Volume 16, Issue 2 (2024)
Iran J War Public Health 2024, 16(2): 161-167 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2024/04/22 | Accepted: 2024/08/6 | Published: 2024/08/21
Received: 2024/04/22 | Accepted: 2024/08/6 | Published: 2024/08/21
How to cite this article
M. Noori A, Al-Obaidi M. Social Interaction and Its Association with Quality of Life among Lower Limb Amputees. Iran J War Public Health 2024; 16 (2) :161-167
URL: http://ijwph.ir/article-1-1455-en.html
URL: http://ijwph.ir/article-1-1455-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Authors
A.K. M. Noori *1, M.J.L. Al-Obaidi2
1- Department of Community Health, Faculty of Nursing, University of Baghdad, Baghdad, Iraq
2- Department of Tropical Biological Research, Faculty of Science, University of Baghdad, Baghdad, Iraq
2- Department of Tropical Biological Research, Faculty of Science, University of Baghdad, Baghdad, Iraq
Full-Text (HTML) (1537 Views)
Introduction
Amputation is one of the main causes of permanent disability. The loss of a limb, especially a lower limb, represents a significant physical and mental challenge for individuals, profoundly affecting their quality of life (QoL). Individuals with lower limb amputations face various challenges, including learning to care for their amputated limb, relearning how to walk, and finding ways to adjust to and cope with their loss. Lower limb amputation can lead to mobility limitations, altered body image, and feelings of dependency, all of which collectively impact an individual’s social interactions and overall well-being [1]. Amputation is frequently linked to feelings of anxiety, isolation, and depression, which can alter the social and leisure activities of individuals with lower limb amputations. Approximately 73.5% of limb losses involve lower limb amputations, primarily resulting from traumatic injuries and vascular diseases. Conditions, such as lower limb amputation, stroke, or spinal cord injuries often hinder individuals from carrying out daily activities and participating in physical and social engagements. In Iraq, lower limb amputations primarily result from a combination of factors, including war-related accidents, diabetes, and inadequate healthcare infrastructure. Prolonged wars, including battles, as well as recent conflicts involving insurgencies and terrorist activities, have significantly contributed to the high incidence of necessary amputations [2]. Additionally, Iraq’s healthcare system has been under immense pressure, limiting its ability to effectively manage chronic conditions such as diabetes, which in turn increases the risk of complications involving peripheral vascular disturbances that can lead to amputation [3].
The prevalence of lower extremity amputations in Iraq is very high. The period following the 2003 invasion highlighted a significant increase in amputations, many of which are attributable to conflict-related injuries. Furthermore, Iraq suffers from one of the highest rates of diabetes in the Middle East, which exacerbates the problem. Access to the best treatment and rehabilitation services in hospitals is also limited, resulting in many patients with chronic diseases not receiving timely treatment, thereby increasing the likelihood of complications that may require amputation. Thus, lower limb amputations remain a severe public health issue in Iraq, underscoring the need to enhance healthcare offerings and infrastructure [4-6]. Amputation necessitates that patients reorganize their lifestyles, potentially altering their work situations or even leaving their jobs altogether. Those who have experienced amputations often find themselves less independent and need to depend on others for assistance. The loss of a limb can trigger a grieving process that requires time for adjustment. During this adjustment period, individuals may experience various physical, functional, and psychological challenges as they navigate their new circumstances.
Social interaction plays a pivotal role in the lives of people with lower extremity amputations. Engaging in social activities and maintaining relationships can enhance emotional well-being, provide a sense of belonging, and improve overall life enjoyment [7]. However, the stigma and physical obstacles associated with amputation can limit social engagement, leading to isolation and a diminished QoL [8]. It is crucial to explore how social interaction affects the QoL of lower limb amputees to identify areas for intervention and support [1]. Social support emerges as an important mediator in the relationship between social interaction and QoL among lower-limb amputees. Social support includes emotional, informational, and practical assistance gained from family, friends, and the broader community. Research shows that strong social support networks can mitigate negative outcomes related to amputation, enhance resilience, and promote better health outcomes [9]. For lower extremity amputees, a social mentor can facilitate participation in social activities, boost self-esteem, and provide essential resources for coping with the challenges of amputation [10].
QoL is commonly defined as a general sense of well-being that relates to an individual’s perception of health and their ability to function effectively. Numerous studies connect QoL to functional capacity, suggesting that if a person cannot achieve full physical capability, their QoL is likely to be diminished. Although studies on QoL and amputees are becoming more common, QoL remains a relatively underexplored concept within this group. Over the past decade, research focusing on the psychosocial aspects of patients with limb amputations has gained traction in the literature. Individuals with lower limb amputations emphasize the significance of QoL in determining successful treatment outcomes. Despite this recognition, there are still relatively few studies that examine the various factors affecting the QoL for these individuals. Amputation profoundly impacts both physical and psychological well-being, leading to numerous changes in life [11]. One of the most critical consequences is functional limitation, which, if not properly managed, can result in permanent disability and may be perceived as a traumatic experience [12]. Consequently, losing a limb is a significant event that disrupts multiple aspects of a person’s life, including mobility [13], social participation [13], and the ability to return to work [14].
Individuals who have undergone lower limb amputation face an increased risk of reduced engagement in daily and social activities, which can adversely affect their QoL. Knežević et al. conducted a study comparing the QoL between patients who underwent amputation and healthy individuals. They found that individuals with intact limbs reported a significantly better QoL compared to those who had undergone amputation. Specifically, patients who had below-knee amputations demonstrated better physical performance and overall health than those who had above-knee amputations, who experienced an even lower QoL [15]. Mohammed et al. affirmed that lower limb amputation negatively impacts both physical and mental health. Their research indicated that factors such as age, sex, the location of the amputation, and marital status significantly affect QoL, while education level, type of employment, and living conditions do not have a notable impact on the QoL for patients following amputation [16]. Amputation is a multifaceted process that extends beyond a mere physical occurrence. QoL and health-related QoL in individuals with lower limb amputations tend to be lower at first but can be enhanced through several factors. These include the level of amputation and the underlying medical condition that necessitated it, overall clinical health, perceived social support, motivation, personal and social attributes, as well as the presence of depression, anxiety, and coping mechanisms [17]. Therefore, this study aimed to investigate the relationship between social interaction and QoL among lower extremity amputees, with specific attention to the mediating role of social support.
Instrument and Methods
Study design
This cross-sectional study was conducted on individuals who had undergone lower limb amputation and were receiving rehabilitation services in Baghdad from April to June 2024.
Inclusion criteria included adults aged 18 years and older who had undergone a lower limb amputation and had been living with the condition for at least six months. Participants were required to have the cognitive ability to understand and respond to the questionnaires and interviews, ensuring the reliability of the self-reported data. Additionally, they needed to provide informed consent to participate in the study. Exclusion criteria included individuals with severe psychiatric problems or cognitive impairments that may prevent them from perceiving and completing the test instruments. Those who had undergone amputations within the past six months were excluded to avoid confounding factors related to immediate postoperative recovery. Participants with concurrent underlying medical conditions, including advanced cancers or terminal organ disease, which would significantly impact QoL regardless of the nature of the amputation, were also excluded from the study.
Samples size
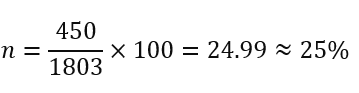
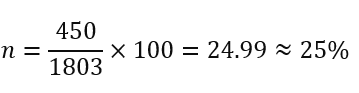
A sample size of 450 participants was determined using electrophoresis analysis to ensure adequate statistical power and the subjects were selected using convenience sampling method. Recruitment was facilitated through direct contact with patients in the centers and cooperation with healthcare companies. Given that 25% of the study group had an amputation and that 1803 visits to rehabilitation facilities occurred in a given month, this sample size was chosen in part due to these factors.
Research tools
The study tools were organized using a questionnaire designed to identify the socio-demographic characteristics, including age, gender, educational level, monthly income, and profession. Specific metrics were utilized extensively to investigate the information and data collected:
Social interaction
To operationalize social integration, the social integration subscale of the short form of the Craig Handicap Assessment and Reporting Technique (CHART) [18] was used. The CHART as a reliable test has been validated in the amputee population [19]. Scores are reported on a scale from 0 to 100, with lower ratings indicating a lower level of social integration. For the analysis, three categories of social integration, including high, medium, and low were created. Due to a significant ceiling effect in the chart scores, excessive social integration was defined as an excellent score of 100, while moderate and low social integration were determined based on the average social integration score for individuals without the highest ratings. Here, Cronbach’s alpha for this scale was 0.87, indicating its strong reliability.
Social support
The Social Support Rating Scale (SSRS) was used to assess patients’ social support and has been validated in Arabic [20]. The Cronbach’s alpha for this scale in this study was 0.79, indicating a good level of reliability.
Quality of Life
The World Health Organization Quality of Life-BREF (WHOQOL-BREF) is a 26-item assessment that includes questions on QoL and general health, as well as four domains, including physical health (seven items), psychological health (six items), social connections (three items), and environmental health (eight items). The physical health domain covers topics, such as energy, pain, sleep, mobility, daily activities, and functional capability. The psychological health domain includes measurements related to self-image, negative thoughts, positive attitudes, self-esteem, mental state, learning capacity, memory focus, and religion. The social relationships domain encompasses questions about sex life, social support, and personal connections. The environmental health domain includes aspects such as financial resources, safety, health and social services, physical living environment, learning opportunities, recreation, general environment (noise, air pollution, etc.), and transportation. Here, the Cronbach’s alpha was found to be 0.83.
Statistical analysis
All statistical analyses were conducted using SPSS version 20.0 software. Numbers and probabilities were used to rank the parameters, while the mean and standard deviation were utilized to statistically describe the continuous parameters. The Kolmogorov-Smirnov and Shapiro-Wilk tests were used to assess normality. Additionally, associations and predictions between the study parameters were examined using the Pearson correlation coefficient. A significance threshold of 0.05 was applied for the statistical interpretations.
Findings
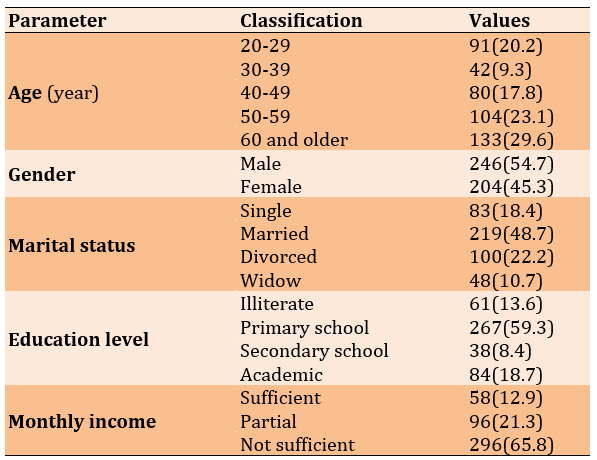
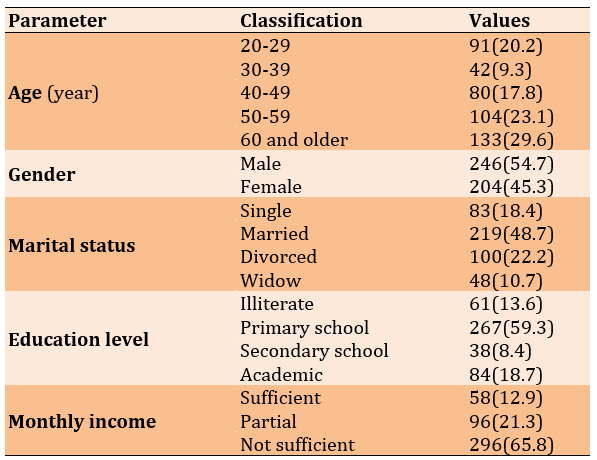
The average age of participants was 47.61±14.84 years, and ages ranged from 22 to 74 years. In terms of gender, lower limb amputation was more common among males (54.7%), while the remaining participants were female (45.3%). Regarding marital status, the majority were married (48.7%). In terms of educational attainment, more than half of the studied population were primary school graduates (59.3%). One-third of the observed population did not have sufficient monthly income (65.8%; Table 1).
Table 1. Frequency of participants’ sociodemographic characteristics
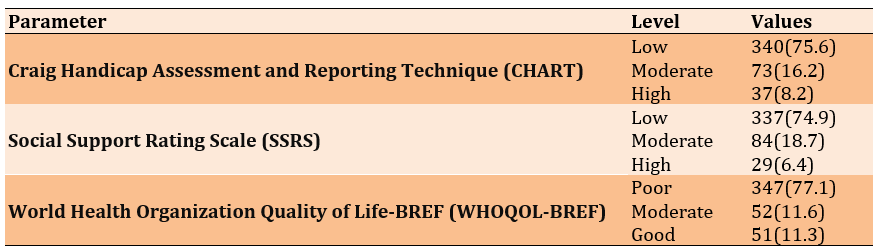
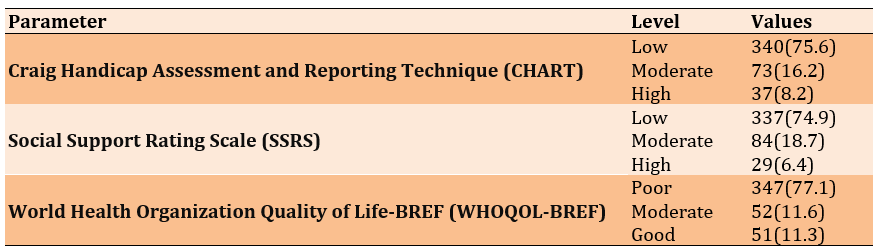
Also, 75.6% of lower limb amputees had low social interaction. Additionally, 74.9% reported receiving low social support, and 77.1% mentioned poor QoL (Table 2).
Table 2. Frequency of study samples based on the used scales
There was a strong correlation between social interaction and social support (r=0.754), a positive correlation between social interaction and QoL (r=0.830), and a positive correlation between social support and QoL among lower limb amputees (r=0.779; Table 3).
Table 3. Correlation between social interaction, quality of life, and social support among lower limb amputees

For every increase in social support by 0.36, there was a probability of an increase in social interaction by 0.71 among lower limb amputees (R2=0.56). Also, for every increase in social interaction by 0.14, there was a probability of an increase in QoL by 0.90 among lower limb amputees (R2=0.68). In addition for every increase in social support by 0.16, there was a probability of an increase in QoL by 0.89 among lower limb amputees (R2=0.60).
Discussion
This study aimed to investigate the association between social interaction and quality of life among lower limb amputees, specifically focusing on the mediating role of social support. We found that 75.6% of limb loss amputees had low social interaction, which highlights a significant social challenge faced by this population. Amputation can lead to social isolation due to various factors, including mobility barriers, mental distress, and societal stigma. This loss of social interaction can contribute to feelings of loneliness and depression, as supported by previous research indicating that amputees often encounter barriers in maintaining their social networks and engaging in community activities [21]. Furthermore, the physical and emotional adjustments required after amputation can hinder an individual’s ability to participate in social activities, exacerbating the sense of isolation [22].
In addition to low social interaction, 74.9% of lower limb amputees reported receiving low social support, underscoring another critical issue. Social guidance is a critical factor in the rehabilitation and overall well-being of amputees. It has been proven that robust social support networks can enhance coping mechanisms, improve mental outcomes, and facilitate better adaptation to new physical realities [9, 23]. The lack of adequate social support can result in increased stress, anxiety, and depression among amputees, hindering their rehabilitation process and QoL [24]. This deficiency in social support may stem from the loss of relationships, changes in social roles, and the inability of family and friends to fully understand and support the amputee’s needs. The reported 77.1% of limb loss amputees experiencing poor QoL is indicative of the profound impact amputation has on various life domains. QoL encompasses physical, mental, and social well-being, all of which can be significantly affected by amputation. Previous studies have consistently found that amputees tend to report lower QoL compared to the general population, with issues such as chronic pain, phantom limb sensations, and loss of mobility contributing to this decline [25]. Psychological factors, including despair, anxiety, and body image disturbances, also play a significant role in diminishing QoL among amputees [26]. The interrelationship among low social interaction, insufficient social support, and poor QoL presents a complex network of challenges that need to be addressed holistically to improve the overall well-being of limb-loss amputees.
The findings that a majority of limb loss amputees experience low social interaction, inadequate social support, and a negative QoL are consistent with current literature. These interrelated issues underscore the importance of comprehensive rehabilitation programs that address not only the physical but also the social and mental needs of amputees. Interventions aimed at improving social integration, providing robust social support networks, and enhancing mental health services are crucial for improving the QoL for this population. Future research needs to continue exploring these dimensions and develop targeted strategies to mitigate the negative effects of amputation on social and mental well-being.
Understanding the effective correlation between social interaction and social support among lower limb amputees is critical for enhancing their overall well-being and QoL. Previous studies have consistently demonstrated that social support plays a significant role in mitigating the psychosocial challenges faced by individuals with limb loss [9, 23]. The findings indicated that for each increase in perceived social support by 0.36 units, there was a corresponding increase of 0.71 units in social interaction levels among this population. This aligns with a longitudinal study focusing on amputees, reporting an association between higher levels of perceived social support and increased engagement in social activities. This study reported that individuals who perceive greater support from their social networks tend to participate more actively in social interactions, thereby fostering a sense of belonging and reducing feelings of isolation [27]. This is consistent with the results of the current study, which demonstrated a quantifiable relationship between perceived social support and actual social engagement among lower limb amputees. The positive correlation identified between social interaction and social support underscores the importance of targeted interventions that strengthen social networks within the amputee community. By addressing and improving perceived levels of social support, healthcare professionals and support providers can potentially enhance the social integration and well-being of individuals adjusting to life after limb loss.
Increased social interaction correlates with a better QoL among lower limb amputees, the results underscoring the important role of social support in rehabilitation and adjustment post-amputation. Previous research supports this relationship, suggesting that social interaction serves as a buffer against mental distress and promotes overall well-being [28]. The observed increase in life satisfaction by 0.90 for each 0.14 increase in social interaction aligns with research highlighting the psychosocial benefits of social networks among individuals facing significant health challenges [29]. Moreover, the large coefficient of determination suggests that social interaction explains a substantial proportion of the variance in exceptional life outcomes among limb loss amputees. This reinforces the robustness of the relationship identified in the study and indicates that interventions focused on enhancing social integration may yield significant improvements in quality-of-life metrics [9, 23]. These interventions may include support groups, peer counseling programs, and community reintegration projects, all aimed at strengthening social ties and reducing isolation among amputees. The study findings provide compelling evidence that increased social interaction is significantly associated with improved QoL among limb-loss amputees. By recognizing and enhancing the supportive role of social networks, healthcare providers can better tailor interventions to promote not only physical recovery but also psychosocial adjustment and overall well-being for individuals living with limb loss.
Based on the findings that growth in social support was correlated with improved QoL among limb loss amputees, the outcomes underscore the significant role of social support networks in rehabilitation and adjustment following amputation. This relationship aligns with prior studies indicating that social support serves as a critical determinant of well-being and adaptation to disability [30, 31]. Social support not only enhances mental resilience but also contributes to physical rehabilitation outcomes, suggesting a multifaceted effect on overall QoL [32]. Moreover, the located coefficient of 0.16 indicates a direct, albeit modest, linear correlation between social support and QoL enhancements among limb loss amputees. This finding echoes the conclusions of Rafnsson et al., who referred to comparable developments in their longitudinal study on disability and social integration. They argued that higher levels of social support facilitate greater emotional adjustment and participation in social activities, thereby improving perceived life satisfaction and reducing mental distress [33]. The robustness of these findings is further supported by the substantial R2 value of 0.60, indicating that approximately 60.7% of the variance in QoL among limb loss amputees can be explained by variations in social support levels. This statistical significance underscores the practical implications for healthcare providers and policymakers, emphasizing the importance of fostering supportive environments and interventions aimed at bolstering social networks for individuals adapting to limb loss.
Several limitations must be acknowledged. The substantial reliance on self-reported measures of social interaction, social support, and QoL introduces potential response biases and subjective interpretations. The observer’s focus on a selected population (lower limb amputees) may also limit the generalizability of the findings to broader groups of amputees or those with different levels of amputation. Additionally, the study did not examine potential confounding factors, such as comorbidities or socioeconomic status, which may have an impact on both social interaction and QoL outcomes.
The high incidence of low social interaction, inadequate social support, and poor QoL underscores the need for interventions that enhance both social support structures and opportunities for social interaction among this population. The strong correlations identified within the figures emphasize the potential benefits of increasing social support and fostering greater social interaction, which can be linked to improvements in the quality of QoL. Therefore, it is recommended that interventions focus on enhancing social support networks and promoting opportunities for social interaction to improve the well-being of lower-limb amputees.
Conclusion
Lower limb amputees face significant challenges related to social interaction, social support, and overall QoL.
Acknowledgments: We would like to thank all the participants who permitted us to interview them for their close cooperation and participation.
Ethical Permissions: Ethical approval was obtained from the Research Ethics Committee at the University of Baghdad/College of Nursing (No.: 341, dated 4/02/2024).
Conflicts of Interests: The authors declared no conflicts of interests.
Authors' Contribution: M Noori AK (First Author), Introduction Writer/Methodologist/Main Researcher (50%); Al-Obaidi MJL (Second Author), Assistant Researcher/Discussion Writer/Statistical Analyst (50%)
Funding/Support: The present study did not receive any financial support.
Amputation is one of the main causes of permanent disability. The loss of a limb, especially a lower limb, represents a significant physical and mental challenge for individuals, profoundly affecting their quality of life (QoL). Individuals with lower limb amputations face various challenges, including learning to care for their amputated limb, relearning how to walk, and finding ways to adjust to and cope with their loss. Lower limb amputation can lead to mobility limitations, altered body image, and feelings of dependency, all of which collectively impact an individual’s social interactions and overall well-being [1]. Amputation is frequently linked to feelings of anxiety, isolation, and depression, which can alter the social and leisure activities of individuals with lower limb amputations. Approximately 73.5% of limb losses involve lower limb amputations, primarily resulting from traumatic injuries and vascular diseases. Conditions, such as lower limb amputation, stroke, or spinal cord injuries often hinder individuals from carrying out daily activities and participating in physical and social engagements. In Iraq, lower limb amputations primarily result from a combination of factors, including war-related accidents, diabetes, and inadequate healthcare infrastructure. Prolonged wars, including battles, as well as recent conflicts involving insurgencies and terrorist activities, have significantly contributed to the high incidence of necessary amputations [2]. Additionally, Iraq’s healthcare system has been under immense pressure, limiting its ability to effectively manage chronic conditions such as diabetes, which in turn increases the risk of complications involving peripheral vascular disturbances that can lead to amputation [3].
The prevalence of lower extremity amputations in Iraq is very high. The period following the 2003 invasion highlighted a significant increase in amputations, many of which are attributable to conflict-related injuries. Furthermore, Iraq suffers from one of the highest rates of diabetes in the Middle East, which exacerbates the problem. Access to the best treatment and rehabilitation services in hospitals is also limited, resulting in many patients with chronic diseases not receiving timely treatment, thereby increasing the likelihood of complications that may require amputation. Thus, lower limb amputations remain a severe public health issue in Iraq, underscoring the need to enhance healthcare offerings and infrastructure [4-6]. Amputation necessitates that patients reorganize their lifestyles, potentially altering their work situations or even leaving their jobs altogether. Those who have experienced amputations often find themselves less independent and need to depend on others for assistance. The loss of a limb can trigger a grieving process that requires time for adjustment. During this adjustment period, individuals may experience various physical, functional, and psychological challenges as they navigate their new circumstances.
Social interaction plays a pivotal role in the lives of people with lower extremity amputations. Engaging in social activities and maintaining relationships can enhance emotional well-being, provide a sense of belonging, and improve overall life enjoyment [7]. However, the stigma and physical obstacles associated with amputation can limit social engagement, leading to isolation and a diminished QoL [8]. It is crucial to explore how social interaction affects the QoL of lower limb amputees to identify areas for intervention and support [1]. Social support emerges as an important mediator in the relationship between social interaction and QoL among lower-limb amputees. Social support includes emotional, informational, and practical assistance gained from family, friends, and the broader community. Research shows that strong social support networks can mitigate negative outcomes related to amputation, enhance resilience, and promote better health outcomes [9]. For lower extremity amputees, a social mentor can facilitate participation in social activities, boost self-esteem, and provide essential resources for coping with the challenges of amputation [10].
QoL is commonly defined as a general sense of well-being that relates to an individual’s perception of health and their ability to function effectively. Numerous studies connect QoL to functional capacity, suggesting that if a person cannot achieve full physical capability, their QoL is likely to be diminished. Although studies on QoL and amputees are becoming more common, QoL remains a relatively underexplored concept within this group. Over the past decade, research focusing on the psychosocial aspects of patients with limb amputations has gained traction in the literature. Individuals with lower limb amputations emphasize the significance of QoL in determining successful treatment outcomes. Despite this recognition, there are still relatively few studies that examine the various factors affecting the QoL for these individuals. Amputation profoundly impacts both physical and psychological well-being, leading to numerous changes in life [11]. One of the most critical consequences is functional limitation, which, if not properly managed, can result in permanent disability and may be perceived as a traumatic experience [12]. Consequently, losing a limb is a significant event that disrupts multiple aspects of a person’s life, including mobility [13], social participation [13], and the ability to return to work [14].
Individuals who have undergone lower limb amputation face an increased risk of reduced engagement in daily and social activities, which can adversely affect their QoL. Knežević et al. conducted a study comparing the QoL between patients who underwent amputation and healthy individuals. They found that individuals with intact limbs reported a significantly better QoL compared to those who had undergone amputation. Specifically, patients who had below-knee amputations demonstrated better physical performance and overall health than those who had above-knee amputations, who experienced an even lower QoL [15]. Mohammed et al. affirmed that lower limb amputation negatively impacts both physical and mental health. Their research indicated that factors such as age, sex, the location of the amputation, and marital status significantly affect QoL, while education level, type of employment, and living conditions do not have a notable impact on the QoL for patients following amputation [16]. Amputation is a multifaceted process that extends beyond a mere physical occurrence. QoL and health-related QoL in individuals with lower limb amputations tend to be lower at first but can be enhanced through several factors. These include the level of amputation and the underlying medical condition that necessitated it, overall clinical health, perceived social support, motivation, personal and social attributes, as well as the presence of depression, anxiety, and coping mechanisms [17]. Therefore, this study aimed to investigate the relationship between social interaction and QoL among lower extremity amputees, with specific attention to the mediating role of social support.
Instrument and Methods
Study design
This cross-sectional study was conducted on individuals who had undergone lower limb amputation and were receiving rehabilitation services in Baghdad from April to June 2024.
Inclusion criteria included adults aged 18 years and older who had undergone a lower limb amputation and had been living with the condition for at least six months. Participants were required to have the cognitive ability to understand and respond to the questionnaires and interviews, ensuring the reliability of the self-reported data. Additionally, they needed to provide informed consent to participate in the study. Exclusion criteria included individuals with severe psychiatric problems or cognitive impairments that may prevent them from perceiving and completing the test instruments. Those who had undergone amputations within the past six months were excluded to avoid confounding factors related to immediate postoperative recovery. Participants with concurrent underlying medical conditions, including advanced cancers or terminal organ disease, which would significantly impact QoL regardless of the nature of the amputation, were also excluded from the study.
Samples size
A sample size of 450 participants was determined using electrophoresis analysis to ensure adequate statistical power and the subjects were selected using convenience sampling method. Recruitment was facilitated through direct contact with patients in the centers and cooperation with healthcare companies. Given that 25% of the study group had an amputation and that 1803 visits to rehabilitation facilities occurred in a given month, this sample size was chosen in part due to these factors.
Research tools
The study tools were organized using a questionnaire designed to identify the socio-demographic characteristics, including age, gender, educational level, monthly income, and profession. Specific metrics were utilized extensively to investigate the information and data collected:
Social interaction
To operationalize social integration, the social integration subscale of the short form of the Craig Handicap Assessment and Reporting Technique (CHART) [18] was used. The CHART as a reliable test has been validated in the amputee population [19]. Scores are reported on a scale from 0 to 100, with lower ratings indicating a lower level of social integration. For the analysis, three categories of social integration, including high, medium, and low were created. Due to a significant ceiling effect in the chart scores, excessive social integration was defined as an excellent score of 100, while moderate and low social integration were determined based on the average social integration score for individuals without the highest ratings. Here, Cronbach’s alpha for this scale was 0.87, indicating its strong reliability.
Social support
The Social Support Rating Scale (SSRS) was used to assess patients’ social support and has been validated in Arabic [20]. The Cronbach’s alpha for this scale in this study was 0.79, indicating a good level of reliability.
Quality of Life
The World Health Organization Quality of Life-BREF (WHOQOL-BREF) is a 26-item assessment that includes questions on QoL and general health, as well as four domains, including physical health (seven items), psychological health (six items), social connections (three items), and environmental health (eight items). The physical health domain covers topics, such as energy, pain, sleep, mobility, daily activities, and functional capability. The psychological health domain includes measurements related to self-image, negative thoughts, positive attitudes, self-esteem, mental state, learning capacity, memory focus, and religion. The social relationships domain encompasses questions about sex life, social support, and personal connections. The environmental health domain includes aspects such as financial resources, safety, health and social services, physical living environment, learning opportunities, recreation, general environment (noise, air pollution, etc.), and transportation. Here, the Cronbach’s alpha was found to be 0.83.
Statistical analysis
All statistical analyses were conducted using SPSS version 20.0 software. Numbers and probabilities were used to rank the parameters, while the mean and standard deviation were utilized to statistically describe the continuous parameters. The Kolmogorov-Smirnov and Shapiro-Wilk tests were used to assess normality. Additionally, associations and predictions between the study parameters were examined using the Pearson correlation coefficient. A significance threshold of 0.05 was applied for the statistical interpretations.
Findings
The average age of participants was 47.61±14.84 years, and ages ranged from 22 to 74 years. In terms of gender, lower limb amputation was more common among males (54.7%), while the remaining participants were female (45.3%). Regarding marital status, the majority were married (48.7%). In terms of educational attainment, more than half of the studied population were primary school graduates (59.3%). One-third of the observed population did not have sufficient monthly income (65.8%; Table 1).
Table 1. Frequency of participants’ sociodemographic characteristics
Also, 75.6% of lower limb amputees had low social interaction. Additionally, 74.9% reported receiving low social support, and 77.1% mentioned poor QoL (Table 2).
Table 2. Frequency of study samples based on the used scales
There was a strong correlation between social interaction and social support (r=0.754), a positive correlation between social interaction and QoL (r=0.830), and a positive correlation between social support and QoL among lower limb amputees (r=0.779; Table 3).
Table 3. Correlation between social interaction, quality of life, and social support among lower limb amputees

For every increase in social support by 0.36, there was a probability of an increase in social interaction by 0.71 among lower limb amputees (R2=0.56). Also, for every increase in social interaction by 0.14, there was a probability of an increase in QoL by 0.90 among lower limb amputees (R2=0.68). In addition for every increase in social support by 0.16, there was a probability of an increase in QoL by 0.89 among lower limb amputees (R2=0.60).
Discussion
This study aimed to investigate the association between social interaction and quality of life among lower limb amputees, specifically focusing on the mediating role of social support. We found that 75.6% of limb loss amputees had low social interaction, which highlights a significant social challenge faced by this population. Amputation can lead to social isolation due to various factors, including mobility barriers, mental distress, and societal stigma. This loss of social interaction can contribute to feelings of loneliness and depression, as supported by previous research indicating that amputees often encounter barriers in maintaining their social networks and engaging in community activities [21]. Furthermore, the physical and emotional adjustments required after amputation can hinder an individual’s ability to participate in social activities, exacerbating the sense of isolation [22].
In addition to low social interaction, 74.9% of lower limb amputees reported receiving low social support, underscoring another critical issue. Social guidance is a critical factor in the rehabilitation and overall well-being of amputees. It has been proven that robust social support networks can enhance coping mechanisms, improve mental outcomes, and facilitate better adaptation to new physical realities [9, 23]. The lack of adequate social support can result in increased stress, anxiety, and depression among amputees, hindering their rehabilitation process and QoL [24]. This deficiency in social support may stem from the loss of relationships, changes in social roles, and the inability of family and friends to fully understand and support the amputee’s needs. The reported 77.1% of limb loss amputees experiencing poor QoL is indicative of the profound impact amputation has on various life domains. QoL encompasses physical, mental, and social well-being, all of which can be significantly affected by amputation. Previous studies have consistently found that amputees tend to report lower QoL compared to the general population, with issues such as chronic pain, phantom limb sensations, and loss of mobility contributing to this decline [25]. Psychological factors, including despair, anxiety, and body image disturbances, also play a significant role in diminishing QoL among amputees [26]. The interrelationship among low social interaction, insufficient social support, and poor QoL presents a complex network of challenges that need to be addressed holistically to improve the overall well-being of limb-loss amputees.
The findings that a majority of limb loss amputees experience low social interaction, inadequate social support, and a negative QoL are consistent with current literature. These interrelated issues underscore the importance of comprehensive rehabilitation programs that address not only the physical but also the social and mental needs of amputees. Interventions aimed at improving social integration, providing robust social support networks, and enhancing mental health services are crucial for improving the QoL for this population. Future research needs to continue exploring these dimensions and develop targeted strategies to mitigate the negative effects of amputation on social and mental well-being.
Understanding the effective correlation between social interaction and social support among lower limb amputees is critical for enhancing their overall well-being and QoL. Previous studies have consistently demonstrated that social support plays a significant role in mitigating the psychosocial challenges faced by individuals with limb loss [9, 23]. The findings indicated that for each increase in perceived social support by 0.36 units, there was a corresponding increase of 0.71 units in social interaction levels among this population. This aligns with a longitudinal study focusing on amputees, reporting an association between higher levels of perceived social support and increased engagement in social activities. This study reported that individuals who perceive greater support from their social networks tend to participate more actively in social interactions, thereby fostering a sense of belonging and reducing feelings of isolation [27]. This is consistent with the results of the current study, which demonstrated a quantifiable relationship between perceived social support and actual social engagement among lower limb amputees. The positive correlation identified between social interaction and social support underscores the importance of targeted interventions that strengthen social networks within the amputee community. By addressing and improving perceived levels of social support, healthcare professionals and support providers can potentially enhance the social integration and well-being of individuals adjusting to life after limb loss.
Increased social interaction correlates with a better QoL among lower limb amputees, the results underscoring the important role of social support in rehabilitation and adjustment post-amputation. Previous research supports this relationship, suggesting that social interaction serves as a buffer against mental distress and promotes overall well-being [28]. The observed increase in life satisfaction by 0.90 for each 0.14 increase in social interaction aligns with research highlighting the psychosocial benefits of social networks among individuals facing significant health challenges [29]. Moreover, the large coefficient of determination suggests that social interaction explains a substantial proportion of the variance in exceptional life outcomes among limb loss amputees. This reinforces the robustness of the relationship identified in the study and indicates that interventions focused on enhancing social integration may yield significant improvements in quality-of-life metrics [9, 23]. These interventions may include support groups, peer counseling programs, and community reintegration projects, all aimed at strengthening social ties and reducing isolation among amputees. The study findings provide compelling evidence that increased social interaction is significantly associated with improved QoL among limb-loss amputees. By recognizing and enhancing the supportive role of social networks, healthcare providers can better tailor interventions to promote not only physical recovery but also psychosocial adjustment and overall well-being for individuals living with limb loss.
Based on the findings that growth in social support was correlated with improved QoL among limb loss amputees, the outcomes underscore the significant role of social support networks in rehabilitation and adjustment following amputation. This relationship aligns with prior studies indicating that social support serves as a critical determinant of well-being and adaptation to disability [30, 31]. Social support not only enhances mental resilience but also contributes to physical rehabilitation outcomes, suggesting a multifaceted effect on overall QoL [32]. Moreover, the located coefficient of 0.16 indicates a direct, albeit modest, linear correlation between social support and QoL enhancements among limb loss amputees. This finding echoes the conclusions of Rafnsson et al., who referred to comparable developments in their longitudinal study on disability and social integration. They argued that higher levels of social support facilitate greater emotional adjustment and participation in social activities, thereby improving perceived life satisfaction and reducing mental distress [33]. The robustness of these findings is further supported by the substantial R2 value of 0.60, indicating that approximately 60.7% of the variance in QoL among limb loss amputees can be explained by variations in social support levels. This statistical significance underscores the practical implications for healthcare providers and policymakers, emphasizing the importance of fostering supportive environments and interventions aimed at bolstering social networks for individuals adapting to limb loss.
Several limitations must be acknowledged. The substantial reliance on self-reported measures of social interaction, social support, and QoL introduces potential response biases and subjective interpretations. The observer’s focus on a selected population (lower limb amputees) may also limit the generalizability of the findings to broader groups of amputees or those with different levels of amputation. Additionally, the study did not examine potential confounding factors, such as comorbidities or socioeconomic status, which may have an impact on both social interaction and QoL outcomes.
The high incidence of low social interaction, inadequate social support, and poor QoL underscores the need for interventions that enhance both social support structures and opportunities for social interaction among this population. The strong correlations identified within the figures emphasize the potential benefits of increasing social support and fostering greater social interaction, which can be linked to improvements in the quality of QoL. Therefore, it is recommended that interventions focus on enhancing social support networks and promoting opportunities for social interaction to improve the well-being of lower-limb amputees.
Conclusion
Lower limb amputees face significant challenges related to social interaction, social support, and overall QoL.
Acknowledgments: We would like to thank all the participants who permitted us to interview them for their close cooperation and participation.
Ethical Permissions: Ethical approval was obtained from the Research Ethics Committee at the University of Baghdad/College of Nursing (No.: 341, dated 4/02/2024).
Conflicts of Interests: The authors declared no conflicts of interests.
Authors' Contribution: M Noori AK (First Author), Introduction Writer/Methodologist/Main Researcher (50%); Al-Obaidi MJL (Second Author), Assistant Researcher/Discussion Writer/Statistical Analyst (50%)
Funding/Support: The present study did not receive any financial support.
Keywords:
References
1. Calabrese L, Maffoni M, Torlaschi V, Pierobon A. What is hidden behind amputation? Quanti-qualitative systematic review on psychological adjustment and quality of life in lower limb amputees for non-traumatic reasons. Healthcare. 2023;11(11):1661. [Link] [DOI:10.3390/healthcare11111661]
2. Hassan NS. Risk factors for diabetic foot amputation in sample of Iraqi patients. Natl J Clin Orthop. 2019;3(3):36-9. [Link] [DOI:10.33545/orthor.2019.v3.i3a.159]
3. Radhi MM. Degree of disease acceptance and health seeking behaviors for type 2 diabetic patients at diabetic center in Hilla City. Medico Leg Update. 2020;20(2):853-8. [Link] [DOI:10.37506/mlu.v20i2.1347]
4. Melcer T, Walker J, Sechriest VF, Bhatnagar V, Richard E, Perez K, et al. A retrospective comparison of five‐year health outcomes following upper limb amputation and serious upper limb injury in the Iraq and Afghanistan conflicts. PM R. 2019;11(6):577-89. [Link] [DOI:10.1002/pmrj.12047]
5. Yasir AA, Qassim WJ, Radhi MM. Assessment the feeling of psychological loneliness among wives of martyrs in the light of some social variables in Babylon Governorate/Iraq. J Pharm Sci Res. 2018;10(1):40-4. [Link]
6. Qassim WJ, Yasir AA, Radhi MM. Assessment of self hardness and its relationship to treatment acceptance for patients with diabetes mellitus at diabetic center in Hilla City/Iraq. J Pharm Sci Res. 2018;10(1):142-5. [Link]
7. Pereira MG, Ramos C, Lobarinhas A, Machado JC, Pedras S. Satisfaction with life in individuals with a lower limb amputation: The importance of active coping and acceptance. Scand J Psychol. 2018;59(4):414-21. [Link] [DOI:10.1111/sjop.12444]
8. Kizilkurt OK, Kizilkurt T, Gulec MY, Giynas FE, Polat G, Kilicoglu OI, et al. Quality of life after lower extremity amputation due to diabetic foot ulcer: The role of prosthesis-related factors, body image, self-esteem, and coping styles. Dusunen Adam J Psychiatry Neurolog Sci. 2020;33(2):109-19. [Link] [DOI:10.14744/DAJPNS.2020.00070]
9. Juma Elywy G, Radhi MM, Khyoosh Al-Eqabi QA. Social support and its association with the quality of life (QoL) of amputees. Iran Rehabil J. 2022;20(2):253-60. [Link] [DOI:10.32598/irj.20.2.1784.1]
10. Radhi MM, Abd RK, Al Eqabi QA. The body image and its relation to self-esteem among amputation patients at Artificial Limbs Hospital at Kut City, Iraq. J Public Health Afr. 2022;13(4):1-9. [Link] [DOI:10.4081/jphia.2022.1228]
11. Gozaydinoglu S, Hosbay Z, Durmaz H. Body image perception, compliance with a prosthesis and cognitive performance in transfemoral amputees. Acta orthopaedica et traumatologica turcica. 2019;53(3):221-5. [Link] [DOI:10.1016/j.aott.2019.03.014]
12. Canbolat Seyman C, Uzar Ozcetin YS. "I wish I could have my leg": a qualitative study on the experiences of individuals with lower limb amputation. Clin Nurs Res. 2022;31(3):509-18. [Link] [DOI:10.1177/10547738211047711]
13. Benavent JV, Tenías JM, Pellin A, Casaña Mohedo J, Cabellos-García AC, Gea-Caballero V. Sociodemographic determinants for the health-related quality of life of patients with vascular amputations as determined with the prosthesis evaluation questionnaire. Int J Environ Res Public Health. 2020;17(8):2691. [Link] [DOI:10.3390/ijerph17082691]
14. Unwin J, Kacperek L, Clarke C. A prospective study of positive adjustment to lower limb amputation. Clin Rehabil. 2009;23(11):1044-50. [Link] [DOI:10.1177/0269215509339001]
15. Knežević A, Salamon T, Milankov M, Ninković S, Jeremić-Knežević M, Tomašević-Todorović S. Assessment of quality of life in patients after lower limb amputation. Med Pregl. 2015;68(3-4):103-8. [Link] [DOI:10.2298/MPNS1504103K]
16. Mohammed SA, Shebl AM. Quality of life among Egyptian patients with upper and lower limb amputation: sex differences. Adv Med. 2014;2014(1):674323. [Link] [DOI:10.1155/2014/674323]
17. Calabrese L, Maffoni M, Torlaschi V, Pierobon A. What is hidden behind amputation? Quanti-qualitative systematic review on psychological adjustment and quality of life in lower limb amputees for non-traumatic reasons. Healthcare. 2023; 11(11): 1661. [Link] [DOI:10.3390/healthcare11111661]
18. Walker N, Mellick D, Brooks CA, Whiteneck GG. Measuring participation across impairment groups using the craig handicap assessment reporting technique. Am J Phys Med Rehabil. 2003;82(12):936-41. [Link] [DOI:10.1097/01.PHM.0000098041.42394.9A]
19. Walker JL, Knapp D, Minter C, Boakes JL, Salazar JC, Sanders JO, et al. Adult outcomes following amputation or lengthening for fibular deficiency. J Bone Joint Surg Am. 2009;91(4):797-804. [Link] [DOI:10.2106/JBJS.G.01297]
20. Merhi R, Kazarian SS. Validation of the Arabic translation of the multidimensional scale of perceived social support (Arabic-MSPSS) in a Lebanese community sample. Arab J Psychiatry. 2012;23(2):159-68. [Link] [DOI:10.1037/t89612-000]
21. Al-Eqabi QA, Niazy SM, Radhi MM. Amputation-related factors influencing activities of daily living among amputees. Iran J War Public Health. 2024;16(2):123-9. [Link]
22. Radhi MM, Al-Eqabi QA, Hindi NK. Rehabilitation problems of people with motor disabilities at Babylon center for rehabilitation of the disabled. Med J Babylon. 2023;20(4):838-43. [Link] [DOI:10.4103/MJBL.MJBL_674_23]
23. AL-Jubori RH, Yasir AA, Hindi NK. Quality of life among amputees: A mediating role of social support. Med J Babylon. 2023;20(2):315-21. [Link] [DOI:10.4103/MJBL.MJBL_330_22]
24. Radhi MM, Juma Elywy G, Al-Eqabi QAK. Burdens among wives of disabled people in the light of some social variables. Iran Rehabil J. 2023;21(3):473-84. [Link] [DOI:10.32598/irj.21.3.1765.3]
25. Kh AL-Jubori RH, Yasir AA, Hindi KK. Quality of life and its related factors among amputees in Babylon province, Iraq. Iran Rehabil J. 2023;21(2):273-82. [Link] [DOI:10.32598/irj.21.2.1765.2]
26. Eskridge SL, Watrous JR, McCabe CT, Clouser MC, Galarneau MR. The relationship between self-reported physical functioning, mental health, and quality of life in service members after combat-related lower extremity amputation. Disabil Rehabil. 2022;44(13):3189-95. [Link] [DOI:10.1080/09638288.2020.1863481]
27. Wadey R, Day M. A longitudinal examination of leisure time physical activity following amputation in England. Psychol Sport Exerc. 2018;37:251-61. [Link] [DOI:10.1016/j.psychsport.2017.11.005]
28. Pedras S, Vilhena E, Carvalho R, Pereira MG. Psychosocial adjustment to a lower limb amputation ten months after surgery. Rehabil Psychol. 2018;63(3):418-30. [Link] [DOI:10.1037/rep0000189]
29. Elywy GJ, Radhi MM, AlEqabi QA. Relationship between social support and self-hardiness among breast cancer women in Nasiriyah, Iraq. J Pak Med Assoc. 2023;73(9):S9-14. [Link] [DOI:10.47391/JPMA.IQ-02]
30. Emerson E, Fortune N, Llewellyn G, Stancliffe R. Loneliness, social support, social isolation and wellbeing among working age adults with and without disability: Cross-sectional study. Disabil Health J. 2021;14(1):100965. [Link] [DOI:10.1016/j.dhjo.2020.100965]
31. Malih Radhi M, Zair Balat K. Health literacy and its association with medication adherence in patients with hypertension: A mediating role of social support. Iran Rehabil J. 2024;22(1):117-28. [Link] [DOI:10.32598/irj.22.1.1989.1]
32. Kever A, Buyukturkoglu K, Riley CS, De Jager PL, Leavitt VM. Social support is linked to mental health, quality of life, and motor function in multiple sclerosis. J Neurol. 2021;268(5):1827-36. [Link] [DOI:10.1007/s00415-020-10330-7]
33. Rafnsson SB, Orrell M, D'Orsi E, Hogervorst E, Steptoe A. Loneliness, social integration, and incident dementia over 6 years: Prospective findings from the English longitudinal study of ageing. J Gerontol B Psychol Sci Soc Sci. 2020;75(1):114-24. [Link] [DOI:10.1093/geronb/gbx087]