Volume 16, Issue 2 (2024)
Iran J War Public Health 2024, 16(2): 117-122 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2024/03/27 | Accepted: 2024/05/10 | Published: 2024/06/25
Received: 2024/03/27 | Accepted: 2024/05/10 | Published: 2024/06/25
How to cite this article
Kassid M, Mohammed Z. Healthcare Services and its Association with Quality of Life among Amputees. Iran J War Public Health 2024; 16 (2) :117-122
URL: http://ijwph.ir/article-1-1402-en.html
URL: http://ijwph.ir/article-1-1402-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Authors
M.M. Kassid *1, Z.J. Mohammed2
1- Thiqar Health Directorate, Ministry of Health, Nasiriya, Iraq
2- Department of Basic Sciences, College of Nursing, University of Baghdad, Baghdad, Iraq
2- Department of Basic Sciences, College of Nursing, University of Baghdad, Baghdad, Iraq
Full-Text (HTML) (439 Views)
Introduction
Amputation, the surgical removal of limbs and extremities, can lead to various challenges that individuals must confront post-surgery, impacting their physical, psychological, and social well-being negatively [1]. Anatomical loss also results in the loss of function, alterations in body mass distribution, coordination issues, and psychosocial challenges. The World Health Organization (WHO) estimates that between 40 and 70 million individuals worldwide experience limb loss, a number projected to increase in the upcoming decades [2]. Within this demographic, quality of life (QOL) stands out as a central concern, as it is influenced by factors, such as access to and utilization of healthcare services that cater to the unique needs of amputees more effectively than others [3]. The WHO describes QOL as an individual’s subjective assessment of their life circumstances within the framework of culture, values, and in relation to the challenges, aspirations, and benchmarks established by environmental factors [4]. QOL is associated with many factors and refers to different aspects of human life, such as the mental, physical, spiritual, and social aspects. Knežević et al. conducted a study comparing the QOL between individuals who have undergone amputation and those who have not. The research revealed that individuals with intact limbs reported significantly higher QOL compared to those who had undergone amputation. Specifically, individuals who had undergone below-the-knee amputation exhibited better physical abilities and overall health compared to those who had undergone above-the-knee amputation, with the latter group reporting even lower QOL [5]. Sihn et al. further validated that individuals who have undergone amputation at or above the knee joint experienced a notably reduced QOL. Their findings indicated that individuals post-thigh amputation reported a lower QOL when compared to the general population [6].
The research underscores the necessity of comprehensive care for amputees, emphasizing the importance of adequately preparing them for life post-amputation and raising awareness among the public about the mental and functional impacts of limb loss. Individuals who have undergone amputation face significant challenges, including stress, pain, and emotional distress. The lack of limbs is a huge problem, independent of the reasons for amputation. Following amputation it is crucial to start active rehabilitation, including physical therapy and occupational therapy, encouraging the patient to apply prosthesis and return to his/her routine social activities. The provision of integrated healthcare services significantly enhances the effective management of the multifaceted needs of individuals with amputations [7]. Accessing healthcare services is a human right. It is essential to establish an efficient rehabilitation plan encompassing physical therapy, prosthetic and orthotic interventions, psychological support, and social integration. Proper care and rehabilitation significantly contribute to improvement in performance in patients following limb amputation. This comprehensive approach leads to improved overall well-being and functional outcomes for individuals who have experienced limb loss. Through utilizing such services, individuals with limb loss not only experience physical recovery but also learn to adapt and cope with life’s challenges, ultimately enhancing their QOL. Despite ensuring healthcare access for amputees, disparities in healthcare utilization persist due to various factors, including socioeconomic status, geographical location, and healthcare infrastructure. Studies indicate that individuals from disadvantaged communities or low-income households face barriers to accessing timely and sufficient healthcare services, exacerbating health outcomes and disparities in QOL [8]. Additionally, unequal distribution of healthcare infrastructure, particularly in rural regions or impoverished neighborhoods, further widens existing gaps in the healthcare system, limiting access to specialized care and rehabilitation facilities for individuals with amputations [9]. Dillingham et al. suggested that receiving in-hospital care and rehabilitation has a beneficial impact on individuals post-amputation compared to those discharged to nursing homes or their residences during the postoperative phase. A suitable strategy involving rehabilitation and specialized care facilities can reduce mortality rates, lower the need for reamputation, enhance patient stability, and improve proficiency in prosthetic use [10]. Wegener et al. discussed the influence of self-health management on behavioral changes over specific time periods. Their study aimed to evaluate the acceptance and communication skills of individuals post-lower limb amputation based on self-health management, with the hypothesis that this approach would yield better outcomes compared to traditional support groups. Participants underwent specialized interventions, with those in the self-management (SM) group participating in nine 90-minute group sessions led by trained facilitators. After 6 months, individuals in the SM group exhibited reduced levels of depression, fewer functional limitations, and increased self-efficacy. These interventions were particularly effective for individuals within three years of amputation and those under 65 years old, showcasing the potential to significantly enhance societal functioning for individuals post-amputation [11].
At the household level, rehabilitation service providers can more effectively evaluate the structural environment of persons with disabilities (PWDs) and tailor their treatment strategies to suit the physical settings of these individuals. It is essential for organizations to enhance PWDs’ access by covering transportation costs and offering multipurpose cash transfers or conditional cash transfers. These measures have proven to eliminate financial obstacles, enhance access to medications, and boost mental well-being in low and middle-income nations.
It is crucial to analyze the correlation between healthcare provision and the QOL of amputees for the purpose of policy intervention and healthcare delivery solutions aimed at enhancing outcomes for this group of individuals. While existing literature has focused extensively on rehabilitation interventions, their impact on functional outcomes, and QOL, there is a need for comprehensive studies that explore the role of health services across the diverse demographic and clinical profiles of amputees [1]. Therefore, research investigating healthcare accessibility, treatment adherence, and patients’ self-assessed outcomes can provide insights for policymaking to enhance healthcare services and the well-being of individuals who have experienced limb loss [12].
This study aimed to examine the relationship between QOL and healthcare services among amputees, considering demographic, clinical, and psychosocial factors. By closely examining healthcare utilization patterns, rehabilitation interventions, and patient-reported outcomes, the study aims to identify the key factors influencing QOL outcomes within the studied population.
Instrument and Methods
Study design
This descriptive correlational study investigated the relationship between healthcare services and QOL among clients with amputations and was conducted from October 1, 2023, to March 21, 2024.
Study setting and sample
This study was conducted at the Baghdad Health Directorate, specifically at the Al-Rusafa/Al-Salam, Al-Ghadeer, and Sadr Al-Qana, Al-Rusafa/Al-Mustafa, and Al-Hamza Centers for the Rehabilitation of the Disabled. A sample of 200 clients was selected by convenience (non-probability) sampling based on the inclusion criteria, including individuals who have undergone amputation, individuals at varying levels of education, individuals from diverse age groups, and volunteers who agreed to participate in the study after providing their consent.
Study instrument
The used questionnaire includes socio-demographic characteristics, such as age, gender, marital status, education level, occupation, monthly income, reasons for amputation, site of amputation, duration of amputation, and use of assistive devices. The tool used to measure healthcare services was adopted and developed in a previous study [13]. The researchers employed this instrument, primarily based on an extensive literature review, input from experts working with amputee patients, and insights gained from a preliminary study involving a sample of 20 individuals who were asked open-ended questions. The Cronbach’s alpha value in the current study was 0.82, indicating high reliability. QOL, assessed using a tool adopted and developed in previous studies [1, 14], was evaluated for amputee patients. To conduct the QoL assessment, researchers utilized a specialized instrument, drawing from an extensive literature review, expert opinions from professionals working with amputee patients, and insights gained from a preliminary study involving 20 participants who were asked open-ended questions. The Cronbach’s alpha value in the current study was 0.87, indicating high reliability.
Data collection
The researcher conducted interviews with clients at the specified rehabilitation center, providing instructions, addressing their form-related queries, encouraging their participation, and expressing gratitude for their cooperation. Individual interview techniques were employed, with each interview lasting 15-20 minutes, following the essential steps outlined in the study design.
Statistical analysis
All statistical analyses were carried out using SPSS 20.0 software. Numbers and percentages were utilized to rank the parameters, while mean and standard deviation were used to describe continuous parameters statistically. Normality was assessed using Kolmogorov-Smirnov and Shapiro-Wilk tests. Furthermore, a simple linear regression analysis was conducted to assess the relationship between the groups, with a statistical significance threshold set at 0.05.
Findings
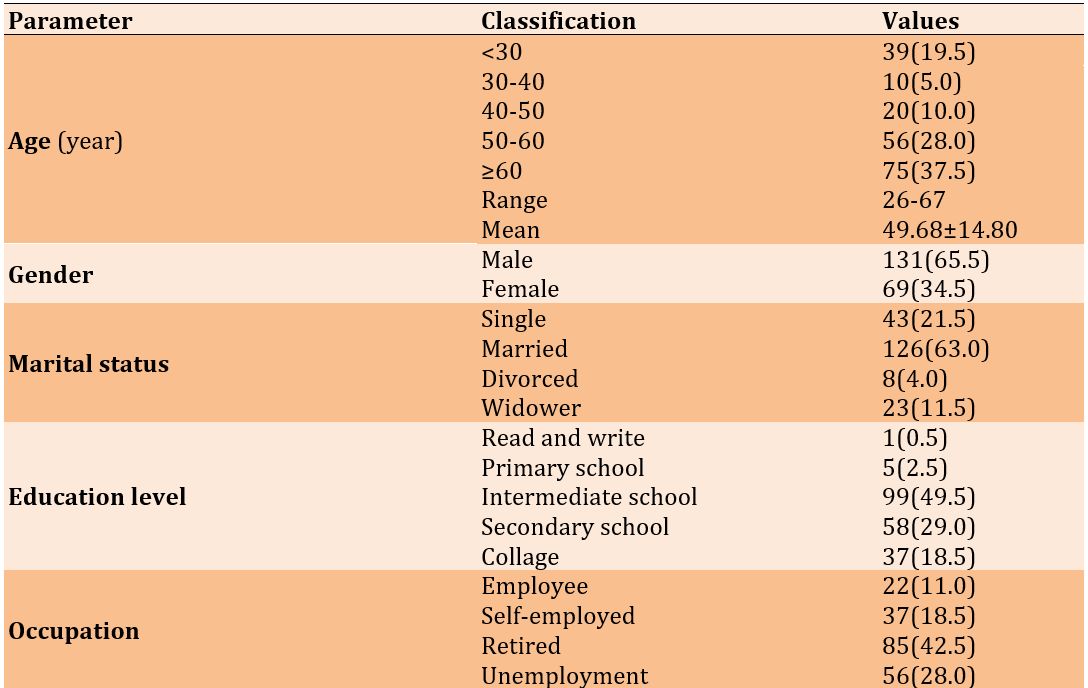
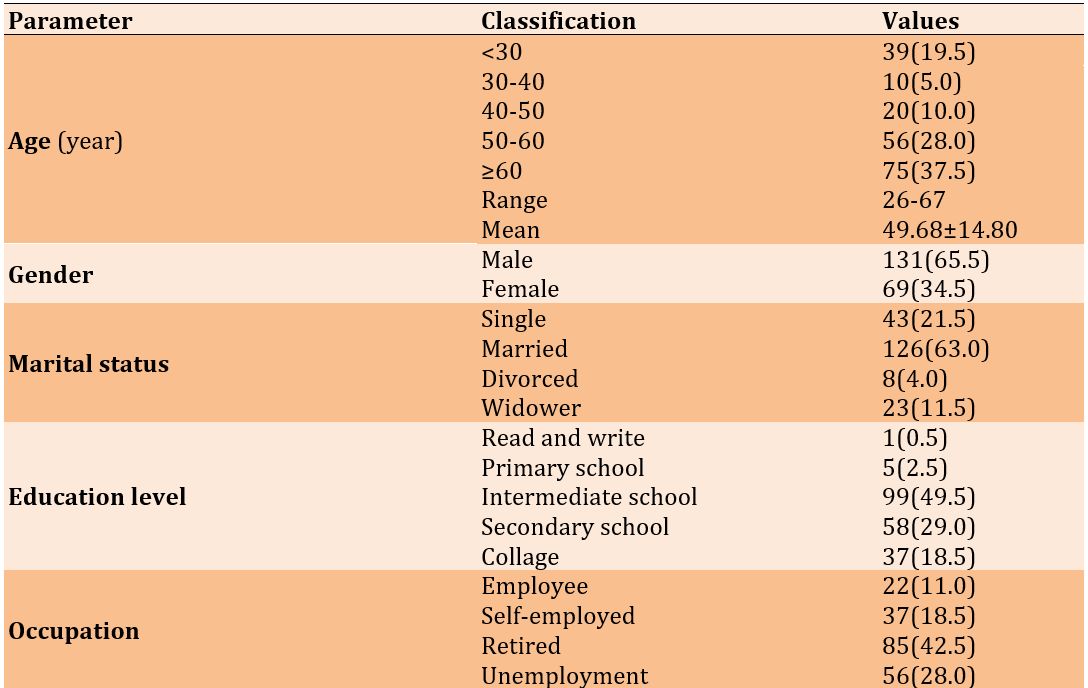
Healthcare services and QOL were comparable between amputees and non-amputees. The participants’ ages ranged from 24 to 67 years, with an average age of 49.68. The gender distribution was 65.5% male and 34.5% female. A majority of the participants were married (63%), while nearly half had completed intermediate school (49.5%). Among the participants, 42.5% were retirees. The most commonly reported income range was between 100 and less than 200 dollars (47%). The primary reason for amputation was health conditions, predominantly affecting the lower extremities (73%). On average, the number of years since amputation was 14.71%, and 48.5% of respondents were using artificial limbs (Table 1).
Table 1. Frequency and mean values of socio-demographic characteristics of the subjects
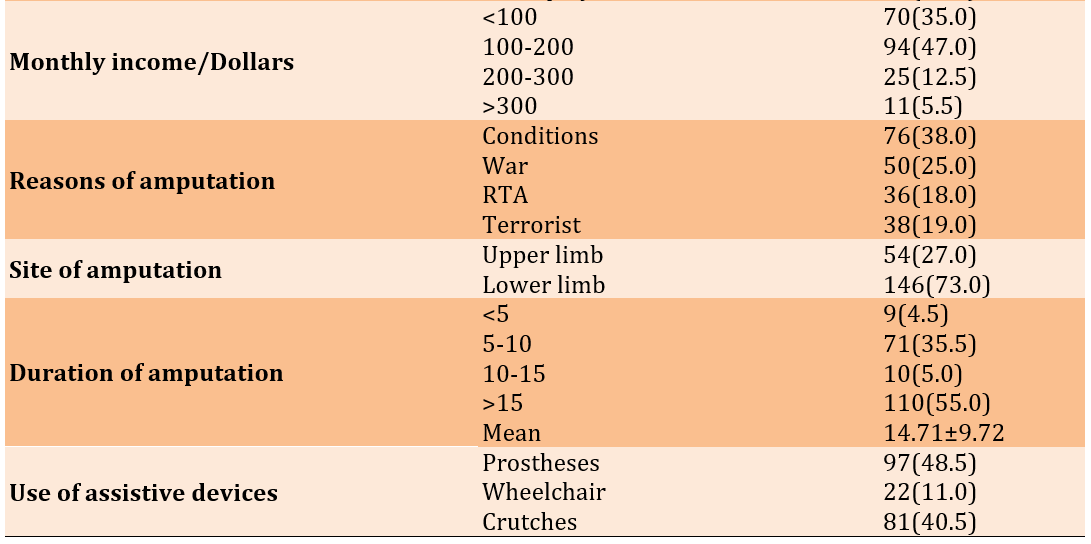
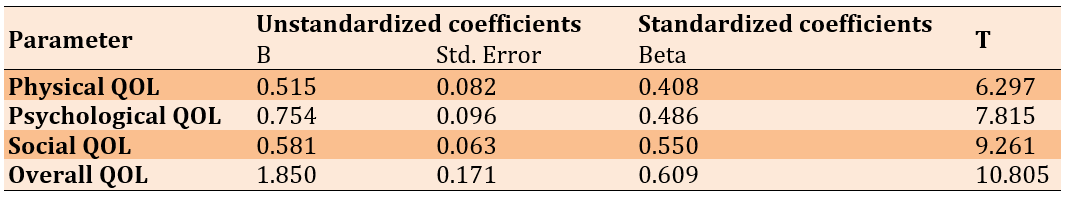
The results of the simple linear regression analysis indicated a significant and positive relationship between healthcare services for amputees and various dimensions of their QOL with a p-value of 0.0001. Specifically, the analysis showed that an increase in healthcare services was correlated with higher levels of physical QOL (β=0.408), psychological QOL (β=0.486), social QOL (β=0.550), and overall QOL (β=0.609; Table 2).
Table 2. Relationship between healthcare services and quality of life (QOL) of amputees
Discussion
This study involving 200 individuals compared two groups based on healthcare services and QOL. This research, encompassing patients aged between 24 and 67 years with an average age of 49.68, provided comprehensive insights into demographic statistics and socio-economic factors influencing their healthcare experiences and QOL. The findings of this study are in line with a case-control study that included patients with ulcerative colitis, which represented a chronic disease and its challenging consequences that occur in old age [15]. The gender distribution among the participants was noteworthy, with 65.5% being male and 34.5% female, suggesting a slight male predominance. The results confirm the expected pattern that major chronic diseases are predominantly found in men within the comparison group [16].
Moreover, a significant proportion of the participants, 63% of them, were married, suggesting potential effects on family support and caregiving patterns for both groups. These results are consistent with a study conducted in heart centers in Baghdad, where the majority of individuals, regardless of their diseases, are married [17]. The educational attainment of the participants was also a crucial factor, with nearly half of them having completed secondary education (49.5%), providing insights into the diverse educational backgrounds of the study participants. These findings mirror those of the study conducted at Al-Muthanna Teaching Hospital involving dialysis patients, indicating a high percentage of patients with limited educational levels [18]. Additionally, retirees were well-represented among the respondents (42.5%), possibly indicating the influence of access to healthcare services and financial stability post-retirement. These findings are consistent with a study among diabetic foot patients, which reveals that the majority of them are already retired [19].
The participants’ incomes were distributed as follows: 47% earned 100 to less than 200 dollars per month, potentially leading to economic challenges in accessing healthcare and other essential services. A study conducted in Babil Governorate echoes the results of research carried out in the same province (Iraq), indicating that individuals with limited incomes are more likely to experience psychological loneliness [20]. The research highlighted that common health disorders, primarily affecting the lower limbs, were the leading cause of amputation among the participants, accounting for 73% of the cases. This underscores the importance of preventive healthcare measures and early intervention in reducing the incidence of conditions necessitating amputation. Similar findings were reported at the Babylon Center for Disabled People Rehabilitation Unit [21]. Furthermore, the average number of years since amputation was 14.71, indicating a significant period post-amputation that may require comprehensive management of long-term physical and psychosocial issues associated with limb loss [22].
The results of a simple linear regression analysis demonstrated that providing medical care to amputees significantly enhances their physical QOL. The regression coefficient (β) of 0.408 suggests that healthcare services lead to a one-unit increase in the physical QOL for amputees. This finding is consistent with previous studies indicating that medical interventions are crucial for enhancing the QOL for individuals with amputations [23]. Healthcare professionals can offer personalized treatments such as prosthetic fitting, rehabilitation programs, and psychological support, addressing the diverse and intricate needs of amputees, thereby enhancing their physical functioning and overall QOL. By recognizing the impact of healthcare services on physical well-being, healthcare professionals are likely to prioritize treatments like prosthetic fitting, rehabilitation programs, and psychological support, ultimately resulting in an improved QOL for individuals with limb loss. In essence, the medical services provided serve as evidence of the significant positive effects of healthcare services on the lives of amputees, enhancing their QOL and promoting self-reliance.
The results of the simple linear regression analysis indicated a significant and positive relationship between physical well-being and healthcare services tailored for amputees. Consistent with other research emphasizing the crucial role of care interventions in enhancing the overall well-being of the general population [24], this study aligns with these established findings. The positive coefficient suggests that a focus on healthcare services addressing amputation-related needs correlates with improved mental health among those affected. These results support previous research advocating for a holistic care approach that encompasses both physical and psychological aspects of treatment for patients with limb loss.
This discovery reinforces the current understanding among medical professionals regarding the interconnectedness of physical health and psychological well-being, particularly evident in populations facing significant health challenges like limb loss [25]. Ultimately, the findings underscored the effectiveness of targeted healthcare interventions for amputees, emphasizing the necessity of a comprehensive approach that considers not only their medical requirements but also their emotional and psychological well-being.
The positive and significant correlation between the social well-being of amputees and accessible personalized healthcare services underscores the importance of tailored medical care for individuals affected by limb loss as a preferred approach for enhancing their QOL. Additional findings from the study suggested that the quality of healthcare played a pivotal role as one of the primary determinants of psychosocial well-being among amputees [26, 27]. This statistically significant relationship builds upon previous study findings, indicating that targeted healthcare interventions effectively contribute to the recovery and adaptation of individuals who have experienced limb loss. Consistent with evidence from prior research, holistic healthcare models that address the individual needs of amputees by catering not only to their physical requirements but also to social inclusion and psychological resilience are more effective [28]. These results prompt stakeholders to consider and implement healthcare integration strategies that can ultimately foster social integration and well-being for individuals who have lost their limbs within society.
The comparison of healthcare services for amputees and their overall QOL, as analyzed through simple linear regression, revealed a significant relationship. The positive estimate (β=0.609) affirmed that healthcare initiatives have a substantial positive impact on the QOL for individuals who have lost limbs. This finding aligns with previous research emphasizing that successful healthcare interventions are a key factor in enhancing the lives of amputees [1]. Therefore, the study’s outcome underscores the critical need to prioritize and enhance healthcare services for amputees to improve their QOL. Furthermore, the study reinforced the interconnectedness of healthcare accessibility and quality for amputees, emphasizing the importance of resource allocation and the development of targeted strategies to enhance healthcare accessibility and quality for this population. By recognizing and addressing the specific healthcare needs of this diverse group, we can not only enhance their QOL but also establish a more equitable and inclusive healthcare system [29]. The insights derived from this research hold practical significance for the healthcare system, enabling them to tailor their services and interventions to support amputees, thereby contributing to their well-being and social inclusion. As a result, it is advisable for policymakers and healthcare providers to prioritize the accessibility and quality of healthcare services customized to meet the unique requirements of amputees, ultimately enhancing their overall QOL.
Conclusion
There is a robust and positive correlation between healthcare services for amputees and their comprehensive QOL, encompassing physical, psychological, and social aspects.
Acknowledgments: We would like to thank all the participants who permitted us to interview herm for close cooperation and participation.
Ethical Permission: Ethical approval was obtained from the Research Ethics Committee of the College of Nursing/ University of Baghdad (No.: 709, dated 2/10/2023).
Conflicts of Interests: The authors reported no conflicts of interests.
Authors’ Contribution: Kassid MM (First Author), Methodologist/Main Researcher/Discussion Writer (50%); Mohammed ZJ (Second Author), Introduction Writer/Methodologist/Assistant Researcher/Statistical Analyst (50%)
Funding/Support: The present study was not financially supported.
Amputation, the surgical removal of limbs and extremities, can lead to various challenges that individuals must confront post-surgery, impacting their physical, psychological, and social well-being negatively [1]. Anatomical loss also results in the loss of function, alterations in body mass distribution, coordination issues, and psychosocial challenges. The World Health Organization (WHO) estimates that between 40 and 70 million individuals worldwide experience limb loss, a number projected to increase in the upcoming decades [2]. Within this demographic, quality of life (QOL) stands out as a central concern, as it is influenced by factors, such as access to and utilization of healthcare services that cater to the unique needs of amputees more effectively than others [3]. The WHO describes QOL as an individual’s subjective assessment of their life circumstances within the framework of culture, values, and in relation to the challenges, aspirations, and benchmarks established by environmental factors [4]. QOL is associated with many factors and refers to different aspects of human life, such as the mental, physical, spiritual, and social aspects. Knežević et al. conducted a study comparing the QOL between individuals who have undergone amputation and those who have not. The research revealed that individuals with intact limbs reported significantly higher QOL compared to those who had undergone amputation. Specifically, individuals who had undergone below-the-knee amputation exhibited better physical abilities and overall health compared to those who had undergone above-the-knee amputation, with the latter group reporting even lower QOL [5]. Sihn et al. further validated that individuals who have undergone amputation at or above the knee joint experienced a notably reduced QOL. Their findings indicated that individuals post-thigh amputation reported a lower QOL when compared to the general population [6].
The research underscores the necessity of comprehensive care for amputees, emphasizing the importance of adequately preparing them for life post-amputation and raising awareness among the public about the mental and functional impacts of limb loss. Individuals who have undergone amputation face significant challenges, including stress, pain, and emotional distress. The lack of limbs is a huge problem, independent of the reasons for amputation. Following amputation it is crucial to start active rehabilitation, including physical therapy and occupational therapy, encouraging the patient to apply prosthesis and return to his/her routine social activities. The provision of integrated healthcare services significantly enhances the effective management of the multifaceted needs of individuals with amputations [7]. Accessing healthcare services is a human right. It is essential to establish an efficient rehabilitation plan encompassing physical therapy, prosthetic and orthotic interventions, psychological support, and social integration. Proper care and rehabilitation significantly contribute to improvement in performance in patients following limb amputation. This comprehensive approach leads to improved overall well-being and functional outcomes for individuals who have experienced limb loss. Through utilizing such services, individuals with limb loss not only experience physical recovery but also learn to adapt and cope with life’s challenges, ultimately enhancing their QOL. Despite ensuring healthcare access for amputees, disparities in healthcare utilization persist due to various factors, including socioeconomic status, geographical location, and healthcare infrastructure. Studies indicate that individuals from disadvantaged communities or low-income households face barriers to accessing timely and sufficient healthcare services, exacerbating health outcomes and disparities in QOL [8]. Additionally, unequal distribution of healthcare infrastructure, particularly in rural regions or impoverished neighborhoods, further widens existing gaps in the healthcare system, limiting access to specialized care and rehabilitation facilities for individuals with amputations [9]. Dillingham et al. suggested that receiving in-hospital care and rehabilitation has a beneficial impact on individuals post-amputation compared to those discharged to nursing homes or their residences during the postoperative phase. A suitable strategy involving rehabilitation and specialized care facilities can reduce mortality rates, lower the need for reamputation, enhance patient stability, and improve proficiency in prosthetic use [10]. Wegener et al. discussed the influence of self-health management on behavioral changes over specific time periods. Their study aimed to evaluate the acceptance and communication skills of individuals post-lower limb amputation based on self-health management, with the hypothesis that this approach would yield better outcomes compared to traditional support groups. Participants underwent specialized interventions, with those in the self-management (SM) group participating in nine 90-minute group sessions led by trained facilitators. After 6 months, individuals in the SM group exhibited reduced levels of depression, fewer functional limitations, and increased self-efficacy. These interventions were particularly effective for individuals within three years of amputation and those under 65 years old, showcasing the potential to significantly enhance societal functioning for individuals post-amputation [11].
At the household level, rehabilitation service providers can more effectively evaluate the structural environment of persons with disabilities (PWDs) and tailor their treatment strategies to suit the physical settings of these individuals. It is essential for organizations to enhance PWDs’ access by covering transportation costs and offering multipurpose cash transfers or conditional cash transfers. These measures have proven to eliminate financial obstacles, enhance access to medications, and boost mental well-being in low and middle-income nations.
It is crucial to analyze the correlation between healthcare provision and the QOL of amputees for the purpose of policy intervention and healthcare delivery solutions aimed at enhancing outcomes for this group of individuals. While existing literature has focused extensively on rehabilitation interventions, their impact on functional outcomes, and QOL, there is a need for comprehensive studies that explore the role of health services across the diverse demographic and clinical profiles of amputees [1]. Therefore, research investigating healthcare accessibility, treatment adherence, and patients’ self-assessed outcomes can provide insights for policymaking to enhance healthcare services and the well-being of individuals who have experienced limb loss [12].
This study aimed to examine the relationship between QOL and healthcare services among amputees, considering demographic, clinical, and psychosocial factors. By closely examining healthcare utilization patterns, rehabilitation interventions, and patient-reported outcomes, the study aims to identify the key factors influencing QOL outcomes within the studied population.
Instrument and Methods
Study design
This descriptive correlational study investigated the relationship between healthcare services and QOL among clients with amputations and was conducted from October 1, 2023, to March 21, 2024.
Study setting and sample
This study was conducted at the Baghdad Health Directorate, specifically at the Al-Rusafa/Al-Salam, Al-Ghadeer, and Sadr Al-Qana, Al-Rusafa/Al-Mustafa, and Al-Hamza Centers for the Rehabilitation of the Disabled. A sample of 200 clients was selected by convenience (non-probability) sampling based on the inclusion criteria, including individuals who have undergone amputation, individuals at varying levels of education, individuals from diverse age groups, and volunteers who agreed to participate in the study after providing their consent.
Study instrument
The used questionnaire includes socio-demographic characteristics, such as age, gender, marital status, education level, occupation, monthly income, reasons for amputation, site of amputation, duration of amputation, and use of assistive devices. The tool used to measure healthcare services was adopted and developed in a previous study [13]. The researchers employed this instrument, primarily based on an extensive literature review, input from experts working with amputee patients, and insights gained from a preliminary study involving a sample of 20 individuals who were asked open-ended questions. The Cronbach’s alpha value in the current study was 0.82, indicating high reliability. QOL, assessed using a tool adopted and developed in previous studies [1, 14], was evaluated for amputee patients. To conduct the QoL assessment, researchers utilized a specialized instrument, drawing from an extensive literature review, expert opinions from professionals working with amputee patients, and insights gained from a preliminary study involving 20 participants who were asked open-ended questions. The Cronbach’s alpha value in the current study was 0.87, indicating high reliability.
Data collection
The researcher conducted interviews with clients at the specified rehabilitation center, providing instructions, addressing their form-related queries, encouraging their participation, and expressing gratitude for their cooperation. Individual interview techniques were employed, with each interview lasting 15-20 minutes, following the essential steps outlined in the study design.
Statistical analysis
All statistical analyses were carried out using SPSS 20.0 software. Numbers and percentages were utilized to rank the parameters, while mean and standard deviation were used to describe continuous parameters statistically. Normality was assessed using Kolmogorov-Smirnov and Shapiro-Wilk tests. Furthermore, a simple linear regression analysis was conducted to assess the relationship between the groups, with a statistical significance threshold set at 0.05.
Findings
Healthcare services and QOL were comparable between amputees and non-amputees. The participants’ ages ranged from 24 to 67 years, with an average age of 49.68. The gender distribution was 65.5% male and 34.5% female. A majority of the participants were married (63%), while nearly half had completed intermediate school (49.5%). Among the participants, 42.5% were retirees. The most commonly reported income range was between 100 and less than 200 dollars (47%). The primary reason for amputation was health conditions, predominantly affecting the lower extremities (73%). On average, the number of years since amputation was 14.71%, and 48.5% of respondents were using artificial limbs (Table 1).
Table 1. Frequency and mean values of socio-demographic characteristics of the subjects
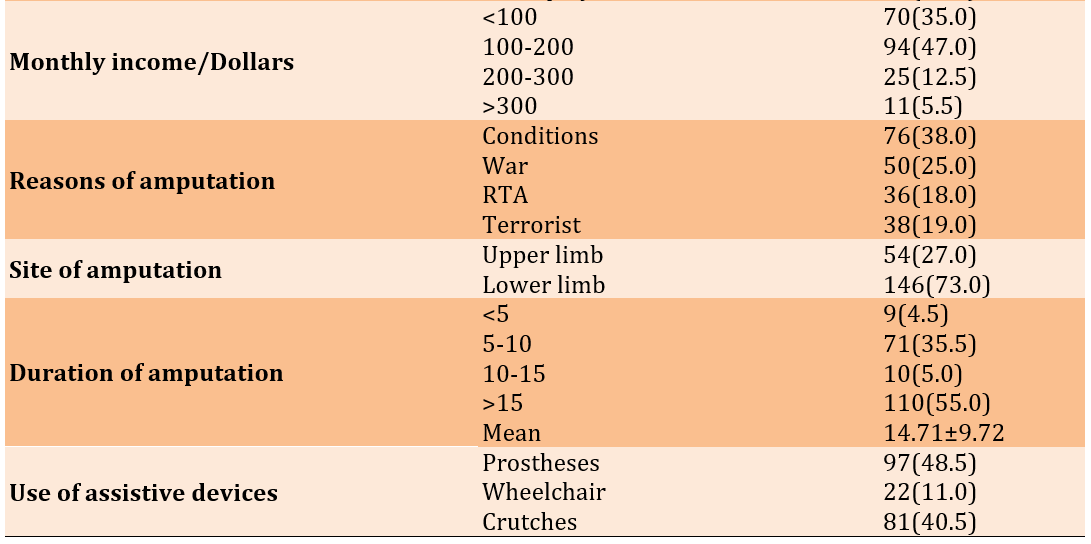
The results of the simple linear regression analysis indicated a significant and positive relationship between healthcare services for amputees and various dimensions of their QOL with a p-value of 0.0001. Specifically, the analysis showed that an increase in healthcare services was correlated with higher levels of physical QOL (β=0.408), psychological QOL (β=0.486), social QOL (β=0.550), and overall QOL (β=0.609; Table 2).
Table 2. Relationship between healthcare services and quality of life (QOL) of amputees
Discussion
This study involving 200 individuals compared two groups based on healthcare services and QOL. This research, encompassing patients aged between 24 and 67 years with an average age of 49.68, provided comprehensive insights into demographic statistics and socio-economic factors influencing their healthcare experiences and QOL. The findings of this study are in line with a case-control study that included patients with ulcerative colitis, which represented a chronic disease and its challenging consequences that occur in old age [15]. The gender distribution among the participants was noteworthy, with 65.5% being male and 34.5% female, suggesting a slight male predominance. The results confirm the expected pattern that major chronic diseases are predominantly found in men within the comparison group [16].
Moreover, a significant proportion of the participants, 63% of them, were married, suggesting potential effects on family support and caregiving patterns for both groups. These results are consistent with a study conducted in heart centers in Baghdad, where the majority of individuals, regardless of their diseases, are married [17]. The educational attainment of the participants was also a crucial factor, with nearly half of them having completed secondary education (49.5%), providing insights into the diverse educational backgrounds of the study participants. These findings mirror those of the study conducted at Al-Muthanna Teaching Hospital involving dialysis patients, indicating a high percentage of patients with limited educational levels [18]. Additionally, retirees were well-represented among the respondents (42.5%), possibly indicating the influence of access to healthcare services and financial stability post-retirement. These findings are consistent with a study among diabetic foot patients, which reveals that the majority of them are already retired [19].
The participants’ incomes were distributed as follows: 47% earned 100 to less than 200 dollars per month, potentially leading to economic challenges in accessing healthcare and other essential services. A study conducted in Babil Governorate echoes the results of research carried out in the same province (Iraq), indicating that individuals with limited incomes are more likely to experience psychological loneliness [20]. The research highlighted that common health disorders, primarily affecting the lower limbs, were the leading cause of amputation among the participants, accounting for 73% of the cases. This underscores the importance of preventive healthcare measures and early intervention in reducing the incidence of conditions necessitating amputation. Similar findings were reported at the Babylon Center for Disabled People Rehabilitation Unit [21]. Furthermore, the average number of years since amputation was 14.71, indicating a significant period post-amputation that may require comprehensive management of long-term physical and psychosocial issues associated with limb loss [22].
The results of a simple linear regression analysis demonstrated that providing medical care to amputees significantly enhances their physical QOL. The regression coefficient (β) of 0.408 suggests that healthcare services lead to a one-unit increase in the physical QOL for amputees. This finding is consistent with previous studies indicating that medical interventions are crucial for enhancing the QOL for individuals with amputations [23]. Healthcare professionals can offer personalized treatments such as prosthetic fitting, rehabilitation programs, and psychological support, addressing the diverse and intricate needs of amputees, thereby enhancing their physical functioning and overall QOL. By recognizing the impact of healthcare services on physical well-being, healthcare professionals are likely to prioritize treatments like prosthetic fitting, rehabilitation programs, and psychological support, ultimately resulting in an improved QOL for individuals with limb loss. In essence, the medical services provided serve as evidence of the significant positive effects of healthcare services on the lives of amputees, enhancing their QOL and promoting self-reliance.
The results of the simple linear regression analysis indicated a significant and positive relationship between physical well-being and healthcare services tailored for amputees. Consistent with other research emphasizing the crucial role of care interventions in enhancing the overall well-being of the general population [24], this study aligns with these established findings. The positive coefficient suggests that a focus on healthcare services addressing amputation-related needs correlates with improved mental health among those affected. These results support previous research advocating for a holistic care approach that encompasses both physical and psychological aspects of treatment for patients with limb loss.
This discovery reinforces the current understanding among medical professionals regarding the interconnectedness of physical health and psychological well-being, particularly evident in populations facing significant health challenges like limb loss [25]. Ultimately, the findings underscored the effectiveness of targeted healthcare interventions for amputees, emphasizing the necessity of a comprehensive approach that considers not only their medical requirements but also their emotional and psychological well-being.
The positive and significant correlation between the social well-being of amputees and accessible personalized healthcare services underscores the importance of tailored medical care for individuals affected by limb loss as a preferred approach for enhancing their QOL. Additional findings from the study suggested that the quality of healthcare played a pivotal role as one of the primary determinants of psychosocial well-being among amputees [26, 27]. This statistically significant relationship builds upon previous study findings, indicating that targeted healthcare interventions effectively contribute to the recovery and adaptation of individuals who have experienced limb loss. Consistent with evidence from prior research, holistic healthcare models that address the individual needs of amputees by catering not only to their physical requirements but also to social inclusion and psychological resilience are more effective [28]. These results prompt stakeholders to consider and implement healthcare integration strategies that can ultimately foster social integration and well-being for individuals who have lost their limbs within society.
The comparison of healthcare services for amputees and their overall QOL, as analyzed through simple linear regression, revealed a significant relationship. The positive estimate (β=0.609) affirmed that healthcare initiatives have a substantial positive impact on the QOL for individuals who have lost limbs. This finding aligns with previous research emphasizing that successful healthcare interventions are a key factor in enhancing the lives of amputees [1]. Therefore, the study’s outcome underscores the critical need to prioritize and enhance healthcare services for amputees to improve their QOL. Furthermore, the study reinforced the interconnectedness of healthcare accessibility and quality for amputees, emphasizing the importance of resource allocation and the development of targeted strategies to enhance healthcare accessibility and quality for this population. By recognizing and addressing the specific healthcare needs of this diverse group, we can not only enhance their QOL but also establish a more equitable and inclusive healthcare system [29]. The insights derived from this research hold practical significance for the healthcare system, enabling them to tailor their services and interventions to support amputees, thereby contributing to their well-being and social inclusion. As a result, it is advisable for policymakers and healthcare providers to prioritize the accessibility and quality of healthcare services customized to meet the unique requirements of amputees, ultimately enhancing their overall QOL.
Conclusion
There is a robust and positive correlation between healthcare services for amputees and their comprehensive QOL, encompassing physical, psychological, and social aspects.
Acknowledgments: We would like to thank all the participants who permitted us to interview herm for close cooperation and participation.
Ethical Permission: Ethical approval was obtained from the Research Ethics Committee of the College of Nursing/ University of Baghdad (No.: 709, dated 2/10/2023).
Conflicts of Interests: The authors reported no conflicts of interests.
Authors’ Contribution: Kassid MM (First Author), Methodologist/Main Researcher/Discussion Writer (50%); Mohammed ZJ (Second Author), Introduction Writer/Methodologist/Assistant Researcher/Statistical Analyst (50%)
Funding/Support: The present study was not financially supported.
Keywords:
References
1. Elywy GJ, Radhi MM, Khyoosh Al-Eqabi QA. Social support and its association with the quality of life (QoL) of amputees. Iran Rehabil J. 2022;20(2):253-60. [Link] [DOI:10.32598/irj.20.2.1784.1]
2. Zhang Y, Lazzarini PA, McPhail SM, Van Netten JJ, Armstrong DG, Pacella RE. Global disability burdens of diabetes-related lower-extremity complications in 1990 and 2016. Diabetes Care. 2020;43(5):964-74. [Link] [DOI:10.2337/dc19-1614]
3. Elywy GJ, Radhi MM, Khyoosh Al-Eqabi QA. Relationship between social support and self-hardiness among breast cancer women in Nasiriyah, Iraq. J Pak Med Assoc. 2023;73(9):S9-14. [Link] [DOI:10.47391/JPMA.IQ-02]
4. Uchmanowicz I., Jankowska-Polańska B. Quality of life in internal diseases - selected research questionnaires. Wydawnictwo ECKP. Wrocław 2013. [Link]
5. Knežević A, Salamon T, Milankov M, Ninković S, Jeremić-Knežević M, Tomašević-Todorović S. Assessment of quality of life in patients after lower limb amputation. Medicinski Pregled. 2015;68(3-4):103-8. [Link] [DOI:10.2298/MPNS1504103K]
6. Sinha R, van den Heuvel WJ, Arokiasamy P. Factors affecting quality of life in lower limb amputees. Prosthetics and orthotics international. 2011;35(1):90-6. [Link] [DOI:10.1177/0309364610397087]
7. Radhi MM, Abd RK, Al Eqabi QA. The body image and its relation to self-esteem among amputation patients at Artificial Limbs Hospital at Kut City, Iraq. J Public Health Afr. 2022;13(4):1. [Link] [DOI:10.4081/jphia.2022.1228]
8. Fanaroff AC, Yang L, Nathan AS, Khatana SA, Julien H, Wang TY, et al. Geographic and socioeconomic disparities in major lower extremity amputation rates in metropolitan areas. J Am Heart Assoc. 2021;10(17):e021456. [Link] [DOI:10.1161/JAHA.121.021456]
9. Sayeed MS, Oakman J, Stuckey R. Factors influencing access to and participation in rehabilitation for people with lower limb amputation in East, South, and Southeast Asian developing countries: The perspective of rehabilitation professionals-a qualitative study. Disabil Rehabil. 2024;46(10):2097-116. [Link] [DOI:10.1080/09638288.2023.2217383]
10. Dillingham TR, Pezzin LE. Rehabilitation setting and associated mortality and medical stability among persons with amputations. Arch Phys Med Rehabil. 2008;89(6):1038-45. [Link] [DOI:10.1016/j.apmr.2007.11.034]
11. Wegener ST, Mackenzie EJ, Ephraim P, Ehde D, Williams R. Self-management improves outcomes in persons with limb loss. Arch Phys Med Rehabil. 2009;90(3):373-80. [Link] [DOI:10.1016/j.apmr.2008.08.222]
12. Creager MA, Matsushita K, Arya S, Beckman JA, Duval S, Goodney PP, et al. Reducing nontraumatic lower-extremity amputations by 20% by 2030: Time to get to our feet: A policy statement from the American Heart Association. Circulation. 2021;143(17):e875-91. [Link] [DOI:10.1161/CIR.0000000000000967]
13. Chetty V, Dunpath T, Meghnath S, Mothalal S, Sewmungal V, Kunene U, et al. Satisfaction and adherence of patients with amputations to physiotherapy service at public hospitals in KwaZulu-Natal, South Africa. Afr Health Sci. 2015;15(2):450-6. [Link] [DOI:10.4314/ahs.v15i2.19]
14. Murad SH, Al-Jawary BJ. Assessment of quality of life of amputee in war victims. Ann Coll Med Mosul. 2008;34(1):42-53. [Link] [DOI:10.33899/mmed.2008.32521]
15. Ahmed FF, Hassan HB. Effectiveness of an instructional program on patients with ulcerative colitis adherence for medication and diet to prevent colorectal cancer: Case and control study. Iraqi Natl J Nurs Spec. 2022;35(1):70-81. [Link] [DOI:10.58897/injns.v35i1.505]
16. Qassim WJ, Yasir AA, Radhi MM. Assessment of self-hardness and its relationship to treatment acceptance for patients with diabetes mellitus at diabetic center in Hilla City/Iraq. J Pharm Sci Res. 2018;10(1):142-5. [Link]
17. Mousa AM, Mansour K. Effectiveness of an instructional program concerning healthy lifestyle on patients' attitudes after percutaneous coronary intervention at cardiac centers in Baghdad City. Iraqi Natl J Nurs Spec. 2020;33(1):1-11. [Link] [DOI:10.58897/injns.v33i1.396]
18. Hussein M, Ahmed S. Effectiveness of an educational program on patients' knowledge concerning care of vascular access of hemodialysis in Al-Muthana Teaching Hospitals. Iraqi Natl J Nurs Spec. 2020;33(1):33-43. [Link] [DOI:10.58897/injns.v33i1.399]
19. Khudhair SS, Ahmed SA. Type 2 diabetic patients' knowledge regarding preventive measures of diabetic foot. Iraqi Natl J Nurs Spec. 2022;35(2):22-30. [Link] [DOI:10.58897/injns.v35i2.506]
20. Yasir AA, Qassim WJ, Radhi MM. Assessment the feeling of psychological loneliness among wives of martyrs in the light of some social variables in Babylon Governorate/Iraq. J Pharm Sci Res. 2018;10(1):40-4. [Link]
21. Alkadem ATA, Noori AK. Self-esteem and its correlation with quality of life among amputees. Iran J War Public Health. 2023;15(3):315-21. [Link] [DOI:10.58209/ijwph.15.3.315]
22. Twair AL Hamad HAA, Hassan HB. Effectiveness of instructional program on patients' nutritional habits for patients with peptic ulcer. Iraqi Natl J Nurs Spec. 2023;36(1):35-48. [Link] [DOI:10.58897/injns.v36i1.637]
23. Gil S, Fernandez-Pineda I, Rao B, Neel MD, Baker JN, Wu H, et al. Role of amputation in improving mobility, pain outcomes, and emotional and psychological well-being in children with metastatic osteosarcoma. Am J Hosp Palliat Care. 2019;36(2):105-10. [Link] [DOI:10.1177/1049909118791119]
24. Fragala MS, Cadore EL, Dorgo S, Izquierdo M, Kraemer WJ, Peterson MD, et al. Resistance training for older adults: Position statement from the national strength and conditioning association. J Strength Cond Res. 2019;33(8):2019-52. [Link] [DOI:10.1519/JSC.0000000000003230]
25. Calabrese L, Maffoni M, Torlaschi V, Pierobon A. What is hidden behind amputation? Quanti-qualitative systematic review on psychological adjustment and quality of life in lower limb amputees for non-traumatic reasons. Healthcare. 2023;11(11):1661. [Link] [DOI:10.3390/healthcare11111661]
26. Brier MJ, Williams RM, Turner AP, Henderson AW, Roepke AM, Norvell DC, et al. Quality of relationships with caregivers, depression, and life satisfaction after dysvascular lower extremity amputation. Arch Phys Med Rehabil. 2018;99(3):452-8. [Link] [DOI:10.1016/j.apmr.2017.09.110]
27. Radhi MM, Elywy GJ, Khyoosh Al-Eqabi QA. Burdens among wives of disabled people in the light of some social variables. Iran Rehabil J. 2023;21(3):473-84. [Link] [DOI:10.32598/irj.21.3.1765.3]
28. AL-Jubori RH, Yasir AA, Hindi NK. Quality of life among amputees: A mediating role of social support. Med J Babylon. 2023;20(2):315-21. [Link] [DOI:10.4103/MJBL.MJBL_330_22]
29. Wurdeman SR, Stevens PM, Campbell JH. Mobility analysis of amputees (MAAT I): Quality of life and satisfaction are strongly related to mobility for patients with a lower limb prosthesis. Prosthet Orthot Int. 2018;42(5):498-503. [Link] [DOI:10.1177/0309364617736089]