Volume 17, Issue 1 (2025)
Iran J War Public Health 2025, 17(1): 23-27 |
Back to browse issues page
Article Type:
Subject:
Ethics code: IR.IAU.YAZD.REC.1401.081
History
Received: 2025/01/7 | Accepted: 2025/02/23 | Published: 2025/02/26
Received: 2025/01/7 | Accepted: 2025/02/23 | Published: 2025/02/26
How to cite this article
Hoboubati H, Anoosheh V, Rostami M, Seyedmirza S, Sharifyazdi M, Fallahzadeh H. Association Between COVID-19 Infection and Recurrence of Lumbar Intervertebral Disc Herniation After Laminectomy and Discectomy Surgery. Iran J War Public Health 2025; 17 (1) :23-27
URL: http://ijwph.ir/article-1-1537-en.html
URL: http://ijwph.ir/article-1-1537-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Authors
H. Hoboubati1, V.S. Anoosheh2, M. Rostami3, S.M.A. Seyedmirza *4, M. Sharifyazdi5, H. Fallahzadeh6
1- Department of Medical Sciences, Medical Faculty, Yazd Branch, Islamic Azad University, Yazd, Iran
2- “Department of Ergonomics, School of Health” and “Student Research Committee”, Shiraz University of Medical Sciences, Shiraz, Iran
3- Department of Languages and Literature, Faculty of Humanities, Yazd University, Yazd, Iran
4- Department of Medicine, Faculty of Medicine, Yazd Branch, Islamic Azad University, Yazd, Iran
5- Department of Infection Diseases, Infectious Diseases Research Center, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
6- “Department of Biostatistics and Epidemiology, School of Public Health” and “Research Center for Healthcare Data Modeling”, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
2- “Department of Ergonomics, School of Health” and “Student Research Committee”, Shiraz University of Medical Sciences, Shiraz, Iran
3- Department of Languages and Literature, Faculty of Humanities, Yazd University, Yazd, Iran
4- Department of Medicine, Faculty of Medicine, Yazd Branch, Islamic Azad University, Yazd, Iran
5- Department of Infection Diseases, Infectious Diseases Research Center, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
6- “Department of Biostatistics and Epidemiology, School of Public Health” and “Research Center for Healthcare Data Modeling”, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
Full-Text (HTML) (570 Views)
Introduction
Low back pain is a prevalent health issue with significant healthcare costs [1-3]. Approximately 85% of individuals experience low back pain at some point [4]. It is the fifth most common reason for physician visits in the United States [2, 5]. Lumbar intervertebral disc herniation (LDH) is a frequent condition, with an estimated two million new cases occurring annually in the United States [6]. LDH can cause significant pain and disability, often necessitating surgical intervention.
Laminectomy and discectomy (LD) are common surgical procedures for LDH, involving the removal of part of the vertebra (lamina) and the damaged disc [7]. Most patients with low back pain receive prescription medications, including nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, and opioid analgesics [2]. However, evidence on the effectiveness of these treatments remains limited [2]. Surgery is another widely used treatment for intervertebral disc disorders [8], with disc herniation recurrence being one of the most common postoperative complications [9].
Recurrent disc herniation is a significant issue in primary LDH surgery, with a recurrence rate of 4.62% reported in Hoogland et al.’s 2008 study [10]. This is particularly relevant for transforaminal endoscopic discectomy, a common surgical approach for LDH. The incidence of incision-related herniation, a potential complication of this surgery, has a 40% recurrence rate after surgical repair [11]. Several studies have identified smoking and diabetes as risk factors for recurrence [12], while others have examined the influence of age, gender, BMI, and occupation, demonstrating their impact on recurrence rates [12]. Identifying and mitigating these risk factors is essential to reducing postoperative recurrence rates [13].
In December 2019, a novel coronavirus emerged in Wuhan, China, rapidly spreading worldwide and leading to the COVID-19 pandemic [14-17]. While most infected individuals remained asymptomatic or experienced mild symptoms, some suffered severe complications [18]. Although respiratory symptoms were the most common manifestations [19], extrapulmonary complications, including coagulation disorders, kidney dysfunction, and cardiac issues, were also reported.
COVID-19 triggers an excessive immune response characterized by elevated levels of inflammatory cytokines, chemokines, and free radicals, resulting in severe lung and other organ damage [20]. Among its pathophysiological effects, severe COVID-19 may contribute to intervertebral disc degeneration through inflammatory cytokines and oxidative stress mediators [18]. Oxidative stress damages proteins, lipids, and DNA, affecting the structure and function of various organs and tissues [21]. The excessive immune response induced by COVID-19, with heightened inflammatory cytokines, chemokines, and free radicals, further exacerbates tissue damage [18].
The relationship between COVID-19 infection and recurrent lumbar intervertebral disc herniation remains unclear. However, some reports and case studies suggest a potential association. For instance, a series of cases have documented spinal infections following COVID-19, including spondylodiscitis in the lumbar spine in patients with a history of COVID-19 infection [22].
Several mechanisms may explain how COVID-19 increases the risk of LDH recurrence after LD surgery. First, COVID-19-induced inflammation may cause chronic spinal inflammation, leading to disc degeneration and a higher risk of herniation. Second, COVID-19-related immune system alterations may make individuals more susceptible to infections, including disc infections contributing to LDH recurrence [18]. Third, COVID-19-induced coagulation abnormalities increase the risk of blood clots, which may damage intervertebral discs and lead to herniation [23].
Despite the potential connection, there is a significant gap in the literature regarding the direct impact of COVID-19 on disc herniation recurrence after surgery. Most existing studies focus on the systemic effects of COVID-19 [18, 22, 23], with few specifically examining its role in increasing recurrence risk following laminectomy and discectomy.
This study addressed the research gap by analyzing the incidence and severity of COVID-19 infection in patients who underwent lumbar disc surgery and comparing these findings to recurrence rates. Additionally, the study evaluated the impact of COVID-19 treatments, including hospitalization and remdesivir administration, on disc herniation recurrence.
Instrument and Methods
Design and sampling
This study was conducted in 2024 as a retrospective case-control study by reviewing the medical records of all patients who underwent laminectomy or discectomy surgery in Yazd County hospitals from 2020 to the first half of 2022. Patients with lumbar disc herniation who underwent discectomy and laminectomy and experienced recurrence were randomly selected from this population using simple randomization. From the list of eligible patients, 150 individuals were selected using a random number table and divided into two groups; case (50 patients) and control (100 patients).
A power analysis was performed using G*Power software to determine an appropriate sample size and ensure sufficient statistical power. A statistical power of 80% and a significance level of 0.05 were considered. Based on previous studies and the expected differences between the recurrence and non-recurrence groups, a minimum sample size of 150 patients was determined. This sample size enables the identification of significant effects between COVID-19 and disc herniation recurrence.
Instrument
Data collection was conducted through fieldwork by reviewing patient records and making telephone calls to patients. Data were extracted from the hospital records of patients who had undergone discectomy and laminectomy. At the same time, information on COVID-19 history and herniation recurrence was obtained through telephone follow-ups and patient records. Data were gathered using a researcher-designed questionnaire, which included variables such as age, sex, BMI, history of underlying diseases, operated disc level, time interval to recurrence and reoperation, occurrence of COVID-19, number of infections, hospitalization duration, type of hospitalization, PCR test results, and type of treatment received.
The study included patients with a history of discectomy or laminectomy, complete medical records, and consent to participate. Exclusion criteria included incomplete medical records, patient refusal to participate, and the presence of lumbar spondylolisthesis.
Demographic variables were assessed in both groups to ensure comparability. The groups were matched as much as possible regarding age, sex, and underlying diseases. The number of COVID-19 infections was determined using CT scans, PCR, or rapid antigen tests. Official data were used for patients whose test results were recorded in the Shahid Sadoughi Hospital Genetic Laboratory system and the Healthcare Monitoring Database. For other patients, positive test results or radiological signs were confirmed through telephone interviews. The severity of the disease was categorized based on hospitalization in the infectious disease ward, outpatient treatment, or ICU admission. The total hospitalization duration was extracted from patient records. All patients' underlying diseases were also documented.
Procedure
After obtaining the needed permissions and ethical approval, to reassess recurrence, patients were re-contacted, and their medical records were reviewed in cases of symptom recurrence, reoperation, or follow-up visits with physicians. COVID-19 status was confirmed using PCR, antigen, and medical history reviews.
Data analysis
Statistical methods such as logistic regression and propensity score matching were applied to control age, BMI, and comorbidities. Additionally, the study and control groups were matched for these parameters to ensure that observed differences were attributable to COVID-19 rather than other risk factors. Data were entered into SPSS 26 software and analyzed using Chi-square, T-test, and ANOVA.
Findings
71 women (47.3%) and 79 men (52.7%) participated. The average age was 53.71±12.55 (20 to 82) years.
Seventy-three people (48.7%) were infected with COVID-19; 40 individuals (40%) of the control (without recurrence) and 33 individuals (66%) of the case (with lumbar intervertebral disc herniation recurrence) group (p=0.03). Sixteen people (10.7%) were hospitalized due to COVID-19; 7 individuals (7%) of the control (without recurrence) and nine individuals (18%) of the case (with lumbar intervertebral disc herniation recurrence) group (p=0.04). Eleven people (7.3%) received remdesivir; 4 individuals (4%) of the control (without recurrence) and seven individuals (14%) of the case (with lumbar intervertebral disc herniation recurrence) group (p=0.027). Seven people (4.7%) received anticoagulant drugs; 4 individuals (4%) of the control (without recurrence) and three individuals (6%) of the case (with lumbar intervertebral disc herniation recurrence) group (p=0.584). Thirteen people (8.7%) received corticosteroid medication; 6 individuals (6%) of the control (without recurrence) and seven individuals (14%) of the case (with lumbar intervertebral disc herniation recurrence) group (p=0.101).
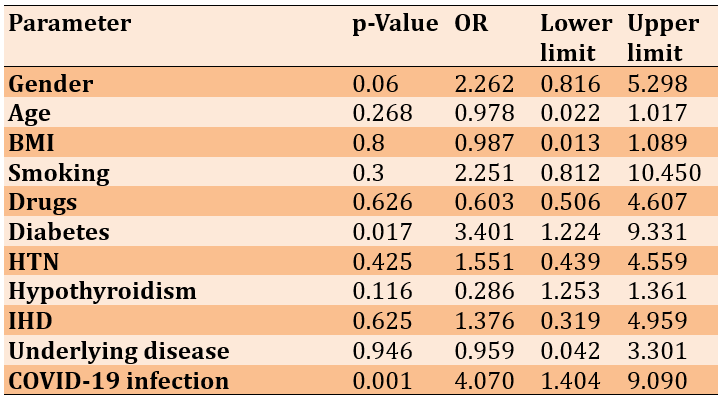
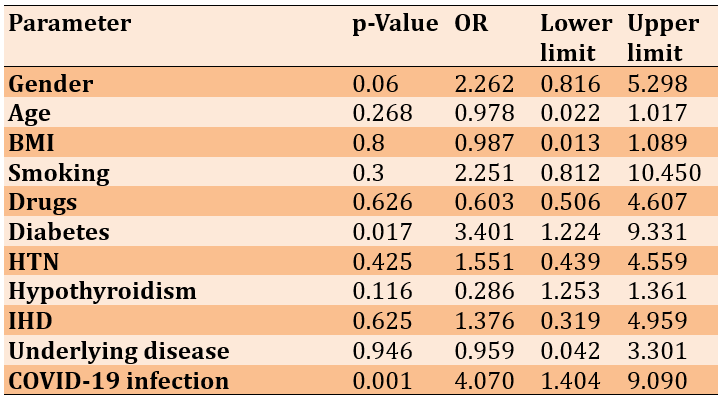
The logistic regression showed that the included parameters explained 15.1% to 21% of the variability. Diabetes patients were 3.4 times more likely to experience disc herniation recurrence (p=0.017), and COVID-19 patients were 4 times more likely to experience recurrence (p=0.001; Table 1).
Table 1. Logistic regression to quantify the relationship between risk factors
Discussion
This study was conducted to investigate the relationship between infection with COVID-19 and the recurrence of lumbar intervertebral disc herniation after laminectomy and discectomy surgery. Degeneration of the intervertebral disc after discectomy is a common problem. Recurrence of herniation is the main cause of debilitating pain. Disability and reoperation after surgery are primary and, therefore, important in determining postoperative success. This type of complication also imposes a significant burden on the healthcare system [23]. It is now known that COVID-19 is primarily a respiratory disease that affects various organ systems, including peripheral nerves and skeletal muscles [22]. Since the beginning of the COVID-19 pandemic, scientific reports have described cases of neurological damage and investigated the potential neurotropic nature of the acute respiratory syndrome of the COVID-19 virus. The neurological impact has become an important area of study as global data collection has shown that it is one of the most common, persistent, and debilitating effects of COVID-19 [24].
In this research, the patients who were re-operated after lumbar intervertebral disc herniation in the period after the outbreak of COVID-19 from 2019 to the first half of 2011 (50 people) were examined after collecting the necessary information. Also, 100 patients who underwent lumbar intervertebral disc herniation and did not have relapses were examined as a control group. Of 50 patients with lumbar disc herniation, 30 were male, and 20 were male. They were women. On the other hand, among 100 people in the group without recurrence, 49 were men and 51 were women. The average age in the group of patients without recurrence of lumbar intervertebral disc herniation was 53.65±12.68. The range of changes was 20 to 82 years. In the patients with lumbar intervertebral disc herniation recurrence group, the average age was 53.84±12.12, and the range of changes was 33 to 79 years. Then, the two groups were examined regarding the infection rate with COVID-19, the number of times they were infected, the type and duration of hospitalization, and the type of treatment received.
This study had a significant relationship between the recurrence of lumbar intervertebral disc herniation and COVID-19 infection. In a study by Somma et al. 2022 on the effect of COVID-19 infection on herniated disc patients treated with ozone, 47 patients were evaluated. Among the 47 people, 19 people were infected with COVID-19 and recovered without symptoms, and the rest did not have COVID-19. In patients who had a previous history of COVID-19, the average reduction of ODI (Oswestry Disability Index) one and three months later was 11.58 and 20.63, respectively, while in people who did not have COVID-19, this average was in one and three months, respectively. It was 20.93 and 22.07 for treatment. Also, the treatment success rate was 84.2% in the group with COVID-19 and 85.7% in the other group. Their study showed that infection with COVID-19 can prolong the recovery time of patients treated for disc herniation, which was in line with the present study [25].
Intervertebral disc space infection can be a serious and debilitating complication of any procedure that allows bacteria to enter the sensitive disc space. Most disc space infections occur after cervical or lumbar laminectomy [26].
In terms of received treatments, receiving remdesivir and symptomatic treatments had a significant relationship with the recurrence of lumbar intervertebral disc herniation. This can be due to the type of disease caused by the common species at the time of remdesivir drug use, as well as the greater severity of the disease, which caused the use of this drug in the treatment process. On the other hand, receiving anticoagulant and corticosteroid drugs did not increase the risk of recurrence of intervertebral disc herniation [27].
Despite its valuable findings, this study has limitations that should be considered when interpreting the results. One of the main limitations is its retrospective design, which may be subject to selection bias and limited access to precise data. Additionally, multiple confounding variables such as patients' underlying conditions, the initial severity of lumbar disc disease, lifestyle, physical activity levels, immune status, and the use of other medications could influence the results. The inability to fully control these factors may affect the observed relationship between COVID-19, the use of remdesivir, and recurrent lumbar disc herniation. Therefore, to confirm these findings, conducting prospective studies with better control of confounding variables is necessary. Healthcare providers should monitor these patients for symptom severity, neurological complications, and medication effects, and prevent the worsening of symptoms and complications through inflammation control, maintaining proper physical activity, and stress management.
Conclusion
COVID-19 infection and its recurrence are associated with the recurrence of lumbar disc herniation.
Acknowledgments: The authors thank Islamic Azad University Yazd Medical School.
Ethical Permissions: It has the code of ethics from the Islamic Azad University Yazd Medical School (IR.IAU.YAZD.REC.1401.081).
Conflicts of Interests: The authors declare no conflicts of interest.
Authors' Contribution: Hoboubati H (First Author), Introduction Writer/Methodologist/Main Researcher (30%); Seyedmirza SMA (Second Author), Assistant Researcher/Statistical Analyst (20%); Sharifyazdi M (Third Author), Statistical Analyst (10%); Rostami M (Fourth Author), Introduction Writer/Assistant Researcher/Discussion Writer (10%); Anoosheh VS (Fifth Author), Introduction Writer/Assistant Researcher/Discussion Writer (20%); Fallahzadeh H (Sixth Author), Statistical Analyst (10%)
Funding/Support: This study was financially supported by Yazd Branch, Islamic Azad University of Medical Sciences, Iran.
Low back pain is a prevalent health issue with significant healthcare costs [1-3]. Approximately 85% of individuals experience low back pain at some point [4]. It is the fifth most common reason for physician visits in the United States [2, 5]. Lumbar intervertebral disc herniation (LDH) is a frequent condition, with an estimated two million new cases occurring annually in the United States [6]. LDH can cause significant pain and disability, often necessitating surgical intervention.
Laminectomy and discectomy (LD) are common surgical procedures for LDH, involving the removal of part of the vertebra (lamina) and the damaged disc [7]. Most patients with low back pain receive prescription medications, including nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, and opioid analgesics [2]. However, evidence on the effectiveness of these treatments remains limited [2]. Surgery is another widely used treatment for intervertebral disc disorders [8], with disc herniation recurrence being one of the most common postoperative complications [9].
Recurrent disc herniation is a significant issue in primary LDH surgery, with a recurrence rate of 4.62% reported in Hoogland et al.’s 2008 study [10]. This is particularly relevant for transforaminal endoscopic discectomy, a common surgical approach for LDH. The incidence of incision-related herniation, a potential complication of this surgery, has a 40% recurrence rate after surgical repair [11]. Several studies have identified smoking and diabetes as risk factors for recurrence [12], while others have examined the influence of age, gender, BMI, and occupation, demonstrating their impact on recurrence rates [12]. Identifying and mitigating these risk factors is essential to reducing postoperative recurrence rates [13].
In December 2019, a novel coronavirus emerged in Wuhan, China, rapidly spreading worldwide and leading to the COVID-19 pandemic [14-17]. While most infected individuals remained asymptomatic or experienced mild symptoms, some suffered severe complications [18]. Although respiratory symptoms were the most common manifestations [19], extrapulmonary complications, including coagulation disorders, kidney dysfunction, and cardiac issues, were also reported.
COVID-19 triggers an excessive immune response characterized by elevated levels of inflammatory cytokines, chemokines, and free radicals, resulting in severe lung and other organ damage [20]. Among its pathophysiological effects, severe COVID-19 may contribute to intervertebral disc degeneration through inflammatory cytokines and oxidative stress mediators [18]. Oxidative stress damages proteins, lipids, and DNA, affecting the structure and function of various organs and tissues [21]. The excessive immune response induced by COVID-19, with heightened inflammatory cytokines, chemokines, and free radicals, further exacerbates tissue damage [18].
The relationship between COVID-19 infection and recurrent lumbar intervertebral disc herniation remains unclear. However, some reports and case studies suggest a potential association. For instance, a series of cases have documented spinal infections following COVID-19, including spondylodiscitis in the lumbar spine in patients with a history of COVID-19 infection [22].
Several mechanisms may explain how COVID-19 increases the risk of LDH recurrence after LD surgery. First, COVID-19-induced inflammation may cause chronic spinal inflammation, leading to disc degeneration and a higher risk of herniation. Second, COVID-19-related immune system alterations may make individuals more susceptible to infections, including disc infections contributing to LDH recurrence [18]. Third, COVID-19-induced coagulation abnormalities increase the risk of blood clots, which may damage intervertebral discs and lead to herniation [23].
Despite the potential connection, there is a significant gap in the literature regarding the direct impact of COVID-19 on disc herniation recurrence after surgery. Most existing studies focus on the systemic effects of COVID-19 [18, 22, 23], with few specifically examining its role in increasing recurrence risk following laminectomy and discectomy.
This study addressed the research gap by analyzing the incidence and severity of COVID-19 infection in patients who underwent lumbar disc surgery and comparing these findings to recurrence rates. Additionally, the study evaluated the impact of COVID-19 treatments, including hospitalization and remdesivir administration, on disc herniation recurrence.
Instrument and Methods
Design and sampling
This study was conducted in 2024 as a retrospective case-control study by reviewing the medical records of all patients who underwent laminectomy or discectomy surgery in Yazd County hospitals from 2020 to the first half of 2022. Patients with lumbar disc herniation who underwent discectomy and laminectomy and experienced recurrence were randomly selected from this population using simple randomization. From the list of eligible patients, 150 individuals were selected using a random number table and divided into two groups; case (50 patients) and control (100 patients).
A power analysis was performed using G*Power software to determine an appropriate sample size and ensure sufficient statistical power. A statistical power of 80% and a significance level of 0.05 were considered. Based on previous studies and the expected differences between the recurrence and non-recurrence groups, a minimum sample size of 150 patients was determined. This sample size enables the identification of significant effects between COVID-19 and disc herniation recurrence.
Instrument
Data collection was conducted through fieldwork by reviewing patient records and making telephone calls to patients. Data were extracted from the hospital records of patients who had undergone discectomy and laminectomy. At the same time, information on COVID-19 history and herniation recurrence was obtained through telephone follow-ups and patient records. Data were gathered using a researcher-designed questionnaire, which included variables such as age, sex, BMI, history of underlying diseases, operated disc level, time interval to recurrence and reoperation, occurrence of COVID-19, number of infections, hospitalization duration, type of hospitalization, PCR test results, and type of treatment received.
The study included patients with a history of discectomy or laminectomy, complete medical records, and consent to participate. Exclusion criteria included incomplete medical records, patient refusal to participate, and the presence of lumbar spondylolisthesis.
Demographic variables were assessed in both groups to ensure comparability. The groups were matched as much as possible regarding age, sex, and underlying diseases. The number of COVID-19 infections was determined using CT scans, PCR, or rapid antigen tests. Official data were used for patients whose test results were recorded in the Shahid Sadoughi Hospital Genetic Laboratory system and the Healthcare Monitoring Database. For other patients, positive test results or radiological signs were confirmed through telephone interviews. The severity of the disease was categorized based on hospitalization in the infectious disease ward, outpatient treatment, or ICU admission. The total hospitalization duration was extracted from patient records. All patients' underlying diseases were also documented.
Procedure
After obtaining the needed permissions and ethical approval, to reassess recurrence, patients were re-contacted, and their medical records were reviewed in cases of symptom recurrence, reoperation, or follow-up visits with physicians. COVID-19 status was confirmed using PCR, antigen, and medical history reviews.
Data analysis
Statistical methods such as logistic regression and propensity score matching were applied to control age, BMI, and comorbidities. Additionally, the study and control groups were matched for these parameters to ensure that observed differences were attributable to COVID-19 rather than other risk factors. Data were entered into SPSS 26 software and analyzed using Chi-square, T-test, and ANOVA.
Findings
71 women (47.3%) and 79 men (52.7%) participated. The average age was 53.71±12.55 (20 to 82) years.
Seventy-three people (48.7%) were infected with COVID-19; 40 individuals (40%) of the control (without recurrence) and 33 individuals (66%) of the case (with lumbar intervertebral disc herniation recurrence) group (p=0.03). Sixteen people (10.7%) were hospitalized due to COVID-19; 7 individuals (7%) of the control (without recurrence) and nine individuals (18%) of the case (with lumbar intervertebral disc herniation recurrence) group (p=0.04). Eleven people (7.3%) received remdesivir; 4 individuals (4%) of the control (without recurrence) and seven individuals (14%) of the case (with lumbar intervertebral disc herniation recurrence) group (p=0.027). Seven people (4.7%) received anticoagulant drugs; 4 individuals (4%) of the control (without recurrence) and three individuals (6%) of the case (with lumbar intervertebral disc herniation recurrence) group (p=0.584). Thirteen people (8.7%) received corticosteroid medication; 6 individuals (6%) of the control (without recurrence) and seven individuals (14%) of the case (with lumbar intervertebral disc herniation recurrence) group (p=0.101).
The logistic regression showed that the included parameters explained 15.1% to 21% of the variability. Diabetes patients were 3.4 times more likely to experience disc herniation recurrence (p=0.017), and COVID-19 patients were 4 times more likely to experience recurrence (p=0.001; Table 1).
Table 1. Logistic regression to quantify the relationship between risk factors
Discussion
This study was conducted to investigate the relationship between infection with COVID-19 and the recurrence of lumbar intervertebral disc herniation after laminectomy and discectomy surgery. Degeneration of the intervertebral disc after discectomy is a common problem. Recurrence of herniation is the main cause of debilitating pain. Disability and reoperation after surgery are primary and, therefore, important in determining postoperative success. This type of complication also imposes a significant burden on the healthcare system [23]. It is now known that COVID-19 is primarily a respiratory disease that affects various organ systems, including peripheral nerves and skeletal muscles [22]. Since the beginning of the COVID-19 pandemic, scientific reports have described cases of neurological damage and investigated the potential neurotropic nature of the acute respiratory syndrome of the COVID-19 virus. The neurological impact has become an important area of study as global data collection has shown that it is one of the most common, persistent, and debilitating effects of COVID-19 [24].
In this research, the patients who were re-operated after lumbar intervertebral disc herniation in the period after the outbreak of COVID-19 from 2019 to the first half of 2011 (50 people) were examined after collecting the necessary information. Also, 100 patients who underwent lumbar intervertebral disc herniation and did not have relapses were examined as a control group. Of 50 patients with lumbar disc herniation, 30 were male, and 20 were male. They were women. On the other hand, among 100 people in the group without recurrence, 49 were men and 51 were women. The average age in the group of patients without recurrence of lumbar intervertebral disc herniation was 53.65±12.68. The range of changes was 20 to 82 years. In the patients with lumbar intervertebral disc herniation recurrence group, the average age was 53.84±12.12, and the range of changes was 33 to 79 years. Then, the two groups were examined regarding the infection rate with COVID-19, the number of times they were infected, the type and duration of hospitalization, and the type of treatment received.
This study had a significant relationship between the recurrence of lumbar intervertebral disc herniation and COVID-19 infection. In a study by Somma et al. 2022 on the effect of COVID-19 infection on herniated disc patients treated with ozone, 47 patients were evaluated. Among the 47 people, 19 people were infected with COVID-19 and recovered without symptoms, and the rest did not have COVID-19. In patients who had a previous history of COVID-19, the average reduction of ODI (Oswestry Disability Index) one and three months later was 11.58 and 20.63, respectively, while in people who did not have COVID-19, this average was in one and three months, respectively. It was 20.93 and 22.07 for treatment. Also, the treatment success rate was 84.2% in the group with COVID-19 and 85.7% in the other group. Their study showed that infection with COVID-19 can prolong the recovery time of patients treated for disc herniation, which was in line with the present study [25].
Intervertebral disc space infection can be a serious and debilitating complication of any procedure that allows bacteria to enter the sensitive disc space. Most disc space infections occur after cervical or lumbar laminectomy [26].
In terms of received treatments, receiving remdesivir and symptomatic treatments had a significant relationship with the recurrence of lumbar intervertebral disc herniation. This can be due to the type of disease caused by the common species at the time of remdesivir drug use, as well as the greater severity of the disease, which caused the use of this drug in the treatment process. On the other hand, receiving anticoagulant and corticosteroid drugs did not increase the risk of recurrence of intervertebral disc herniation [27].
Despite its valuable findings, this study has limitations that should be considered when interpreting the results. One of the main limitations is its retrospective design, which may be subject to selection bias and limited access to precise data. Additionally, multiple confounding variables such as patients' underlying conditions, the initial severity of lumbar disc disease, lifestyle, physical activity levels, immune status, and the use of other medications could influence the results. The inability to fully control these factors may affect the observed relationship between COVID-19, the use of remdesivir, and recurrent lumbar disc herniation. Therefore, to confirm these findings, conducting prospective studies with better control of confounding variables is necessary. Healthcare providers should monitor these patients for symptom severity, neurological complications, and medication effects, and prevent the worsening of symptoms and complications through inflammation control, maintaining proper physical activity, and stress management.
Conclusion
COVID-19 infection and its recurrence are associated with the recurrence of lumbar disc herniation.
Acknowledgments: The authors thank Islamic Azad University Yazd Medical School.
Ethical Permissions: It has the code of ethics from the Islamic Azad University Yazd Medical School (IR.IAU.YAZD.REC.1401.081).
Conflicts of Interests: The authors declare no conflicts of interest.
Authors' Contribution: Hoboubati H (First Author), Introduction Writer/Methodologist/Main Researcher (30%); Seyedmirza SMA (Second Author), Assistant Researcher/Statistical Analyst (20%); Sharifyazdi M (Third Author), Statistical Analyst (10%); Rostami M (Fourth Author), Introduction Writer/Assistant Researcher/Discussion Writer (10%); Anoosheh VS (Fifth Author), Introduction Writer/Assistant Researcher/Discussion Writer (20%); Fallahzadeh H (Sixth Author), Statistical Analyst (10%)
Funding/Support: This study was financially supported by Yazd Branch, Islamic Azad University of Medical Sciences, Iran.
Keywords:
Lumbar Disc Herniation [MeSH], COVID-19 [MeSH], Recurrence [MeSH], Laminectomy [MeSH], Discectomy [MeSH], Remdesivir [MeSH]
References
1. Chou R, Qaseem A, Snow V, Casey D, Cross JT, Shekelle P, et al. Diagnosis and treatment of low back pain: A joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147(7):478-91. [Link] [DOI:10.7326/0003-4819-147-7-200710020-00006]
2. Hart LG, Deyo RA, Cherkin DC. Physician office visits for low back pain. Frequency, clinical evaluation, and treatment patterns from a U.S. national survey. Spine. 1995;20(1):11-9. [Link] [DOI:10.1097/00007632-199501000-00003]
3. Crook J, Rideout E, Browne G. The prevalence of pain complaints in a general population. Pain. 1984;18(3):299-314. [Link] [DOI:10.1016/0304-3959(84)90824-8]
4. Louw QA, Morris LD, Grimmer-Somers K. The prevalence of low back pain in Africa: A systematic review. BMC Musculoskelet Disord. 2007;8:105. [Link] [DOI:10.1186/1471-2474-8-105]
5. Chou R, Huffman LH, American Pain Society, American College of Physicians. Medications for acute and chronic low back pain: A review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med. 2007;147(7):505-14 [Link] [DOI:10.7326/0003-4819-147-7-200710020-00008]
6. Donahue SP, Kowalski RP, Eller AW, DeVaro JM, Jewart BH. Empiric treatment of endophthalmitis. Are aminoglycosides necessary?. Arch Ophthalmol. 1994;112(1):45-7. [Link] [DOI:10.1001/archopht.1994.01090130055016]
7. Corniola MV, Tessitore E, Schaller K, Gautschi OP. Lumbar disc herniation--diagnosis and treatment. REVUE MÉDICALE SUISSE. 2014;10(454):2376-82. [French] [Link] [DOI:10.53738/REVMED.2014.10.454.2376]
8. Wennberg JE, Cooper M. Spine surgery: Dartmouth Atlas of health care: Studies of surgical variation. Lebanon: The Dartmouth Institute for Health Policy and Clinical Practice; 2022. [Link]
9. Kamper SJ, Ostelo RW, Rubinstein SM, Nellensteijn JM, Peul WC, Arts MP, et al. Minimally invasive surgery for lumbar disc herniation: A systematic review and meta-analysis. Eur Spine J. 2014;23(5):1021-43. [Link] [DOI:10.1007/s00586-013-3161-2]
10. Hoogland T, Van Den Brekel-Dijkstra K, Schubert M, Miklitz B. Endoscopic transforaminal discectomy for recurrent lumbar disc herniation: A prospective, cohort evaluation of 262 consecutive cases. Spine. 2008;33(9):973-8. [Link] [DOI:10.1097/BRS.0b013e31816c8ade]
11. Mudge M, Hughes LE. Incisional hernia: A 10 year prospective study of incidence and attitudes. Br J Surg. 1985;72(1):70-1. [Link] [DOI:10.1002/bjs.1800720127]
12. Huang W, Han Z, Liu J, Yu L, Yu X. Risk factors for recurrent lumbar disc herniation: A systematic review and meta-analysis. Medicine. 2016;95(2):e2378. [Link] [DOI:10.1097/MD.0000000000002378]
13. Jacob L, Oh H, Smith L, Koyanagi A, Konrad M, Kostev K. Impact of the coronavirus disease 2019 (COVID-19) pandemic on the diagnosis of neck and low back pain in outpatient practices in Germany. Prev Med Rep. 2023;31:102096. [Link] [DOI:10.1016/j.pmedr.2022.102096]
14. Zhu H, Wei L, Niu P. The novel coronavirus outbreak in Wuhan, China. Glob Health Res Policy. 2020;5:6. [Link] [DOI:10.1186/s41256-020-00135-6]
15. Wong NSQ, Liu C, Lin MT, Lee IXY, Tong L, Liu YC. Neuropathic corneal pain after coronavirus disease 2019 (COVID-19) infection. Diseases. 2024;12(2):37. [Link] [DOI:10.3390/diseases12020037]
16. Zangrillo A, Beretta L, Silvani P, Colombo S, Scandroglio AM, Dell'Acqua A, et al. Fast reshaping of intensive care unit facilities in a large metropolitan hospital in Milan, Italy: Facing the COVID-19 pandemic emergency. Crit Care Resusc. 2020;22(2):91-4. [Link] [DOI:10.51893/2020.2.pov1]
17. Özgüç S, Kaplan Serin E, Tanriverdi D. Death anxiety associated with coronavirus (COVID-19) disease: A systematic review and meta-analysis. Omega. 2024;88(3):823-56. [Link] [DOI:10.1177/00302228211050503]
18. Lopes LR, Kasinski SK. The potential impact of COVID-19 and diabetes on intervertebral disc degeneration. Einstein. 2022;19:eCE6911. [Link] [DOI:10.31744/einstein_journal/2021CE6911]
19. Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. Int J Antimicrob Agents. 2020;55(3):105924. [Link] [DOI:10.1016/j.ijantimicag.2020.105924]
20. Mohamed Khosroshahi L, Rokni M, Mokhtari T, Noorbakhsh F. Immunology, immunopathogenesis and immunotherapeutics of COVID-19; an overview. Int Immunopharmacol. 2021;93:107364. [Link] [DOI:10.1016/j.intimp.2020.107364]
21. Lim S, Bae JH, Kwon HS, Nauck MA. COVID-19 and diabetes mellitus: From pathophysiology to clinical management. Nat Rev Endocrinol. 2021;17(1):11-30. [Link] [DOI:10.1038/s41574-020-00435-4]
22. Mohamed Ramlee FA, Harun MHB, Nagaretnam V, Lim TS, Aris HF, Tan CN. A case series of spinal infections following COVID-19: A delayed complication. Cureus. 2022;14(9):e29272. [Link] [DOI:10.7759/cureus.29272]
23. Shepard N, Cho W. Recurrent lumbar disc herniation: A review. Global Spine J. 2019;9(2):202-9. [Link] [DOI:10.1177/2192568217745063]
24. Suh J, Amato AA. Neuromuscular complications of coronavirus disease-19. Curr Opin Neurol. 2021;34(5):669-74. [Link] [DOI:10.1097/WCO.0000000000000970]
25. Hogberg HT, Lam A, Ohayon E, Shahbaz MA, Clerbaux LA, Bal-Price A, et al. The adverse outcome pathway framework applied to neurological symptoms of COVID-19. Cells. 2022;11(21):3411. [Link] [DOI:10.3390/cells11213411]
26. Somma F, Negro A, D'Agostino V, Piscitelli V, Pace G, Tortora M, et al. COVID-19 and low back pain: Previous infections lengthen recovery time after intradiscal ozone therapy in patients with herniated lumbar disc. Radiol Med. 2022;127(6):673-80. [Link] [DOI:10.1007/s11547-022-01500-w]
27. Zeiger HE, Zampella EJ. Intervertebral disc infection after lumbar chemonucleolysis: Report of a case. Neurosurgery. 1986;18(5):616-21. [Link] [DOI:10.1227/00006123-198605000-00017]