Volume 15, Issue 2 (2023)
Iran J War Public Health 2023, 15(2): 123-131 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2023/04/21 | Accepted: 2023/06/12 | Published: 2023/08/1
Received: 2023/04/21 | Accepted: 2023/06/12 | Published: 2023/08/1
How to cite this article
Lorestani F, Zarghami M, Shatrian F, Mosavi B. Mental Health Model of Iranian Veterans with Network Analysis Approach. Iran J War Public Health 2023; 15 (2) :123-131
URL: http://ijwph.ir/article-1-1345-en.html
URL: http://ijwph.ir/article-1-1345-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
1- Department of Psychology, Saveh Branch, Islamic Azad University, Saveh, Iran
2- Behavioral Sience Research Center, Lifestyle Research Institue, Baqiyatullah University of Medical Sciences, Tehran, Iran, Behavioral Sience Research Center, Lifestyle Research Institue, Baqiyatullah University of Medical Sciences, Shikh Bahei, Tehran, Iran. Postal Code: 1435916471 (zar100@gmail.com)
3- Prevention Department, Janbazan Medical and Engineering Research Center, Tehran Iran
2- Behavioral Sience Research Center, Lifestyle Research Institue, Baqiyatullah University of Medical Sciences, Tehran, Iran, Behavioral Sience Research Center, Lifestyle Research Institue, Baqiyatullah University of Medical Sciences, Shikh Bahei, Tehran, Iran. Postal Code: 1435916471 (zar100@gmail.com)
3- Prevention Department, Janbazan Medical and Engineering Research Center, Tehran Iran
Full-Text (HTML) (832 Views)
Introduction
Health means the feeling of complete physical, mental, social and spiritual well-being [1]. Mental health is one of the determining and important criteria for people's health and sustainable development of any country. The Sustainable Development Goals of the United Nations are being implemented as a “common plan" to create a more just and sustainable world as a global action. In fact, mental health is the basic pillar of these actions because as the World Health Organization (WHO) has declared, "Without mental health there will be no health or sustainable development” [2]. Mental health is “a state of well-being in which a person realizes own abilities, can cope with the normal stresses of life, work productively and fruitfully, and contribute to her society” [3]. Mental health acts as an inseparable component of overall health and well-being and plays an important role in maintaining physical health and quality of life [4-6].
Bratman et al. state that various mutual factors affect mental health, including social, economic, psychological, physiological, behavioral, environmental, genetic, and epigenetic effects [7]. Three components of mental health have been identified, which include emotional well-being, psychological well-being, and social well-being [8]. A mentally healthy person performs well in different environments, including home, school, and society. Lack of mental health can turn into mental disorders. Mental disorders are defined by the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5) as clinically significant cognitive, emotional regulation, or behavioral disorders that reflect disturbances in psychological, biological, or developmental processes [9].
Mental disorders rank sixth in the world and eighth in the Middle East region. Depression and anxiety disorders have the highest disease burden among mental disorders [10]. According to reports, in the countries of Iran, Bahrain and Qatar, mental disorders have the highest burden of disease. Many factors cause mental disorders, the most important of which are probably economic problems, war and unrest in the Middle East region. One of the factors that cause and reveal mental disorders is war. War has direct and indirect effects on deaths and threats to human health even years after its end [11].
Unfortunately, Iraq's attack on Iran led to a war that is considered an important event in the history of people's lives. A bitter social reality whose psychological injuries will haunt the victims long after the war. Researches show that most veterans do not have a suitable emotional, social, and health adaptation situation [12]. Studies have shown that about 50% of war veterans suffer from Post-Traumatic Stress Disorder (PTSD) [13]. PTSD is associated with other disorders, such as sleep disorders. Most sufferers of PTSD experience sleep disorders throughout their lives [14].
Mental disorders commonly increase mortality by 50%. Therefore, it is not surprising that mental health problems also add greatly to the cost of physical health care. The high prevalence of mental health problems is an important factor in increasing health costs and national economic changes [15].
Among the factors affecting health, the share of genetic and biological factors is only 15%, while the major impact is related to social factors that are caused by people's living and working conditions. Along with background factors such as gender, marital status, and age, psychological variables such as feelings of insecurity, painful experiences, satisfaction with life, social support and trust, and religiosity contribute the most [16]. The model of mental health developed for the spouses of veterans contains indicators of physical, mental, social, and spiritual health and has three dimensions: balance in personality, trying to satisfy needs, and creating a positive environment [17].
Another review based on positive psychology has provided a model for mental health sustainability. Unlike common models and interventions, this model is based on the psychological well-being component. This model states that doctors and researchers can use it to develop, implement and evaluate more balanced treatment. The psychological well-being component seeks to guide people and patients with mental disorders to understand how to regulate their mental health. Common treatments emphasize barriers, but the presented model focuses on reinforcement resources that are involved in better adaptation of mental health and psychological well-being. The sustainable mental health model focuses on identifying the individual's abilities to deal with life's stresses. This model has been suggested as a primary, combined treatment and even as an individual-strengthening intervention in those with chronic psychological disorders [18].
Reflective and formative interpretations are two traditional approaches that investigate the pattern of relationships. Borsboom believes that these two approaches do not provide a correct explanation of the relationships between psychological structures and variables [19]. The third approach that is proposed as an alternative is a network of variables in which psychological constructs are conceptualized. Borsboom offers two reasons for using the new approach. 1) The models and theories related to hidden variables have dominated the field of psychological measurement. 2) Unlike hidden models, the network perspective has helped to expand dynamic systems [20]. The science of network analysis provides the possibility to present integrated models of psychological structures. Network analysis is an interdisciplinary activity that combines psychological theories and quantitative statistical and mathematical methodology in the field of psychology and psychometrics and provides a suitable answer to analytical discussions in this field [19]. The network analysis approach is opposite to reductionism, and the methodology in network analysis is a form of holism. If the human psyche and personality are viewed from the perspective of a network, in addition to the importance of the components in its formation, the whole personality and psyche are also considered important. The use of the network model has expanded in the last few years in examining sets of variables that have an internal relationship with each other. Determining the structure of relationships between family members based on personality characteristics is the title of a study that was conducted using the network analysis technique. The patterns drawn in this study have shown that in families, parents have the shortest personality distance between family members [21].
Network analysis is based on a different theory and specific ontological and methodological assumptions, based on which it also suggests special techniques for collecting, analyzing data, and fitting theoretical models [22]. Therefore, networks can provide models based on data [23].
The method of network analysis raises and expresses many concepts within itself. Each concept produced is a method with the help of which one can understand the hidden facts in the network [24]. A network is defined as a set of nodes and relationships between them. Nodes can be individuals, groups, organizations, countries, etc. In network analysis, the study of relationships between nodes is desired. These relationships may be directed, undirected, weighted, or binary (zero and one). A network is a tool to show the elements of a system and their internal relationship. The relationship is the unit of network analysis [25].
In network literature, variables are called nodes. If a line (edge) is drawn between two variables or nodes, it shows that there is a significant relationship between the two variables. The absence of a connecting line between two variables indicates the absence of a significant relationship between them. The greater the significant relationship between the nodes, the thicker the edge, and the thinner the diameter of the edge, the lower the intensity of the significant relationship [26]. It can be said that network analysis is an abstract model, and it can be easily used to describe various types of phenomena, such as social relations, technological and biological structures, and information networks [23].
Due to the consequences of mental health problems both at the macro level and at the micro level in the society, on the other hand, the problems caused by the war, the vulnerability of veterans has always been considered, and it has been specifically addressed in the laws. According to Article 15 of the comprehensive law on providing services to martyrs, the Shahid Foundation is obliged to cooperate with the Ministry of Health, Treatment, and Medical Education to provide and improve the level of health and treatment and to monitor and control the physical and mental condition of the families of martyrs, veterans, freedmen, and their dependents, to create a comprehensive medical and paramedical information bank and to prepare health records for them. To provide the most suitable services and ways to respond to the challenges and concerns of policymakers, planners, and experts in the field of mental health at Shahid Foundation, the undeniable fact is revealed, which is "the vital role of health-related information in planning and benefiting from available information and data". In the health system, collecting comprehensive and complete information on the population and their health status is considered the most key tool to develop appropriate policies, interventions, and plans that meet the needs of the society. Also, using this information, it is possible to monitor progress and achievements on a national and international scale [27].
Therefore, referring to Article 15 of the comprehensive law on providing services to veterans and due to the prevalence and occurrence, and chronicity of psychiatric disorders and the cost of psychological interventions [15], it is necessary and of particular importance to provide a specific model of the mental health of veterans that can help managers in making decisions.
Guy Rocher believes that resorting to models is an inevitable necessity in all sciences, because most philosophers, thinkers, and researchers, who have discussed the social life of man, have always resorted to analogies or some images to introduce society to themselves. Due to the fact that the social reality is ambiguous, multiple and elusive, to the extent that the human mind does not have the ability to fully understand this reality in its entirety and dynamics, so to be able to talk about this complex reality and break it down into its components and elements, analogies are made. This analogy is made between complex society and simpler and better-known objects and beings, which are called models [28]. A working model can help predict events, and this is the predictor symbol of the model.
By examining the research that has been conducted in the community of veterans and martyrs, no model was found in the field of mental health, and the research conducted are mainly related to the investigation of one aspect of mental health or the effectiveness of a treatment model. The research conducted by foreign researchers has not provided a model of mental health of veterans, and in this case, the lack of such a model is felt both inside and outside the country. Therefore, presenting the mental health model of veterans to identify the determining factors of their mental health to formulate policies and appropriate interventions with the target group is an inevitable necessity. Therefore, the present study aimed to provide a model of the mental health of veterans and identify its determining factors.
Information and Methods
This study is an exploratory research based on correlational network data analysis. The registered data of veterans in the Comprehensive Integrated Information System of Veterans (Sajaya System) was used as the source for analysis. In this system, in addition to demographic information, including age, percentage of veterans, number of children, employment standby, and receiving the pension, psychiatric diagnoses, therapeutic interventions, and questionnaires related to quality of life (SF-12) and Bartel of veterans. The Sejaya system has been launched since the establishment of the Foundation of Martyrs and Veterans Affairs, and other information has been loaded in it over time. The data of this bank has been uploaded since 2019 and is renewed every six months. To identify the pattern of mental health of veterans, the data of mental health components, including Bartel questionnaire information, quality of life, hospitalization history and psychiatric diagnoses, were used. In addition to the above information, data related to the General Health Questionnaire (GHQ) and Symptom Checklist 90 (SCL-90) were also used.
The data of this study was extracted in the second 6 months of 2020, and the national code of veterans was used to unify the data. The basic information of 601,330 veterans in 2020 has been registered in the Sajaya system. Out of the total statistical population, in 83,142 cases, only Bartel and SF-12 questionnaires had been filled in the data bank. In total, 9244 cases had data related to mental health, including data from Bartel, SF-12, SCL-90, and GHQ questionnaires. The analysis were performed on the data of the same bank, regardless of the type of veteran. The questionnaires used in this analysis are as follows:
1) 12-Item Short Form Health Survey (SF-12): SF-12 has 8 subscales that determine quality of life. SF-12 dimensions include: physical functioning, physical role, bodily pain, general health, social functioning, emotional role, vitality, and mental health. A higher score indicates a better quality of life. The validity of the questionnaire was investigated by Montazeri et al. in Iran and confirmed with Cronbach's alpha of 0.73 for the physical component and 0.72 for the psychological component [29].
2) Bartel Questionnaire: This questionnaire evaluates the level of independence of a person in performing daily self-care activities such as hygiene and grooming, eating, bathing, etc., in terms of the amount of help from others. The total score of each person shows the level of independence and dependence in daily activities. This tool has 10 questions, and the level of dependency and independence of the person is evaluated with 0, 2, 5, 8 and 10 scores. A score of 10 means complete independence of the person, and a score of zero means inability to work. This questionnaire has been tested in different age groups of the elderly and patients in various countries, and its reliability has been reported between 60% and 93% [30].
3) Symptom Checklist 90 (SCL-90): This questionnaire is a general tool for measuring the health status of people aged 14 years and above. It includes subscales of somatization, obsessive-compulsive, interpersonal sensibility, depression, anxiety, anger-hostility, phobic-anxiety, paranoid ideation, and psychoticism. The reliability of this tool has been reported to be more than 90% [31].
4) General Health Questionnaire (GHQ): This questionnaire has 28 questions and four subscales of somatic symptoms, anxiety and sleeplessness, social dysfunction, and severe depression and suicidal tendency. Each subscale has 7 questions, and each question is rated on a four-point scale (No, a little, much, very much). Five scores are obtained from this test, 4 of which are related to the subscales, and the other is the sum of the scores of the subscales. This instrument shows general health in 4 levels: none or the least, mild, moderate, and severe. This questionnaire has adequate validity and reliability and has a high predictive power in diagnosing positive and negative cases of psychological disorders [31].
Other variables examined in this study were: age, number of children, employment status, total percentage of veterans, percentage of neurological and mental illness, total hospitalization history during one year, and history of hospitalization in the psychiatric department.
Network indexes were calculated to get the importance of each variable in the network pattern of their relationships. In this study, five network indexes were calculated, which are strength value, closeness value, Benit value, eigenvector centrality value, and leverage value. The first index investigated in the network was the strength index, which refers to the strength of the direct connection of a node with other nodes. The closeness index shows which variables are closer to all variables on average. This index shows the degree of closeness of the variables. Benit index refers to the communication importance of a node and its role in the communication between different nodes. As its name suggests, Benit index shows the connectivity between different nodes. A node with a greater Benit is responsible for transmitting more information in the entire network. The eigenvector centrality index is used to measure the level of influence of a node in the network. Each of the nodes in the network that has a higher value of the eigenvector centrality, the level of their influence in the network is higher. The value of this index is related to the number of connections with other nodes, but it is more affected by the connections with more important nodes in the network. In other words, it is possible that a node in the network has a high degree score (which is solely dependent on the number of connections), but the value of its eigenvector is low. On the other hand, it is possible that the Benit value of a node that considers most of the communication of separate parts of the network is high, but because it is far from the power center of the network, it has a low eigenvector value. In fact, the value of the eigenvector of the node indicates the sphere of influence of the node in the network. The leverage centrality index is another new index in the field of network data analysis and considers the degree of a node in relation to its neighboring nodes. For example, if we consider a social network where person A is in contact with people who are not related to other people in the network (low level), the degree of leverage of this person will increase. A node with a high degree of leverage has a high control over the transmission of information to its neighboring nodes. A node with a negative centrality of leverage is affected by its neighboring nodes because although the nodes interact with them, they also interact with many other nodes, and the positive value of the centrality of leverage indicates that its neighboring nodes are less inclined to communicate with other nodes. Except Benit index, the score range of the indexes is between 0 and 1. The range of Benit index score is between 0 and -2N [20].
The variables were entered into the R software, and the relationship between them was determined based on the degree of correlation in the matrix, which is a two-dimensional space. In order to discover the relationship pattern between the variables and their internal relationship, this matrix was used as the input of the data relationship discovery algorithm. First, the values of the variables were standardized, and the standardized values were entered into the network analysis. To achieve the communication model based on network data analysis, first the distance matrix of the variables was calculated. The inverse value of this distance matrix was considered as the intensity of the relationship between the variables and was used as the input of the network data analysis, and then the network indices were calculated for each variable. Finally, the network pattern was drawn as a visual representation of the relationships between the variables.
Network data analysis was done using graph theory. qgraph software package with the aim of drawing the network of relationships and igraph in order to check the significance of network relationships were written under R language. Spearman's correlation was used to determine the intensity of correlation between both nodes (variables).
Findings
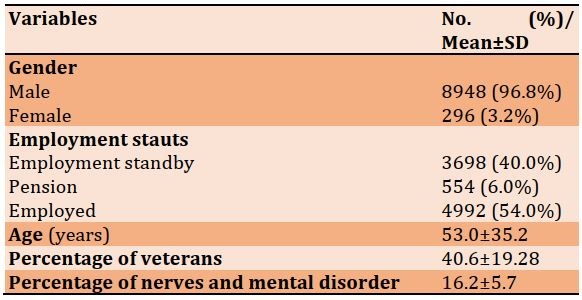
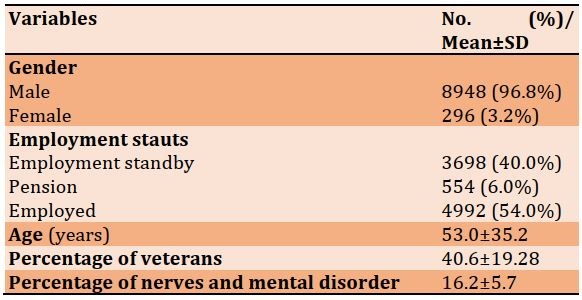
Data analysis was done based on the data bank of the Foundation of Martyrs and Veterans Affairs with 9244 samples. The demographic characteristics of the studied population are presented in Table 1.
Table 1) Demographic characteristics of the studied population (n=9244)
The indexes of the mental health network of veterans based on each variable are presented in Table 2. The first index examined was the strength index (the strength of a node's direct connection with other nodes). Age, number of children, percentage of veterans, percentage of neurological and mental disorders, physical functioning, bodily pain, and mental health were the variables that had the most strength. In addition, the age, number of children, and the percentage of neurological and mental disorders from the demographic characteristics and physical functioning, bodily pain, and mental health from the variables of the quality of life had the highest direct relationship with other variables of the mental health network of veterans.
Table 2) The indexes of the mental health network of veterans based on each variable
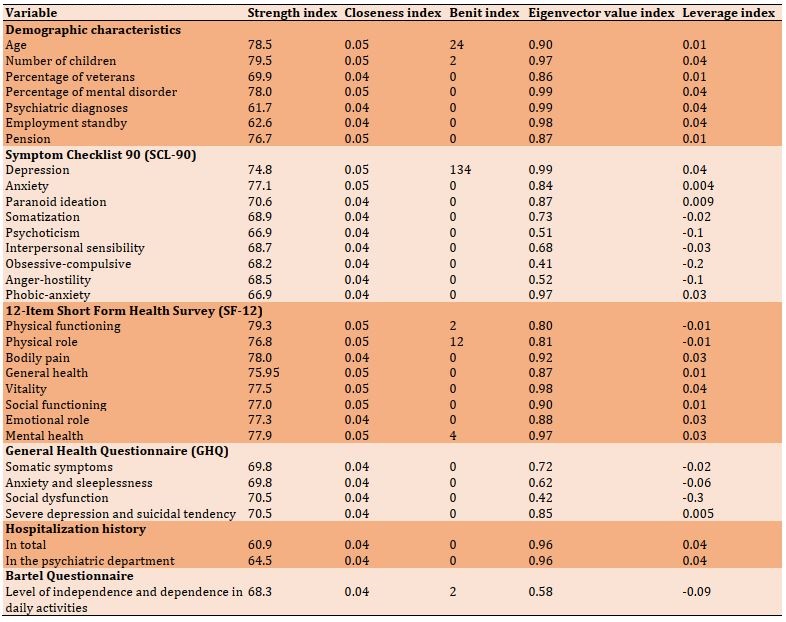
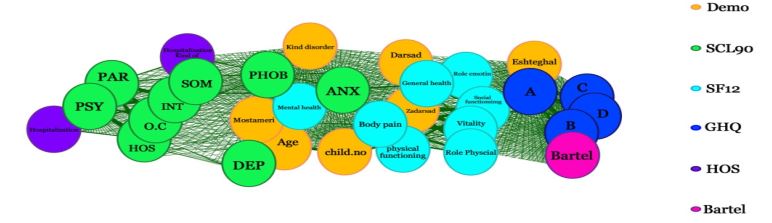
Figure 1) Mental health network in Iranian veterans
The second index examined was the closeness index. The closeness index value of all the variables that entered the model was between 0.04-0.05. All the variables whose closeness was 0.05 had more closeness than other variables. Age, number of children, pension, percentage of neurological and mental disorders, physical functioning, depression, anxiety, general health, physical role, physical functioning, social functioning, and vitality had the greatest value of closeness in the mental health network of veterans. In this index, all variables of SF-12 except for physical pain, variables of age and number of children from demographic characteristics, and anxiety and depression from the SCL-90 scale were closer than other network variables.
The Benit index in this study was between 0 and 134. The Benit value for the variables of depression, age, mental health, physical role, physical functioning, and the number of children in the mental health network of veterans was non-zero. The depression variable played the most important role in the communication path between two network nodes (134 times). After that, the two variables of age (24 times) and mental health (12 times) were in the way of the variables and had the biggest role in information transfer in the whole network. The value of the remaining variables was zero.
The eigenvector was the fourth most important index of the network. The value of the eigenvector in all variables except the obsessive-compulsive variable and social dysfunction was above 0.5. The variables of number of children, percentage of mental disorders, psychiatric diagnoses, especially depression, employment standby, physical problems, and vitality had the highest eigenvector values in the mental health network of veterans.
The fifth index of the network was the centrality of leverage, and its value was between -0.3 and 0.3. The variables of the number of children, the percentage of mental disorders, depression, vitality, history of hospitalization, and the type of hospitalization had higher values (positive) with the mental health network. On the other hand, the level of independence and dependence in daily activities and the variables of obsessive-compulsive, anger-hostility, interpersonal sensibility, and social dysfunction had less desire to communicate with other variables due to the centrality of negative leverage.
Figure 1 is the mental health network of Iranian veterans, which was obtained from the analysis of variables. In this figure, all the edges were drawn in the same color, meaning that the correlations were significantly positive. In addition, there was no significant negative correlation for any of the nodes. This figure shows that the overall shape of the network was intertwined (intertwining means the close relationship of the variables with each other), but some parts of the mental health variables of the veterans have a higher intertwining and are very closely related to each other and have formed a cluster in the network. The meaning of cluster is the accumulation of some variables together in one part of the network. Demographic variables, except employment, quality of life variables (SF-12), and variables of anxiety, depression, and phobia from SCL-90 had a very close relationship with each other and formed the central cluster of the network. On the other hand, the employment variable along with GHQ and Bartel variables formed another cluster on the right side of the network. On the left side, SCL-90 variables (except for depression, anxiety, and phobia, which were placed in the central cluster) formed another cluster with hospitalization history variables. In general, the network consists of three clusters.
Discussion
In this study, for the first time, we described and analyzed the mental health network of veterans based on national data with the amount of 9244 records. The results of this study have shown that the mental health network of veterans consists of various factors and has formed three clusters. The variables within each cluster have a high correlation, and none of the variables in the network have a negative correlation. In this network, all the variables are related to each other, but some of them have a significant role and contribution to this network. This result is in line with the opinion of Bratman et al., who state that various mutual factors can affect mental health, including social, economic, psychological, physiological, behavioral, environmental, genetic, and epigenetic influences [7].
As the indexes and the shape of the network show, the mental health network of veterans consists of a central cluster where the central variables gathered and two peripheral clusters. The cluster in the center of the network plays a very important role in the mental health of veterans. Peripheral variables play a lesser role in the network.
The high values of the network indicators in the variables of quality of life and their placement in the center show the importance of these variables as the main determinants in the mental health of veterans. As Liu et al. state: quality of life is one of the subsets of emotional well-being [32].
In the literature related to emotional well-being, it has been described in different ways, which includes positive and negative dimensions of emotions: the positive dimension of emotional well-being is such as happiness, passion, hope, and satisfaction, and its negative dimension is such as anger, anxiety, and depression [8]. The negative dimension of emotional well-being is visible in the mental health network of veterans in such a way that the variables of quality of life with anxiety and depression, phobia, type of psychiatric disorder and the percentage of veterans and the percentage of neurological and mental disorders are in the same cluster. These results are consistent with the findings of Khoravandi et al. [11]. Noorbala also states that depression and anxiety disorders have the highest disease burden among mental disorders [10].
The variables of age, number of children, pension, type of psychiatric disorder, percentage of veterans and percentage of neurological and mental disorders are also in the center of mental health network of veterans. The centrality of these variables shows their importance and effectiveness in the mental health of veterans. In this regard, Tavakol mentioned the age variable as one of the underlying variables of mental health in his research [33].
As it is clear on the right side of the network, three of the variables related to general health (anxiety and sleeplessness, social dysfunction, and severe depression) have a high correlation with the level of dependency in daily activities. These variables overlap closely with each other and can explain each other. Somatic symptoms, from general health components, have a high correlation with the employment standby of veterans separately. These variables formed the peripheral variables of the mental health network, which have a lesser role than the central variables in the mental health network. Wang et al. suggested that social welfare plays a fundamental role in achieving and maintaining mental health and in preventing and improving health problems [4]. Emotional support from the category social well-being refers to having close relationships with family and friends and feeling loved and cared for, having someone to trust and rely on in difficult life situations, and handling the demands of daily life such as going to appointments, shopping, helping in finance, paying bills, etc. Bjørlykhaug et al. state that social well-being is related to people's physical, functional, social, psychological, and emotional health [34]. They also consider the performance of daily tasks and the degree of dependence on others in the category of physical and social functions, which is consistent with the important role of these variables in the mental health network of veterans [34].
In the other part of the mental health network of veterans, which is closer to the central core of the network, the variables of percentage of veterans, general health, and percentage of mental disorder, bodily pain, and physical functioning are close to the central core. These variables also overlap with each other. Two of the variables of this category, namely physical functioning and bodily pain, have a high strength and correlation with the number of children. Baloglu et al. [8] consider anger, anxiety, and depression to be part of the negative dimensions of emotional well-being. In this study, the negative dimensions of emotional well-being in the mental health network of veterans are evident. Anxiety, sleeplessness, and depression as negative dimensions of emotional well-being are variables that have a significant contribution to the mental health network of veterans and are close to the central core.
On the left side of the mental health network, hospitalization history with paranoid variables and psychoticism showed a very strong correlation. These variables have a strong correlation with the type and history of hospitalization and factors such as anger-hostility, interpersonal sensibility, somatization, and obsessive-compulsive. In this regard, Mikaeili et al. state that the most veterans do not have a suitable adaptation situation in terms of emotional and social health [12]. Despite the close relationship between these variables, due to their location on the periphery of the network, they had a lesser role in the network than the central variables.
Strengths and weaknesses of the study
One of the strengths of this study was the use of the database of the Iranian veterans' information system. On the other hand, the survey was conducted in all veteran groups without considering the percentage or specific type of veterans. The advantage of this study compared to other studies that have been done so far was to address the mental health status of veterans with extensive data in the form of network analysis and model presentation. This study also had limitations and weaknesses, including the lack of similar studies for comparison. Another limitation was the lack of data related to other determinants of mental health, such as education, economic status, underlying diseases, and spiritual factor.
Suggestions
Considering the undeniable impact of mental health in daily life and its deep impact on other health sectors (social, physical and spiritual health), mental health custodians and policymakers in the Foundation of Martyrs and Veterans should pay serious attention to the determinants and factors affecting veterans' health. Therefore, based on the findings of this study, it is suggested to provide any services and support packages to increase the quality of life of veterans according to their age. It seems that they should avoid providing services in a one-dimensional way, and interventions should be provided systematically (providing a package of treatment, education, and support). Since other factors except those mentioned in the study can be effective in the mental health of veterans, it is recommended to include these factors in the comprehensive integrated information system of veterans. The inclusion of mental health questionnaires and other determinants in Sajaya and their completion by veterans can help to periodically monitor the mental health status of veterans.
Researchers are also suggested to consider other determinants of mental health in their investigations. It is also recommended to study the mental health status of veterans using data analysis in different groups of veterans.
Conclusion
The mental health model of Iranian veterans is an intertwined network of variables. Despite the intertwining of all variables, some variables are in the center of the network and have more influence in this network. The main determinants of mental health are variables related to the quality of life along with age, number of children, percentage of neurological and mental disorders, depression, and anxiety, which play a significant role in the mental health network of veterans.
Acknowledgements: We are grateful to all the people who helped in any way to make this work.
Ethical Permission: This study was approved by the Veterans Research Institute with the ethical code IR.ISAAR.REC.1401.007.
Conflict of Interests: There is no conflict of interest.
Authors’ Contribution: Lorestani F (First Author), Main Researcher (65%); Zarghami MH (Second Author), Methodologist/Discussion Writer (15%); Shatrian F (Third Author), Statistical Analyst (5%); Mosavi B (Fourth Author), Introduction Writer (15%)
Funding: The present article is taken from a doctoral thesis.
Health means the feeling of complete physical, mental, social and spiritual well-being [1]. Mental health is one of the determining and important criteria for people's health and sustainable development of any country. The Sustainable Development Goals of the United Nations are being implemented as a “common plan" to create a more just and sustainable world as a global action. In fact, mental health is the basic pillar of these actions because as the World Health Organization (WHO) has declared, "Without mental health there will be no health or sustainable development” [2]. Mental health is “a state of well-being in which a person realizes own abilities, can cope with the normal stresses of life, work productively and fruitfully, and contribute to her society” [3]. Mental health acts as an inseparable component of overall health and well-being and plays an important role in maintaining physical health and quality of life [4-6].
Bratman et al. state that various mutual factors affect mental health, including social, economic, psychological, physiological, behavioral, environmental, genetic, and epigenetic effects [7]. Three components of mental health have been identified, which include emotional well-being, psychological well-being, and social well-being [8]. A mentally healthy person performs well in different environments, including home, school, and society. Lack of mental health can turn into mental disorders. Mental disorders are defined by the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5) as clinically significant cognitive, emotional regulation, or behavioral disorders that reflect disturbances in psychological, biological, or developmental processes [9].
Mental disorders rank sixth in the world and eighth in the Middle East region. Depression and anxiety disorders have the highest disease burden among mental disorders [10]. According to reports, in the countries of Iran, Bahrain and Qatar, mental disorders have the highest burden of disease. Many factors cause mental disorders, the most important of which are probably economic problems, war and unrest in the Middle East region. One of the factors that cause and reveal mental disorders is war. War has direct and indirect effects on deaths and threats to human health even years after its end [11].
Unfortunately, Iraq's attack on Iran led to a war that is considered an important event in the history of people's lives. A bitter social reality whose psychological injuries will haunt the victims long after the war. Researches show that most veterans do not have a suitable emotional, social, and health adaptation situation [12]. Studies have shown that about 50% of war veterans suffer from Post-Traumatic Stress Disorder (PTSD) [13]. PTSD is associated with other disorders, such as sleep disorders. Most sufferers of PTSD experience sleep disorders throughout their lives [14].
Mental disorders commonly increase mortality by 50%. Therefore, it is not surprising that mental health problems also add greatly to the cost of physical health care. The high prevalence of mental health problems is an important factor in increasing health costs and national economic changes [15].
Among the factors affecting health, the share of genetic and biological factors is only 15%, while the major impact is related to social factors that are caused by people's living and working conditions. Along with background factors such as gender, marital status, and age, psychological variables such as feelings of insecurity, painful experiences, satisfaction with life, social support and trust, and religiosity contribute the most [16]. The model of mental health developed for the spouses of veterans contains indicators of physical, mental, social, and spiritual health and has three dimensions: balance in personality, trying to satisfy needs, and creating a positive environment [17].
Another review based on positive psychology has provided a model for mental health sustainability. Unlike common models and interventions, this model is based on the psychological well-being component. This model states that doctors and researchers can use it to develop, implement and evaluate more balanced treatment. The psychological well-being component seeks to guide people and patients with mental disorders to understand how to regulate their mental health. Common treatments emphasize barriers, but the presented model focuses on reinforcement resources that are involved in better adaptation of mental health and psychological well-being. The sustainable mental health model focuses on identifying the individual's abilities to deal with life's stresses. This model has been suggested as a primary, combined treatment and even as an individual-strengthening intervention in those with chronic psychological disorders [18].
Reflective and formative interpretations are two traditional approaches that investigate the pattern of relationships. Borsboom believes that these two approaches do not provide a correct explanation of the relationships between psychological structures and variables [19]. The third approach that is proposed as an alternative is a network of variables in which psychological constructs are conceptualized. Borsboom offers two reasons for using the new approach. 1) The models and theories related to hidden variables have dominated the field of psychological measurement. 2) Unlike hidden models, the network perspective has helped to expand dynamic systems [20]. The science of network analysis provides the possibility to present integrated models of psychological structures. Network analysis is an interdisciplinary activity that combines psychological theories and quantitative statistical and mathematical methodology in the field of psychology and psychometrics and provides a suitable answer to analytical discussions in this field [19]. The network analysis approach is opposite to reductionism, and the methodology in network analysis is a form of holism. If the human psyche and personality are viewed from the perspective of a network, in addition to the importance of the components in its formation, the whole personality and psyche are also considered important. The use of the network model has expanded in the last few years in examining sets of variables that have an internal relationship with each other. Determining the structure of relationships between family members based on personality characteristics is the title of a study that was conducted using the network analysis technique. The patterns drawn in this study have shown that in families, parents have the shortest personality distance between family members [21].
Network analysis is based on a different theory and specific ontological and methodological assumptions, based on which it also suggests special techniques for collecting, analyzing data, and fitting theoretical models [22]. Therefore, networks can provide models based on data [23].
The method of network analysis raises and expresses many concepts within itself. Each concept produced is a method with the help of which one can understand the hidden facts in the network [24]. A network is defined as a set of nodes and relationships between them. Nodes can be individuals, groups, organizations, countries, etc. In network analysis, the study of relationships between nodes is desired. These relationships may be directed, undirected, weighted, or binary (zero and one). A network is a tool to show the elements of a system and their internal relationship. The relationship is the unit of network analysis [25].
In network literature, variables are called nodes. If a line (edge) is drawn between two variables or nodes, it shows that there is a significant relationship between the two variables. The absence of a connecting line between two variables indicates the absence of a significant relationship between them. The greater the significant relationship between the nodes, the thicker the edge, and the thinner the diameter of the edge, the lower the intensity of the significant relationship [26]. It can be said that network analysis is an abstract model, and it can be easily used to describe various types of phenomena, such as social relations, technological and biological structures, and information networks [23].
Due to the consequences of mental health problems both at the macro level and at the micro level in the society, on the other hand, the problems caused by the war, the vulnerability of veterans has always been considered, and it has been specifically addressed in the laws. According to Article 15 of the comprehensive law on providing services to martyrs, the Shahid Foundation is obliged to cooperate with the Ministry of Health, Treatment, and Medical Education to provide and improve the level of health and treatment and to monitor and control the physical and mental condition of the families of martyrs, veterans, freedmen, and their dependents, to create a comprehensive medical and paramedical information bank and to prepare health records for them. To provide the most suitable services and ways to respond to the challenges and concerns of policymakers, planners, and experts in the field of mental health at Shahid Foundation, the undeniable fact is revealed, which is "the vital role of health-related information in planning and benefiting from available information and data". In the health system, collecting comprehensive and complete information on the population and their health status is considered the most key tool to develop appropriate policies, interventions, and plans that meet the needs of the society. Also, using this information, it is possible to monitor progress and achievements on a national and international scale [27].
Therefore, referring to Article 15 of the comprehensive law on providing services to veterans and due to the prevalence and occurrence, and chronicity of psychiatric disorders and the cost of psychological interventions [15], it is necessary and of particular importance to provide a specific model of the mental health of veterans that can help managers in making decisions.
Guy Rocher believes that resorting to models is an inevitable necessity in all sciences, because most philosophers, thinkers, and researchers, who have discussed the social life of man, have always resorted to analogies or some images to introduce society to themselves. Due to the fact that the social reality is ambiguous, multiple and elusive, to the extent that the human mind does not have the ability to fully understand this reality in its entirety and dynamics, so to be able to talk about this complex reality and break it down into its components and elements, analogies are made. This analogy is made between complex society and simpler and better-known objects and beings, which are called models [28]. A working model can help predict events, and this is the predictor symbol of the model.
By examining the research that has been conducted in the community of veterans and martyrs, no model was found in the field of mental health, and the research conducted are mainly related to the investigation of one aspect of mental health or the effectiveness of a treatment model. The research conducted by foreign researchers has not provided a model of mental health of veterans, and in this case, the lack of such a model is felt both inside and outside the country. Therefore, presenting the mental health model of veterans to identify the determining factors of their mental health to formulate policies and appropriate interventions with the target group is an inevitable necessity. Therefore, the present study aimed to provide a model of the mental health of veterans and identify its determining factors.
Information and Methods
This study is an exploratory research based on correlational network data analysis. The registered data of veterans in the Comprehensive Integrated Information System of Veterans (Sajaya System) was used as the source for analysis. In this system, in addition to demographic information, including age, percentage of veterans, number of children, employment standby, and receiving the pension, psychiatric diagnoses, therapeutic interventions, and questionnaires related to quality of life (SF-12) and Bartel of veterans. The Sejaya system has been launched since the establishment of the Foundation of Martyrs and Veterans Affairs, and other information has been loaded in it over time. The data of this bank has been uploaded since 2019 and is renewed every six months. To identify the pattern of mental health of veterans, the data of mental health components, including Bartel questionnaire information, quality of life, hospitalization history and psychiatric diagnoses, were used. In addition to the above information, data related to the General Health Questionnaire (GHQ) and Symptom Checklist 90 (SCL-90) were also used.
The data of this study was extracted in the second 6 months of 2020, and the national code of veterans was used to unify the data. The basic information of 601,330 veterans in 2020 has been registered in the Sajaya system. Out of the total statistical population, in 83,142 cases, only Bartel and SF-12 questionnaires had been filled in the data bank. In total, 9244 cases had data related to mental health, including data from Bartel, SF-12, SCL-90, and GHQ questionnaires. The analysis were performed on the data of the same bank, regardless of the type of veteran. The questionnaires used in this analysis are as follows:
1) 12-Item Short Form Health Survey (SF-12): SF-12 has 8 subscales that determine quality of life. SF-12 dimensions include: physical functioning, physical role, bodily pain, general health, social functioning, emotional role, vitality, and mental health. A higher score indicates a better quality of life. The validity of the questionnaire was investigated by Montazeri et al. in Iran and confirmed with Cronbach's alpha of 0.73 for the physical component and 0.72 for the psychological component [29].
2) Bartel Questionnaire: This questionnaire evaluates the level of independence of a person in performing daily self-care activities such as hygiene and grooming, eating, bathing, etc., in terms of the amount of help from others. The total score of each person shows the level of independence and dependence in daily activities. This tool has 10 questions, and the level of dependency and independence of the person is evaluated with 0, 2, 5, 8 and 10 scores. A score of 10 means complete independence of the person, and a score of zero means inability to work. This questionnaire has been tested in different age groups of the elderly and patients in various countries, and its reliability has been reported between 60% and 93% [30].
3) Symptom Checklist 90 (SCL-90): This questionnaire is a general tool for measuring the health status of people aged 14 years and above. It includes subscales of somatization, obsessive-compulsive, interpersonal sensibility, depression, anxiety, anger-hostility, phobic-anxiety, paranoid ideation, and psychoticism. The reliability of this tool has been reported to be more than 90% [31].
4) General Health Questionnaire (GHQ): This questionnaire has 28 questions and four subscales of somatic symptoms, anxiety and sleeplessness, social dysfunction, and severe depression and suicidal tendency. Each subscale has 7 questions, and each question is rated on a four-point scale (No, a little, much, very much). Five scores are obtained from this test, 4 of which are related to the subscales, and the other is the sum of the scores of the subscales. This instrument shows general health in 4 levels: none or the least, mild, moderate, and severe. This questionnaire has adequate validity and reliability and has a high predictive power in diagnosing positive and negative cases of psychological disorders [31].
Other variables examined in this study were: age, number of children, employment status, total percentage of veterans, percentage of neurological and mental illness, total hospitalization history during one year, and history of hospitalization in the psychiatric department.
Network indexes were calculated to get the importance of each variable in the network pattern of their relationships. In this study, five network indexes were calculated, which are strength value, closeness value, Benit value, eigenvector centrality value, and leverage value. The first index investigated in the network was the strength index, which refers to the strength of the direct connection of a node with other nodes. The closeness index shows which variables are closer to all variables on average. This index shows the degree of closeness of the variables. Benit index refers to the communication importance of a node and its role in the communication between different nodes. As its name suggests, Benit index shows the connectivity between different nodes. A node with a greater Benit is responsible for transmitting more information in the entire network. The eigenvector centrality index is used to measure the level of influence of a node in the network. Each of the nodes in the network that has a higher value of the eigenvector centrality, the level of their influence in the network is higher. The value of this index is related to the number of connections with other nodes, but it is more affected by the connections with more important nodes in the network. In other words, it is possible that a node in the network has a high degree score (which is solely dependent on the number of connections), but the value of its eigenvector is low. On the other hand, it is possible that the Benit value of a node that considers most of the communication of separate parts of the network is high, but because it is far from the power center of the network, it has a low eigenvector value. In fact, the value of the eigenvector of the node indicates the sphere of influence of the node in the network. The leverage centrality index is another new index in the field of network data analysis and considers the degree of a node in relation to its neighboring nodes. For example, if we consider a social network where person A is in contact with people who are not related to other people in the network (low level), the degree of leverage of this person will increase. A node with a high degree of leverage has a high control over the transmission of information to its neighboring nodes. A node with a negative centrality of leverage is affected by its neighboring nodes because although the nodes interact with them, they also interact with many other nodes, and the positive value of the centrality of leverage indicates that its neighboring nodes are less inclined to communicate with other nodes. Except Benit index, the score range of the indexes is between 0 and 1. The range of Benit index score is between 0 and -2N [20].
The variables were entered into the R software, and the relationship between them was determined based on the degree of correlation in the matrix, which is a two-dimensional space. In order to discover the relationship pattern between the variables and their internal relationship, this matrix was used as the input of the data relationship discovery algorithm. First, the values of the variables were standardized, and the standardized values were entered into the network analysis. To achieve the communication model based on network data analysis, first the distance matrix of the variables was calculated. The inverse value of this distance matrix was considered as the intensity of the relationship between the variables and was used as the input of the network data analysis, and then the network indices were calculated for each variable. Finally, the network pattern was drawn as a visual representation of the relationships between the variables.
Network data analysis was done using graph theory. qgraph software package with the aim of drawing the network of relationships and igraph in order to check the significance of network relationships were written under R language. Spearman's correlation was used to determine the intensity of correlation between both nodes (variables).
Findings
Data analysis was done based on the data bank of the Foundation of Martyrs and Veterans Affairs with 9244 samples. The demographic characteristics of the studied population are presented in Table 1.
Table 1) Demographic characteristics of the studied population (n=9244)
The indexes of the mental health network of veterans based on each variable are presented in Table 2. The first index examined was the strength index (the strength of a node's direct connection with other nodes). Age, number of children, percentage of veterans, percentage of neurological and mental disorders, physical functioning, bodily pain, and mental health were the variables that had the most strength. In addition, the age, number of children, and the percentage of neurological and mental disorders from the demographic characteristics and physical functioning, bodily pain, and mental health from the variables of the quality of life had the highest direct relationship with other variables of the mental health network of veterans.
Table 2) The indexes of the mental health network of veterans based on each variable
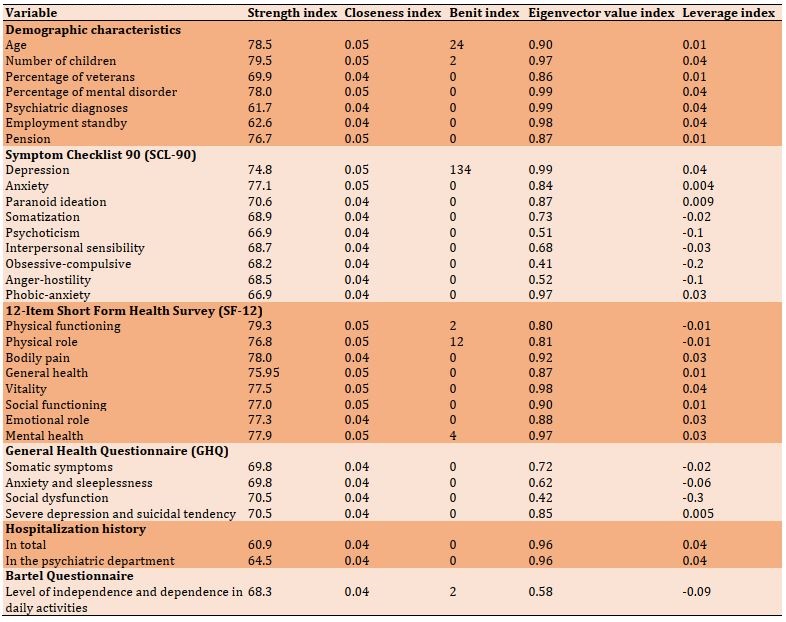
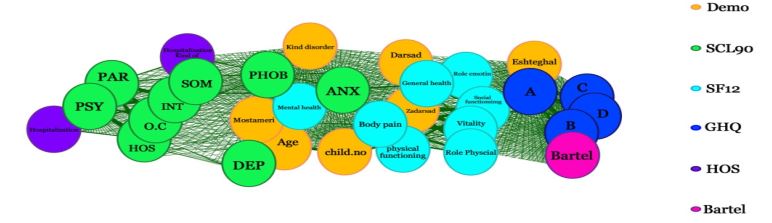
Figure 1) Mental health network in Iranian veterans
The second index examined was the closeness index. The closeness index value of all the variables that entered the model was between 0.04-0.05. All the variables whose closeness was 0.05 had more closeness than other variables. Age, number of children, pension, percentage of neurological and mental disorders, physical functioning, depression, anxiety, general health, physical role, physical functioning, social functioning, and vitality had the greatest value of closeness in the mental health network of veterans. In this index, all variables of SF-12 except for physical pain, variables of age and number of children from demographic characteristics, and anxiety and depression from the SCL-90 scale were closer than other network variables.
The Benit index in this study was between 0 and 134. The Benit value for the variables of depression, age, mental health, physical role, physical functioning, and the number of children in the mental health network of veterans was non-zero. The depression variable played the most important role in the communication path between two network nodes (134 times). After that, the two variables of age (24 times) and mental health (12 times) were in the way of the variables and had the biggest role in information transfer in the whole network. The value of the remaining variables was zero.
The eigenvector was the fourth most important index of the network. The value of the eigenvector in all variables except the obsessive-compulsive variable and social dysfunction was above 0.5. The variables of number of children, percentage of mental disorders, psychiatric diagnoses, especially depression, employment standby, physical problems, and vitality had the highest eigenvector values in the mental health network of veterans.
The fifth index of the network was the centrality of leverage, and its value was between -0.3 and 0.3. The variables of the number of children, the percentage of mental disorders, depression, vitality, history of hospitalization, and the type of hospitalization had higher values (positive) with the mental health network. On the other hand, the level of independence and dependence in daily activities and the variables of obsessive-compulsive, anger-hostility, interpersonal sensibility, and social dysfunction had less desire to communicate with other variables due to the centrality of negative leverage.
Figure 1 is the mental health network of Iranian veterans, which was obtained from the analysis of variables. In this figure, all the edges were drawn in the same color, meaning that the correlations were significantly positive. In addition, there was no significant negative correlation for any of the nodes. This figure shows that the overall shape of the network was intertwined (intertwining means the close relationship of the variables with each other), but some parts of the mental health variables of the veterans have a higher intertwining and are very closely related to each other and have formed a cluster in the network. The meaning of cluster is the accumulation of some variables together in one part of the network. Demographic variables, except employment, quality of life variables (SF-12), and variables of anxiety, depression, and phobia from SCL-90 had a very close relationship with each other and formed the central cluster of the network. On the other hand, the employment variable along with GHQ and Bartel variables formed another cluster on the right side of the network. On the left side, SCL-90 variables (except for depression, anxiety, and phobia, which were placed in the central cluster) formed another cluster with hospitalization history variables. In general, the network consists of three clusters.
Discussion
In this study, for the first time, we described and analyzed the mental health network of veterans based on national data with the amount of 9244 records. The results of this study have shown that the mental health network of veterans consists of various factors and has formed three clusters. The variables within each cluster have a high correlation, and none of the variables in the network have a negative correlation. In this network, all the variables are related to each other, but some of them have a significant role and contribution to this network. This result is in line with the opinion of Bratman et al., who state that various mutual factors can affect mental health, including social, economic, psychological, physiological, behavioral, environmental, genetic, and epigenetic influences [7].
As the indexes and the shape of the network show, the mental health network of veterans consists of a central cluster where the central variables gathered and two peripheral clusters. The cluster in the center of the network plays a very important role in the mental health of veterans. Peripheral variables play a lesser role in the network.
The high values of the network indicators in the variables of quality of life and their placement in the center show the importance of these variables as the main determinants in the mental health of veterans. As Liu et al. state: quality of life is one of the subsets of emotional well-being [32].
In the literature related to emotional well-being, it has been described in different ways, which includes positive and negative dimensions of emotions: the positive dimension of emotional well-being is such as happiness, passion, hope, and satisfaction, and its negative dimension is such as anger, anxiety, and depression [8]. The negative dimension of emotional well-being is visible in the mental health network of veterans in such a way that the variables of quality of life with anxiety and depression, phobia, type of psychiatric disorder and the percentage of veterans and the percentage of neurological and mental disorders are in the same cluster. These results are consistent with the findings of Khoravandi et al. [11]. Noorbala also states that depression and anxiety disorders have the highest disease burden among mental disorders [10].
The variables of age, number of children, pension, type of psychiatric disorder, percentage of veterans and percentage of neurological and mental disorders are also in the center of mental health network of veterans. The centrality of these variables shows their importance and effectiveness in the mental health of veterans. In this regard, Tavakol mentioned the age variable as one of the underlying variables of mental health in his research [33].
As it is clear on the right side of the network, three of the variables related to general health (anxiety and sleeplessness, social dysfunction, and severe depression) have a high correlation with the level of dependency in daily activities. These variables overlap closely with each other and can explain each other. Somatic symptoms, from general health components, have a high correlation with the employment standby of veterans separately. These variables formed the peripheral variables of the mental health network, which have a lesser role than the central variables in the mental health network. Wang et al. suggested that social welfare plays a fundamental role in achieving and maintaining mental health and in preventing and improving health problems [4]. Emotional support from the category social well-being refers to having close relationships with family and friends and feeling loved and cared for, having someone to trust and rely on in difficult life situations, and handling the demands of daily life such as going to appointments, shopping, helping in finance, paying bills, etc. Bjørlykhaug et al. state that social well-being is related to people's physical, functional, social, psychological, and emotional health [34]. They also consider the performance of daily tasks and the degree of dependence on others in the category of physical and social functions, which is consistent with the important role of these variables in the mental health network of veterans [34].
In the other part of the mental health network of veterans, which is closer to the central core of the network, the variables of percentage of veterans, general health, and percentage of mental disorder, bodily pain, and physical functioning are close to the central core. These variables also overlap with each other. Two of the variables of this category, namely physical functioning and bodily pain, have a high strength and correlation with the number of children. Baloglu et al. [8] consider anger, anxiety, and depression to be part of the negative dimensions of emotional well-being. In this study, the negative dimensions of emotional well-being in the mental health network of veterans are evident. Anxiety, sleeplessness, and depression as negative dimensions of emotional well-being are variables that have a significant contribution to the mental health network of veterans and are close to the central core.
On the left side of the mental health network, hospitalization history with paranoid variables and psychoticism showed a very strong correlation. These variables have a strong correlation with the type and history of hospitalization and factors such as anger-hostility, interpersonal sensibility, somatization, and obsessive-compulsive. In this regard, Mikaeili et al. state that the most veterans do not have a suitable adaptation situation in terms of emotional and social health [12]. Despite the close relationship between these variables, due to their location on the periphery of the network, they had a lesser role in the network than the central variables.
Strengths and weaknesses of the study
One of the strengths of this study was the use of the database of the Iranian veterans' information system. On the other hand, the survey was conducted in all veteran groups without considering the percentage or specific type of veterans. The advantage of this study compared to other studies that have been done so far was to address the mental health status of veterans with extensive data in the form of network analysis and model presentation. This study also had limitations and weaknesses, including the lack of similar studies for comparison. Another limitation was the lack of data related to other determinants of mental health, such as education, economic status, underlying diseases, and spiritual factor.
Suggestions
Considering the undeniable impact of mental health in daily life and its deep impact on other health sectors (social, physical and spiritual health), mental health custodians and policymakers in the Foundation of Martyrs and Veterans should pay serious attention to the determinants and factors affecting veterans' health. Therefore, based on the findings of this study, it is suggested to provide any services and support packages to increase the quality of life of veterans according to their age. It seems that they should avoid providing services in a one-dimensional way, and interventions should be provided systematically (providing a package of treatment, education, and support). Since other factors except those mentioned in the study can be effective in the mental health of veterans, it is recommended to include these factors in the comprehensive integrated information system of veterans. The inclusion of mental health questionnaires and other determinants in Sajaya and their completion by veterans can help to periodically monitor the mental health status of veterans.
Researchers are also suggested to consider other determinants of mental health in their investigations. It is also recommended to study the mental health status of veterans using data analysis in different groups of veterans.
Conclusion
The mental health model of Iranian veterans is an intertwined network of variables. Despite the intertwining of all variables, some variables are in the center of the network and have more influence in this network. The main determinants of mental health are variables related to the quality of life along with age, number of children, percentage of neurological and mental disorders, depression, and anxiety, which play a significant role in the mental health network of veterans.
Acknowledgements: We are grateful to all the people who helped in any way to make this work.
Ethical Permission: This study was approved by the Veterans Research Institute with the ethical code IR.ISAAR.REC.1401.007.
Conflict of Interests: There is no conflict of interest.
Authors’ Contribution: Lorestani F (First Author), Main Researcher (65%); Zarghami MH (Second Author), Methodologist/Discussion Writer (15%); Shatrian F (Third Author), Statistical Analyst (5%); Mosavi B (Fourth Author), Introduction Writer (15%)
Funding: The present article is taken from a doctoral thesis.
Keywords:
References
1. Watson D, Mowling C. Young minds and young bodies: Supportive teaching strategies for children with mental health concerns. Strategies. 2020;33(5):3-11. [Link] [DOI:10.1080/08924562.2020.1781005]
2. World Health Organization. The WHO special initiative for mental health (2019-2023): universal health coverage for mental health [Internet]. Geneva: World Health Organization; 2019 [cited 2020 July 15]. Available from: https://apps.who.int/iris/handle/10665/310981 [Link]
3. World Health Organization. Promoting mental health: concepts, emerging evidence, practice: summary report [Internet]. Geneva: World Health Organization; 2004 [cited 2019 July 15]. Available from: https://apps.who.int/iris/handle/10665/42940 [Link]
4. Wang J, Mann F, Lloyd-Evans, Ma R, Johnson S. Associations between loneliness and perceived social support and outcomes of mental health problems: a systematic review. BMC Psychiatry. 2018;18(1):156. [Link] [DOI:10.1186/s12888-018-1736-5]
5. Vaillant GE. Normality and mental health. In: Sadock B, Sadock V, Ruiz P, editors. Kaplan and Sadock's comprehensive textbook of psychiatry. 10th Edition. Philadelphia: Lippincott Williams & Wilkins; 2017. [Link]
6. Sen P, Crowley G, Arnell P, Katona C, Pillay M, Waterman LZ, et al. The UK's exportation of asylum obligations to Rwanda: A challenge to mental health, ethics and the law. Med Sci Law. 2022;62(3):165-7. [Link] [DOI:10.1177/00258024221104163]
7. Bratman GN, Anderson CB, Berman MG, Cochran B, de Vries S, Flanders J, et al. Nature and mental health: An ecosystem service perspective. Sci Adv. 2019;5(7):eaax0903. [Link] [DOI:10.1126/sciadv.aax0903]
8. Baloglu S, Busser J, Cain L. Impact of experience on emotional well-being and loyalty. J Hospital Market Manag. 2019;28(4):427-45. [Link] [DOI:10.1080/19368623.2019.1527269]
9. Bitsko RH, Claussen AH, Lichstein J, Black LI, Jones SE, Danielson ML, et al. Mental health surveillance among children - United States, 2013-2019. MMWR Suppl. 2022;71(2):1-42. [Link] [DOI:10.15585/mmwr.su7102a1]
10. Noorbala A, Namani F, Yahyvi J, Anvari S, Mahmodiazar M. The burden of mental disorders: a study of the Middle East countries during the period of 2000-2017. Sci Res J Med Syst. 2020;38(1):19-26. [Persian] [Link]
11. Khoravandi M, Mardani Rad M, Mashayekh M, Salmani Pour R. Relationship of early maladaptive schemas with religion orientation and matrimony conflicts of veterans with more than 25% disability rate in Tehran City. Iran J War Public Health. 2021;13(1):49-55. [Link]
12. Mikaeili N, Einy S, Taghavy R. Role of coping styles, locus of control, and emotional intelligence in predicting social adjustment of veterans with post-traumatic stress disorder.Iran J War Public Health. 2018;10(4):195-201. [Link] [DOI:10.29252/ijwph.10.4.195]
13. Kamalmanesh A, Maredpour A. Evaluation of post-traumatic stress disorder among war survivors. Health Res J. 2017;2(2):87-98. [Persian] [Link] [DOI:10.18869/acadpub.hrjbaq.2.2.87]
14. Abdoulmalk L, Amiri H, Hosseini SS, Amirpour B, Afshariniya K. The relationship and predicting role of sleep quality and sexual self-esteem in secondary post-traumatic stress disorder among wives of veterans. Milit Caring Sci. 2019;6(3):187-97. [Persian] [Link] [DOI:10.29252/mcs.6.3.4]
15. LayaRd R. The economics of mental health [Internet]. Germany: IZA World of Labor; 2017 [cited 2022 May 25]. Available from: https://wol.iza.org/articles/economics-of-mental-health/long [Link] [DOI:10.15185/izawol.321]
16. Richter D, Dixon J. Models of mental health problems: a quasi-systematic review of theoretical approaches. J Ment Health. 2023;32(2):396-406. [Link] [DOI:10.1080/09638237.2021.2022638]
17. Jilanchi M, Borjali M, Vatankhah HR, Mashayekh M, Zali AR. Identification of mental health model related to Iranian culture for the war veterans' spouses. Ebnesina 2021;23(1):15-24. [Persian] [Link]
18. Bohlmeijer E, Westerhof G. The model for sustainable mental health: future directions for integrating positive psychology into mental health care. Front Psychol. 2021;12:747999. [Link] [DOI:10.3389/fpsyg.2021.747999]
19. Borsboom D. Psychometric perspectives on diagnostic systems. J Clin Psychol. 2008 64(9):1089-108. [Link] [DOI:10.1002/jclp.20503]
20. Borsboom D, Cramer AOJ, Schmittmann VD, Epskamp S, Waldorp LJ. The small world of psychopathology. PLoS One. 2011;6(11):e27407. [Link] [DOI:10.1371/journal.pone.0027407]
21. Sadeghi Zamani F, Zarghami MH. Network data analysis application in family distance according to personality dimensions (NEO). Q Psychomet. 2018;7(25):83-99. [Persian] [Link]
22. Zarghmi MH, Delavar A, Falsafinejad MR, Dortaj F, Khoshsokhan M. Network data analysis application in coexistence studies. Educ Measur Quar. 2014;4(16):1-29. [Persian] [Link]
23. Borsboom D, Deserno MK, Rhemtulla M, Epskamp S, Fried EI, McNally R, et al. Network analysis of multivariate data in psychological science. Nat Rev Method Primers. 2021;1:58. [Link] [DOI:10.1038/s43586-021-00055-w]
24. Chen Y, Jin Q, Fang H, Lei H, Hu J, Wu Y, et al. Analytic network process: Academic insights and perspectives analysis. J Clean Product. 2019;235(16):1276-94. [Link] [DOI:10.1016/j.jclepro.2019.07.016]
25. Bastani S, Raissi M. Social network analysis method: using the whole networks approach in the study of open source communities. Iran J Soc Stud. 2011;5(2):31-57. [Persian] [Link]
26. Araghi L, Taheri A, Ramazani ZJ, Abbaspour A, Zarghmi MH. Network data analysis in the question analysis process. Q Educ Measur. 2017;7(28):207-40. [Persian] [Link]
27. Nasrollah Pourshirvnani SD, Mouodi S. Evidence-based policy making in the health system and its achievements and challenges in Iran. Babol: General Education Department of Baoul of Medical Science; 2013. [Persian] [Link]
28. Fried EI. Theories and models: What they are, what they are for, and what they are about. 2020. Psychol Inq. 2020;31(4):336-44. [Link] [DOI:10.1080/1047840X.2020.1854011]
29. Montazeri A, Vahdaninia M, Mousavi SJ, Omidvari S. The Iranian version of 12-item short form health survey (SF-12): factor structure, internal consistency and construct validity. BMC Public Health. 2009;9:341. [Link] [DOI:10.1186/1471-2458-9-341]
30. Tagharrobi Z, Sharifi K, Sooky Z. Psychometric evaluation of Shah Version of modified Barthel index in elderly people residing in Kashan Golabchi nursing home. Feyz 2011;15(3):213-24. [Persian] [Link]
31. Anisi J, Babaei S, Barani M, Mohammadlo H, Ebrahimi F. Determine the psychometric properties by Symptom Checklist-90-Revised (SCL-90-R) among military forces . Ebnesina 2016;17(4):13-18. [Persian] [Link]
32. Liu X, Ping S, Gao, W. Changes in undergraduate students' psychological well-being as they experience university life. Int J Environ Res Public Health. 2019;16(16):2864. [Link] [DOI:10.3390/ijerph16162864]
33. Tavakol M, Ekhlasi E, Rasoulinejad SP. Systematic review of studies on the determinants of mental health in Iranian society Exploration case: Internal scientific research articles 1399-1385. J Soc Work Res. 2020;7(23):1-46. [Link]
34. Bjørlykhaug KI, Karlsson B, Hesook SK, Kleppe LC. Social support and recovery from mental health problems: A scoping review. Nordic Soc Work Res. 2022;12(5):666-97. [Link] [DOI:10.1080/2156857X.2020.1868553]