisation, management, and structure for prevention of health-care-associated infection: A systematic review and expert consensus. Lancet Infect Dis. 2015;15(2):212-24. [Link] [DOI:10.1016/S1473-3099(14)70854-0]
3. Capuzzo M, Volta C, Tassinati T, Moreno R, Valentin A, Guidet B, et al. Hospital mortality of adults admitted to Intensive Care Units in hospitals with and without Intermediate Care Units: A multicentre European cohort study. Crit Care. 2014;18(5):551. [Link] [DOI:10.1186/s13054-014-0551-8]
4. Marshall JC, Bosco L, Adhikari NK, Connolly B, Diaz JV, Dorman T, et al. What is an intensive care unit? A report of the task force of the World Federation of Societies of Intensive and Critical Care Medicine. J Crit Care. 2017;37:270-6. [Link] [DOI:10.1016/j.jcrc.2016.07.015]
5. James FR, Power N, Laha S. Decision-making in intensive care medicine-A review. J Intensive Care Soc. 2018;19(3):247-58. [Link] [DOI:10.1177/1751143717746566]
6. Griffin KM, Karas MG, Ivascu NS, Lief L. Hospital preparedness for COVID-19: A practical guide from a critical care perspective. Am J Respir Crit Care Med. 2020;201(11):1337-44. [Link] [DOI:10.1164/rccm.202004-1037CP]
7. Inoue S, Hatakeyama J, Kondo Y, Hifumi T, Sakuramoto H, Kawasaki T, et al. Post-intensive care syndrome: Its pathophysiology, prevention, and future directions. Acute Med Surg. 2019;6(3):233-46. [Link] [DOI:10.1002/ams2.415]
8. Pamplin J, Nemeth CP, Serio-Melvin ML, Murray SJ, Rule GT, Veinott ES, et al. Improving clinician decisions and communication in critical care using novel information technology. Mil Med. 2020;185(1-2):e254-61. [Link]
9. He J, Baxter SL, Xu J, Xu J, Zhou X, Zhang K. The practical implementation of artificial intelligence technologies in medicine. Nat Med. 2019;25(1):30-6. [Link] [DOI:10.1038/s41591-018-0307-0]
10. Gholami B, Haddad WM, Bailey JM. AI in the ICU: In the intensive care unit, artificial intelligence can keep watch. IEEE Spectrum. 2018;55(10):31-5. [Link] [DOI:10.1109/MSPEC.2018.8482421]
11. Gluyas H. Effective communication and teamwork promotes patient safety. Nurs Stand. 2015;29(49):50-7. [Link] [DOI:10.7748/ns.29.49.50.e10042]
12. Schultz MJ, Dunser MW, Dondorp AM, Adhikari NK, Iyer S, Kwizera A, et al. Current challenges in the management of sepsis in ICUs in resource-poor settings and suggestions for the future. Intensive Care Med. 2017;43(5):612-24. [Link] [DOI:10.1007/s00134-017-4750-z]
13. Curtis JR, Engelberg RA, Bensink ME, Ramsey SD. End-of-life care in the intensive care unit: Can we simultaneously increase quality and reduce costs?. Am J Respir Crit Care Med. 2012;186(7):587-92. [Link] [DOI:10.1164/rccm.201206-1020CP]
14. Longo MC. Good practices in health care "management experimentation models": Insights from an international public-private partnership on transplantation and advanced specialized therapies. Adv Health Care Manag. 2015;17:71-115. [Link] [DOI:10.1108/S1474-823120140000017005]
15. Pierre MS, Grawe P, Bergstrom J, Neuhaus C. 20 years after To Err Is Human: A bibliometric analysis of 'the IOM report's' impact on research on patient safety. Saf Sci. 2022;147:105593. [Link] [DOI:10.1016/j.ssci.2021.105593]
16. Koseoglu MA, Akdeve E, Gedik İ, Bertsch A. A bibliometric analysis of strategic management articles in healthcare management literature: Past, present, and future. Int J Healthc Manag. 2015;8(1):27-33. [Link] [DOI:10.1179/2047971914Y.0000000089]
17. Matlakala MC, Bezuidenhout MC, Botha AD. Strategies to address management challenges in larger intensive care units. J Nurs Manag. 2015;23(7):945-53. [Link] [DOI:10.1111/jonm.12240]
18. Poncette AS, Spies C, Mosch L, Schieler M, Weber-Carstens S, Krampe H, et al. Clinical requirements of future patient monitoring in the intensive care unit: Qualitative study. JMIR Med Inform. 2019;7(2):e13064. [Link] [DOI:10.2196/13064]
19. Donovan AL, Aldrich JM, Gross AK, Barchas DM, Thornton KC, Schell-Chaple HM, et al. Interprofessional care and teamwork in the ICU. Crit Care Med. 2018;46(6):980-90. [Link] [DOI:10.1097/CCM.0000000000003067]
20. Rasouli A, Ketabchi M. Identifying and explaining the components of organizational culture in Baharloo hospital in Tehran and providing a solution to tackle the challenges: A qualitative study. Health Manag Inf Sci. 2023;10(3):130-8. [Link]
21. Labarère J, Renaud B, Fine MJ. How to derive and validate clinical prediction models for use in intensive care medicine. Intensive Care Med. 2014;40(4):513-27. [Link] [DOI:10.1007/s00134-014-3227-6]
22. Saghafian S, Austin G, Traub SJ. Operations research/management contributions to emergency department patient flow optimization: Review and research prospects. IIE Trans Healthc Syst Eng. 2015;5(2):101-23. [Link] [DOI:10.1080/19488300.2015.1017676]
23. Dharmani P, Das S, Prashar S. A bibliometric analysis of creative industries: Current trends and future directions. J Bus Res. 2021;135(2):252-67. [Link] [DOI:10.1016/j.jbusres.2021.06.037]
24. Patrick Z, Hee OC. A bibliometric analysis of global online marketing research trends. Int J Acad Res Bus Soc Sci. 2020;10(5):770-87. [Link] [DOI:10.6007/IJARBSS/v10-i5/7248]
25. Iqbal W, Qadir J, Tyson G, Mian AN, Ul Hassan S, Crowcroft J. A bibliometric analysis of publications in computer networking research. Scientometrics. 2019;119(2):1121-55. [Link] [DOI:10.1007/s11192-019-03086-z]
26. Yoon B, Park I, Yun D, Park G. Exploring promising vacant technology areas in a technology-oriented company based on bibliometric analysis and visualization. Technol Anal Strateg Manag. 2019;31(4):388-405. [Link] [DOI:10.1080/09537325.2018.1516864]
27. Medina E, Mazaira A, Alén E. Innovation in the broadcasters' business model: A bibliometric and review approach. Eur Res Manag Bus Econ. 2022;28(3):100202. [Link] [DOI:10.1016/j.iedeen.2022.100202]
28. Baas J, Schotten M, Plume A, Côté G, Karimi R. Scopus as a curated, high-quality bibliometric data source for academic research in quantitative science studies. Quant Sci Stud. 2020;1(1):377-86. [Link] [DOI:10.1162/qss_a_00019]
29. Ekong M, Monga TS, Daher JC, Sashank M, Soltani SR, Nwangene NL, et al. From the intensive care unit to recovery: Managing post-intensive care syndrome in critically ill patients. Cureus. 2024;16(5):e61443. [Link] [DOI:10.7759/cureus.61443]
30. Khanuja A, Sreedharan R, Sharma N. Bibliometric analysis on usage of industry 4.0 technologies in healthcare. TQM J. 2024;1(1):252. [Link] [DOI:10.1108/TQM-08-2023-0252]
31. Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;180(7):934-43. [Link] [DOI:10.1001/jamainternmed.2020.0994]
32. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: The task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37(27):2129-200. [Link] [DOI:10.1093/eurheartj/ehw128]
33. Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. 2020;323(16):1574-81. [Link] [DOI:10.1001/jama.2020.5394]
34. Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016;315(8):788-800. [Link] [DOI:10.1001/jama.2016.0291]
35. Olson G, Davis AM. Diagnosis and treatment of adults with community-acquired pneumonia. JAMA. 2020;323(9):885-6. [Link] [DOI:10.1001/jama.2019.21118]
36. Young BE, Ong SWX, Kalimuddin S, Low JG, Tan SY, Loh J, et al. Epidemiologic features and clinical course of patients infected with SARS-CoV-2 in Singapore. JAMA. 2020;323(15):1488-94. [Link] [DOI:10.1001/jama.2020.3204]
37. Byrne RA, Rossello X, Coughlan JJ, Barbato E, Berry C, Chieffo A, et al. 2023 ESC guidelines for the management of acute coronary syndromes. Eur Heart J. 2023;44(38):3720-826. [Link] [DOI:10.1093/eurheartj/ehad191]
38. Mouncey PR, Osborn TM, Power GS, Harrison DA, Sadique MZ, Grieve RD, et al. Trial of early, goal-directed resuscitation for septic shock. N Engl J Med. 2015;372(14):1301-11. [Link] [DOI:10.1056/NEJMoa1500896]
39. Liu Q, Luo D, Haase JE, Guo Q, Wang XQ, Liu S, et al. The experiences of health-care providers during the COVID-19 crisis in China: A qualitative study. Lancet Glob Health. 2020;8(6):e790-8. [Link] [DOI:10.1016/S2214-109X(20)30204-7]
40. Liang W, Liang H, Ou L, Chen B, Chen A, Li C, et al. Development and validation of a clinical risk score to predict the occurrence of critical illness in hospitalized patients with COVID-19. JAMA Intern Med. 2020;180(8):1081-9. [Link] [DOI:10.1001/jamainternmed.2020.2033]
41. Supic ZT, Bjegovic V, Marinkovic J, Milicevic MS, Vasic V. Hospital management training and improvement in managerial skills: Serbian experience. Health Policy. 2010;96(1):80-9. [Link] [DOI:10.1016/j.healthpol.2010.01.002]
42. Karatas M, Eriskin L, Deveci M, Pamucar D, Garg H. Big data for healthcare industry 4.0: Applications, challenges and future perspectives. Expert Syst Appl. 2022;200:116912. [Link] [DOI:10.1016/j.eswa.2022.116912]
43. Herraiz-Recuenco L, Alonso-Martínez L, Hannich-Schneider S, Puente-Alcaraz J. Causes of stress among healthcare professionals and successful hospital management approaches to mitigate it during the COVID-19 pandemic: A cross-sectional study. Int J Environ Res Public Health. 2022;19(19):12963. [Link] [DOI:10.3390/ijerph191912963]
44. Al-Amin M, Makarem SC, Rosko M. Efficiency and hospital effectiveness in improving hospital consumer assessment of healthcare providers and systems ratings. Health Care Manage Rev. 2016;41(4):296-305. [Link] [DOI:10.1097/HMR.0000000000000076]
45. Farmakis D, Parissis J, Karavidas A, Karvounis C, Triposkiadis F, Filippatos G, et al. In-hospital management of acute heart failure: Practical recommendations and future perspectives. Int J Cardiol. 2015;201:231-6. [Link] [DOI:10.1016/j.ijcard.2015.08.030]
46. Andry JF, James S, Christian S, Dela H. Evaluation and recommendation IT governance in hospital base on COBIT framework. Int J Open Inf Technol. 2019;7(5):51-8. [Link]
47. Dash S, Shakyawar SK, Sharma M, Kaushik S. Big data in healthcare: Management, analysis and future prospects. J Big Data. 2019;6(1):54. [Link] [DOI:10.1186/s40537-019-0217-0]
48. Krampe H, Denke C, Gülden J, Mauersberger VM, Ehlen L, Schönthaler E, et al. Perceived severity of stressors in the intensive care unit: A systematic review and semi-quantitative analysis of the literature on the perspectives of patients, health care providers and relatives. J Clin Med. 2021;10(17):3928. [Link] [DOI:10.3390/jcm10173928]
49. Noome M, Beneken Genaamd Kolmer DM, Van Leeuwen E, Dijkstra BM, Vloet LC. The nursing role during end-of-life care in the intensive care unit related to the interaction between patient, family and professional: An integrative review. Scand J Caring Sci. 2016;30(4):645-61. [Link] [DOI:10.1111/scs.12315]
50. Gutierrez C, Brown ART, Herr MM, Kadri SS, Hill B, Rajendram P, et al. The chimeric antigen receptor-intensive care unit (CAR-ICU) initiative: Surveying intensive care unit practices in the management of CAR T-cell associated toxicities. J Crit Care. 2020;58:58-64. [Link] [DOI:10.1016/j.jcrc.2020.04.008]
51. Jackson JC, Santoro MJ, Ely TM, Boehm L, Kiehl AL, Anderson LS, et al. Improving patient care through the prism of psychology: Application of Maslow's hierarchy to sedation, delirium, and early mobility in the intensive care unit. J Crit Care. 2014;29(3):438-44. [Link] [DOI:10.1016/j.jcrc.2014.01.009]
52. Liébana-Rodríguez M, Recacha-Villamor E, Díaz-Molina C, Pérez-Palacios P, Martín-Hita L, Enríquez-Maroto F, et al. Outbreaks by Klebsiella oxytoca in neonatal intensive care units: Analysis of an outbreak in a tertiary hospital and systematic review. ENFERMEDADES INFECCIOSAS Y MICROBIOLOGIA CLINICA. 2024;42(6):294-301. [Link] [DOI:10.1016/j.eimce.2023.04.018]
53. Wunderlich MM, Frey N, Amende-Wolf S, Hinrichs C, Balzer F, Poncette AS. Alarm management in provisional COVID-19 intensive care units: Retrospective analysis and recommendations for future pandemics. JMIR Med Inform. 2024;12:e58347. [Link] [DOI:10.2196/58347]
54. HU W, Qutayan SMSB, Othman MDDNB. Influence of digital health technologies among healthcare providers on long-term care services implementation for elderly with disabilities. J Ecohumanism. 2024;3(6):1412-21. [Link] [DOI:10.62754/joe.v3i6.4119]
55. Holt G, Hughes D. Consensus study on UK weight management services' response to COVID-19: Best practices in outpatient management, governance and digital solutions. J Hum Nutr Diet. 2024;37(5):1255-64. [Link] [DOI:10.1111/jhn.13346]
56. Hesselink G, Verhage R, Van Der Horst ICC, Van Der Hoeven H, Zegers M. Consensus-based indicators for evaluating and improving the quality of regional collaborative networks of intensive care units: Results of a nationwide Delphi study. J Crit Care. 2024;79:154440. [Link] [DOI:10.1016/j.jcrc.2023.154440]
57. Van Alphen A, Lekkerkerker C, Van Exel J, De Jong RB, Ahaus K. Patients' perspectives on ethical principles to fairly allocate scarce surgical resources during the COVID-19 pandemic in the Netherlands: A Q-methodology study. BMJ Open. 2024;14(9):e086681. [Link] [DOI:10.1136/bmjopen-2024-086681]
58. Nyarko BA, Yin Z, Chai X, Yue L. Nurses' alarm fatigue, influencing factors, and its relationship with burnout in the critical care units: A cross-sectional study. Aust Crit Care. 2024;37(2):273-80. [Link] [DOI:10.1016/j.aucc.2023.06.010]
59. Masud FN, Sasangohar F, Ratnani I, Fatima S, Hernandez MA, Riley T, et al. Past, present, and future of sustainable intensive care: Narrative review and a large hospital system experience. Crit Care. 2024;28(1):154. [Link] [DOI:10.1186/s13054-024-04937-9]
60. Leonardi R, Bellinzoni P, Broglia L, Colombo R, De Marchi D, Falcone L, et al. Hospital care in departments defined as COVID-free: A proposal for a safe hospitalization protecting healthcare professionals and patients not affected by COVID-19. ARCHIVIO ITALIANO DI UROLOGIA E ANDROLOGIA. 2020;92(2):67-72. [Link] [DOI:10.4081/aiua.2020.2.67]
61. Bai J, Fügener A, Schoenfelder J, Brunner JO. Operations research in intensive care unit management: A literature review. Health Care Manag Sci. 2018;21(1):1-24. [Link] [DOI:10.1007/s10729-016-9375-1]
62. Thompson DR, Hamilton DK, Cadenhead CD, Swoboda SM, Schwindel SM, Anderson DC, et al. Guidelines for intensive care unit design. Crit Care Med. 2012;40(5):1586-600. [Link] [DOI:10.1097/CCM.0b013e3182413bb2]
63. Nates JL, Nunnally M, Kleinpell R, Blosser S, Goldner J, Birriel B, et al. ICU admission, discharge, and triage guidelines: A framework to enhance clinical operations, development of institutional policies, and further research. Crit Care Med. 2016;44(8):1553-602. [Link] [DOI:10.1097/CCM.0000000000001856]
64. Soori H. Errors in medical procedures. In: Errors in medical science investigations. Singapore: Springer; 2024. p. 205-24. [Link] [DOI:10.1007/978-981-99-8521-0_11]
65. Gomides MDA, Fontes AMS, Silveira AOSM, Sadoyama G. Patient safety culture in the intensive care unit: Cross-study. J Infect Dev Ctries. 2019;13(6):496-503. [Link] [DOI:10.3855/jidc.11166]
66. Orenstein EW, Ferro DF, Bonafide CP, Landrigan CP, Gillespie S, Muthu N. Hidden health IT hazards: A qualitative analysis of clinically meaningful documentation discrepancies at transfer out of the pediatric intensive care unit. JAMIA Open. 2019;2(3):392-8. [Link] [DOI:10.1093/jamiaopen/ooz026]
67. Hashmi M, Taqi A, Memon MI, Ali SM, Khaskheli S, Sheharyar M, et al. A national survey of critical care services in hospitals accredited for training in a lower-middle income country: Pakistan. J Crit Care. 2020;60:273-8. [Link] [DOI:10.1016/j.jcrc.2020.08.017]
68. Yang H, Hao Y, Qi CZ, Chai X, Wu EQ. Estimation of total costs in pediatric and young adult patients with relapsed or refractory acute lymphoblastic leukemia receiving Tisagenlecleucel from a U.S. hospital's perspective. J Manag Care Spec Pharm. 2020;26(8):971-80. [Link] [DOI:10.18553/jmcp.2020.20052]
69. Mendelson M, Booyens L, Boutall A, Cairncross L, Calligaro G, Dave JA, et al. The mechanics of setting up a COVID-19 response: Experiences of the COVID-19 epidemic from Groote Schuur Hospital, Cape Town, South Africa. S Afr Med J. 2020;110(10):968-72. [Link] [DOI:10.7196/SAMJ.2020.v110i10.15215]
70. Presanis AM, Kunzmann K, Grosso FM, Jackson CH, Corbella A, Grasselli G, et al. Risk factors associated with severe hospital burden of COVID-19 disease in Regione Lombardia: A cohort study. BMC Infect Dis. 2021;21(1):1041. [Link] [DOI:10.1186/s12879-021-06750-z]
71. Cai H, Tu B, Ma J, Chen L, Fu L, Jiang Y, et al. Psychological impact and coping strategies of frontline medical staff in Hunan between January and March 2020 during the outbreak of coronavirus disease 2019 (COVID‑19) in Hubei, China. Med Sci Monit. 2020;26:e924171. [Link] [DOI:10.12659/MSM.924171]
72. Søvold LE, Naslund JA, Kousoulis AA, Saxena S, Qoronfleh MW, Grobler C, et al. Prioritizing the mental health and well-being of healthcare workers: An urgent global public health priority. Front Public Health. 2021;9:679397. [Link] [DOI:10.3389/fpubh.2021.679397]
73. Fleischmann-Struzek C, Mellhammar L, Rose N, Cassini A, Rudd KE, Schlattmann P, et al. Incidence and mortality of hospital- and ICU-treated sepsis: Results from an updated and expanded systematic review and meta-analysis. Intensive Care Med. 2020;46(8):1552-62. [Link] [DOI:10.1007/s00134-020-06151-x]
74. Weled BJ, Adzhigirey LA, Hodgman TM, Brilli RJ, Spevetz A, Kline AM, et al. Critical care delivery: The importance of process of care and ICU structure to improved outcomes: An update from the American College of Critical Care Medicine Task Force on Models of Critical Care. Crit Care Med. 2015;43(7):1520-5. [Link] [DOI:10.1097/CCM.0000000000000978]
75. Alshamrani M. IoT and artificial intelligence implementations for remote healthcare monitoring systems: A survey. J King Saud Univ Comput Inf Sci. 2022;34(8):4687-701. [Link] [DOI:10.1016/j.jksuci.2021.06.005]
76. Pascarelli-Romano JM. The effectiveness of a digital literacy curriculum on research literacy and final rubric research outcome scores for English composition students [dissertation]. Chandler: Trident University International; 2020. [Link]
77. Bueno WP, Saurin TA, Wachs P, Kuchenbecker R, Braithwaite J. Coping with complexity in intensive care units: A systematic literature review of improvement interventions. Saf Sci. 2019;118(3):814-25. [Link] [DOI:10.1016/j.ssci.2019.06.023]
78. Singh VK, Singh P, Karmakar M, Leta J, Mayr P. The journal coverage of Web of Science, Scopus and Dimensions: A comparative analysis. Scientometrics. 2021;126(1):5113-42. [Link] [DOI:10.1007/s11192-021-03948-5]