Volume 14, Issue 4 (2022)
Iran J War Public Health 2022, 14(4): 425-431 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2022/08/12 | Accepted: 2022/11/13 | Published: 2022/11/29
Received: 2022/08/12 | Accepted: 2022/11/13 | Published: 2022/11/29
How to cite this article
Vozianov S, Shamraev S, Ridchenko M, Shamraeva D. Comparative Analysis of Immediate Results and Complications of Open Urethroplasty. Iran J War Public Health 2022; 14 (4) :425-431
URL: http://ijwph.ir/article-1-1264-en.html
URL: http://ijwph.ir/article-1-1264-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
1- Institute of Urology named of academician O. F. Vozianov, National Academy of Medical Sciences of Ukraine, Kyiv, Ukraine
2- 4th Urological Department, Institute of Urology named of academician O.F. Vozianov, National Academy of Medical Sciences of Ukraine, Kyiv, Ukraine
2- 4th Urological Department, Institute of Urology named of academician O.F. Vozianov, National Academy of Medical Sciences of Ukraine, Kyiv, Ukraine
Full-Text (HTML) (670 Views)
Introduction
It is believed that the leading cause of the development of traumatic Urethral Stricture (US) is the negative impact of urine on the tissues surrounding the urethra and the emerging infection. Damage (inflammation or trauma) triggers this multistep pathological process. According to research by various authors, pathogenetic development can take place in several directions:
1. Primary minor damage to the urethra → disruption of the mucous membrane → urinary cysts → microabscesses → proliferation → development of granulation tissue → stricture;
2. Primary significant injury of the urethra with its complete necrosis → urinary cysts → microabscesses → proliferation → development of granulation tissue → stricture/obliteration;
3. Stricture → bulging → repeated trauma to the urethra and urinary extravasation → progression of fibrotic processes [1, 2].
The study of the role of spongiofibrosis – the main process in the formation of strictures – allowed explaining the reasons for the ineffectiveness of urethral bogging and evaluating the results of Internal Optical Urethrotomy (IOUT), during which radical removal of sclerotized tissues of the urinary canal is not performed. The only pathogenetically determined method of treating urethral strictures is urethroplasty, in which the narrowing is excised within healthy tissues, while today, there is no universal surgical technique that will be the same for different types of strictures [3-7]. The biggest difficulty is the treatment of long strictures of the urethra. About 200 types of urethroplasty were proposed for surgical correction of this pathology by the end of the 20th century [8, 9]. Such a number of operative methods indicates insufficient effectiveness of most of them. Literary data indicate the absence of standards for diagnosis and treatment of this pathology. It has not been decided which plastic material is more favorable for the restoration of the urethra and the method of its fixation. Internal optical ureterotomy provides a long-term, recurrence-free result in only 10-35% of cases. Anastomotic urethroplasty is performed when the length of strictures/obliterations does not exceed 2 cm with an efficiency of 65.2-73.1% over 5 years [10].
The fate of patients with post-traumatic distract defects of the urethra (that is, its obliteration) is extremely difficult conditioned upon the 40-50% probability of recurrence. At the same time, in 2.5-3.6% of patients, lifelong epicystostomy or perineal urethrostomy with female-type urination is imposed, which significantly worsens the quality of life of patients [11-13]. In recent years, a number of effective urethroplasty has been proposed, which increase the lumen of the urethra conditioned upon free and displaced flaps and grafts. Since 2003, the "Institute of Urology of the National Academy of Medical Sciences of Ukraine" has been registering the examination and treatment of patients with urinary tract strictures/obliterations of various etiologies and complexity. In 2003-2019, 1301 surgical interventions were performed for US. In 147 cases, patients underwent various types of open urethroplasty.
The present study aimed to evaluate and analyze the postoperative complications in patients with open urethroplasty.
Instrument and Methods
In this study, the clinical data of the medical histories of 147 patients with long urethral strictures and obliterations were retrospectively evaluated. All patients were male and between 13 and 85 years old. The observation lasted from 6 to 18 months in 2020-2022.
The patients were examined under the accepted standards of providing urological care [14-16]. The localization and length of the stricture and the degree of spongiofibrosis were evaluated according to the results of ultrasonography and retrograde or micturition urethrocystography (in some patients according to the data of spiral computed tomography, SCT) in angiomode. All patients were examined according to the scheme that is shown in Figure 1.

Figure 1) Patient examination algorithm (Abbreviation: IPSS, International Prostate Symptom Score; US, Urethral Stricture)
Regarding the types of surgical operations, patients were divided into 3 groups:
• Group I) Buccal Urethral Plastic surgery (BUP)
• Group II) Urethra-Urethra- or urethra-prostate Anastomosis (UUA)
• Group III) Plastic replacement with a Skin-Fascial Flap (PSFF)
The choice of anesthesiological support was determined based on the duration, scope of operations, and the degree of surgical risk according to Charlson's comorbidity index with points of 0, 1, 2, and more than 2 [17]. In the postoperative period, antibiotics were prescribed (depending on the urine culture data), and antioxidant and angiotropic therapy was carried out. In the case of recurrent US, physiotherapy was added to pharmacotherapy for three months.
Thus, based on a combination of factors that determine the characteristics of the course of the therapy process, it is possible to identify key points of contact between characteristic features for further analysis within the framework of the study. The result of this is the definition of complications that were evaluated according to the Clavien-Dindo scale, which since 2004 has been a standard for communication between surgical doctors [17, 18]. When perusing the publication devoted to the 5-year experience of using the Clavien-Dindo classification, it was found that most authors additionally introduce the concepts of "small" and "major" complications: I and II are classified as minor, and III-V classes are classified as major. When evaluating postoperative complications, we also used this division.
To separate patients according to the complexity of urethral strictures/obliterations, the length, localization, number of strictures, etiology, recurrence, and severity of spongiofibrosis were comprehensively evaluated. Strictures/obliterations were divided into low complexity (from 1 to 3 points), medium complexity (from 4 to 6 points), and complex US (from 7 to 10 points) [19].
The difference between the mean values was analyzed using the student t-test. P<0.05 was considered the significant level.
Findings
The mean age of patients was 42.3±1.8 years, and the mean observation duration was 16.8±2.2 months.
In the preoperative period, the disease duration (from the onset of symptoms to hospitalization) was up to 1 year in 45 patients, 1-2 years in 20 patients, 2-4 years in 21 patients, and more than 4 years in 61 patients. Correction of strictures and obliterations of the urethra in the form of reconstructive operations (UUA, PSFF, and BUP) was found in 35 (23.8%) patients. Internal optical urethrotomy was performed in 88 patients (59.9%). Accordingly, strictures and obliterations that were already amenable to surgical treatment were considered recurrent and accounted for 123 cases (83.7%). The degree of urinary tract symptoms was low in 5 patients (3.4%), moderate in 8 patients (5.4%), and severe in 20 patients (13.6%). Another 114 patients (77.5%) were admitted to the clinic with epicystostomy drainage.
70 patients (47.6%) were placed in group I (BUP), 65 patients (44.2%) in group II (UUA), and 12 patients (8.2%) in group III (PSFF).
All operations were performed in the typical lithotomy position of the patient under epidural anesthesia in 45 patients (30.6%) and total IV anesthesia with endotracheal intubation in 102 patients (69.4%). Charlson's comorbidity index was 0 for 52 patients (35.4%), 1 point for 52 patients (35.4%), 2 points for 24 patients (16.3%), and more than 2 points for 19 patients (12.9%).
To evaluate the results and postoperative complications of surgical corrections of urethral strictures and obliterations, all patients were divided into 3 groups, including group I: patients without complications or with class I complications (n=98, 66.7%), group II: patients with class II-IIIa postoperative complications according to the Clavien-Dindo classification (n=30, 20.4%), and group III: men with class IIIb-IV complications (n=28, 19.0%). There were no complications after Class V Clavien-Dindo surgery. If you add up the number of all patients in groups 1, 2, and 3, the sum of patients will be greater than 147. It can be explained by the fact that some patients underwent internal optical urethrotomy in the remote postoperative period, but the improvement after this operation was not long-lasting and in the subsequent patients repeated urethroplasty was performed. A comparison of all three groups by reason, localization, length, and type of primary surgical correction is presented in Table 1.
More than 50% of patients in both groups had functional epicystostomy drainage: in the first group 46 patients (92.0%), and the second group 58 patients (59.8%). To the increase in the complexity of surgical treatment methods, the average operation time increased from 155.3±9.0 minutes in the first group, up to 170.4±6.6 minutes in another group, and blood loss from 93.0±6.8 ml to 155.0±7.6 ml, respectively. In the first group, the average time of urethral catheterization in the postoperative period was 19.9±0.7 days, and in the other group, it was 19.2±0.7 days, which was not significantly different. The postoperative bed-day was significantly shorter in the second group (10.4±0.5 days) compared to the first group (21.3±1.2 days).
According to the type of surgical treatment in the first group, the majority of patients performed urethral-urethral or urethral-prostatic anastomosis (n=42, 84.0%). Plastic skin-fascial flap and buccal urethral plastic surgery were performed for 8 patients (16.0%). In the second group, there were changes in the number of buccal urethral plastic surgery (n=69, 71.1%), which
made up the majority. UUA was performed in 23 patients (23.7%), and PSFF was performed in 8 cases (8.2%).
Table 1) Comparative assessment of patients according to the level of postoperative complications
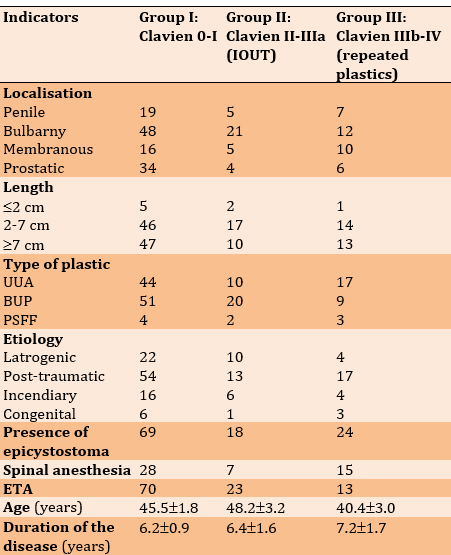

According to the etiology, the patients of group 1 had post-traumatic strictures in 54 patients (55.1%), iatrogenic strictures in 22 patients (22.4%), post-inflammatory US in 16 patients (16.3%), and congenital urethral defects in 6 patients (6.1%). In group 2, iatrogenic strictures accounted for 33.3%, and post-traumatic strictures for 43.3%. Post-inflammatory and congenital strictures in the second group of patients were much smaller, 6 (20%) and 1 (3.3%), respectively. There were 17 (60.7%) patients in the third group with post-traumatic urethral strictures/obliterations, 4 patients (14.3%) each had iatrogenic and post-inflammatory urinary US, and only 3 patients (10.7%) of this group had congenital ones. When comparing the number of patients according to the etiology of all three groups, post-traumatic strictures accounted for a significantly greater number at 58.7%, followed by iatrogenic US at 25.2%.
In group I, according to the type of surgical treatment, the majority of patients was divided into UUA (n=44, 62.0%) and BUP (n=51, 63.8%) among all patients who underwent surgical interventions. There were 4 patients (44.4%) in group I after PSFF. There were more patients in group II with complications of II-IIIa classes after BUP (n= 20, 25.0%). IOUT after UUA was performed in 10 cases (14.1%), and after PSFF in 2 (22.2%). Repeated urethroplasty was more often performed in patients with a history of UUA in 17 patients (23.9%). There were 9 patients (11.2%) in group III after BUP and 3 patients (33.3%) after PSFF.
The average age was significantly lower in patients of group III (40.4±3.0 years), but the average duration of the disease in this group was longer compared to the other groups (7.2±1.7 years). In groups, I and II, the average age and duration of the disease did not differ significantly. Most patients had OU: 70.4% of patients in group I, 60.0% in group II, and 85.7% in group III. In groups II and III, the average length of strictures/obliterations of the urethra did not differ significantly and was 6.1±0.8 and 6.9±0.6 cm, respectively. And in group I, the average length of the stricture was significantly smaller compared to the other groups and was 4.2±0.3 cm. When evaluating the scores of the complexity of the US, the highest score was found in group III (8.6±0.3). In group II, it was slightly smaller (8.3±0.3). In group I, the US complexity score was significantly lower (7.0±0.2), which indicates that in the study, most of the urethral strictures were complex.
The time of urethral drainage was 12-32 days. Of these, the catheter was removed in 53 patients (36.1%), within 15-20 days in 67 patients (45.6%), and more than 20 days (20-32 days) in 27 patients (18.4%). The average time of urethral drainage in group I was 19.3±0.7 days, in group II 22.0±1.5 days, and in group III 18.0±0.9 days.
The average bed-day was higher in groups I (8.9±1.2 days) and III (14.3±1.5 days), and in group II (11.4±1.2 days) was significantly smaller than all the studied groups. When comparing the average drainage time of postoperative wounds, it was 3.7±0.3 days compared to 4.3±0.3 days in group I and 1.3±0.3 days in group III. When analyzing the results of the operations of 147 patients, one can pay attention to an increase in the number of replacement and augmentation buccal plastics over the years from 4 to 69 and a decrease in the number of Urethra-Urethra and Urethra-prostate anastomoses from 42 to 23.
For a more detailed study of the results of surgical corrections of long strictures and obliterations of the urethra, depending on the year it was performed at the Institute of Urology of the National Academy of Medical Sciences of Ukraine, patients were divided into two groups. The first group consisted of 50 patients (34.0%) who were operated on from 2000 to 2014, and the second group consisted of 97 patients (66.0%) operated on from 2015 to 2020 (Table 2).
Table 2) Comparative evaluation of the results of surgical corrections of US depending on the years of its implementation
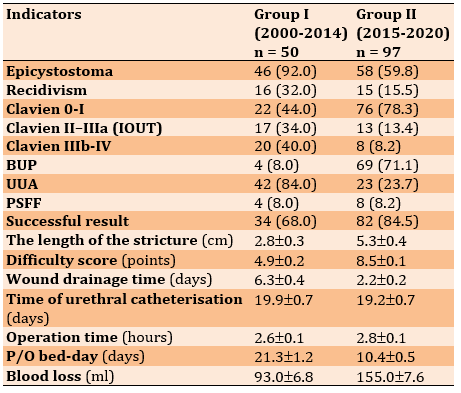
An assessment and comparison of postoperative complications between the two groups were carried out: In 44.0% of patients in the first group, the p/o period proceeded without complications or with postoperative complications of class I, and in the second group, this indicator was 78.3%. Class II-IIIa complications, according to Clavien-Dindo and conducting IOUT in the distant p/o period, as a method of treatment of relapse were observed in 17 patients of the first group (34.0%). This indicator was 13 (13.4%) in the second group, which indicates a decrease in the number of this type of postoperative complications from the accumulation of experience.
Recurrences of urethral strictures and obliterations that required repeated urethroplasty were observed in 20 patients (40.0%) of the first group and 8 patients (8.2%) of another group. This is evidenced by the lower percentage of repeated operations in the second group. The successful outcome of treatment was observed in 34 patients (68.0%) of the first group and in 82 patients (84.5%) of the second group. There were 16 patients (32%) in the first group and 15 (15.5%) in the second group who underwent repeated urethroplasty in the separated postoperative period as a result of failure of the primary treatment.
Discussion
According to our results, when comparing the number of patients according to the etiology of all three groups, post-traumatic strictures accounted for a significantly greater number at 58.7%, followed by iatrogenic US at 25.2%. The pathogenesis of these two etiologies is the same because iatrogenia is an injury to the urethra caused by the actions of medical personnel [20].
The time of urethral drainage was 12-32 days. Of these, the catheter was removed in 53 patients (36.1%), within 15-20 days in 67 patients (45.6%), and more than 20 days (20-32 days) in 27 patients (18.4%). The average time of urethral drainage in group I was 19.3±0.7 days, in group II 22.0±1.5 days, and in group III 18.0±0.9 days, which is consistent with other studies [21-25].
The average bed-day was higher in groups I (8.9±1.2 days) and III (14.3±1.5 days), and in group II (11.4±1.2 days) was significantly smaller than all the studied groups. When comparing the average drainage time of postoperative wounds, it was 3.7±0.3 days compared to 4.3±0.3 days in group I and 1.3±0.3 days in group III. When analyzing the results of the operations of 147 patients, one can pay attention to an increase in the number of replacement and augmentation buccal plastics over the years from 4 to 69 and a decrease in the number of Urethra-Urethra and Urethra-prostate anastomoses from 42 to 23, which also is consistent with other studies [26, 27].
It is important during the patient's initial request for medical help to conduct a maximum examination to choose a rational method of surgical treatment, according to modern standards, with a minimal probability of recurrence. The main methods of surgical treatment of long urethral strictures and obliterations are Urethra-Urethral, Urethra -prostatic, or Urethra-vesico Anastomosis (UUA), buccal Urethral Plasty (BUP), and Plasty with a Skin-Fascial Flap (PSFF).
Despite the active study of research and methods of treatment of patients with strictures and obliterations of the urethra (OU) in the world and own experience of treating more than 1300 patients with various types and lengths of strictures and obliterations of the urethra, the occurrence of early and late postoperative complications and recurrences after surgical treatment was not avoided [13, 14, 28-30].
In clinical practice, internal urethrotomy is a simple procedure and is recommended as first-line treatment for short urethral strictures, Mazdak et al. say [10]. Internal urethrotomy refers to any procedure that exposes the stricture by cutting it or removing it transurethrally. The most common complication of internal urethrotomy is recurrence of the stricture. The success rate of treatment with internal urethrotomy is approximately 20%. Injection of triamcinolone significantly reduced recurrence of stenosis after internal urethrotomy [31, 32]. More research is needed to confirm its effectiveness and safety.
According to Sheehan et al. [15], urethral strictures have various etiologies, most often iatrogenic or inflammatory in the anterior urethra and iatrogenic/surgical or traumatic in the posterior urethra. Diagnosis and treatment planning depend on urethrography, which is usually performed with a combination of retrograde urethrography and ureteral cystourethrography to assess the anterior and posterior urethra, respectively. Although this is most often performed under fluoroscopy, ultrasound urethrography is an alternative, although at the expense of the posterior urethra, it is only visualized using a transrectal approach [33-36].
In addition to understanding urethral anatomy, familiarity with normal periurethral structures is essential to avoid misdiagnoses, such as Cowper's ducts, Littre's glands, prostate, and ejaculatory ducts. Surgical treatment depends on the location, length, and the number of strictures, and options range from balloon dilation to endoscopic urethrotomy to anastomosis and replacement urethrotomy. Postoperative management includes urethrography to detect potential complications, including urethral leakage, graft failure, and recurrence of the stricture [37, 38].
Pompeo et al. [24] noted that penile cancer is a devastating disease that is usually diagnosed late, requiring extensive resections, causing changes in self-esteem and body image, affecting sexual and urinary functions, and impairing the quality of life. They determined that penile-conserving surgery should only be indicated for superficial penile cancer and isolated invasive lesions. Applicants for PSS must adhere to follow-up requirements that allow for early detection of local recurrences [39]. Quick and efficient rescue procedures are imperative in such situations.
Pfalzgraf et al. [26] studied the indications, the operative technique, and the results of two-stage urethroplasty of the oral mucosa (BM) and the mesh graft for the treatment of urethral strictures. Long strictures with severe spongiform fibrosis are an indication of a two-stage urethroplasty (BM and mesh graft). Excellent results can be achieved with both techniques with similar complication rates. The mesh graft technique remains the last option for a complex group of patients.
Barbagli et al. [27] conclude that the surgical treatment of bulbar urethral strictures remains one of the most difficult problems in reconstructive surgery. Urethral strictures are generally classified as traumatic and non-traumatic, depending on the etiology. Traumatic strictures are caused by trauma and define a tear in the urethra with obliteration of the urethral lumen, ending in fibrous fissures between the ends of the urethra. Traumatic obliteration of strictures requires cross-sectioning of the urethra to completely remove the fibrous tissue covering the ends of the urethra [40]. In contrast, nontraumatic and unobstructed urethral strictures require augmentation of the urethral plate with oral mucosa grafts. Nowadays, it is still difficult to choose the right surgical intervention to repair the stenosis of the eyeball without obliteration.
Conclusion
During the patient's initial request for medical help, it is important to conduct a maximum examination to choose a rational method of surgical treatment, according to modern standards, with a minimum probability of recurrence. However, early and late postoperative complications and recurrence after surgical treatment are not prevented.
Acknowledgments: None declared.
Ethical Permissions: For this type of study, the approval of the ethics committee is not required in the country where the study was conducted.
Conflicts of Interests: The authors declare no conflict of interests.
Authors’ Contribution: Vozianov S (First Author), Introduction Writer/Main Researcher (25%); Shamraev S (Second Author), Methodologist/Statistical Analyst (25%); Ridchenko M (Third Author), Discussion Writer/Data Analyst (25%); Shamraeva D (Forth Author), Assistant Researcher/Discussion Writer (25%)
Funding/Support: None declared.A
It is believed that the leading cause of the development of traumatic Urethral Stricture (US) is the negative impact of urine on the tissues surrounding the urethra and the emerging infection. Damage (inflammation or trauma) triggers this multistep pathological process. According to research by various authors, pathogenetic development can take place in several directions:
1. Primary minor damage to the urethra → disruption of the mucous membrane → urinary cysts → microabscesses → proliferation → development of granulation tissue → stricture;
2. Primary significant injury of the urethra with its complete necrosis → urinary cysts → microabscesses → proliferation → development of granulation tissue → stricture/obliteration;
3. Stricture → bulging → repeated trauma to the urethra and urinary extravasation → progression of fibrotic processes [1, 2].
The study of the role of spongiofibrosis – the main process in the formation of strictures – allowed explaining the reasons for the ineffectiveness of urethral bogging and evaluating the results of Internal Optical Urethrotomy (IOUT), during which radical removal of sclerotized tissues of the urinary canal is not performed. The only pathogenetically determined method of treating urethral strictures is urethroplasty, in which the narrowing is excised within healthy tissues, while today, there is no universal surgical technique that will be the same for different types of strictures [3-7]. The biggest difficulty is the treatment of long strictures of the urethra. About 200 types of urethroplasty were proposed for surgical correction of this pathology by the end of the 20th century [8, 9]. Such a number of operative methods indicates insufficient effectiveness of most of them. Literary data indicate the absence of standards for diagnosis and treatment of this pathology. It has not been decided which plastic material is more favorable for the restoration of the urethra and the method of its fixation. Internal optical ureterotomy provides a long-term, recurrence-free result in only 10-35% of cases. Anastomotic urethroplasty is performed when the length of strictures/obliterations does not exceed 2 cm with an efficiency of 65.2-73.1% over 5 years [10].
The fate of patients with post-traumatic distract defects of the urethra (that is, its obliteration) is extremely difficult conditioned upon the 40-50% probability of recurrence. At the same time, in 2.5-3.6% of patients, lifelong epicystostomy or perineal urethrostomy with female-type urination is imposed, which significantly worsens the quality of life of patients [11-13]. In recent years, a number of effective urethroplasty has been proposed, which increase the lumen of the urethra conditioned upon free and displaced flaps and grafts. Since 2003, the "Institute of Urology of the National Academy of Medical Sciences of Ukraine" has been registering the examination and treatment of patients with urinary tract strictures/obliterations of various etiologies and complexity. In 2003-2019, 1301 surgical interventions were performed for US. In 147 cases, patients underwent various types of open urethroplasty.
The present study aimed to evaluate and analyze the postoperative complications in patients with open urethroplasty.
Instrument and Methods
In this study, the clinical data of the medical histories of 147 patients with long urethral strictures and obliterations were retrospectively evaluated. All patients were male and between 13 and 85 years old. The observation lasted from 6 to 18 months in 2020-2022.
The patients were examined under the accepted standards of providing urological care [14-16]. The localization and length of the stricture and the degree of spongiofibrosis were evaluated according to the results of ultrasonography and retrograde or micturition urethrocystography (in some patients according to the data of spiral computed tomography, SCT) in angiomode. All patients were examined according to the scheme that is shown in Figure 1.

Figure 1) Patient examination algorithm (Abbreviation: IPSS, International Prostate Symptom Score; US, Urethral Stricture)
Regarding the types of surgical operations, patients were divided into 3 groups:
• Group I) Buccal Urethral Plastic surgery (BUP)
• Group II) Urethra-Urethra- or urethra-prostate Anastomosis (UUA)
• Group III) Plastic replacement with a Skin-Fascial Flap (PSFF)
The choice of anesthesiological support was determined based on the duration, scope of operations, and the degree of surgical risk according to Charlson's comorbidity index with points of 0, 1, 2, and more than 2 [17]. In the postoperative period, antibiotics were prescribed (depending on the urine culture data), and antioxidant and angiotropic therapy was carried out. In the case of recurrent US, physiotherapy was added to pharmacotherapy for three months.
Thus, based on a combination of factors that determine the characteristics of the course of the therapy process, it is possible to identify key points of contact between characteristic features for further analysis within the framework of the study. The result of this is the definition of complications that were evaluated according to the Clavien-Dindo scale, which since 2004 has been a standard for communication between surgical doctors [17, 18]. When perusing the publication devoted to the 5-year experience of using the Clavien-Dindo classification, it was found that most authors additionally introduce the concepts of "small" and "major" complications: I and II are classified as minor, and III-V classes are classified as major. When evaluating postoperative complications, we also used this division.
To separate patients according to the complexity of urethral strictures/obliterations, the length, localization, number of strictures, etiology, recurrence, and severity of spongiofibrosis were comprehensively evaluated. Strictures/obliterations were divided into low complexity (from 1 to 3 points), medium complexity (from 4 to 6 points), and complex US (from 7 to 10 points) [19].
The difference between the mean values was analyzed using the student t-test. P<0.05 was considered the significant level.
Findings
The mean age of patients was 42.3±1.8 years, and the mean observation duration was 16.8±2.2 months.
In the preoperative period, the disease duration (from the onset of symptoms to hospitalization) was up to 1 year in 45 patients, 1-2 years in 20 patients, 2-4 years in 21 patients, and more than 4 years in 61 patients. Correction of strictures and obliterations of the urethra in the form of reconstructive operations (UUA, PSFF, and BUP) was found in 35 (23.8%) patients. Internal optical urethrotomy was performed in 88 patients (59.9%). Accordingly, strictures and obliterations that were already amenable to surgical treatment were considered recurrent and accounted for 123 cases (83.7%). The degree of urinary tract symptoms was low in 5 patients (3.4%), moderate in 8 patients (5.4%), and severe in 20 patients (13.6%). Another 114 patients (77.5%) were admitted to the clinic with epicystostomy drainage.
70 patients (47.6%) were placed in group I (BUP), 65 patients (44.2%) in group II (UUA), and 12 patients (8.2%) in group III (PSFF).
All operations were performed in the typical lithotomy position of the patient under epidural anesthesia in 45 patients (30.6%) and total IV anesthesia with endotracheal intubation in 102 patients (69.4%). Charlson's comorbidity index was 0 for 52 patients (35.4%), 1 point for 52 patients (35.4%), 2 points for 24 patients (16.3%), and more than 2 points for 19 patients (12.9%).
To evaluate the results and postoperative complications of surgical corrections of urethral strictures and obliterations, all patients were divided into 3 groups, including group I: patients without complications or with class I complications (n=98, 66.7%), group II: patients with class II-IIIa postoperative complications according to the Clavien-Dindo classification (n=30, 20.4%), and group III: men with class IIIb-IV complications (n=28, 19.0%). There were no complications after Class V Clavien-Dindo surgery. If you add up the number of all patients in groups 1, 2, and 3, the sum of patients will be greater than 147. It can be explained by the fact that some patients underwent internal optical urethrotomy in the remote postoperative period, but the improvement after this operation was not long-lasting and in the subsequent patients repeated urethroplasty was performed. A comparison of all three groups by reason, localization, length, and type of primary surgical correction is presented in Table 1.
More than 50% of patients in both groups had functional epicystostomy drainage: in the first group 46 patients (92.0%), and the second group 58 patients (59.8%). To the increase in the complexity of surgical treatment methods, the average operation time increased from 155.3±9.0 minutes in the first group, up to 170.4±6.6 minutes in another group, and blood loss from 93.0±6.8 ml to 155.0±7.6 ml, respectively. In the first group, the average time of urethral catheterization in the postoperative period was 19.9±0.7 days, and in the other group, it was 19.2±0.7 days, which was not significantly different. The postoperative bed-day was significantly shorter in the second group (10.4±0.5 days) compared to the first group (21.3±1.2 days).
According to the type of surgical treatment in the first group, the majority of patients performed urethral-urethral or urethral-prostatic anastomosis (n=42, 84.0%). Plastic skin-fascial flap and buccal urethral plastic surgery were performed for 8 patients (16.0%). In the second group, there were changes in the number of buccal urethral plastic surgery (n=69, 71.1%), which
made up the majority. UUA was performed in 23 patients (23.7%), and PSFF was performed in 8 cases (8.2%).
Table 1) Comparative assessment of patients according to the level of postoperative complications
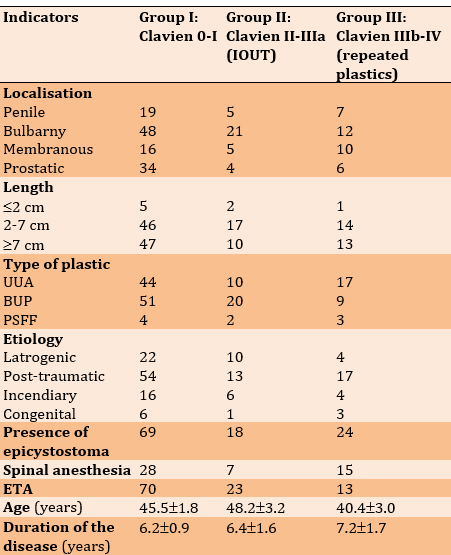

According to the etiology, the patients of group 1 had post-traumatic strictures in 54 patients (55.1%), iatrogenic strictures in 22 patients (22.4%), post-inflammatory US in 16 patients (16.3%), and congenital urethral defects in 6 patients (6.1%). In group 2, iatrogenic strictures accounted for 33.3%, and post-traumatic strictures for 43.3%. Post-inflammatory and congenital strictures in the second group of patients were much smaller, 6 (20%) and 1 (3.3%), respectively. There were 17 (60.7%) patients in the third group with post-traumatic urethral strictures/obliterations, 4 patients (14.3%) each had iatrogenic and post-inflammatory urinary US, and only 3 patients (10.7%) of this group had congenital ones. When comparing the number of patients according to the etiology of all three groups, post-traumatic strictures accounted for a significantly greater number at 58.7%, followed by iatrogenic US at 25.2%.
In group I, according to the type of surgical treatment, the majority of patients was divided into UUA (n=44, 62.0%) and BUP (n=51, 63.8%) among all patients who underwent surgical interventions. There were 4 patients (44.4%) in group I after PSFF. There were more patients in group II with complications of II-IIIa classes after BUP (n= 20, 25.0%). IOUT after UUA was performed in 10 cases (14.1%), and after PSFF in 2 (22.2%). Repeated urethroplasty was more often performed in patients with a history of UUA in 17 patients (23.9%). There were 9 patients (11.2%) in group III after BUP and 3 patients (33.3%) after PSFF.
The average age was significantly lower in patients of group III (40.4±3.0 years), but the average duration of the disease in this group was longer compared to the other groups (7.2±1.7 years). In groups, I and II, the average age and duration of the disease did not differ significantly. Most patients had OU: 70.4% of patients in group I, 60.0% in group II, and 85.7% in group III. In groups II and III, the average length of strictures/obliterations of the urethra did not differ significantly and was 6.1±0.8 and 6.9±0.6 cm, respectively. And in group I, the average length of the stricture was significantly smaller compared to the other groups and was 4.2±0.3 cm. When evaluating the scores of the complexity of the US, the highest score was found in group III (8.6±0.3). In group II, it was slightly smaller (8.3±0.3). In group I, the US complexity score was significantly lower (7.0±0.2), which indicates that in the study, most of the urethral strictures were complex.
The time of urethral drainage was 12-32 days. Of these, the catheter was removed in 53 patients (36.1%), within 15-20 days in 67 patients (45.6%), and more than 20 days (20-32 days) in 27 patients (18.4%). The average time of urethral drainage in group I was 19.3±0.7 days, in group II 22.0±1.5 days, and in group III 18.0±0.9 days.
The average bed-day was higher in groups I (8.9±1.2 days) and III (14.3±1.5 days), and in group II (11.4±1.2 days) was significantly smaller than all the studied groups. When comparing the average drainage time of postoperative wounds, it was 3.7±0.3 days compared to 4.3±0.3 days in group I and 1.3±0.3 days in group III. When analyzing the results of the operations of 147 patients, one can pay attention to an increase in the number of replacement and augmentation buccal plastics over the years from 4 to 69 and a decrease in the number of Urethra-Urethra and Urethra-prostate anastomoses from 42 to 23.
For a more detailed study of the results of surgical corrections of long strictures and obliterations of the urethra, depending on the year it was performed at the Institute of Urology of the National Academy of Medical Sciences of Ukraine, patients were divided into two groups. The first group consisted of 50 patients (34.0%) who were operated on from 2000 to 2014, and the second group consisted of 97 patients (66.0%) operated on from 2015 to 2020 (Table 2).
Table 2) Comparative evaluation of the results of surgical corrections of US depending on the years of its implementation
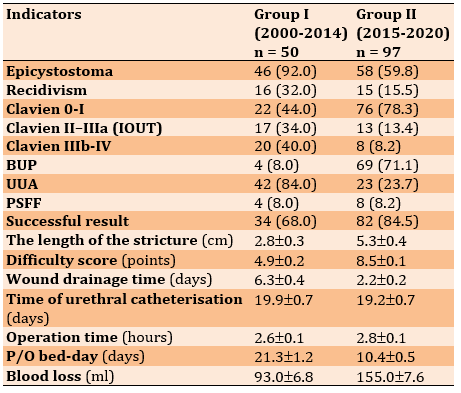
An assessment and comparison of postoperative complications between the two groups were carried out: In 44.0% of patients in the first group, the p/o period proceeded without complications or with postoperative complications of class I, and in the second group, this indicator was 78.3%. Class II-IIIa complications, according to Clavien-Dindo and conducting IOUT in the distant p/o period, as a method of treatment of relapse were observed in 17 patients of the first group (34.0%). This indicator was 13 (13.4%) in the second group, which indicates a decrease in the number of this type of postoperative complications from the accumulation of experience.
Recurrences of urethral strictures and obliterations that required repeated urethroplasty were observed in 20 patients (40.0%) of the first group and 8 patients (8.2%) of another group. This is evidenced by the lower percentage of repeated operations in the second group. The successful outcome of treatment was observed in 34 patients (68.0%) of the first group and in 82 patients (84.5%) of the second group. There were 16 patients (32%) in the first group and 15 (15.5%) in the second group who underwent repeated urethroplasty in the separated postoperative period as a result of failure of the primary treatment.
Discussion
According to our results, when comparing the number of patients according to the etiology of all three groups, post-traumatic strictures accounted for a significantly greater number at 58.7%, followed by iatrogenic US at 25.2%. The pathogenesis of these two etiologies is the same because iatrogenia is an injury to the urethra caused by the actions of medical personnel [20].
The time of urethral drainage was 12-32 days. Of these, the catheter was removed in 53 patients (36.1%), within 15-20 days in 67 patients (45.6%), and more than 20 days (20-32 days) in 27 patients (18.4%). The average time of urethral drainage in group I was 19.3±0.7 days, in group II 22.0±1.5 days, and in group III 18.0±0.9 days, which is consistent with other studies [21-25].
The average bed-day was higher in groups I (8.9±1.2 days) and III (14.3±1.5 days), and in group II (11.4±1.2 days) was significantly smaller than all the studied groups. When comparing the average drainage time of postoperative wounds, it was 3.7±0.3 days compared to 4.3±0.3 days in group I and 1.3±0.3 days in group III. When analyzing the results of the operations of 147 patients, one can pay attention to an increase in the number of replacement and augmentation buccal plastics over the years from 4 to 69 and a decrease in the number of Urethra-Urethra and Urethra-prostate anastomoses from 42 to 23, which also is consistent with other studies [26, 27].
It is important during the patient's initial request for medical help to conduct a maximum examination to choose a rational method of surgical treatment, according to modern standards, with a minimal probability of recurrence. The main methods of surgical treatment of long urethral strictures and obliterations are Urethra-Urethral, Urethra -prostatic, or Urethra-vesico Anastomosis (UUA), buccal Urethral Plasty (BUP), and Plasty with a Skin-Fascial Flap (PSFF).
Despite the active study of research and methods of treatment of patients with strictures and obliterations of the urethra (OU) in the world and own experience of treating more than 1300 patients with various types and lengths of strictures and obliterations of the urethra, the occurrence of early and late postoperative complications and recurrences after surgical treatment was not avoided [13, 14, 28-30].
In clinical practice, internal urethrotomy is a simple procedure and is recommended as first-line treatment for short urethral strictures, Mazdak et al. say [10]. Internal urethrotomy refers to any procedure that exposes the stricture by cutting it or removing it transurethrally. The most common complication of internal urethrotomy is recurrence of the stricture. The success rate of treatment with internal urethrotomy is approximately 20%. Injection of triamcinolone significantly reduced recurrence of stenosis after internal urethrotomy [31, 32]. More research is needed to confirm its effectiveness and safety.
According to Sheehan et al. [15], urethral strictures have various etiologies, most often iatrogenic or inflammatory in the anterior urethra and iatrogenic/surgical or traumatic in the posterior urethra. Diagnosis and treatment planning depend on urethrography, which is usually performed with a combination of retrograde urethrography and ureteral cystourethrography to assess the anterior and posterior urethra, respectively. Although this is most often performed under fluoroscopy, ultrasound urethrography is an alternative, although at the expense of the posterior urethra, it is only visualized using a transrectal approach [33-36].
In addition to understanding urethral anatomy, familiarity with normal periurethral structures is essential to avoid misdiagnoses, such as Cowper's ducts, Littre's glands, prostate, and ejaculatory ducts. Surgical treatment depends on the location, length, and the number of strictures, and options range from balloon dilation to endoscopic urethrotomy to anastomosis and replacement urethrotomy. Postoperative management includes urethrography to detect potential complications, including urethral leakage, graft failure, and recurrence of the stricture [37, 38].
Pompeo et al. [24] noted that penile cancer is a devastating disease that is usually diagnosed late, requiring extensive resections, causing changes in self-esteem and body image, affecting sexual and urinary functions, and impairing the quality of life. They determined that penile-conserving surgery should only be indicated for superficial penile cancer and isolated invasive lesions. Applicants for PSS must adhere to follow-up requirements that allow for early detection of local recurrences [39]. Quick and efficient rescue procedures are imperative in such situations.
Pfalzgraf et al. [26] studied the indications, the operative technique, and the results of two-stage urethroplasty of the oral mucosa (BM) and the mesh graft for the treatment of urethral strictures. Long strictures with severe spongiform fibrosis are an indication of a two-stage urethroplasty (BM and mesh graft). Excellent results can be achieved with both techniques with similar complication rates. The mesh graft technique remains the last option for a complex group of patients.
Barbagli et al. [27] conclude that the surgical treatment of bulbar urethral strictures remains one of the most difficult problems in reconstructive surgery. Urethral strictures are generally classified as traumatic and non-traumatic, depending on the etiology. Traumatic strictures are caused by trauma and define a tear in the urethra with obliteration of the urethral lumen, ending in fibrous fissures between the ends of the urethra. Traumatic obliteration of strictures requires cross-sectioning of the urethra to completely remove the fibrous tissue covering the ends of the urethra [40]. In contrast, nontraumatic and unobstructed urethral strictures require augmentation of the urethral plate with oral mucosa grafts. Nowadays, it is still difficult to choose the right surgical intervention to repair the stenosis of the eyeball without obliteration.
Conclusion
During the patient's initial request for medical help, it is important to conduct a maximum examination to choose a rational method of surgical treatment, according to modern standards, with a minimum probability of recurrence. However, early and late postoperative complications and recurrence after surgical treatment are not prevented.
Acknowledgments: None declared.
Ethical Permissions: For this type of study, the approval of the ethics committee is not required in the country where the study was conducted.
Conflicts of Interests: The authors declare no conflict of interests.
Authors’ Contribution: Vozianov S (First Author), Introduction Writer/Main Researcher (25%); Shamraev S (Second Author), Methodologist/Statistical Analyst (25%); Ridchenko M (Third Author), Discussion Writer/Data Analyst (25%); Shamraeva D (Forth Author), Assistant Researcher/Discussion Writer (25%)
Funding/Support: None declared.A
Keywords:
References
1. Tussupkaliev B, Zhumalina A, Zhekeyeva B, Sergazina T. The content of some essential micronutrients in infants with low birth weight with intrauterine herpes infection. Georg Med News. 2016;253:67-72. [Russian] [Link]
2. Dobrovanov O, Kralinsky K, Molcan J, Kovalchuk VP. Relevance of ultrasound neonatal screening of the urinary system. Ross Vestn Perinat Ped. 2019;64(2):68-72. [Link] [DOI:10.21508/1027-4065-2019-64-3-68-72]
3. Vozianov SO, Gorpinchenko II, Shamrayev SM, Babyuk IO, Rydchenko MA, Kozachikhina SI, et al. Comparative evaluation of the different types of open urethroplasty in long stricture and obliteration of the urethra. Health Man. 2016;2(57):22-6. [Russian] [Link] [DOI:10.30841/2307-5090.2(57).2016.82936]
4. Fedorchenko V, Polyanskaya V, Zachepilo S, Bobrova N, Loban G. Comprehensive study of anti-fungal effect of evgenol emulsion in polysorbat-80 on reference strain of candida albicans atcc 885-653. Georgian Med News. 2018;(282):166-70. [Russian] [Link]
5. Navruzov SN, Polatova DSh, Gafoor-Akhunov MA, Gabdikarimov KH. The value of marker proteins p53, bcl-2, Ki-67 in predicting the effectiveness of treatment for osteogenic sarcoma of tubular bones. Vopr Onkol. 2012;58(5):691-3. [Russian] [Link]
6. Tołodziecki MM, Chudański MM, Ponikowska I, Adamczyk P. Nonalcoholic fatty liver disease in obese patients. Wiad Lek. 2014;67(2 Pt 1):76-9. [Link]
7. Nazarchuk OA, Dmytriiev DV, Dmytriiev KD, Nazarchuk HH, Zaletskiy BV. Characteristics of infectious complications in critically ill patients. Wiad Lek. 2018;71(9):1784-92. [Link]
8. Palminteri E, Berdondini E, Verze P, De Nunzio C, Vitarelli A, Carmignani L. Contemporary urethral stricture characteristics in the developed world. Urology. 2013;81(1):191-6. [Link] [DOI:10.1016/j.urology.2012.08.062]
9. Kahokehr AA, Granieri MA, Webster GD, Peterson AC. A Critical Analysis of Bulbar Urethroplasty Stricture Recurrence: Characteristics and Management. J Urol. 2018;200(6):1302-7. [Link] [DOI:10.1016/j.juro.2018.07.036]
10. Mazdak H, Izadpanahi MH, Ghalamkari A, Kabiri M, Khorrami MH, Nouri-Mahdavi K, et al. Internal urethrotomy and intraurethral submucosal injection of triamcinolone in short bulbar urethral strictures. Int Urol Nephrol. 2010;42(3):565-8. [Link] [DOI:10.1007/s11255-009-9663-5]
11. Tavakkoli Tabassi K, Yarmohamadi A, Mohammadi S. Triamcinolone injection following internal urethrotomy for treatment of urethral stricture. Urol J. 2011;8(2):132-6. [Link]
12. Vozianov SO, Shamraev SM, Sosnin MD, Leonenko AM, Hrytsayuk AA. Long-term oncological results of radical prostatectomy in patients with localized prostate cancer. Health Man. 2018;(1):132-5. [Ukrainian] [Link] [DOI:10.30841/2307-5090.1.2018.144490]
13. Sertcelik MN, Bozkurt IH, Yalcinkaya F, Zengin K. Long-term results of permanent urethral stent Memotherm implantation in the management of recurrent bulbar urethral stenosis. BJU Int. 2011;108(11):1839-42. [Link] [DOI:10.1111/j.1464-410X.2011.10230.x]
14. Rusakov VI. Surgery of the urethra. Moscow: Meditsina; 1991. [Russian] [Link]
15. Sheehan JL, Naringrekar HV, Misiura AK, Deshmukh SP, Roth CG. The pre-operative and post-operative imaging appearances of urethral strictures and surgical techniques. Abdom Radiol (NY). 2021;46(5):2115-26. [Link] [DOI:10.1007/s00261-020-02879-8]
16. Ayoob A, Dawkins A, Gupta S, Nair R. Anterior urethral strictures and retrograde urethrography: An update for radiologists. Clin Imaging. 2020;67:37-48. [Link] [DOI:10.1016/j.clinimag.2020.05.008]
17. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187-96. [Link] [DOI:10.1097/SLA.0b013e3181b13ca2]
18. Clavien PA, Strasberg SM. Severity grading of surgical complications. Ann Surg. 2009;250(2):197-8. [Link] [DOI:10.1097/SLA.0b013e3181b6dcab]
19. Order of the Ministry of Health of Ukraine No. 330. On the introduction of the electronic version of accounting statistical forms in medical and preventive institutions. 2005. [Ukrainian] [Link]
20. Dvoretsky LI. Iatrogeniа in internist practice. Ter Arkh. 2019;91(1):129-36. [Link] [DOI:10.26442/00403660.2019.01.000041]
21. Vozianov S, Chernenko V, Savchuk V, Chernenko D, Sokolenko S, Bondarenko Y. Contact pneumatic ureterolithotripsy using the LMA StoneBreaker lithotripter and the search for ways to increase its effectiveness. Health Man. 2021;2:26-31. [Ukrainian] [Link] [DOI:10.30841/2307-5090.2.2021.237528]
22. Liu JS, Walker K, Stein D, Prabhu S, Hofer MD, Han J, et al. Lichen sclerosus and isolated bulbar urethral stricture disease. J Urol. 2014;192(3):775-9. [Link] [DOI:10.1016/j.juro.2014.03.090]
23. Brandes SB, Morey AF. Advanced male urethral and genital reconstructive surgery. New York: Springer; 2014. [Link] [DOI:10.1007/978-1-4614-7708-2]
24. Pompeo AC, Zequi Sde C, Pompeo AS. Penile cancer: organ-sparing surgery. Curr Opin Urol. 2015;25(2):121-8. [Link] [DOI:10.1097/MOU.0000000000000149]
25. Dy GW, Granieri MA, Fu BC, Vanni AJ, Voelzke B, Rourke KF, et al. Presenting complications to a reconstructive urologist after masculinizing genital reconstructive surgery. Urology. 2019;132:202-6. [Link] [DOI:10.1016/j.urology.2019.04.051]
26. Pfalzgraf D, Olianas R, Schreiter F, Fisch M. Two-staged urethroplasty: buccal mucosa and mesh graft techniques. Aktuelle Urol. 2010;41 Suppl 1:S5-9. [Link] [DOI:10.1055/s-0029-1224664]
27. Barbagli G, Bandini M, Balò S, Sansalone S, Butnaru D, Lazzeri M. Surgical treatment of bulbar urethral strictures: tips and tricks. Int Braz J Urol. 2020;46(4):511-8. [Link] [DOI:10.1590/s1677-5538.ibju.2020.99.04]
28. Stankiewicz R, Firszt-Adamczyk A, Czarnecki J, Adamczyk-Kipigroch H, Adamczyk P, Sinica W, et al. Recombinant tissue plasminogen activator for therapy of right atrial thrombus in a 2-year old child with nephrotic syndrome. Przeglad Pediatr. 2007;37(4):413-7. [Polish] [Link]
29. Jabbarov OO, Daminov BT, Boboev KT, Tursunova LD, Tashpulatova MX, Maksudova LI. Associations of polymorphic markers aluins/deli>D Ace T-786C gene Enos3 in diabetic nefropate progressing for type 2 diabetes mellitus. Int J Res Pharm Sci. 2020;11(4):6028-32. [Link] [DOI:10.26452/ijrps.v11i4.3268]
30. Tapbergenov SO, Zhetpisbaev BA, Ilderbayev OZ, Zhetpisbaeva HS, Olzhayeva RR, Prozor II, et al. Free radical oxidation in rats in the delayed period after combined exposure to dust and radiation. Bull Exp Biol Med. 2013;154(6):747-9. [Link] [DOI:10.1007/s10517-013-2046-z]
31. Nahaichuk VI, Nazarchuk OA, Osadchuk NI, Dmytriiev DV, Nazarchuk HH. The analytical prognosis of the susceptibility to aminoglycosides and doxycycline inacinetobacter baumanniiisoolated from burns of intensive care unit patients. Wiad Lek. 2018;71(3 Pt 2):705-9. [Link]
32. Chulenbayeva L, Ilderbayev O, Taldykbayev Z, Ilderbayeva G, Argynbekova A. Phytocorrection of immunological and biochemical changes in the combined impact of coal dust and high dose of radiation. Georgian Med News. 2018;(Issue):141-50. [Russian] [Link]
33. Dmytriiev D. Assessment and treatment of postoperative pain in children. Anaesth Pain Intensive Care. 2018;22(3):392-400. [Link]
34. Molcan J, Dobrovanov A, Koren R, Kralinsky K, Balaz V. Unilateral scrotal hernia with dual ureter herniation: The first experience of successful surgical correction. Pediatr - Zhur im GN Speranskogo. 2021;100(4):171-5. [Russian] [Link] [DOI:10.24110/0031-403X-2021-100-4-171-175]
35. Tusupkaliev BT, Zhumalina AK, Zhekeyeva BA, Baizhanova RM. The state of proinflammatory and anti-inflammatory cytokines in blood serum of infants with low birth weight in the prsesence of intrauterine infection. Int J Pharm Technol. 2016;8(2):13676-93. [Link]
36. Dmitriev DV, Katilov OV, Kalinchuk OV. The role of early enteral nutrition in multimodal program fast track surgery in children. Klin Khir. 2014;9:36-8. [Russian] [Link]
37. Dobrovanov O, Králinský K. Comparison of effectiveness and sensitivity of prenatal and postnatal sonografic diagnostics of anomalies the uropoetic system in Slovakia. Lek Obz. 2020;69(4):130-3. [Slovak] [Link]
38. Serniak YP, Sagalevych AI, Frolov OS, Serniak PY., Kryvopustov MS. Extraperitoneoscopic radical prostatectomy after pelvic sugery procedures. Wiad Lek. 2020;73(6):1093-6. [Link] [DOI:10.36740/WLek202006102]
39. Zhumalina AK, Tusupkaliev BT, Zame YA, Voloshina LV, Darzhanova KB. Clinical and immunological aspects of newborn adaptation born from mothers with intrauterine infection [Aspectos clínicos e imunológicos da adaptação do recém-nascido de mãe com infecção intrauterina]. Period Tche Quimica. 2020;17(34):656-66. [Link] [DOI:10.52571/PTQ.v17.n34.2020.680_P34_pgs_656_666.pdf]
40. Dobrovanov O, Králinský K. Sonographic screening of congenital kidney malformations in Slovakia. Lek Obz. 2018;67(12):426-9. [Slovak] [Link]