Volume 16, Issue 2 (2024)
Iran J War Public Health 2024, 16(2): 215-220 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2024/07/20 | Accepted: 2024/09/9 | Published: 2024/09/28
Received: 2024/07/20 | Accepted: 2024/09/9 | Published: 2024/09/28
How to cite this article
Ibrahim A, Yasiry A. Nursing Documentation of Hygiene Practices in Intensive Care Units. Iran J War Public Health 2024; 16 (2) :215-220
URL: http://ijwph.ir/article-1-1492-en.html
URL: http://ijwph.ir/article-1-1492-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Authors
A.F. Ibrahim *1, A.A. Yasiry1
1- Department of Family and Community Health, College of Nursing, Babylon University, Babylon, Iraq
Full-Text (HTML) (899 Views)
Introduction
Nursing documentation serves various functions, including being a component of nurses' medical notes and a source of fundamental and crucial information about healthcare, a patient record that includes all written information about a patient's condition and requirements, and nursing chores [1].
Monitoring compliance rates with hygiene practices and identifying areas needing improvement is essential. Research has shown that structured feedback mechanisms can enhance adherence to hygiene protocols among healthcare workers [2]. For instance, observational studies have highlighted significant variations in compliance rates among different professional groups within ICUs, underscoring the need for targeted interventions [3]. Moreover, effective nursing documentation is indispensable for inter-professional communication, ensuring that all healthcare team members are well-informed about a patient's condition and care plan [4, 5]. This continuity of care is particularly critical in high-stakes environments such as intensive care units (ICUs), where patients often face severe health challenges and require coordinated efforts from multiple healthcare providers. Quality documentation also serves as a legal safeguard for nurses, providing evidence of care rendered and protecting against potential litigation [5, 7]. Beyond its legal and communicative roles, nursing documentation is integral to broader quality improvement initiatives within healthcare organizations. By analyzing documentation trends, healthcare administrators and quality improvement teams can identify systemic issues in patient care practices, recognize error or omission patterns, and formulate enhancement strategies. This process is essential for the ongoing elevation of care standards and the development of evidence-based policies and procedures that can be adopted across the organization to improve patient care quality [8-9].
The medical record is a legally enforceable document that serves multiple functions. From a legal perspective, preventing potential legal issues arising from professional misconduct or negligence is crucial. According to Wang et al. [10], the medical record of a patient represents the sole permanent account of their care from the time of admission until discharge. This comprehensive documentation provides a factual basis for the patient's medical history. It plays a critical role in legal proceedings, serving as key evidence in cases involving malpractice, personal injury, and insurance claims [11, 12]. The integrity and accuracy of these records are of utmost importance; they must be clear, concise, and complete to withstand scrutiny in a court of law [13]. Inadequate documentation can have significant repercussions for healthcare providers, including legal liability and damage to professional credibility [13, 15]. Additionally, the medical record is a communication tool among healthcare professionals, promoting continuity of care and facilitating informed decision-making [14, 15]. As healthcare increasingly transitions to electronic health records, maintaining legal standards for documentation becomes even more crucial, necessitating strict adherence to privacy laws and regulations concerning patient information [13]. The medical record is not merely a repository of patient information; it is a critical instrument for safeguarding both patient rights and healthcare provider responsibilities within the complex landscape of modern medicine.
As a result, nurses are encouraged to examine their documentation processes critically to guarantee that the documentation is understandable to readers both within and outside the field. Documentation is more important because it is a communication tool for all healthcare personnel [16].
Effective nursing documentation ensures continuity of care, enhances patient safety and facilitates inter-professional collaboration among healthcare providers. It offers a comprehensive overview of patient assessments, nursing diagnoses, interventions, and evaluations, essential for informed decision-making and quality care delivery [17]. High-quality documentation reflects the care nurses provide and serves as a legal record that can protect nurses and healthcare institutions from potential litigation [18, 19]. Furthermore, precise and accurate documentation is critical for meeting regulatory requirements and professional standards, demonstrating accountability and adherence to best practices in patient care [6, 19-21]. Research suggests poor documentation can lead to misunderstandings in patient status and care plans, ultimately jeopardizing patient outcomes [20]. Therefore, nurses need continuous education and training to refine their documentation skills and ensure that their records are complete, concise, and compliant with established guidelines [21, 22]. By prioritizing effective documentation practices, nurses can significantly enhance the overall quality of healthcare delivery and improve communication within the healthcare team.
Various factors, such as unclear language or the use of unauthorized acronyms, can impede the documentation of a patient's condition, care, and responses to treatment according to established nursing documentation standards [23].
Accurate documentation of hygiene practices in ICUs, such as oral care to prevent ventilator-associated pneumonia, is crucial for communication among healthcare providers and directly impacts patient outcomes [1, 24]. The World Health Organization (WHO) [25] advocates for establishing and promoting health policies to enhance oral care for patients. Enhanced oral health has been shown to inhibit the colonization of respiratory pathogens in the oropharynx, thereby decreasing the incidence of infections and other respiratory diseases, ultimately leading to improved morbidity and mortality rates [26]. Furthermore, effective oral care practices can significantly lower ventilator-associated pneumonia rates in ICUs [27]. Consequently, inadequate oral health can result in oral diseases [28], contributing to a greater health burden and increased economic costs [28]. The knowledge, attitudes, and practices of nursing personnel across various ranks and positions heavily influence the provision of quality oral care within hospital environments. Most studies focusing on the knowledge, attitudes, and practices of nursing staff regarding oral care have been conducted specifically in ICUs, with fewer exploring acute hospital environments, such as medical and surgical wards or general hospital settings [29]. In Hong Kong, only one qualitative study has been conducted that involved interviews with ten ICU nurses, revealing that oral care procedures were assigned a relatively low priority compared to other nursing interventions [30]. Additionally, the need for standardized tools for assessing knowledge, attitudes, and practices has hindered the comparison of different studies.
By promoting inter-professional collaboration and ensuring critical information is readily accessible, precise documentation of hygiene practices in ICUs reduces the risk of healthcare-associated infections and reinforces the accountability and professionalism of nursing practice [17, 19, 21]. Nurses with access to resources for learning about oral care will likely enhance their practice, leading to more frequent and effective treatment of intubated patients [31].
This study explored nurses' attitudes toward these practices and their understanding of the importance of oral hygiene.
Instrument and Methods
This descriptive cross-sectional study was conducted in the Middle Euphrates Teaching Hospital ICU from 9 February 2023 to 26 June 2024. The convenience sample of 125 nurses was selected.
Nursing documentation serves various functions, including being a component of nurses' medical notes and a source of fundamental and crucial information about healthcare, a patient record that includes all written information about a patient's condition and requirements, and nursing chores [1].
Monitoring compliance rates with hygiene practices and identifying areas needing improvement is essential. Research has shown that structured feedback mechanisms can enhance adherence to hygiene protocols among healthcare workers [2]. For instance, observational studies have highlighted significant variations in compliance rates among different professional groups within ICUs, underscoring the need for targeted interventions [3]. Moreover, effective nursing documentation is indispensable for inter-professional communication, ensuring that all healthcare team members are well-informed about a patient's condition and care plan [4, 5]. This continuity of care is particularly critical in high-stakes environments such as intensive care units (ICUs), where patients often face severe health challenges and require coordinated efforts from multiple healthcare providers. Quality documentation also serves as a legal safeguard for nurses, providing evidence of care rendered and protecting against potential litigation [5, 7]. Beyond its legal and communicative roles, nursing documentation is integral to broader quality improvement initiatives within healthcare organizations. By analyzing documentation trends, healthcare administrators and quality improvement teams can identify systemic issues in patient care practices, recognize error or omission patterns, and formulate enhancement strategies. This process is essential for the ongoing elevation of care standards and the development of evidence-based policies and procedures that can be adopted across the organization to improve patient care quality [8-9].
The medical record is a legally enforceable document that serves multiple functions. From a legal perspective, preventing potential legal issues arising from professional misconduct or negligence is crucial. According to Wang et al. [10], the medical record of a patient represents the sole permanent account of their care from the time of admission until discharge. This comprehensive documentation provides a factual basis for the patient's medical history. It plays a critical role in legal proceedings, serving as key evidence in cases involving malpractice, personal injury, and insurance claims [11, 12]. The integrity and accuracy of these records are of utmost importance; they must be clear, concise, and complete to withstand scrutiny in a court of law [13]. Inadequate documentation can have significant repercussions for healthcare providers, including legal liability and damage to professional credibility [13, 15]. Additionally, the medical record is a communication tool among healthcare professionals, promoting continuity of care and facilitating informed decision-making [14, 15]. As healthcare increasingly transitions to electronic health records, maintaining legal standards for documentation becomes even more crucial, necessitating strict adherence to privacy laws and regulations concerning patient information [13]. The medical record is not merely a repository of patient information; it is a critical instrument for safeguarding both patient rights and healthcare provider responsibilities within the complex landscape of modern medicine.
As a result, nurses are encouraged to examine their documentation processes critically to guarantee that the documentation is understandable to readers both within and outside the field. Documentation is more important because it is a communication tool for all healthcare personnel [16].
Effective nursing documentation ensures continuity of care, enhances patient safety and facilitates inter-professional collaboration among healthcare providers. It offers a comprehensive overview of patient assessments, nursing diagnoses, interventions, and evaluations, essential for informed decision-making and quality care delivery [17]. High-quality documentation reflects the care nurses provide and serves as a legal record that can protect nurses and healthcare institutions from potential litigation [18, 19]. Furthermore, precise and accurate documentation is critical for meeting regulatory requirements and professional standards, demonstrating accountability and adherence to best practices in patient care [6, 19-21]. Research suggests poor documentation can lead to misunderstandings in patient status and care plans, ultimately jeopardizing patient outcomes [20]. Therefore, nurses need continuous education and training to refine their documentation skills and ensure that their records are complete, concise, and compliant with established guidelines [21, 22]. By prioritizing effective documentation practices, nurses can significantly enhance the overall quality of healthcare delivery and improve communication within the healthcare team.
Various factors, such as unclear language or the use of unauthorized acronyms, can impede the documentation of a patient's condition, care, and responses to treatment according to established nursing documentation standards [23].
Accurate documentation of hygiene practices in ICUs, such as oral care to prevent ventilator-associated pneumonia, is crucial for communication among healthcare providers and directly impacts patient outcomes [1, 24]. The World Health Organization (WHO) [25] advocates for establishing and promoting health policies to enhance oral care for patients. Enhanced oral health has been shown to inhibit the colonization of respiratory pathogens in the oropharynx, thereby decreasing the incidence of infections and other respiratory diseases, ultimately leading to improved morbidity and mortality rates [26]. Furthermore, effective oral care practices can significantly lower ventilator-associated pneumonia rates in ICUs [27]. Consequently, inadequate oral health can result in oral diseases [28], contributing to a greater health burden and increased economic costs [28]. The knowledge, attitudes, and practices of nursing personnel across various ranks and positions heavily influence the provision of quality oral care within hospital environments. Most studies focusing on the knowledge, attitudes, and practices of nursing staff regarding oral care have been conducted specifically in ICUs, with fewer exploring acute hospital environments, such as medical and surgical wards or general hospital settings [29]. In Hong Kong, only one qualitative study has been conducted that involved interviews with ten ICU nurses, revealing that oral care procedures were assigned a relatively low priority compared to other nursing interventions [30]. Additionally, the need for standardized tools for assessing knowledge, attitudes, and practices has hindered the comparison of different studies.
By promoting inter-professional collaboration and ensuring critical information is readily accessible, precise documentation of hygiene practices in ICUs reduces the risk of healthcare-associated infections and reinforces the accountability and professionalism of nursing practice [17, 19, 21]. Nurses with access to resources for learning about oral care will likely enhance their practice, leading to more frequent and effective treatment of intubated patients [31].
This study explored nurses' attitudes toward these practices and their understanding of the importance of oral hygiene.
Instrument and Methods
This descriptive cross-sectional study was conducted in the Middle Euphrates Teaching Hospital ICU from 9 February 2023 to 26 June 2024. The convenience sample of 125 nurses was selected.
After a thorough review of the relevant literature, a questionnaire was prepared and modified. This questionnaire covers socio-demographic data (age/years, gender, educational level, marital status, and experience years) and the documentation of nursing hygienic care for hair (2 items), mouth (3 items), eye (4 items), and nose (3 items) for unconscious patients. The results were categorized as poor (1-1.6), fair (1.7-2.3), and good (2.4-3). The reliability of the items was based on the internal consistency of the checklist and assessed by calculating Cronbach's Alpha (0.84).
Data was analyzed using SPSS 25 software with descriptive statistical methods and variance analysis.
Findings
Most participants (74.4%) were between 20 and 29 years old and female (69.6%; Table 1).
Table 1. Distribution of demographic characteristics (n=125)

The nurses expressed fair practices regarding patient hair care (1.88±0.73), mouth care (1.86±0.66), eye care (1.98±0.67), and nose care (1.84±0.47). Overall, 73.6% of the nurses exhibited fair documentation of hygiene practices (Table 2).
Table 2. Documentation of nursing hygienic care for unconscious patients (n=125)


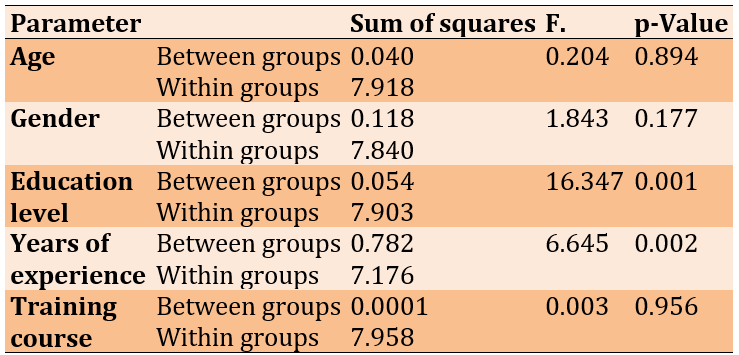
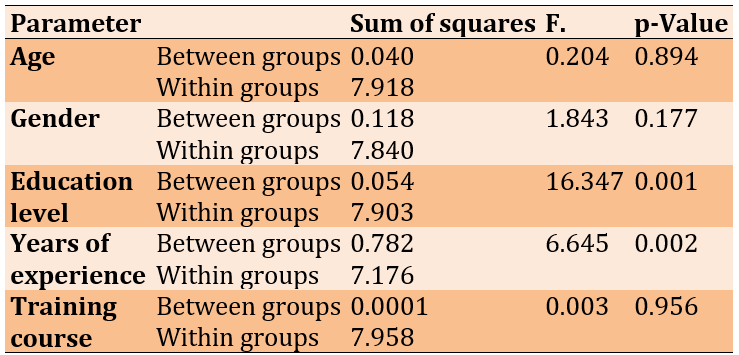
There have been significant differences in nurses’ documentation for hygiene based on their education level and years of experience (Table 3).
Table 3. Statistical differences in nurses’ documentation of hygiene (n=125)
Discussion
They represent the study distribution of the nurses by their demographic characteristics. The age groups that comprised the study's subjects were those between the ages of 20 and 29, accounting for 74.4% of all participants. Young nurses are needed on surgical wards due to the nature of their work. This age group is competent to provide prompt and efficient nursing interventions. The findings of this study are consistent with those of Karthiga Priyadharshini [32], who discovered that most of the study participants were under 40 years old.
Related to gender, female nurses comprised 69.6% of the total number of participants, making up more than half of all nurses. In contrast, male nurses made up 30.4% of the total. These findings concur with Mohaithef [33], who discovered that roughly 51.9% of the participants in their study sample were male. Due to further supported by the observation that hospital wards completely rely on nurses with nursing institute diplomas, even though these nurses still make up a small minority of all registered nurses. This result does not agree with the analysis done by Ebrahim Aboalizm & Abdel Aziz Kasemy [34], who discovered that roughly 45% of the study sample possessed a diploma.
Based on the information gathered from study participants, it can be inferred that 68.0 have fewer than ten years of experience in both the ICU and their profession. This is because many nurses believe that working in ICU calls for much work and a significant amount of skilled and sensitive care when dealing with unconscious patients. It also calls for dealing with patients' relatives and families by giving them the necessary information and education regarding the health conditions of the patients. This result is consistent with the research of Abid et al. [35], which noted that most of their study samples had less.
The results indicate that 76.8% of study participants have training. This is because most nurses are recent hires who have attended nursing documentation training sessions, and some nurses need to be more interested in attending training sessions provided by the hospital's continuing education departments. These findings are consistent with a study by Ali [36] that found that 50% of the study participants lacked communicative skills.
The nurses expressed fair practice regarding hair care. These findings were supported by a study conducted by Kadhim and Khudur [37], which revealed that nurses performed poorly regarding hair care of unconscious patients. This can explain their practice regarding nursing documentation, including the rules of documentation, including what and how to record. According to the study sample, this study demonstrates that the nurses expressed a fair practice regarding mouth care steps documented in items. The findings agree with Kadhim & Khudur [37]. The findings of this study demonstrated that, except for hand washing, The nurses' oral hygiene practices are insufficient. Nursing documentation shows care evaluation and weaknesses in the nursing records, such as difficulties finding important information due to many routine notes [38].
Regarding documenting eye care, the nurses expressed a fair attitude. These findings were inconsistent with a study by Inan & Dinç [1], which pointed out that more than half of the participants had documented the care of the eye. This is related to several reasons. Due to the educational attainment of the study sample, most of them hold a diploma, which limits their experience in presenting and sharing information in innovative ways, such as displaying images and videos of the surgical procedure to unconscious patients.
This table illustrates that the nurses expressed fair practice regarding nose care documentation. These findings were reinforced by Abid et al. [35]. Intravenous fluid, nasogastric tubes, gastrostomies, and oral fluid administration account for 64% of all fluid administration (88%). All of the items have been removed. Nursing documentation effectively requires good practices and skills; novice nurses need help documenting such procedures.
Findings demonstrate that 73.6% of nurses exhibited fair documentation of hygiene practices. These findings were inconsistent with a study by Inan & Dinç [1]. This study found that patients in the ICU are more vulnerable to oral infections because of their medical conditions, and this study's findings are important since providing hygienic care is one of the most essential nursing duties.
The results of the variance analysis indicated no significant differences in the hygienic documentation made by nurses for unconscious patients with regard to age groups. These findings are supported by Inan & Dinç [1], who stated that the age of nurses is considered a non-influencing factor on their performance in documentation hygiene.
These results show that female nurses perform better than men, with no statistically significant difference. There are no significant differences in the preference of female nurses, considering that gender is an ineffective factor, and this cannot be considered in these wards. Based on those regards, Dagnew et al. [39] confirmed that female nurses had more positive attitudes toward nursing documentation of oral hygiene for unconscious patients than male nurses.
Through these significant differences, the educational level is influential in nursing hygiene documentation. It was observed that nurses who graduated college and above are significantly associated with higher practices of nursing documentation of hygiene for unconscious patients, followed by those who are nursing institute graduates, unlike those in nursing school.
The study found that there have been considerable variances in nurses' documentation for hygiene for unconscious patients about years of experience. The years of experience in the critical care unit are considered a challenge in nurses' practices [40]. The significant differences favored those with≥10 years of experience, as they recorded the highest average nursing documentation of hygiene practices, unlike those with <5 years. This variable (years of experience) can be worked on by improving documentation practices by relying on experienced nurses.
It was observed that the significant training was associated with higher documentation of hygiene practices. Training programs, including the proposed rules for the documentation of patients in the ICU, should be adopted for nurses depending on their needs, and their impact on their performances must be evaluated [41]. Finally, nurses at all levels of education do not care about documentation, which gives a relational for their poor levels in all domains of this issue.
Scheduled training sessions should be delivered at the most convenient time for employees. Continuous educational sessions and programs should be applied to enhance nurses’ documentation skills when dealing with critical patients during their care in the ICU. In addition, nurses in Iraq must use an electronic documentation system as part of their work.
Conclusion
The assessment of the nursing staff's documentation is fair. However, there are significant differences in nurses’ documentation for unconscious patients based on education levels and years of experience.
Acknowledgments: None declared by the authors.
Ethical Permissions: The study was conducted in accordance with the ethical principles that have their origin in the Declaration of Helsinki. It was carried out with patients verbal and analytical approval before sample was taken. The study protocol and the subject information and consent form were reviewed and approved by a local ethics committee according to the document (No.38) in date (28/2/2024) to get this approval.
Conflicts of Interests: There were no conflicts.
Authors' Contribution: Ibrahim AF (First Author), Introduction Writer/Methodologist/Original or Assistant Researcher/Discussion Writer (75%); Yasiry AA (Second Author), Statistical Analyst (25%)
Funding/Support: None declared by the authors.
Findings
Most participants (74.4%) were between 20 and 29 years old and female (69.6%; Table 1).
Table 1. Distribution of demographic characteristics (n=125)

The nurses expressed fair practices regarding patient hair care (1.88±0.73), mouth care (1.86±0.66), eye care (1.98±0.67), and nose care (1.84±0.47). Overall, 73.6% of the nurses exhibited fair documentation of hygiene practices (Table 2).
Table 2. Documentation of nursing hygienic care for unconscious patients (n=125)


There have been significant differences in nurses’ documentation for hygiene based on their education level and years of experience (Table 3).
Table 3. Statistical differences in nurses’ documentation of hygiene (n=125)
Discussion
They represent the study distribution of the nurses by their demographic characteristics. The age groups that comprised the study's subjects were those between the ages of 20 and 29, accounting for 74.4% of all participants. Young nurses are needed on surgical wards due to the nature of their work. This age group is competent to provide prompt and efficient nursing interventions. The findings of this study are consistent with those of Karthiga Priyadharshini [32], who discovered that most of the study participants were under 40 years old.
Related to gender, female nurses comprised 69.6% of the total number of participants, making up more than half of all nurses. In contrast, male nurses made up 30.4% of the total. These findings concur with Mohaithef [33], who discovered that roughly 51.9% of the participants in their study sample were male. Due to further supported by the observation that hospital wards completely rely on nurses with nursing institute diplomas, even though these nurses still make up a small minority of all registered nurses. This result does not agree with the analysis done by Ebrahim Aboalizm & Abdel Aziz Kasemy [34], who discovered that roughly 45% of the study sample possessed a diploma.
Based on the information gathered from study participants, it can be inferred that 68.0 have fewer than ten years of experience in both the ICU and their profession. This is because many nurses believe that working in ICU calls for much work and a significant amount of skilled and sensitive care when dealing with unconscious patients. It also calls for dealing with patients' relatives and families by giving them the necessary information and education regarding the health conditions of the patients. This result is consistent with the research of Abid et al. [35], which noted that most of their study samples had less.
The results indicate that 76.8% of study participants have training. This is because most nurses are recent hires who have attended nursing documentation training sessions, and some nurses need to be more interested in attending training sessions provided by the hospital's continuing education departments. These findings are consistent with a study by Ali [36] that found that 50% of the study participants lacked communicative skills.
The nurses expressed fair practice regarding hair care. These findings were supported by a study conducted by Kadhim and Khudur [37], which revealed that nurses performed poorly regarding hair care of unconscious patients. This can explain their practice regarding nursing documentation, including the rules of documentation, including what and how to record. According to the study sample, this study demonstrates that the nurses expressed a fair practice regarding mouth care steps documented in items. The findings agree with Kadhim & Khudur [37]. The findings of this study demonstrated that, except for hand washing, The nurses' oral hygiene practices are insufficient. Nursing documentation shows care evaluation and weaknesses in the nursing records, such as difficulties finding important information due to many routine notes [38].
Regarding documenting eye care, the nurses expressed a fair attitude. These findings were inconsistent with a study by Inan & Dinç [1], which pointed out that more than half of the participants had documented the care of the eye. This is related to several reasons. Due to the educational attainment of the study sample, most of them hold a diploma, which limits their experience in presenting and sharing information in innovative ways, such as displaying images and videos of the surgical procedure to unconscious patients.
This table illustrates that the nurses expressed fair practice regarding nose care documentation. These findings were reinforced by Abid et al. [35]. Intravenous fluid, nasogastric tubes, gastrostomies, and oral fluid administration account for 64% of all fluid administration (88%). All of the items have been removed. Nursing documentation effectively requires good practices and skills; novice nurses need help documenting such procedures.
Findings demonstrate that 73.6% of nurses exhibited fair documentation of hygiene practices. These findings were inconsistent with a study by Inan & Dinç [1]. This study found that patients in the ICU are more vulnerable to oral infections because of their medical conditions, and this study's findings are important since providing hygienic care is one of the most essential nursing duties.
The results of the variance analysis indicated no significant differences in the hygienic documentation made by nurses for unconscious patients with regard to age groups. These findings are supported by Inan & Dinç [1], who stated that the age of nurses is considered a non-influencing factor on their performance in documentation hygiene.
These results show that female nurses perform better than men, with no statistically significant difference. There are no significant differences in the preference of female nurses, considering that gender is an ineffective factor, and this cannot be considered in these wards. Based on those regards, Dagnew et al. [39] confirmed that female nurses had more positive attitudes toward nursing documentation of oral hygiene for unconscious patients than male nurses.
Through these significant differences, the educational level is influential in nursing hygiene documentation. It was observed that nurses who graduated college and above are significantly associated with higher practices of nursing documentation of hygiene for unconscious patients, followed by those who are nursing institute graduates, unlike those in nursing school.
The study found that there have been considerable variances in nurses' documentation for hygiene for unconscious patients about years of experience. The years of experience in the critical care unit are considered a challenge in nurses' practices [40]. The significant differences favored those with≥10 years of experience, as they recorded the highest average nursing documentation of hygiene practices, unlike those with <5 years. This variable (years of experience) can be worked on by improving documentation practices by relying on experienced nurses.
It was observed that the significant training was associated with higher documentation of hygiene practices. Training programs, including the proposed rules for the documentation of patients in the ICU, should be adopted for nurses depending on their needs, and their impact on their performances must be evaluated [41]. Finally, nurses at all levels of education do not care about documentation, which gives a relational for their poor levels in all domains of this issue.
Scheduled training sessions should be delivered at the most convenient time for employees. Continuous educational sessions and programs should be applied to enhance nurses’ documentation skills when dealing with critical patients during their care in the ICU. In addition, nurses in Iraq must use an electronic documentation system as part of their work.
Conclusion
The assessment of the nursing staff's documentation is fair. However, there are significant differences in nurses’ documentation for unconscious patients based on education levels and years of experience.
Acknowledgments: None declared by the authors.
Ethical Permissions: The study was conducted in accordance with the ethical principles that have their origin in the Declaration of Helsinki. It was carried out with patients verbal and analytical approval before sample was taken. The study protocol and the subject information and consent form were reviewed and approved by a local ethics committee according to the document (No.38) in date (28/2/2024) to get this approval.
Conflicts of Interests: There were no conflicts.
Authors' Contribution: Ibrahim AF (First Author), Introduction Writer/Methodologist/Original or Assistant Researcher/Discussion Writer (75%); Yasiry AA (Second Author), Statistical Analyst (25%)
Funding/Support: None declared by the authors.
Keywords:
References
1. Inan NK, Dinç L. Evaluation of nursing documentation on patient hygienic care. Int J Nurs Pract. 2013;19(1):81-7. [Link] [DOI:10.1111/ijn.12030]
2. Asmirajanti M, Hamid AY, Hariyati RT. Nursing care activities based on documentation. BMC Nurs. 2019;18(32):1-5. [Link] [DOI:10.1186/s12912-019-0352-0]
3. Hoffmann M, Sendlhofer G, Gombotz V, Pregartner G, Zierler R, Schwarz C, et al. Hand hygiene compliance in intensive care units: An observational study. Int J Nurs Pract. 2020;26(2):e12789. [Link] [DOI:10.1111/ijn.12789]
4. Styles MM, Schumann MJ, Bickford CJ, White K. Specialization and credentialing in nursing revisited: Understanding the issues, advancing the profession. Silver Spring: Amer Nurs Assn; 2008. [Link]
5. Abdallah KF, Ebraheim MN, Aziz Elbakry MRA. Nurses' performance toward quality documentation for patients in ICU: suggested guidelines. Egypt J Health Care. 2020;11(4):15-31. [Link] [DOI:10.21608/ejhc.2020.124845]
6. Alkouri OA, AlKhatib AJ, Kawafhah M. Importance and implementation of nursing documentation: review study. Eur Sci J. 2016;12(3):101-6. [Link] [DOI:10.19044/esj.2016.v12n3p101]
7. Törnvall E, Wilhelmsson S. Nursing documentation for communicating and evaluating care. J Clini Nurs. 2008;17(16):2116-24. [Link] [DOI:10.1111/j.1365-2702.2007.02149.x]
8. Akhu‐Zaheya L, Al‐Maaitah R, Bany Hani S. Quality of nursing documentation: Paper‐based health records versus electronic‐based health records. J Clin Nurs. 2018;27(3-4):e578-89. [Link] [DOI:10.1111/jocn.14097]
9. Lee RY, Knaplund C, Withall J, Bokhari SM, Cato KD, Rossetti SC. Variability in nursing documentation patterns across patients' hospital stays. InAMIA Annu Sympo Proc. 2023;2023:1037-46. [Link]
10. Wang N, Hailey D, Yu P. Quality of nursing documentation and approaches to its evaluation: A mixed‐method systematic review. J Adv Nurs. 2011;67(9):1858-75. [Link] [DOI:10.1111/j.1365-2648.2011.05634.x]
11. Dwi Hs B. Legal aspect of patient's medical record. Adv Econ Bus Manag Res. 2019;121:76-9. [Link]
12. McCaman B, Hirsh HL. Medical records-legal perspectives. Prim Care Clin Off Pract. 1979;6(3):681-91. [Link] [DOI:10.1016/S0095-4543(21)00822-8]
13. Bignell CA, Petrovskaya O. Understanding the role and impact of electronic health records in labor and delivery nursing practice: A scoping review protocol. Dig Health. 2024;10:20552076241249271. [Link] [DOI:10.1177/20552076241249271]
14. Mello MM, Frakes MD, Blumenkranz E, Studdert DM. Malpractice liability and health care quality: a review. Jama. 2020;323(4):352-66. [Link] [DOI:10.1001/jama.2019.21411]
15. Appel JM. When liability and ethics diverge. Focus. 2019;17(4):382-6. [Link] [DOI:10.1176/appi.focus.20190031]
16. Choi ES, Noh HJ, Chung WG, Mun SJ. Development of a competency for professional oral hygiene care of endotracheally-intubated patients in the intensive care unit: Development and validity evidence. BMC Health Serv Res. 2021;21(1):748. [Link] [DOI:10.1186/s12913-021-06755-z]
17. Currell R, Urquhart C. Nursing record systems: effects on nursing practice and health care outcomes. Cochrane Database Syst Rev. 2018;15(5):CD002099. [Link] [DOI:10.1002/14651858.CD002099.pub3]
18. Thompson D, Johnston P, Spurr C. The impact of electronic medical records on nursing efficiency. J Nurs Adm. 2009;39(10):444-51. [Link] [DOI:10.1097/NNA.0b013e3181b9209c]
19. Hoerbst A, Ammenwerth E. Electronic health records. Meth Inform Med. 2010;49(04):320-36. [Link] [DOI:10.3414/ME10-01-0038]
20. Saranto K, Kinnunen UM, Kivekäs E, Lappalainen AM, Liljamo P, Rajalahti E, et al. Impacts of structuring nursing records: a systematic review. Scand J Caring Sci. 2014;28(4):629-47. [Link] [DOI:10.1111/scs.12094]
21. De Groot K, De Veer AJ, Munster AM, Francke AL, Paans W. Nursing documentation and its relationship with perceived nursing workload: a mixed-methods study among community nurses. BMC Nurs. 2022;21(1):34. [Link] [DOI:10.1186/s12912-022-00811-7]
22. Ehrenberg A, Ehnfors M, Smedby B. Auditing nursing content in patient records. Scandinavian J Caring Sci. 2001;15(2):133-41. [Link] [DOI:10.1046/j.1471-6712.2001.00011.x]
23. Jefferies D, Johnson M, Nicholls D, Lad S. A ward-based writing coach program to improve the quality of nursing documentation. Nurse Educ Today. 2012;32(6):647-51. [Link] [DOI:10.1016/j.nedt.2011.08.017]
24. Artuvan Z, Çetin H. Hand hygiene beliefs and practices conditions of nurses in the intensive care unit: descriptive study. Turkiye Klinikleri J Nurs Sci. 2022;14(2). [Link] [DOI:10.5336/nurses.2021-85041]
25. Hou SI. Health education: theoretical concepts, effective strategies and core competencies. Health Promot Pract. 2014;15(5):619-21. [Link] [DOI:10.1177/1524839914538045]
26. Scannapieco FA. Role of oral bacteria in respiratory infection. J Periodontol. 1999;70(7):793-802. [Link] [DOI:10.1902/jop.1999.70.7.793]
27. Cutler LR, Sluman P. Reducing ventilator associated pneumonia in adult patients through high standards of oral care: a historical control study. Intens Crit Care Nurs. 2014;30(2):61-8. [Link] [DOI:10.1016/j.iccn.2013.08.005]
28. Peres MA, Macpherson LM, Weyant RJ, Daly B, Venturelli R, Mathur MR, et al. Oral diseases: a global public health challenge. The Lancet. 2019;394(10194):249-60. [Link] [DOI:10.1016/S0140-6736(19)31146-8]
29. Rello J, Koulenti D, Blot S, Sierra R, Diaz E, De Waele JJ, Macor A, Agbaht K, Rodriguez A. Oral care practices in intensive care units: a survey of 59 European ICUs. Intens Care Med. 2007;33:1066-70. [Link] [DOI:10.1007/s00134-007-0605-3]
30. Yeung KY, Chui YY. An exploration of factors affecting Hong Kong ICU nurses in providing oral care. J Clin Nurs. 2010;19(21‐22):3063-72. [Link] [DOI:10.1111/j.1365-2702.2010.03344.x]
31. Lin YS, Chang JC, Chang TH, Lou MF. Critical care nurses' knowledge, attitudes and practices of oral care for patients with oral endotracheal intubation: A questionnaire survey. J Clin Nurs. 2011;20(21‐22):3204-14. [Link] [DOI:10.1111/j.1365-2702.2011.03819.x]
32. Karthiga Priyadharshini A. A study to assess the effectiveness of neem extract in promoting oral hygiene among unconscious patients admitted in Rajiv Gandhi Government General Hospital, Chennai [dissertation]. Chennai: College of Nursing, Madras Medical College; 2016. [Link]
33. Mohaithef MA. Assessing hand hygiene practices among nurses in the Kingdom of Saudi Arabia. Open Public Health J. 2020;13(1):220-6. [Link] [DOI:10.2174/1874944502013010220]
34. Ebrahim Aboalizm S, Abdel Aziz Kasemy Z. Nurses knowledge, attitude and practice toward mouth hygiene among critical ill patients. Int J Novel Res Healthc Nurs. 2016;3(3):1-15. [Link]
35. Abid RI, Majeed HM, Mohammed TR. Assessment of nurses documentation for nursing care at surgical wards in Baghdad teaching hospitals. J Pharm Sci Res. 2018;10(10):2568-71. [Link]
36. Ali BG. Assessment of nurses' knowledge regarding care of unconsciousness patients in El-mak Nimer University Hospital. Shendi University, Faculty of Graduated Studies and Scientific Research. 2014;1:1-35. [Link]
37. Kadhim AJ, Khudur KM. Effectiveness of an instructional program on nurses' performance toward unconscious patients' personal hygiene in intensive care unit at teaching neurosurgical hospital at Baghdad City. Drugs Cell Ther Hematol. 2021;10(1):1522-8. [Link]
38. Khudhair AS. Nurse's practice concerning mouth care for unconscious or debilitated patient. Int J Cur Tr Res. 2014;3(2):104-8. [Link]
39. Dagnew ZA, Abraham IA, Beraki GG, Tesfamariam EH, Mittler S, Tesfamichael YZ. Nurses' attitude towards oral care and their practicing level for hospitalized patients in Orotta National Referral Hospital, Asmara-Eritrea: A cross-sectional study. BMC Nurs. 2020;19:63. [Link] [DOI:10.1186/s12912-020-00457-3]
40. Deldar K, Froutan R, Ebadi A. Challenges faced by nurses in using pain assessment scale in patients unable to communicate: A qualitative study. BMC Nurs. 2018;17:11. [Link] [DOI:10.1186/s12912-018-0281-3]
41. Abdallah KF, Ebraheim MN, Aziz Elbakry MRA. Nurses' performance toward quality documentation for patients in ICU: suggested guidelines. Egypt J Health Care. 2020;11(4):15-31. [Link] [DOI:10.21608/ejhc.2020.124845]