Volume 16, Issue 2 (2024)
Iran J War Public Health 2024, 16(2): 131-142 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2024/04/13 | Accepted: 2024/06/16 | Published: 2024/07/21
Received: 2024/04/13 | Accepted: 2024/06/16 | Published: 2024/07/21
How to cite this article
Ghaffari F, Sharififar S, Parsania Z. Ethical Challenges in Nuclear/Radiation Accidents; A Systematic Review. Iran J War Public Health 2024; 16 (2) :131-142
URL: http://ijwph.ir/article-1-1450-en.html
URL: http://ijwph.ir/article-1-1450-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
1- Department of Health in Disasters and Emergencies, Faculty of Nursing, AJA University of Medical Sciences, Tehran, Iran
2- Department of Rehabilitation Management, Faculty of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran
2- Department of Rehabilitation Management, Faculty of Rehabilitation Sciences, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran
Full-Text (HTML) (1252 Views)
Introduction
Ethical issues have been a topic of debate for many years [1]. When planning and executing disaster management, ethical considerations should be taken into account in all stages of the process, including preparation, operation, triage and recovery phases [2]. Ethical discussions and solutions have varied throughout history depending on the time, place, and cultural traditions of the community [3]. The principles of respect for autonomy, non-maleficence, beneficence and justice have been developed by two American philosophers named Beauchamp and Childress [4]. Autonomy refers to an individual's ability to choose what is best for themselves based on their own ideals. Non-maleficence requires healthcare providers to do no harm to their patients, while beneficence aims to enhance the patient's well-being. Justice requires equal treatment for all individuals while also providing for their individual needs [5-7]. It is generally considered unethical to restrict people's freedom, but in some extreme situations, it may be necessary [8]. However, ethical concerns in disasters have received less attention. Disaster risk management and adherence to ethical standards are crucial in such circumstances where resources are scarce and catastrophic disasters cause significant destruction. Ethical concerns that arise during and after disasters include inadequate and unfair distribution of assistance funding, preservation of financial resources and privacy of the injured, and biases in post-accident treatment and triage. Failing to uphold professional ethics during a crisis can worsen the harm inflicted on the injured. Adherence to the four ethical standards is necessary to resolve ethical dilemmas in disasters. Lack of knowledge of a country's culture, language, and policies, absence of specific protocols for specific disasters, poor disaster triage, inadequate distribution of aid services, insufficient follow-up care after the crisis, and reluctance to accept international aid from various communities are some of the ethical issues that arise during catastrophes. Understanding the codes of ethics, principles of professional ethics, and the ethical dilemmas that arise during catastrophes can help managers make better decisions and aid rescue teams when faced with ethical dilemmas [9].
The use of ionizing radiation and radioactive materials has increased significantly with the rapid development of technology in today's world [10]. When individuals are exposed to ionizing radiation or contamination with radioactive materials, it is referred to as a radiation accident [11]. Nuclear catastrophes like those that occurred in Chernobyl and Fukushima have exposed many people to ionizing radiation [12]. While radiation activity is largely helpful, it can also expose others to radiation hazards. Therefore, it is important to consider how to balance risks and benefits, which is an ethical dilemma associated with radiation risk [13]. Accidental accidents and deliberate mishaps involving radiation are both possibilities [14].
Radiation pollution's impacts on people can be divided into two categories; Hereditary and individual effects, as well as early and late consequences. Individual effects lead to acute impacts of radioactive rays due to the radiation of a significant amount in a short period of time, and genetic effects modify the mutation rate of sex cell genes [15]. Accidents involving radiation and nuclear energy can involve both high- and low-level radiation [16].
Radiation and nuclear accidents are highly complex, instantaneous, dynamic, and unpredictable [17]. They differ from other technology risks in several ways. Firstly, there is no safe amount of radiation exposure, making radiation hazards similar to other technology hazards. Secondly, radiation exposure is not a sudden occurrence, and the health of people can be impacted by radiation buildup, which can take a long time to manifest in humans. Thirdly, radiation has a very long half-life and can persist in the environment for a long time, having a lasting impact on future generations. Fourthly, the threat from nuclear weapons can transcend national boundaries [18].
Regarding the effects of radiation exposure, there is a great deal of public and health concern. This concern is brought on not only by the worry of a repeat of the Chernobyl or Fukushima nuclear power plant accidents, but also by the deliberate use of nuclear weapons, radiation-scattering devices, or advanced nuclear devices by rogue nations and terrorist groups. Advanced nations are equipped to handle minor nuclear and radiation events, but they lack the resources and infrastructure required to handle significant nuclear and radiation disasters and catastrophes [19]. There are several ways that nuclear terrorism might manifest itself, such as by exploding a nuclear weapon or using a radioactive dispersion device (Dirty Bomb). A nuclear weapon is a weapon of mass destruction. Although it also produces significant pollution, the bomb is intended to kill humans. A terrorist weapon, a dirty bomb is not a weapon of mass devastation. In actuality, the majority of nuclear terrorism uses weapons of mass disruption rather than weapons of mass devastation [20].
There are many ethical concerns that arise with the management of nuclear accidents. Although efforts to reduce the effects of exposure to ionizing radiation after an accident are made, ethical considerations are often overlooked due to the direct and indirect consequences of these procedures [21]. The Fukushima-Daiichi accident was caused not only by inadequate technological solutions but also by a lack of understanding of social and ethical concerns, such as a lack of transparency and an insufficient safety culture [22]. One of the most important lessons learned from previous nuclear and radiation incidents is that the direct effects of radiation must be taken into account when assessing the acceptability of post-accident ethical management [23]. Factors such as consent, fairness, and accountability must be considered when making ethical evaluations of radiation hazards. Positive and negative ethical considerations must both be taken into account when making judgments about radiation protection. Some therapeutic strategies offer social and ethical benefits in addition to dose reduction [24].
Research question include: 1. What are the fundamental tenets of bioethics in nuclear and radiation events? 2. What are the ethical challenges in nuclear/radiation accidents? 3. What are the solutions to improve ethical issues in nuclear/radiation accidents?
According to the International Commission on Radiological Protection (ICRP), justification is considered a fundamental ethical value. In radiation protection, consequentialism suggests that the benefits or consequences of a protective measure should be the primary factor in determining whether it is beneficial or harmful. Hence, the aim of the current study was to analyze the ethical issues and suggest solutions to mitigate them in case of nuclear and radiation accidents.
Information and Methods
All five stages recommended by Arksey and O'Malley were used in this study: 1. the formulation of the research topic, 2. the selection of studies, 3. the choice of studies, 4. the collection and integration of data, and 5. the summary and reporting of Results [25].
In the first phase, the research question was established as follows, taking into consideration Arksey and O'Malley's advice to perform a targeted review based on the study's goal of ethical challenges in nuclear/radiation accidents.
Search strategy
The search components were: ‘nuclear/radiation accidents’, ‘ethic’ and ‘challenges’. Equivalent words were obtained for each phrase in the MeSH search engines. The words were completed or revised after the specialist’s consultation. In this study, we identified search phrases and keywords for data sources. The search terms included: Ethic, justice, moral, values, ethical challenges, nuclear disasters, nuclear/radiological incidents, nuclear/radiological accidents, nuclear/radiological events, bioethics, evacuation, triage, SHAMISEN, patients' rights, health worker rights, worker rights, rights of vulnerable groups, humanitarian actions, ethics fundamental, national laws, and international treaties. We used the databases from PubMed, Web of Science, and Scopus without any time restrictions to conduct this investigation. English-language articles that addressed ethical issues in nuclear and radiation accidents and methods to mitigate them met the inclusion criteria for this study. Articles that were not directly related to the subject and those for which we did not have access to the complete texts were excluded. The books were excluded and not examined for this investigation.
In order to reduce the risk of bias, the initial review process of the articles in the used databases was done independently by two of the authors of the article and was summarized by another author of the article and finally, the quality of the articles was evaluated based on the PRISMA statement (Figure 1).
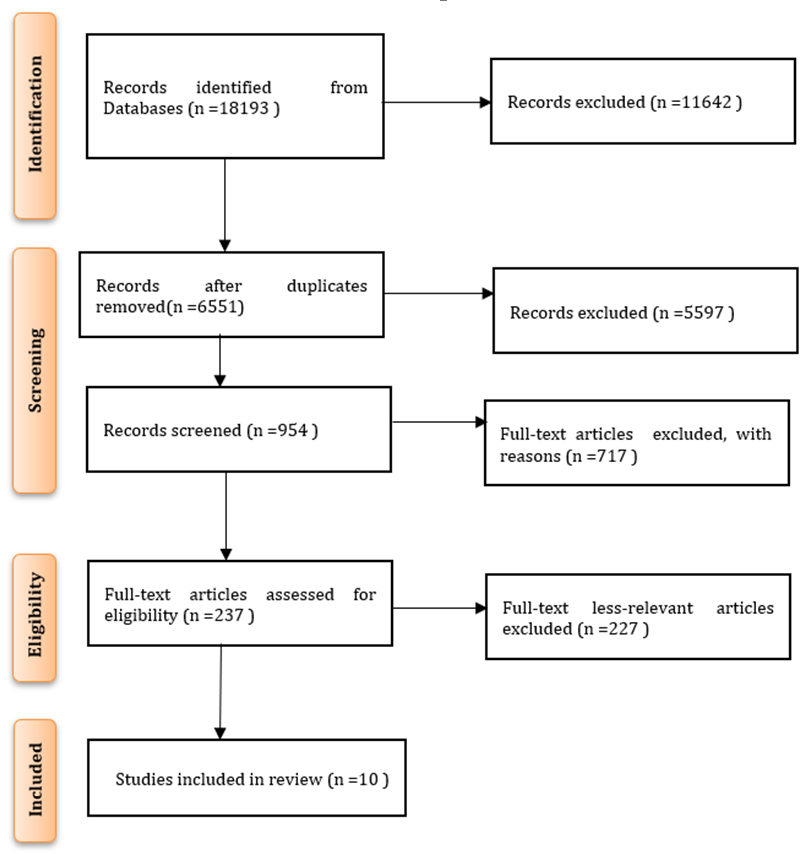
Figure 1. PRISMA diagram
Findings
The researchers looked at the article abstracts in accordance with the entry and exit criteria, separated the relevant items, and extracted the complete texts of those things (Table 1).
Table 1. Characteristics of the studies conducted regarding ethical challenges in nuclear/radiation accidents

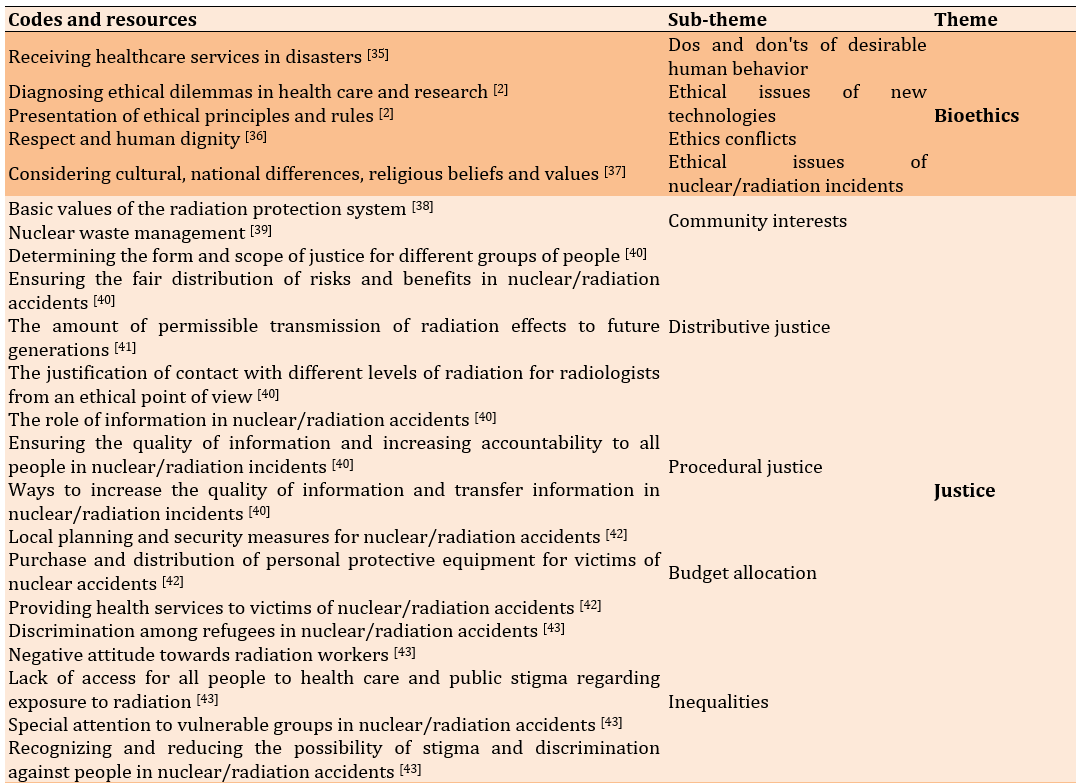
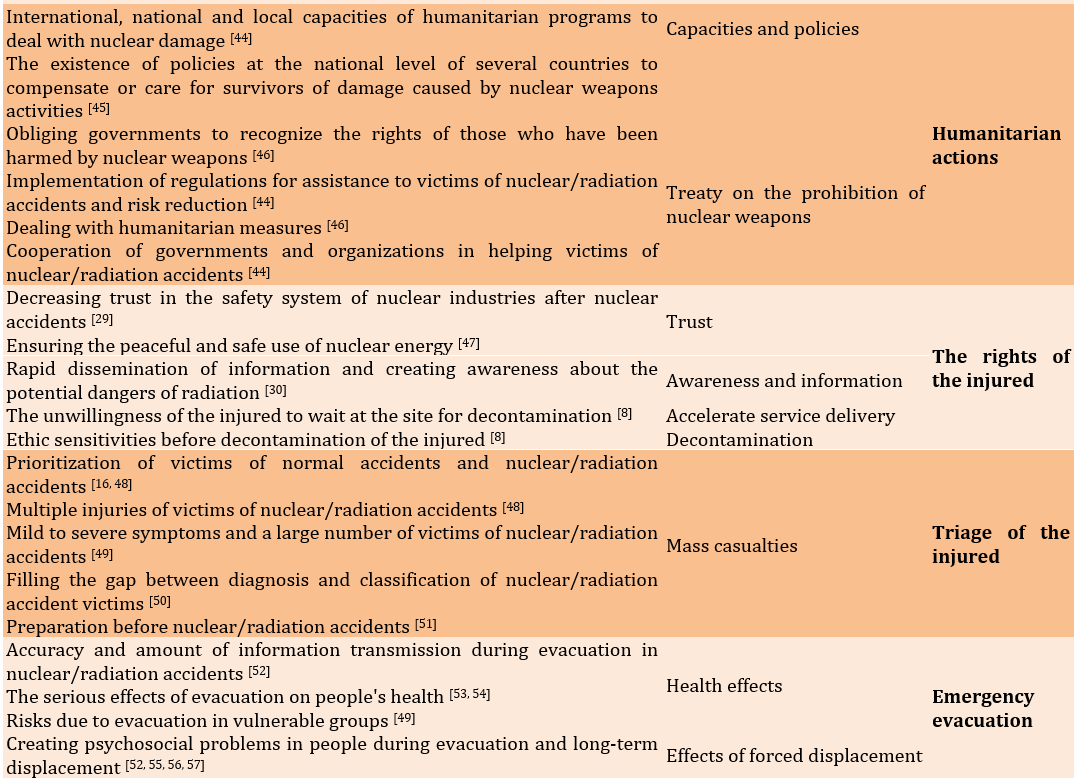
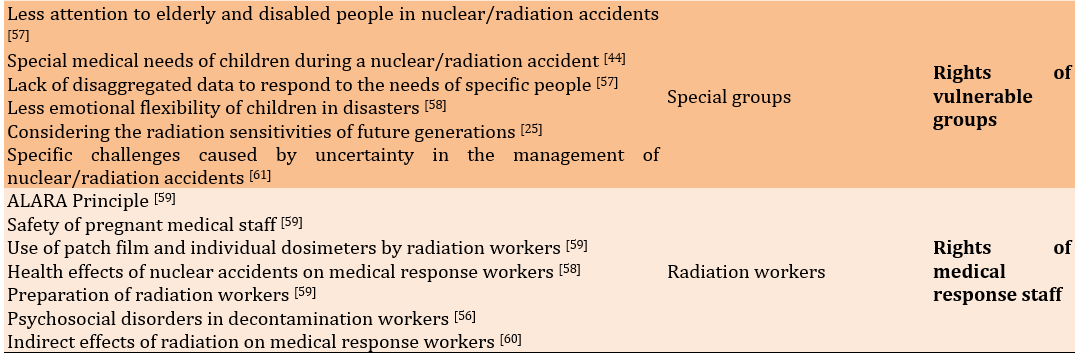
Thematic analysis
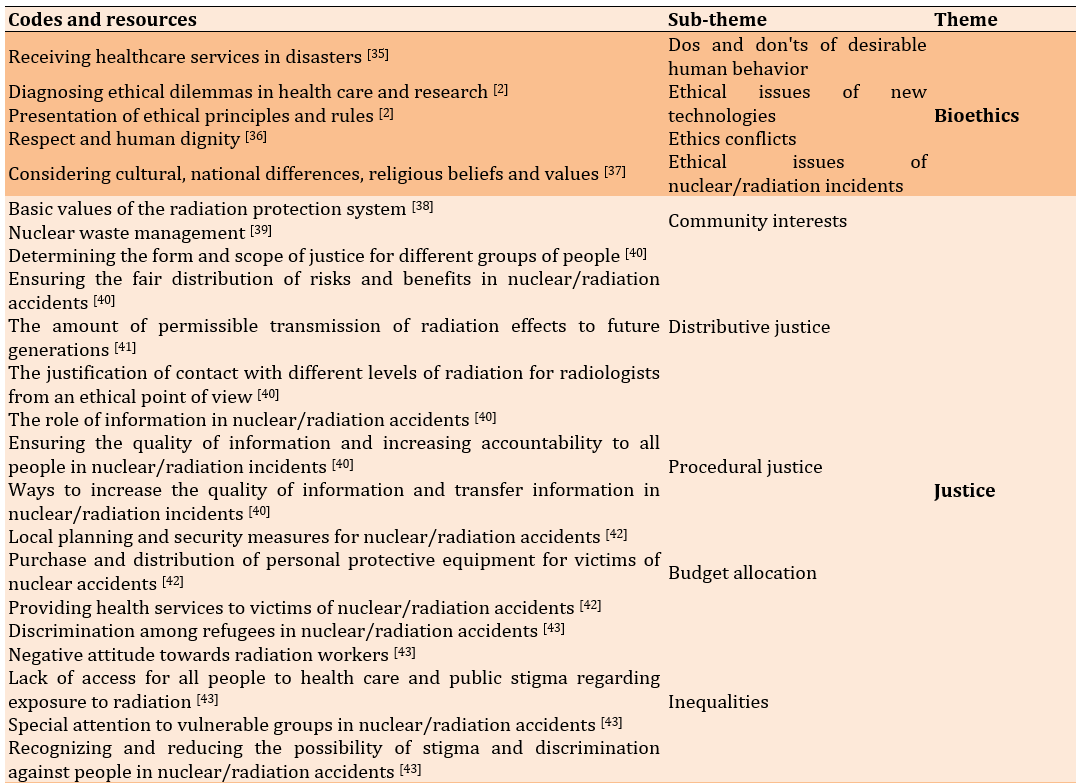
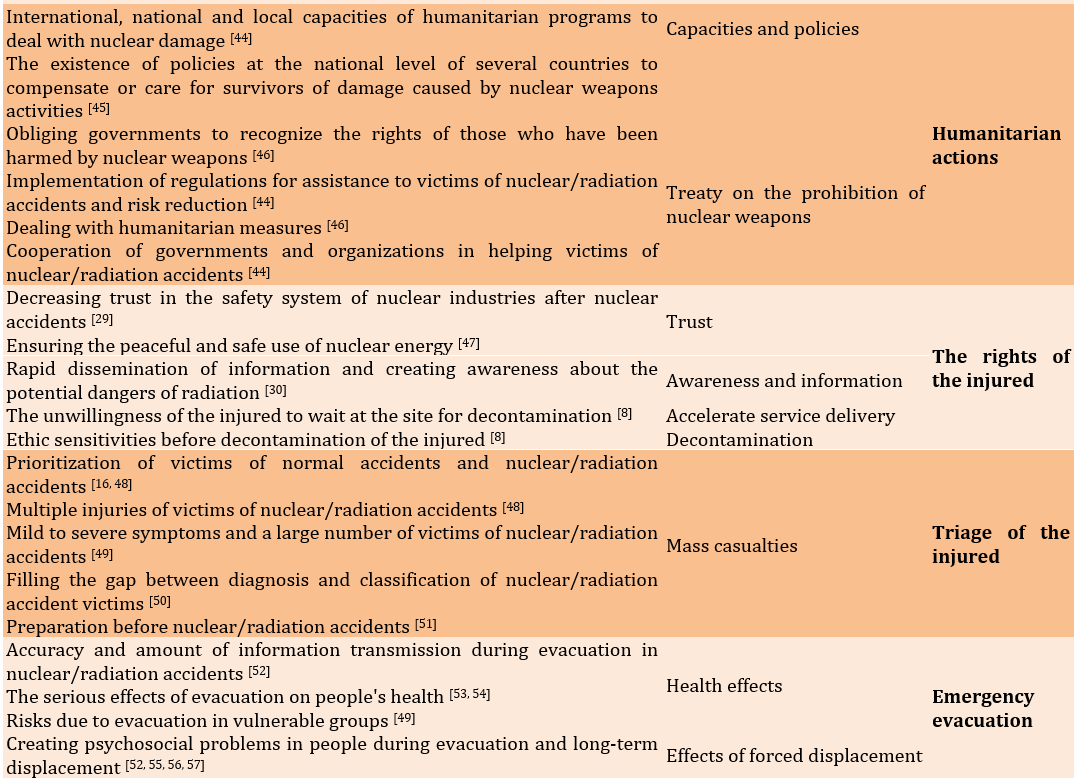
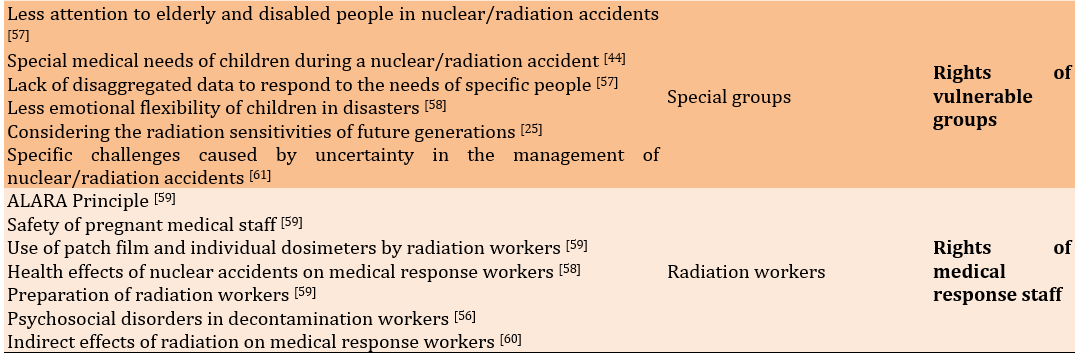
A summary of the articles and sources chosen for examination was presented as the review's last stage. Therefore, it was necessary to locate and review papers that dealt explicitly with ethical dilemmas in nuclear/radiation accidents. After reading the articles multiple times and analyzing them for repetition and relevance, the semantic units pertinent to the study topics were identified. Then, using open coding, subclasses, classes, and themes were created based on the ways in which the various codes varied and resembled one another. The review claimed that eight themes of bioethics, justice, humanitarian activities, rights of the injured, injured triage, emergency evacuation, rights of vulnerable groups, and rights of medical response professionals may be used to categorize ethical difficulties in nuclear/radiation accidents (Table 2).
Table 2. Themes and sub-themes of ethical challenges of nuclear/radiation incidents
1. Principles of bioethics
Bioethics aimed to address what appropriate human actions should be in various healthcare situations, taking into consideration the health status and involvement of each individual [35]. The field of bioethics originated from concerns about the ethical dilemmas arising from emerging technologies and the fair allocation of resources, as well as the lack of regulations over human subjects' research. To assist healthcare professionals and policymakers in resolving ethical quandaries in healthcare and biomedical research, bioethics established a set of ethical principles and guidelines [2]. It seemed that bioethics and its guiding principles direct human behavior towards ethical dilemmas and decisions regarding care and assistance based on respect and dignity for all individuals. The Universal Declaration of Bioethics and Human Rights, issued by UNESCO in 2009, provides the guidelines used in these circumstances, taking into account religious, cultural, and national beliefs, as well as various values, although it was not specifically designed to address ethical issues related to nuclear/radio incidents [37].
2. Justice in nuclear/radiation incidents
The need to respect and take into account everyone's interests was emphasized by the justice principle. Justice-related consideration was a factor in radiation concerns for about 40 years. One of the four fundamental principles that guided the radiation protection system is fairness, according to the most recent version of the ICRP [38]. While procedural justice is concerned with guaranteeing the accuracy of information and raising everyone's level of accountability, distributive justice focuses on defining the nature and parameters of justice for various groups of people. Ensuring that risks and rewards are allocated fairly is the basic objective of distributive justice. Why is radiologists' exposure to various levels of radiation ethically acceptable in regard to distributive justice? How to handle intergenerational and global distribution. Information has a more important function with respect to procedural fairness. How can the quality of information and its conveyance be improved? Does regional crisis management ensure information's veracity and transparency [40]? When we consider the extent or group to whom this distribution applies, particularly when the need to consider temporal distribution and issues of intergenerational fairness are present, they become more complex. How much radiation may we pass on to the next generation, and what justifies it ethically [41]? Allocating funds from the public budget for local planning and security measures, the purchase and distribution of personal protective equipment, and the provision of health services for those affected by nuclear and radiation accidents is a crucial issue of justice in preventing and dealing with the effects of such accidents [42]. Justice demands that those who make decisions work to make up for the disparities that might result from nuclear and radiation accidents. The pursuit of justice in nuclear/radiation accidents necessitates a unique awareness of and responsibility for children, women, the elderly, and other vulnerable populations, as well as an understanding of and commitment to minimizing the likelihood of stigma and prejudice [43]. Worldwide public concern exists over the disposal of garbage in slums or floating in the ocean due to the unresolved global issue of managing nuclear waste. The management of nuclear waste poses a threat to intergenerational justice as it places the burden of waste management on future generations while the current generation benefits significantly from nuclear energy supplies [39].
3. Principles of humanitarian actions in nuclear/radiation incidents
Humanitarian efforts to mitigate the effects of nuclear devastation are currently scattered globally and have not yet been acknowledged as a feasible collective action. However, there are several local, national, and international capacities that need to be improved [44]. At the national level, some countries have implemented programs to aid or compensate those who have been harmed by nuclear weapons activity. These programs are often achieved after lengthy struggles to gain recognition from civil society and social groups [45]. The treaty on the prohibition of nuclear weapons is not just a prohibition treaty; It also imposes extensive positive obligations on governments, including the obligation to address humanitarian concerns and to recognize the rights of those who have been or will be affected by the use and testing of nuclear weapons in the past and in the future [46]. Governments should leverage their experiences in implementing the victim relief, decontamination, and risk reduction provisions of other humanitarian nuclear disarmament treaties while fulfilling their commitments under the NPT [59].
4. Protecting the rights of nuclear victims according to national laws and international treaties
The Fukushima Daiichi power plant tragedy led to widespread mistrust of Japanese citizens and a significant decrease in public acceptance of nuclear power and confidence in the industry's safety systems. This prompted many nations to reevaluate their nuclear energy policies and plans [29]. The international community has long prioritized the safe and peaceful use of nuclear energy, which is supported by a wide range of national and international regulations [47]. The United Nations Charter of Human Rights consists of three primary human rights accords: The Universal Declaration of Human Rights (UDHR), the International Convention on Civil and Political Rights (ICCPR), and the International Convention on Economic, Social and Cultural Rights (ICESCR). Utilizing human rights in post-disaster management aims to prevent harm to affected populations and uphold human dignity during evacuation and transitional periods. During emergency evacuations and the subsequent response phase, challenges arose from balancing government decisions with public concerns, as well as difficulties in implementing bureaucratic procedures and addressing public opposition to nuclear power. Regional and international human rights charters generally protect the right to knowledge and information, which is crucial for building public confidence during sensitive situations like the Fukushima disaster [30]. While the Japanese people demonstrated restraint and tolerance during the emergency evacuation, quicker recognition of the threat could have better prepared them to respond to the disaster. The legal framework for nuclear energy is defined by a collection of enforceable laws, agreements, and standards on a global scale, which continues to evolve over time. Many formerly non-binding standards have become obligations, serving as the foundation for national laws in numerous countries, as they are seen to be in their best interests to uphold international standards [47].
Walking is a challenge for victims of radiation and nuclear weapons. They are undoubtedly feeling a lot of anxiety. Some people could try to eject the area forcibly rather than wait for decontamination. Responders are responsible for reducing the substantial potential hazard that these people offer to others by contaminating them. Decontamination is undoubtedly in the best interest of the general population, however there are ethical considerations. Before disinfection, clothing should be taken off, then it should be replaced with a fresh set. Such practices might be viewed as a serious breach of a person's right to their body [8].
5. Triage of victims of nuclear/radiation accidents
Disparities between requirements and resources are a hallmark of disasters. It may be important to triage the injured based on preset priorities when there are large casualties since it is impossible to give medical care for every victim. Triage is linked to a lot of ethical dilemmas [62]. Even though triage is a crucial issue in all catastrophes because the injured in nuclear/radiation accidents have sustained radiation exposure or radioactive contamination in addition to the normal wounds like burns and trauma, both physical injuries and radioactive contamination should be taken into consideration for the injured's triage [46]. Instead of potentially deadly levels, victims of nuclear terrorism or radiation accidents may get doses with no discernible clinical signs. The casualties might range in number from a few to thousands [49]. Numerous victims of nuclear or radiation accidents may need immediate medical attention to avoid long-term health effects. Triage is therefore an important goal at all stages of emergency preparation, both military and civilian. Bridging the gap between diagnosis and classification of the injured, including those who have not been exposed to radiation (or are simply concerned), those who have been exposed to radiation but do not require special medical treatment, and those who have been exposed to radiation but require dosimetry and begin special treatments, is the main obstacle that needs to be overcome [50]. Isolating victims with considerable biological radiation doses of concern would be the top priority for a medical facility dealing with a major radiation disaster. Identifying which of the found victims needs immediate care will be the second priority. Finally, the topic of selecting and putting into practice the proper therapy will be covered [16]. Prevention is always preferable than treatment in nuclear and radiation accidents. However, the lack of radiation biodosimetry and the ensuing inability to triage owing to the lack of radiation medicine training by emergency response workers may seriously hinder the medical response in the event of a large-scale nuclear crisis or act of terrorism. This lack of readiness is made worse by the public's and the media's pervasive fear of radiation. In reality, a prospective terrorist's attraction to radioactive materials is mostly a result of both inadequate preparation and widespread public anxiety [51].
6. Emergency evacuation in nuclear/radiation accidents
In the event of a nuclear or radiation disaster, it is important to take protective measures such as finding shelter and leaving the area immediately if possible [63]. However, during the Three Mile Island incident, the information provided to local residents was not sufficient. As a result, some people chose to leave on their own, causing heavy traffic and inconvenience [64]. Even though there are technical requirements for evacuation and relocation, research has revealed that these actions might have negative health implications that should be taken into account in future disaster planning and response. In the Fukushima disaster, for instance, the evacuation resulted in the terrible deaths of people in hospitals and medical facilities both during the journey and just after they arrived at their destination [53]. The hazards of evacuation exceeded any possible long-term advantages since there was inadequate previous preparation, transportation, assistance, and facilities for housing and caring for the sick and old in nuclear/radiation incidents. While long-term migration lessens radiation exposure, it can lead to psychological suffering due to home loss, disruption of social and professional connections, issues adjusting to a new environment, fear of radiation-related illnesses, despair, and suicide [52]. The 27,000 evacuees from the Fukushima catastrophe were found to have a significant prevalence of obesity, diabetes, high blood pressure, and abnormalities of lipid metabolism. Additionally, the percentage of evacuees with depression symptoms rose to 14.6% in 2011. The incident's most severe psychological repercussion was suicide in particular (almost five times the proportion of the general population in Japan) [54]. The suicide rate reduced very much after the earthquake and tsunami in two of the three Tohoku prefectures, Miyagi and Iwate, where the consequences of the earthquake and tsunami were quite severe. However, it remained unchanged in Fukushima and then steadily rose [55]. Increased levels of environmental radioactivity continue to induce social and psychological difficulties in those who had to leave their homes and in those who lived in polluted regions after nuclear accidents [56]. Long-term relocation was linked to several health issues, including lifestyle-related illnesses and worse public health following radiation/nuclear events [65].
7. Protecting the rights of vulnerable groups in nuclear/radiation accidents
Disasters have a disproportionate impact on different groups of people. Vulnerable populations, such as women, children, the elderly, and those with disabilities, require special protection during nuclear and radiation disasters. International human rights standards are the basis for safeguarding these communities. Unfortunately, the elderly and disabled are often overlooked in these situations. One of the biggest challenges in protecting vulnerable populations during crises is the lack of specific data that addresses the unique needs and limitations of diverse individuals [57]. Children are at least as likely as adults to experience radiation-related issues after a nuclear or radiation incident, which highlights the importance of addressing their specific medical needs [44].
It is important to consider the sensitivity of neonates, fetuses, and future generations to radiation exposure. Children are more vulnerable to psychological harm during catastrophes as they are less emotionally adaptable [25]. They tend to breathe more quickly, which leads to inhalation of radioactive dust and deposition in their lungs. This makes them more susceptible to radiation, which increases the likelihood of cancer [58].
Nuclear/radiation incident management poses unique problems due to the unpredictability of incident management. It is essential to strike a balance while evaluating measures. Overestimating the potential social and health repercussions of protective measures such as evacuation while underestimating the potential doses and health effects of radiation for vulnerable groups like women, the elderly, and children may not result in affected populations making better decisions [26].
8. Protecting the rights of medical response workers in nuclear/radiation accidents
A specialist medical response is necessary in a number of serious nuclear or radiation situations. Due to their familiarity with radiation and its biological effects, doctors and other health professionals may be selected for incident management, casualty treatment, and specialized labor in a significant radiation event. Medical workers may face a sizable number of possibly contaminated casualties in any kind of nuclear or radiation catastrophe. Any radiation protection program's guiding principle is that radiation workers must keep their own and everyone else's exposure to radiation to an acceptable minimum while executing their responsibilities. ALARA uses four straightforward concepts to minimize any source's potential for danger, including radioactive substances and ionizing radiation. Time, distance, protection, and the eradication or control of pollution are the four guiding concepts. If staff are not careful and take the proper measures, they might unintentionally expose themselves and others to contamination or take massive amounts of it themselves over time. It should be possible to exclude pregnant workers from providing direct care to numerous patients who have been exposed to radiation. Individual dosimeters that have been calibrated should be attached to garments so that contamination may be removed quickly. Video badges should be used to periodically check on radiation employees. The first guideline in managing a nuclear or radiation disaster effectively is for personnel to be ready, and preparedness also necessitates understanding various emergency case scenarios and carrying out suitable drills prior to the catastrophe [59]. The radiation implications of nuclear accidents undoubtedly hurt health of some groups, particularly the pre-hospital emergency personnel in Chernobyl who experienced acute radiation sickness and thyroid cancer as a result of the catastrophe [58]. Workers in the decontamination industry experience PTSD, depression, suicidal thoughts, and anxiety. Many medical workers who experience serious complications in nuclear or radiation accidents do not do so as a direct result of the biological effects of radiation; Rather, they are brought on by the presence of radioactive contamination and as a result of emergency and corrective actions taken, or by uncertainty regarding the amount of radiation and its effects on patients and the elderly [60].
SHAMISEN (improving medical and health supervision in nuclear accidents)
A comprehensive analysis was carried out under the umbrella of SHAMISEN to examine the suggestions and lessons learned from significant nuclear accidents in the past. The analysis focuses on improving the preparedness, response, long-term monitoring, and living conditions of communities affected by past or present nuclear/radiation incidents. The primary areas of emphasis in this analysis are dose assessment, evacuation decision-making, and long-term health monitoring programs. SHAMISEN aims to provide recommendations for medical and health surveillance of communities affected by radiation catastrophes based on the experiences gained from major incidents such as Chernobyl, Fukushima, and others. The recommendations are primarily focused on three key areas:
1. Implementing therapeutic measures to monitor the clinical course of affected individuals in the aftermath of a nuclear disaster.
2. Improving the living conditions of the affected population by attending to their needs and incorporating them into monitoring programs, thereby reducing unnecessary anxiety.
3. Maintaining regular dialogue with the affected population.
By addressing these areas, SHAMISEN hopes to enhance the recovery process and minimize the long-term effects of radiation exposure on impacted communities [26]. Every component of the incident-technical, psychological, social, economic, and ethical is taken into account as part of SHAMISEN's holistic approach to health. Experience indicates that many European countries' reaction plans have not taken rights and ethics seriously enough, and the current proposals have mostly concentrated on technology and paid little attention to psychological, legal, and ethical concerns [44]. The WHO's effort of health guidelines to monitor the health of people exposed to radiation is represented by SHAMISEN, which takes into account the social, psychological, and economic repercussions of radiation accidents as well as the health effects of radiation. The SHAMISEN initiative places a strong emphasis on recognizing the ethical difficulties. Recognizing the ethical issues that might develop in incident management and health monitoring, as well as the complications that can result from the numerous uncertainties surrounding event outcomes, is necessary in response to nuclear and radiological incidents. The first suggestion made by SHAMISEN is that incident management should pay particular attention to the fundamental ethical rule of doing better than damage. Declaring this as the first advice helps to underline that decision-makers and everyone involved in disasters, must be prepared to recognize and handle these problems. Nuclear/radiation incident management, like any other catastrophe management, involves ethical challenges. The following SHAMISEN suggestion places a focus on upholding the affected population's autonomy and dignity throughout health surveillance. There are ways to make sure that managing nuclear accidents may provide impacted communities more respect and dignity. These remedies include things that individuals may do to take back control of their lives and raise awareness among the public to assist the affected population in making their own decisions [26].
Discussion
Improving strategies of ethical issues in radiological/nuclear accidents
Ethical challenges in nuclear and radiation accidents encompass a range of complex issues that revolve around balancing the benefits and risks associated with nuclear energy. These challenges include the need to prioritize safety and security in nuclear power programs to prevent catastrophic accidents that can have far-reaching impacts on global health and the environment. Stakeholders, including governments, international organizations, and industry players, must navigate ethical dilemmas related to maximizing benefits while minimizing harm, ensuring compliance with safety regulations, disclosing accurate information to the public, and providing support to affected populations after accidents. Additionally, ethical considerations extend to the management of radioactive waste, the potential for nuclear accidents and theft, and the long-term implications of such disasters on society, the environment, and international relations. Addressing these ethical challenges requires a comprehensive approach that integrates ethical values and principles to guide decision-making and actions in the nuclear energy sector.
Current international radiation-protection guidelines provided by the ICRP, the IAEA, and the ILO, discussed ethical considerations regarding five important topics in radiation protection and ethics. They present each of these five topics in relation to different ethical perspectives: 1) Fairness vs. Effectiveness, 2) Well-being vs. Financial Concerns, 3) Personal Liberties vs. Community Advantages, 4) Legal Procedures vs. Required Compromises, and 5) Agreement of Stakeholders vs. Managerial Choices [66].
The international community has failed to adequately address the potential risks of nuclear power, particularly in terms of protecting human rights in the aftermath of major nuclear disasters like Chernobyl and Fukushima. It is essential for governments to prioritize human rights when making decisions concerning nuclear energy and for the global community to increase safety standards and ethical values in this sector. Simply increasing inspection measures is insufficient; There needs to be a system of social monitoring and evaluation involving non-profit organizations and NGOs to safeguard human rights and basic freedoms in the nuclear power industry both during normal operations and in times of crisis [67].
The potential ethical challenges of victims in nuclear/radiation accidents have become increasingly important in light of the current state of fossil energies like oil, as well as the trend of countries using nuclear energy and political tensions between countries possessing nuclear technology. The occurrence of future nuclear accidents, whether actual or hypothetical, will require an immediate response from society to meet both immediate and long-term human needs [42]. The belief that there will be no more tragedies like Chernobyl or Fukushima is illogical. In this context, the international community should promote safety regulations, ethical principles, and human values while also being aware of the inherent risks of nuclear technologies. While strict inspection programs by relevant institutions and organizations are necessary, there should also be a monitoring and evaluation mechanism in partnership with non-governmental organizations to ensure that human rights and ethics are upheld in the nuclear energy sector, both under normal circumstances and during emergencies.
Radiation monitoring programs have increased recently, but ethical issues and difficulties should be considered. While health care and monitoring can be beneficial, surveillance can also cause unnecessary anxiety. However, if individuals who do not require specific medical and therapy assistance are not included in the monitoring program, they may experience psychological issues. There is currently no systematic plan in place to deal with health monitoring in nuclear/radiation incidents, which calls for learning from the past. Preparation is key to successful nuclear/radiation incident management, including awareness of various emergency scenarios and knowing how to react in each case before it happens. This is why elected officials, organizations, and responsible individuals must take essential steps to cope with and manage any potential nuclear emergency. Addressing ethical concerns in nuclear/radiological catastrophes can ensure that presumptions, potential conflicts, and justifications for final decisions are as open as possible, enhancing the population's resilience and sense of empowerment. To avoid causing more harm than good and respect basic ethical principles such as independence and equality, it is necessary to pay attention to the social, ethical, and psychological effects of ongoing actions and involve local people in the design, implementation, and follow-up of radiation risk management. In cases of radionuclide contamination, sufferers should be screened for contamination as part of the first triage. Radiation triage is essential to treat patients who have acute radiation sickness and require specialized medical care.
The book "Social and Ethical Aspects of Radiation Risk Management" covers a broad range of issues related to the use of ionizing radiation, including nuclear bomb testing, nuclear safety management, stakeholder engagement, decontamination, radiation environmental hazards, justice in nuclear/radiation accidents, radiation worker health and safety, dosimetry standards, and ethics. It provides a comprehensive solution to the major social and ethical problems associated with ionizing radiation. Emergency medical personnel should be taught the general bioethics of nuclear and radiation events. While it may not be realistic to expect emergency responders from other countries to be able to respond to nuclear or radiological incidents in time, advanced training in bioethics related to such accidents will undoubtedly help ensure their readiness to handle casualties. Organizations should have access to up-to-date information on nuclear power plants in their respective areas, and emergency evacuation procedures should be established in these areas as a precautionary measure to avoid the long-term effects of radiation. Residents must be given detailed instructions on how to take appropriate radiation protection measures, including providing temporary shelter, in the event of a significant radionuclide emission. In densely populated areas, simultaneous evacuation of many people can cause chaos and excessive traffic. Therefore, areas should be divided into blocks to allow for a planned evacuation. Additionally, adequate training should be provided to inhabitants of these locations, and they should be well-informed of the radiation risks. When weighing the benefits of evacuation and relocation against the hazards in nuclear/radiation incidents, psychological and ethical impacts should also be taken into account. One ethical practice that may help populations affected by nuclear and radiological harm become more resilient is stakeholder involvement in radiation monitoring programs.
Despite being seen as a renewable energy source that aids in reducing greenhouse gas emissions, nuclear energy produces extremely hazardous radioactive waste and causes permanent harm to the environment and the health of the public.
Our study's limitations include the lack of uniform methodology among similar studies. Additionally, the inability to access the full text of some articles may have resulted in an incomplete and restricted review.
Conclusion
Eight themes of bioethics, justice, humanitarian activities, rights of the injured, injured triage, emergency evacuation, rights of vulnerable groups, and rights of medical response professionals are used to categorize ethical difficulties in nuclear/radiation accidents
Acknowledgments: Thanks are given to all the researchers whose articles were reviewed in this study.
Ethical Permission: Nothing declared by the authors.
Conflicts of Interests: The authors declare that there are no conflicts of interest regarding the publication of this manuscript.
Authors’ Contribution: Ghaffari F (First Author), Introduction Writer/Main Researcher/Discussion Writer (40%); Sharififar S (Second Author), Methodologist (40%); Parsania Z (Third Author), Statistical Analyst/Assistant Researcher (20%)
Funding/Support: There was no financial support.
Ethical issues have been a topic of debate for many years [1]. When planning and executing disaster management, ethical considerations should be taken into account in all stages of the process, including preparation, operation, triage and recovery phases [2]. Ethical discussions and solutions have varied throughout history depending on the time, place, and cultural traditions of the community [3]. The principles of respect for autonomy, non-maleficence, beneficence and justice have been developed by two American philosophers named Beauchamp and Childress [4]. Autonomy refers to an individual's ability to choose what is best for themselves based on their own ideals. Non-maleficence requires healthcare providers to do no harm to their patients, while beneficence aims to enhance the patient's well-being. Justice requires equal treatment for all individuals while also providing for their individual needs [5-7]. It is generally considered unethical to restrict people's freedom, but in some extreme situations, it may be necessary [8]. However, ethical concerns in disasters have received less attention. Disaster risk management and adherence to ethical standards are crucial in such circumstances where resources are scarce and catastrophic disasters cause significant destruction. Ethical concerns that arise during and after disasters include inadequate and unfair distribution of assistance funding, preservation of financial resources and privacy of the injured, and biases in post-accident treatment and triage. Failing to uphold professional ethics during a crisis can worsen the harm inflicted on the injured. Adherence to the four ethical standards is necessary to resolve ethical dilemmas in disasters. Lack of knowledge of a country's culture, language, and policies, absence of specific protocols for specific disasters, poor disaster triage, inadequate distribution of aid services, insufficient follow-up care after the crisis, and reluctance to accept international aid from various communities are some of the ethical issues that arise during catastrophes. Understanding the codes of ethics, principles of professional ethics, and the ethical dilemmas that arise during catastrophes can help managers make better decisions and aid rescue teams when faced with ethical dilemmas [9].
The use of ionizing radiation and radioactive materials has increased significantly with the rapid development of technology in today's world [10]. When individuals are exposed to ionizing radiation or contamination with radioactive materials, it is referred to as a radiation accident [11]. Nuclear catastrophes like those that occurred in Chernobyl and Fukushima have exposed many people to ionizing radiation [12]. While radiation activity is largely helpful, it can also expose others to radiation hazards. Therefore, it is important to consider how to balance risks and benefits, which is an ethical dilemma associated with radiation risk [13]. Accidental accidents and deliberate mishaps involving radiation are both possibilities [14].
Radiation pollution's impacts on people can be divided into two categories; Hereditary and individual effects, as well as early and late consequences. Individual effects lead to acute impacts of radioactive rays due to the radiation of a significant amount in a short period of time, and genetic effects modify the mutation rate of sex cell genes [15]. Accidents involving radiation and nuclear energy can involve both high- and low-level radiation [16].
Radiation and nuclear accidents are highly complex, instantaneous, dynamic, and unpredictable [17]. They differ from other technology risks in several ways. Firstly, there is no safe amount of radiation exposure, making radiation hazards similar to other technology hazards. Secondly, radiation exposure is not a sudden occurrence, and the health of people can be impacted by radiation buildup, which can take a long time to manifest in humans. Thirdly, radiation has a very long half-life and can persist in the environment for a long time, having a lasting impact on future generations. Fourthly, the threat from nuclear weapons can transcend national boundaries [18].
Regarding the effects of radiation exposure, there is a great deal of public and health concern. This concern is brought on not only by the worry of a repeat of the Chernobyl or Fukushima nuclear power plant accidents, but also by the deliberate use of nuclear weapons, radiation-scattering devices, or advanced nuclear devices by rogue nations and terrorist groups. Advanced nations are equipped to handle minor nuclear and radiation events, but they lack the resources and infrastructure required to handle significant nuclear and radiation disasters and catastrophes [19]. There are several ways that nuclear terrorism might manifest itself, such as by exploding a nuclear weapon or using a radioactive dispersion device (Dirty Bomb). A nuclear weapon is a weapon of mass destruction. Although it also produces significant pollution, the bomb is intended to kill humans. A terrorist weapon, a dirty bomb is not a weapon of mass devastation. In actuality, the majority of nuclear terrorism uses weapons of mass disruption rather than weapons of mass devastation [20].
There are many ethical concerns that arise with the management of nuclear accidents. Although efforts to reduce the effects of exposure to ionizing radiation after an accident are made, ethical considerations are often overlooked due to the direct and indirect consequences of these procedures [21]. The Fukushima-Daiichi accident was caused not only by inadequate technological solutions but also by a lack of understanding of social and ethical concerns, such as a lack of transparency and an insufficient safety culture [22]. One of the most important lessons learned from previous nuclear and radiation incidents is that the direct effects of radiation must be taken into account when assessing the acceptability of post-accident ethical management [23]. Factors such as consent, fairness, and accountability must be considered when making ethical evaluations of radiation hazards. Positive and negative ethical considerations must both be taken into account when making judgments about radiation protection. Some therapeutic strategies offer social and ethical benefits in addition to dose reduction [24].
Research question include: 1. What are the fundamental tenets of bioethics in nuclear and radiation events? 2. What are the ethical challenges in nuclear/radiation accidents? 3. What are the solutions to improve ethical issues in nuclear/radiation accidents?
According to the International Commission on Radiological Protection (ICRP), justification is considered a fundamental ethical value. In radiation protection, consequentialism suggests that the benefits or consequences of a protective measure should be the primary factor in determining whether it is beneficial or harmful. Hence, the aim of the current study was to analyze the ethical issues and suggest solutions to mitigate them in case of nuclear and radiation accidents.
Information and Methods
All five stages recommended by Arksey and O'Malley were used in this study: 1. the formulation of the research topic, 2. the selection of studies, 3. the choice of studies, 4. the collection and integration of data, and 5. the summary and reporting of Results [25].
In the first phase, the research question was established as follows, taking into consideration Arksey and O'Malley's advice to perform a targeted review based on the study's goal of ethical challenges in nuclear/radiation accidents.
Search strategy
The search components were: ‘nuclear/radiation accidents’, ‘ethic’ and ‘challenges’. Equivalent words were obtained for each phrase in the MeSH search engines. The words were completed or revised after the specialist’s consultation. In this study, we identified search phrases and keywords for data sources. The search terms included: Ethic, justice, moral, values, ethical challenges, nuclear disasters, nuclear/radiological incidents, nuclear/radiological accidents, nuclear/radiological events, bioethics, evacuation, triage, SHAMISEN, patients' rights, health worker rights, worker rights, rights of vulnerable groups, humanitarian actions, ethics fundamental, national laws, and international treaties. We used the databases from PubMed, Web of Science, and Scopus without any time restrictions to conduct this investigation. English-language articles that addressed ethical issues in nuclear and radiation accidents and methods to mitigate them met the inclusion criteria for this study. Articles that were not directly related to the subject and those for which we did not have access to the complete texts were excluded. The books were excluded and not examined for this investigation.
In order to reduce the risk of bias, the initial review process of the articles in the used databases was done independently by two of the authors of the article and was summarized by another author of the article and finally, the quality of the articles was evaluated based on the PRISMA statement (Figure 1).
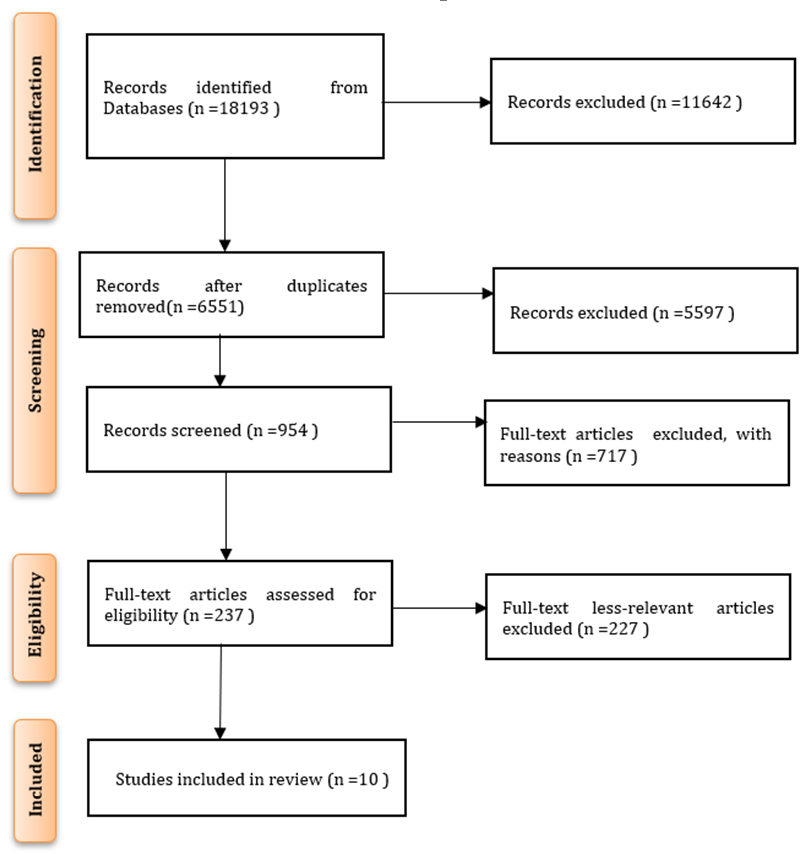
Figure 1. PRISMA diagram
Findings
The researchers looked at the article abstracts in accordance with the entry and exit criteria, separated the relevant items, and extracted the complete texts of those things (Table 1).
Table 1. Characteristics of the studies conducted regarding ethical challenges in nuclear/radiation accidents

Thematic analysis
A summary of the articles and sources chosen for examination was presented as the review's last stage. Therefore, it was necessary to locate and review papers that dealt explicitly with ethical dilemmas in nuclear/radiation accidents. After reading the articles multiple times and analyzing them for repetition and relevance, the semantic units pertinent to the study topics were identified. Then, using open coding, subclasses, classes, and themes were created based on the ways in which the various codes varied and resembled one another. The review claimed that eight themes of bioethics, justice, humanitarian activities, rights of the injured, injured triage, emergency evacuation, rights of vulnerable groups, and rights of medical response professionals may be used to categorize ethical difficulties in nuclear/radiation accidents (Table 2).
Table 2. Themes and sub-themes of ethical challenges of nuclear/radiation incidents
1. Principles of bioethics
Bioethics aimed to address what appropriate human actions should be in various healthcare situations, taking into consideration the health status and involvement of each individual [35]. The field of bioethics originated from concerns about the ethical dilemmas arising from emerging technologies and the fair allocation of resources, as well as the lack of regulations over human subjects' research. To assist healthcare professionals and policymakers in resolving ethical quandaries in healthcare and biomedical research, bioethics established a set of ethical principles and guidelines [2]. It seemed that bioethics and its guiding principles direct human behavior towards ethical dilemmas and decisions regarding care and assistance based on respect and dignity for all individuals. The Universal Declaration of Bioethics and Human Rights, issued by UNESCO in 2009, provides the guidelines used in these circumstances, taking into account religious, cultural, and national beliefs, as well as various values, although it was not specifically designed to address ethical issues related to nuclear/radio incidents [37].
2. Justice in nuclear/radiation incidents
The need to respect and take into account everyone's interests was emphasized by the justice principle. Justice-related consideration was a factor in radiation concerns for about 40 years. One of the four fundamental principles that guided the radiation protection system is fairness, according to the most recent version of the ICRP [38]. While procedural justice is concerned with guaranteeing the accuracy of information and raising everyone's level of accountability, distributive justice focuses on defining the nature and parameters of justice for various groups of people. Ensuring that risks and rewards are allocated fairly is the basic objective of distributive justice. Why is radiologists' exposure to various levels of radiation ethically acceptable in regard to distributive justice? How to handle intergenerational and global distribution. Information has a more important function with respect to procedural fairness. How can the quality of information and its conveyance be improved? Does regional crisis management ensure information's veracity and transparency [40]? When we consider the extent or group to whom this distribution applies, particularly when the need to consider temporal distribution and issues of intergenerational fairness are present, they become more complex. How much radiation may we pass on to the next generation, and what justifies it ethically [41]? Allocating funds from the public budget for local planning and security measures, the purchase and distribution of personal protective equipment, and the provision of health services for those affected by nuclear and radiation accidents is a crucial issue of justice in preventing and dealing with the effects of such accidents [42]. Justice demands that those who make decisions work to make up for the disparities that might result from nuclear and radiation accidents. The pursuit of justice in nuclear/radiation accidents necessitates a unique awareness of and responsibility for children, women, the elderly, and other vulnerable populations, as well as an understanding of and commitment to minimizing the likelihood of stigma and prejudice [43]. Worldwide public concern exists over the disposal of garbage in slums or floating in the ocean due to the unresolved global issue of managing nuclear waste. The management of nuclear waste poses a threat to intergenerational justice as it places the burden of waste management on future generations while the current generation benefits significantly from nuclear energy supplies [39].
3. Principles of humanitarian actions in nuclear/radiation incidents
Humanitarian efforts to mitigate the effects of nuclear devastation are currently scattered globally and have not yet been acknowledged as a feasible collective action. However, there are several local, national, and international capacities that need to be improved [44]. At the national level, some countries have implemented programs to aid or compensate those who have been harmed by nuclear weapons activity. These programs are often achieved after lengthy struggles to gain recognition from civil society and social groups [45]. The treaty on the prohibition of nuclear weapons is not just a prohibition treaty; It also imposes extensive positive obligations on governments, including the obligation to address humanitarian concerns and to recognize the rights of those who have been or will be affected by the use and testing of nuclear weapons in the past and in the future [46]. Governments should leverage their experiences in implementing the victim relief, decontamination, and risk reduction provisions of other humanitarian nuclear disarmament treaties while fulfilling their commitments under the NPT [59].
4. Protecting the rights of nuclear victims according to national laws and international treaties
The Fukushima Daiichi power plant tragedy led to widespread mistrust of Japanese citizens and a significant decrease in public acceptance of nuclear power and confidence in the industry's safety systems. This prompted many nations to reevaluate their nuclear energy policies and plans [29]. The international community has long prioritized the safe and peaceful use of nuclear energy, which is supported by a wide range of national and international regulations [47]. The United Nations Charter of Human Rights consists of three primary human rights accords: The Universal Declaration of Human Rights (UDHR), the International Convention on Civil and Political Rights (ICCPR), and the International Convention on Economic, Social and Cultural Rights (ICESCR). Utilizing human rights in post-disaster management aims to prevent harm to affected populations and uphold human dignity during evacuation and transitional periods. During emergency evacuations and the subsequent response phase, challenges arose from balancing government decisions with public concerns, as well as difficulties in implementing bureaucratic procedures and addressing public opposition to nuclear power. Regional and international human rights charters generally protect the right to knowledge and information, which is crucial for building public confidence during sensitive situations like the Fukushima disaster [30]. While the Japanese people demonstrated restraint and tolerance during the emergency evacuation, quicker recognition of the threat could have better prepared them to respond to the disaster. The legal framework for nuclear energy is defined by a collection of enforceable laws, agreements, and standards on a global scale, which continues to evolve over time. Many formerly non-binding standards have become obligations, serving as the foundation for national laws in numerous countries, as they are seen to be in their best interests to uphold international standards [47].
Walking is a challenge for victims of radiation and nuclear weapons. They are undoubtedly feeling a lot of anxiety. Some people could try to eject the area forcibly rather than wait for decontamination. Responders are responsible for reducing the substantial potential hazard that these people offer to others by contaminating them. Decontamination is undoubtedly in the best interest of the general population, however there are ethical considerations. Before disinfection, clothing should be taken off, then it should be replaced with a fresh set. Such practices might be viewed as a serious breach of a person's right to their body [8].
5. Triage of victims of nuclear/radiation accidents
Disparities between requirements and resources are a hallmark of disasters. It may be important to triage the injured based on preset priorities when there are large casualties since it is impossible to give medical care for every victim. Triage is linked to a lot of ethical dilemmas [62]. Even though triage is a crucial issue in all catastrophes because the injured in nuclear/radiation accidents have sustained radiation exposure or radioactive contamination in addition to the normal wounds like burns and trauma, both physical injuries and radioactive contamination should be taken into consideration for the injured's triage [46]. Instead of potentially deadly levels, victims of nuclear terrorism or radiation accidents may get doses with no discernible clinical signs. The casualties might range in number from a few to thousands [49]. Numerous victims of nuclear or radiation accidents may need immediate medical attention to avoid long-term health effects. Triage is therefore an important goal at all stages of emergency preparation, both military and civilian. Bridging the gap between diagnosis and classification of the injured, including those who have not been exposed to radiation (or are simply concerned), those who have been exposed to radiation but do not require special medical treatment, and those who have been exposed to radiation but require dosimetry and begin special treatments, is the main obstacle that needs to be overcome [50]. Isolating victims with considerable biological radiation doses of concern would be the top priority for a medical facility dealing with a major radiation disaster. Identifying which of the found victims needs immediate care will be the second priority. Finally, the topic of selecting and putting into practice the proper therapy will be covered [16]. Prevention is always preferable than treatment in nuclear and radiation accidents. However, the lack of radiation biodosimetry and the ensuing inability to triage owing to the lack of radiation medicine training by emergency response workers may seriously hinder the medical response in the event of a large-scale nuclear crisis or act of terrorism. This lack of readiness is made worse by the public's and the media's pervasive fear of radiation. In reality, a prospective terrorist's attraction to radioactive materials is mostly a result of both inadequate preparation and widespread public anxiety [51].
6. Emergency evacuation in nuclear/radiation accidents
In the event of a nuclear or radiation disaster, it is important to take protective measures such as finding shelter and leaving the area immediately if possible [63]. However, during the Three Mile Island incident, the information provided to local residents was not sufficient. As a result, some people chose to leave on their own, causing heavy traffic and inconvenience [64]. Even though there are technical requirements for evacuation and relocation, research has revealed that these actions might have negative health implications that should be taken into account in future disaster planning and response. In the Fukushima disaster, for instance, the evacuation resulted in the terrible deaths of people in hospitals and medical facilities both during the journey and just after they arrived at their destination [53]. The hazards of evacuation exceeded any possible long-term advantages since there was inadequate previous preparation, transportation, assistance, and facilities for housing and caring for the sick and old in nuclear/radiation incidents. While long-term migration lessens radiation exposure, it can lead to psychological suffering due to home loss, disruption of social and professional connections, issues adjusting to a new environment, fear of radiation-related illnesses, despair, and suicide [52]. The 27,000 evacuees from the Fukushima catastrophe were found to have a significant prevalence of obesity, diabetes, high blood pressure, and abnormalities of lipid metabolism. Additionally, the percentage of evacuees with depression symptoms rose to 14.6% in 2011. The incident's most severe psychological repercussion was suicide in particular (almost five times the proportion of the general population in Japan) [54]. The suicide rate reduced very much after the earthquake and tsunami in two of the three Tohoku prefectures, Miyagi and Iwate, where the consequences of the earthquake and tsunami were quite severe. However, it remained unchanged in Fukushima and then steadily rose [55]. Increased levels of environmental radioactivity continue to induce social and psychological difficulties in those who had to leave their homes and in those who lived in polluted regions after nuclear accidents [56]. Long-term relocation was linked to several health issues, including lifestyle-related illnesses and worse public health following radiation/nuclear events [65].
7. Protecting the rights of vulnerable groups in nuclear/radiation accidents
Disasters have a disproportionate impact on different groups of people. Vulnerable populations, such as women, children, the elderly, and those with disabilities, require special protection during nuclear and radiation disasters. International human rights standards are the basis for safeguarding these communities. Unfortunately, the elderly and disabled are often overlooked in these situations. One of the biggest challenges in protecting vulnerable populations during crises is the lack of specific data that addresses the unique needs and limitations of diverse individuals [57]. Children are at least as likely as adults to experience radiation-related issues after a nuclear or radiation incident, which highlights the importance of addressing their specific medical needs [44].
It is important to consider the sensitivity of neonates, fetuses, and future generations to radiation exposure. Children are more vulnerable to psychological harm during catastrophes as they are less emotionally adaptable [25]. They tend to breathe more quickly, which leads to inhalation of radioactive dust and deposition in their lungs. This makes them more susceptible to radiation, which increases the likelihood of cancer [58].
Nuclear/radiation incident management poses unique problems due to the unpredictability of incident management. It is essential to strike a balance while evaluating measures. Overestimating the potential social and health repercussions of protective measures such as evacuation while underestimating the potential doses and health effects of radiation for vulnerable groups like women, the elderly, and children may not result in affected populations making better decisions [26].
8. Protecting the rights of medical response workers in nuclear/radiation accidents
A specialist medical response is necessary in a number of serious nuclear or radiation situations. Due to their familiarity with radiation and its biological effects, doctors and other health professionals may be selected for incident management, casualty treatment, and specialized labor in a significant radiation event. Medical workers may face a sizable number of possibly contaminated casualties in any kind of nuclear or radiation catastrophe. Any radiation protection program's guiding principle is that radiation workers must keep their own and everyone else's exposure to radiation to an acceptable minimum while executing their responsibilities. ALARA uses four straightforward concepts to minimize any source's potential for danger, including radioactive substances and ionizing radiation. Time, distance, protection, and the eradication or control of pollution are the four guiding concepts. If staff are not careful and take the proper measures, they might unintentionally expose themselves and others to contamination or take massive amounts of it themselves over time. It should be possible to exclude pregnant workers from providing direct care to numerous patients who have been exposed to radiation. Individual dosimeters that have been calibrated should be attached to garments so that contamination may be removed quickly. Video badges should be used to periodically check on radiation employees. The first guideline in managing a nuclear or radiation disaster effectively is for personnel to be ready, and preparedness also necessitates understanding various emergency case scenarios and carrying out suitable drills prior to the catastrophe [59]. The radiation implications of nuclear accidents undoubtedly hurt health of some groups, particularly the pre-hospital emergency personnel in Chernobyl who experienced acute radiation sickness and thyroid cancer as a result of the catastrophe [58]. Workers in the decontamination industry experience PTSD, depression, suicidal thoughts, and anxiety. Many medical workers who experience serious complications in nuclear or radiation accidents do not do so as a direct result of the biological effects of radiation; Rather, they are brought on by the presence of radioactive contamination and as a result of emergency and corrective actions taken, or by uncertainty regarding the amount of radiation and its effects on patients and the elderly [60].
SHAMISEN (improving medical and health supervision in nuclear accidents)
A comprehensive analysis was carried out under the umbrella of SHAMISEN to examine the suggestions and lessons learned from significant nuclear accidents in the past. The analysis focuses on improving the preparedness, response, long-term monitoring, and living conditions of communities affected by past or present nuclear/radiation incidents. The primary areas of emphasis in this analysis are dose assessment, evacuation decision-making, and long-term health monitoring programs. SHAMISEN aims to provide recommendations for medical and health surveillance of communities affected by radiation catastrophes based on the experiences gained from major incidents such as Chernobyl, Fukushima, and others. The recommendations are primarily focused on three key areas:
1. Implementing therapeutic measures to monitor the clinical course of affected individuals in the aftermath of a nuclear disaster.
2. Improving the living conditions of the affected population by attending to their needs and incorporating them into monitoring programs, thereby reducing unnecessary anxiety.
3. Maintaining regular dialogue with the affected population.
By addressing these areas, SHAMISEN hopes to enhance the recovery process and minimize the long-term effects of radiation exposure on impacted communities [26]. Every component of the incident-technical, psychological, social, economic, and ethical is taken into account as part of SHAMISEN's holistic approach to health. Experience indicates that many European countries' reaction plans have not taken rights and ethics seriously enough, and the current proposals have mostly concentrated on technology and paid little attention to psychological, legal, and ethical concerns [44]. The WHO's effort of health guidelines to monitor the health of people exposed to radiation is represented by SHAMISEN, which takes into account the social, psychological, and economic repercussions of radiation accidents as well as the health effects of radiation. The SHAMISEN initiative places a strong emphasis on recognizing the ethical difficulties. Recognizing the ethical issues that might develop in incident management and health monitoring, as well as the complications that can result from the numerous uncertainties surrounding event outcomes, is necessary in response to nuclear and radiological incidents. The first suggestion made by SHAMISEN is that incident management should pay particular attention to the fundamental ethical rule of doing better than damage. Declaring this as the first advice helps to underline that decision-makers and everyone involved in disasters, must be prepared to recognize and handle these problems. Nuclear/radiation incident management, like any other catastrophe management, involves ethical challenges. The following SHAMISEN suggestion places a focus on upholding the affected population's autonomy and dignity throughout health surveillance. There are ways to make sure that managing nuclear accidents may provide impacted communities more respect and dignity. These remedies include things that individuals may do to take back control of their lives and raise awareness among the public to assist the affected population in making their own decisions [26].
Discussion
Improving strategies of ethical issues in radiological/nuclear accidents
Ethical challenges in nuclear and radiation accidents encompass a range of complex issues that revolve around balancing the benefits and risks associated with nuclear energy. These challenges include the need to prioritize safety and security in nuclear power programs to prevent catastrophic accidents that can have far-reaching impacts on global health and the environment. Stakeholders, including governments, international organizations, and industry players, must navigate ethical dilemmas related to maximizing benefits while minimizing harm, ensuring compliance with safety regulations, disclosing accurate information to the public, and providing support to affected populations after accidents. Additionally, ethical considerations extend to the management of radioactive waste, the potential for nuclear accidents and theft, and the long-term implications of such disasters on society, the environment, and international relations. Addressing these ethical challenges requires a comprehensive approach that integrates ethical values and principles to guide decision-making and actions in the nuclear energy sector.
Current international radiation-protection guidelines provided by the ICRP, the IAEA, and the ILO, discussed ethical considerations regarding five important topics in radiation protection and ethics. They present each of these five topics in relation to different ethical perspectives: 1) Fairness vs. Effectiveness, 2) Well-being vs. Financial Concerns, 3) Personal Liberties vs. Community Advantages, 4) Legal Procedures vs. Required Compromises, and 5) Agreement of Stakeholders vs. Managerial Choices [66].
The international community has failed to adequately address the potential risks of nuclear power, particularly in terms of protecting human rights in the aftermath of major nuclear disasters like Chernobyl and Fukushima. It is essential for governments to prioritize human rights when making decisions concerning nuclear energy and for the global community to increase safety standards and ethical values in this sector. Simply increasing inspection measures is insufficient; There needs to be a system of social monitoring and evaluation involving non-profit organizations and NGOs to safeguard human rights and basic freedoms in the nuclear power industry both during normal operations and in times of crisis [67].
The potential ethical challenges of victims in nuclear/radiation accidents have become increasingly important in light of the current state of fossil energies like oil, as well as the trend of countries using nuclear energy and political tensions between countries possessing nuclear technology. The occurrence of future nuclear accidents, whether actual or hypothetical, will require an immediate response from society to meet both immediate and long-term human needs [42]. The belief that there will be no more tragedies like Chernobyl or Fukushima is illogical. In this context, the international community should promote safety regulations, ethical principles, and human values while also being aware of the inherent risks of nuclear technologies. While strict inspection programs by relevant institutions and organizations are necessary, there should also be a monitoring and evaluation mechanism in partnership with non-governmental organizations to ensure that human rights and ethics are upheld in the nuclear energy sector, both under normal circumstances and during emergencies.
Radiation monitoring programs have increased recently, but ethical issues and difficulties should be considered. While health care and monitoring can be beneficial, surveillance can also cause unnecessary anxiety. However, if individuals who do not require specific medical and therapy assistance are not included in the monitoring program, they may experience psychological issues. There is currently no systematic plan in place to deal with health monitoring in nuclear/radiation incidents, which calls for learning from the past. Preparation is key to successful nuclear/radiation incident management, including awareness of various emergency scenarios and knowing how to react in each case before it happens. This is why elected officials, organizations, and responsible individuals must take essential steps to cope with and manage any potential nuclear emergency. Addressing ethical concerns in nuclear/radiological catastrophes can ensure that presumptions, potential conflicts, and justifications for final decisions are as open as possible, enhancing the population's resilience and sense of empowerment. To avoid causing more harm than good and respect basic ethical principles such as independence and equality, it is necessary to pay attention to the social, ethical, and psychological effects of ongoing actions and involve local people in the design, implementation, and follow-up of radiation risk management. In cases of radionuclide contamination, sufferers should be screened for contamination as part of the first triage. Radiation triage is essential to treat patients who have acute radiation sickness and require specialized medical care.
The book "Social and Ethical Aspects of Radiation Risk Management" covers a broad range of issues related to the use of ionizing radiation, including nuclear bomb testing, nuclear safety management, stakeholder engagement, decontamination, radiation environmental hazards, justice in nuclear/radiation accidents, radiation worker health and safety, dosimetry standards, and ethics. It provides a comprehensive solution to the major social and ethical problems associated with ionizing radiation. Emergency medical personnel should be taught the general bioethics of nuclear and radiation events. While it may not be realistic to expect emergency responders from other countries to be able to respond to nuclear or radiological incidents in time, advanced training in bioethics related to such accidents will undoubtedly help ensure their readiness to handle casualties. Organizations should have access to up-to-date information on nuclear power plants in their respective areas, and emergency evacuation procedures should be established in these areas as a precautionary measure to avoid the long-term effects of radiation. Residents must be given detailed instructions on how to take appropriate radiation protection measures, including providing temporary shelter, in the event of a significant radionuclide emission. In densely populated areas, simultaneous evacuation of many people can cause chaos and excessive traffic. Therefore, areas should be divided into blocks to allow for a planned evacuation. Additionally, adequate training should be provided to inhabitants of these locations, and they should be well-informed of the radiation risks. When weighing the benefits of evacuation and relocation against the hazards in nuclear/radiation incidents, psychological and ethical impacts should also be taken into account. One ethical practice that may help populations affected by nuclear and radiological harm become more resilient is stakeholder involvement in radiation monitoring programs.
Despite being seen as a renewable energy source that aids in reducing greenhouse gas emissions, nuclear energy produces extremely hazardous radioactive waste and causes permanent harm to the environment and the health of the public.
Our study's limitations include the lack of uniform methodology among similar studies. Additionally, the inability to access the full text of some articles may have resulted in an incomplete and restricted review.
Conclusion
Eight themes of bioethics, justice, humanitarian activities, rights of the injured, injured triage, emergency evacuation, rights of vulnerable groups, and rights of medical response professionals are used to categorize ethical difficulties in nuclear/radiation accidents
Acknowledgments: Thanks are given to all the researchers whose articles were reviewed in this study.
Ethical Permission: Nothing declared by the authors.
Conflicts of Interests: The authors declare that there are no conflicts of interest regarding the publication of this manuscript.
Authors’ Contribution: Ghaffari F (First Author), Introduction Writer/Main Researcher/Discussion Writer (40%); Sharififar S (Second Author), Methodologist (40%); Parsania Z (Third Author), Statistical Analyst/Assistant Researcher (20%)
Funding/Support: There was no financial support.
Keywords:
References
1. Geale SK. The ethics of disaster management. Disaster Prev Manag. 2012;21(4):445-62. [Link] [DOI:10.1108/09653561211256152]
2. Kass NE. An ethics framework for public health. Am J Public Health. 2001;91(11):1776-82. [Link] [DOI:10.2105/AJPH.91.11.1776]
3. Souza LFD, Misko MD, Silva L, Poles K, Santos MRD, Bousso RS. Dignified death for children: Perceptions of nurses from an oncology unit. Revista da Escola de Enfermagem da USP. 2013;47(1):30-7. [Portuguese] [Link] [DOI:10.1590/S0080-62342013000100004]
4. Celedón C. Suffering and death in a terminal patient. Revista de Otorrinolaringología y Cirugía de Cabeza y Cuello. 2012;72(3):261-6. [Spanish] [Link] [DOI:10.4067/S0718-48162012000300008]
5. Morita A, Taebi B, Roeser S, editors. The ethics of nuclear energy: Risk, justice and democracy in the post-Fukushima era. Cambridge: Cambridge University Press; 2015. [Link]
6. Doorn N. Resilience indicators: Opportunities for including distributive justice concerns in disaster management. J Risk Res. 2017;20(6):711-31. [Link] [DOI:10.1080/13669877.2015.1100662]
7. Osaki T. Supreme court rules hibakusha overseas are entitled to full medical expenses [Internet]. Tokyo: The Japan Times; 2015 [cited 2024, 21 May]. Available from: https://www.japantimes.co.jp/news/2015/09/08/national/crime-legal/supreme-court-rules-hibakusha-overseas-entitled-full-medical-expenses/ [Link]
8. Schmid SD. Nuclear emergency response: Atomic priests or an international SWAT team?. In: Nuclear disaster at Fukushima Daiichi: Social, political and environmental issues. New York: Routledge; 2013. p. 222-41. [Link]
9. Ten Have H, Jean MS, editors. The UNESCO universal declaration on bioethics and human rights: Background, principles and application. Paris: UNESCO; 2009. [Link]
10. Kollek D. Canadian emergency department preparedness for a nuclear, biological or chemical event. CJEM. 2003;5(1):18-26. [Link] [DOI:10.1017/S148180350000806X]
11. Baniyaghoobi F, Aliyari S, Sharififar S, Pishgooie A. Radiation accidents and how to deal with it. MSC. 2014;1(1):43-51. [Persian] [Link] [DOI:10.18869/acadpub.mcs.1.1.43]
12. Bromet EJ. Emotional consequences of nuclear power plant disasters. Health Phys. 2014;106(2):206-10. [Link] [DOI:10.1097/HP.0000000000000012]
13. Jenkins K, McCauley D, Heffron R, Stephan H, Rehner R. Energy justice: A conceptual review. Energy Res Soc Sci. 2016;11:174-82. [Link] [DOI:10.1016/j.erss.2015.10.004]
14. Rastgu AR. Triage (plan for organizing the sufferers and the injured in accidents and crises). Tehran: PAYAME AMIR Publications, 2008. [Persian] [Link]
15. Neves NMBC, De Siqueira JE. Bioethics in current medical ethics code. Revista Bioética. 2010;18(2):439-50. [Portuguese] [Link]
16. Ohba T, Ishikawa T, Nagai H, Tokonami S, Hasegawa A, Suzuki G. Reconstruction of residents' thyroid equivalent doses from internal radionuclides after the Fukushima Daiichi nuclear power station accident. Sci Rep. 2020;10(1):6262. [Link] [DOI:10.1038/s41598-020-62931-x]
17. Tanigawa K, Hosoi Y, Hirohashi N, Iwasaki Y, Kamiya K. Loss of life after evacuation: Lessons learned from the Fukushima accident. Lancet. 2012;379(9819):889-91. [Link] [DOI:10.1016/S0140-6736(12)60384-5]
18. Taebi B. Justice and good governance in nuclear disasters. In: Ethics and law for chemical, biological, radiological, nuclear & explosive crises. Cham: Springer; 2019. p. 65-74. [Link] [DOI:10.1007/978-3-030-11977-5_6]
19. Gale RP. Medical and policy considerations for nuclear and radiation accidents, incidents and terrorism. Curr Opin Hematol. 2017;24(6):496-501. [Link] [DOI:10.1097/MOH.0000000000000380]
20. Beauchamp TL, Childress JF. Principles of biomedical ethics. Oxford: Oxford University Press; 2001. [Link]
21. World Medical Association. World medical association declaration of Helsinki. Ethical principles for medical research involving human subjects. Bull World Health Organ. 2001;79(4):373-4. [Link] [DOI:10.4414/fms.2001.04031]
22. Taebi B, Mayer M. By accident or by design? Pushing global governance of nuclear safety. Prog Nucl Energy. 2017;99:19-25. [Link] [DOI:10.1016/j.pnucene.2017.04.014]
23. Oughton D, Liutsko L, Midorikawa S, Pirard P, Schneider T, Tomkiv Y. An ethical dimension to accident management and health surveillance. Environ Int. 2021;153:106537. [Link] [DOI:10.1016/j.envint.2021.106537]
24. Oughton D. Ethical values in radiological protection. Radiat Prot Dosim. 1996;68(3-4):203-8. [Link] [DOI:10.1093/oxfordjournals.rpd.a031865]
25. Arksey H, O'Malley L. Scoping studies: Towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19-32. [Link] [DOI:10.1080/1364557032000119616]
26. Ohba T, Liutsko L, Schneider T, Barquinero JF, Crouaïl P, Fattibene P, et al. The SHAMISEN project: Challenging historical recommendations for preparedness, response and surveillance of health and well-being in case of nuclear accidents: Lessons learnt from Chernobyl and Fukushima. Environ Int. 2021;146:106200. [Link] [DOI:10.1016/j.envint.2020.106200]
27. Ohba T, Tanigawa K, Liutsko L. Evacuation after a nuclear accident: Critical reviews of past nuclear accidents and proposal for future planning. Environ Int. 2021;148:106379. [Link] [DOI:10.1016/j.envint.2021.106379]
28. Ahn J, Carson C, Jensen M, Juraku K, Nagasaki S, Tanaka S. Reflections on the Fukushima Daiichi Nuclear Accident: Toward social-scientific literacy and engineering resilience. London: Springer Nature. 2015;Unknown pages. [Link] [DOI:10.1007/978-3-319-12090-4]
29. Khan KJ. Post-disaster policy decision making and the prospects of human rights-The case of Fukushima Daiichi Nuclear Power Plant accident. Sociol Anthropol. 2018;6(1):116-34. [Link] [DOI:10.13189/sa.2018.060111]
30. Wolbarst AB, Wiley Jr AL, Nemhauser JB, Christensen DM, Hendee WR. Medical response to a major radiologic emergency: A primer for medical and public health practitioners. Radiology. 2010;254(1):660-77. [Link] [DOI:10.1148/radiol.09090330]
31. Xiang H, Zhu Y. The ethics issues of nuclear energy: Hard lessons learned from Chernobyl and Fukushima. J Health Ethics. 2011;7(2). [Link] [DOI:10.18785/ojhe.0702.06]
32. Rebera AP, Rafalowski C. On the spot ethical decision-making in CBRN (chemical, biological, radiological or nuclear event) response. Science and engineering ethics. 2014;20(1):735-52. [Link] [DOI:10.1007/s11948-014-9520-5]
33. Labidi S, Mahjoubi H, Essafi F, Salah RB. Natural radioactivity levels in mineral, therapeutic and spring waters in Tunisia. Radiation Physics and Chemistry. 2010;79(12):202-1196. [Link] [DOI:10.1016/j.radphyschem.2010.07.011]
34. Bréchignac F, Oughton D, Mays C, Barnthouse L, Beasley JC, Bonisoli-Alquati A, et al. Addressing ecological effects of radiation on populations and ecosystems to improve protection of the environment against radiation: Agreed statements from a Consensus Symposium. Journal of Environmental Radioactivity. 2016;158:21-9. [Link] [DOI:10.1016/j.jenvrad.2016.03.021]
35. Sandu A. The principles of bioethics and their use in ethical decision-making. Logos Universality Ment Educ Nov Sect Soc Sci. 2020;9(1):139-54. [Link] [DOI:10.18662/lumenss/9.1/39]
36. Ahn J, Carson C, Jensen M, Juraku K, Nagasaki S, Tanaka S. Reflections on the Fukushima Daiichi nuclear accident: Toward social-scientific literacy and engineering resilience. Cham: Springer; 2015. [Link] [DOI:10.1007/978-3-319-12090-4]
37. Bolton M. Humanitarian and environmental action to address nuclear harm. International Disarmament Institute. New York: Pace University; 2017. [Link]
38. Tomkiv Y, Perko T, Sala R, Zeleznik N, Maitre M, Schneider T, et al. Societal uncertainties recognised in recent nuclear and radiological emergencies. Radioprotection. 2020;55(HS1):S151-5. [Link] [DOI:10.1051/radiopro/2020025]
39. Krüetli P, Törnblom K, Helmer W, Stauffacher M. Distributive versus procedural justice in nuclear waste repository siting. In: The ethics of nuclear energy, risk, justice and democracy in post-Fukushima Era. Cambridge: Cambridge University Press; 2015. p. 119-40. [Link] [DOI:10.1017/CBO9781107294905.007]
40. Barber A. Hedonism and the experience machine. Philos Pap. 2011;40(2):257-78. [Link] [DOI:10.1080/05568641.2011.591850]
41. Rebera AP, Rafalowski C. On the spot ethical decision-making in CBRN (chemical, biological, radiological or nuclear event) response: Approaches to on the spot ethical decision-making for first responders to large-scale chemical incidents. Sci Eng Ethics. 2014;20(3):735-52. [Link] [DOI:10.1007/s11948-014-9520-5]
42. Labidi S, Mahjoubi H, Essafi F, Salah RB. Natural radioactivity levels in mineral, therapeutic and spring waters in Tunisia. Radiat Phys Chem. 2010;79(12):1196-202. [Link] [DOI:10.1016/j.radphyschem.2010.07.011]
43. Bréchignac F, Oughton D, Mays C, Barnthouse L, Beasley JC, Bonisoli-Alquati A, et al. Addressing ecological effects of radiation on populations and ecosystems to improve protection of the environment against radiation: Agreed statements from a Consensus Symposium. J Environ Radioact. 2016;158-159:21-9. [Link] [DOI:10.1016/j.jenvrad.2016.03.021]
44. Fernandes MA, Evangelista CB, Platel ICdS, Agra G, Lopes MdS, Rodrigues FdA. The perception by nurses of the significance of palliative care in patients with terminal cancer. Ciência & Saúde Coletiva. 2013;18(9):2589-96. [Portuguese] [Link] [DOI:10.1590/S1413-81232013000900013]
45. WHO. Guidance for managing ethical issues in infectious disease outbreaks. Geneva: World Health Organization; 2016. [Link]
46. Kryshev II, Kryshev AI, Sazykina TG. Dynamics of radiation exposure to marine biota in the area of the Fukushima NPP in March-May 2011. J Environ Radioact. 2012;114:157-61. [Link] [DOI:10.1016/j.jenvrad.2012.04.015]
47. O'Mathúna DP, De Miguel Beriain I. Ethics and law for chemical, biological, radiological, nuclear & explosive disaster. Cham: Springer; 2019. [Link] [DOI:10.1007/978-3-030-11977-5]
48. Saad ERD, Lima AP, Rodrigues C, Amorim F, Yasuda F, Santos GA, et al. Bioethics applied to pharmaceutical research and innovation. Revista de Pesquisa e Inovação Farmacêutica. 2009;1(1):53-62. [Portuguese] [Link]
49. WMA. World medical association international code of medical ethics. Ferney-Voltaire: World Medical Association; 2023. [Link]
50. Maeda M, Oe M. Mental health consequences and social issues after the Fukushima disaster. Asia Pac J Public Health. 2017;29(Suppl 2):36S-46S. [Link] [DOI:10.1177/1010539516689695]
51. Dorr H, Abend M, Blakely WF, Bolduc DL, Boozer D, Costeira T, et al. Using clinical signs and symptoms for medical management of radiation casualties-2015 NATO exercise. Radiat Res. 2017;187(3):273-86. [Link] [DOI:10.1667/RR14619.1]
52. Clarke RH, Valentin J. The history of ICRP and the evolution of its policies: Invited by the commission in October 2008. Ann ICRP. 2009;39(1):75-110. [Link] [DOI:10.1016/j.icrp.2009.07.009]
53. Ohto H, Maeda M, Yabe H, Yasumura S, Bromet EE. Suicide rates in the aftermath of the 2011 earthquake in Japan. Lancet. 2015;385(9979):1727. [Link] [DOI:10.1016/S0140-6736(15)60890-X]
54. Smith JS, Fisher JH. Three mile island: The silent disaster. JAMA. 1981;245(16):1656-9. [Link] [DOI:10.1001/jama.1981.03310410034023]
55. Elbaradei M, Nwogugu E, Rames J. International law and nuclear energy: Overview of the legal framework. IAEA. 1995;37(3):16-25. [Link]
56. Longmuir C, Agyapong V. Social and mental health impact of nuclear disaster in survivors: A narrative review. Behav Sci. 2021;11(8):113. [Link] [DOI:10.3390/bs11080113]
57. Romig LE. Pediatric triage. A system to JumpSTART your triage of young patients at MCIs. JEMS. 2002;27(7):52-8. [Link]
58. Martin PG. Spectroscopy and isotopic analysis of ejecta material. In: The 2011 Fukushima Daiichi nuclear power plant accident: An analysis from the metre to the nanometre scale. Cham: Springer; 2019. p. 251-95. [Link] [DOI:10.1007/978-3-030-17191-9_10]
59. Slim H, Bonwick A. Protection: An ALNAP guide for humanitarian agencies. Oxford: Oxfam; 2006. [Link] [DOI:10.3362/9780855988869]
60. Beauchamp TL, Childress JF. Principles of biomedical ethics. Oxford: Oxford University Press; 1994. [Link]
61. Silva RSD, Campos AER, Pereira Á. Caring for the patient in the process of dying at the Intensive Care Unit. Revista da Escola de Enfermagem da USP. 2011;45(3):738-44. [Portuguese] [Link] [DOI:10.1590/S0080-62342011000300027]
62. Domres B, Koch M, Manger A, Becker HD. Ethics and triage. Prehosp Disaster Med. 2001;16(1):53-8. [Link] [DOI:10.1017/S1049023X00025590]
63. Koch J, Tadmor J. Sheltering-A protective measure following an accidental atmospheric release from a nuclear power plant. Health Phys. 1988;54(6):659-67. [Link] [DOI:10.1097/00004032-198806000-00006]
64. Trotti A, Colevas AD, Setser A, Rusch V, Jaques D, Budach V, et al. CTCAE v3.0: Development of a comprehensive grading system for the adverse effects of cancer treatment. Semin Radiat Oncol. 2003;13(3):176-81. [Link] [DOI:10.1016/S1053-4296(03)00031-6]
65. Handl G. State liability for accidental transnational environmental damage by private persons. Am J Int Law. 1980;74(3):525-65. [Link] [DOI:10.2307/2201649]
66. Shrader-Frechette K, Persson L. Ethical issues in radiation protection. Health Phys. 1997;73(2):378-82. [Link] [DOI:10.1097/00004032-199708000-00011]
67. Xiang H, Zhu Y. The ethics issues of nuclear energy: Hard lessons learned from Chernobyl and Fukushima. J Health Ethics. 2011;7(2):6. [Link] [DOI:10.18785/ojhe.0702.06]









