Volume 14, Issue 4 (2022)
Iran J War Public Health 2022, 14(4): 433-438 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2022/07/26 | Accepted: 2022/11/21 | Published: 2022/11/29
Received: 2022/07/26 | Accepted: 2022/11/21 | Published: 2022/11/29
How to cite this article
Sutriyawan A, Fardhoni F, Yusuff A, Akbar H, Sangaji M. Risk Factors Predicting Hypertension in the Elderly. Iran J War Public Health 2022; 14 (4) :433-438
URL: http://ijwph.ir/article-1-1244-en.html
URL: http://ijwph.ir/article-1-1244-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
1- Department of Public Health, Faculty of Health Sciences, Bhakti Kencana University, Bandung, Indonesia
2- Department of Public Health, Mahardika College of Health Sciences, Cirebon, Indonesia
3- Department of Public Health, Graha Medika Institute of Health and Technology, Kotamobagu, Indonesia
4- Department of Fisheries and Marine Sciences, Faculty of Fisheries and Marine Science, Pattimura University, Ambon, Indonesia
2- Department of Public Health, Mahardika College of Health Sciences, Cirebon, Indonesia
3- Department of Public Health, Graha Medika Institute of Health and Technology, Kotamobagu, Indonesia
4- Department of Fisheries and Marine Sciences, Faculty of Fisheries and Marine Science, Pattimura University, Ambon, Indonesia
Full-Text (HTML) (1424 Views)
Introduction
Hypertension is a global health issue that affects practically everyone. Hypertension affects 1.28 percent of persons aged 30-79 years globally [1, 2], with two-thirds of those affected living in low and middle-income nations [3]. According to WHO data, hypertension affects 22 percent of the global population, with Africa having the highest prevalence of hypertension at 27 percent, the Eastern Mediterranean at 26 percent, and Southeast Asia at 25 percent [4].
The prevalence of hypertension in Indonesia's population aged 18 years is 34.11 percent, up 8.31 percent from 2013 [5]. The age groups with the highest prevalence of hypertension were 75 and up (69.5) and 65-74 years (63.2). This is because, physically, the older a person becomes, the higher their risk of developing hypertension, which is caused by a decrease in organ function in the body [6]. Hypertension, or high blood pressure, is a common condition among the elderly [7]. The current study also found that the prevalence of all four chronic diseases increased with age, likewise found in other studies [8, 9]. Therefore, young adults and middle age should be made known of the alarming trend and statistic in order for them to consider healthier lifestyles to achieve healthy aging [10].
Hypertension is frequently referred to as a "silent disease". Hypertension risk factors are split into two categories: those that cannot be modified and those that can be changed. Age, gender, race, and heredity are all factors that cannot be changed. Smoking, obesity, a sedentary lifestyle, physical activity, sodium intake, low potassium levels, stress, low fiber intake, and alcohol consumption are all modifiable factors [11].
A previous study has shown that persons who have an unhealthy lifestyle, such as lack of physical activity, smoking, excessive salt consumption, and alcohol consumption, are more likely to develop hypertension [12]. Other factors include genetics, obesity, stress, and the use of frying oil [13]. According to another study, hypertension is more likely to occur in those who are obese/overweight and those who are under pressure/stress. The majority of hypertension patients are more common in those who have a family history of hypertension, and lifestyles such as smoking are considered a lifestyle, all of which are harmful to one's health [14].
Ciamis Regency, with a prevalence of 49.6%, and Bandung City, with a prevalence of 36.79%, have the greatest rate of hypertension in West Java [6]. According to preliminary findings from the Neglasari Health Centre in Bandung, hypertension is the second most common condition after ARI. Hypertension affects 6,031 people, with the elderly accounting for 57% of the total. The rise in cases is likely because many people are still unaware that they have hypertension, and those who have been diagnosed with hypertension do not have regular health checks. This is exacerbated by several other factors, including poor people's lifestyles, such as lack of physical activity, stress, the diet that includes foods that cause hypertension in excess, and smoking habits that are difficult to quit [15].
To combat the rising number of cases, efforts have been made to provide health education, home visits, and community engagement. The number of risk factors for hypertension is so high that health personnel face difficulties in prioritizing preventive measures [16]. As a result, all study that can verify the most dominating risk factor for rising cases of hypertension is required. This study aimed to investigate the non-modifiable and modifiable risk variables, as well as the dominating risk factors, that are linked to the development of hypertension in the elderly.
Instrument and Methods
Quantitative research with a cross-sectional research approach was used. This design was used to look at the association between non-modifiable and modifiable risk variables, as well as the most common risk factors linked to hypertension in the elderly. This study took place in the Neglasari Health Centre in Bandung City from January to April 2022.
All patients who visited and received treatment at the general polyclinic and were registered in the Neglasari Health Centre’s report registration were included in this study. The sample size was calculated using "Sample Size for One-Sample Test of Proportion" (Level of Significance 5%, Power 90%). There were 245 respondents in this survey. A basic random strategy was used to collect samples. The instruments used were questionnaires and observation sheets.
The incidence of hypertension was the dependent variable. If the systolic blood pressure is 140 mmHg and diastolic blood pressure is 90 mmHg that is considered hypertension. The information was derived from the patient's medical records. The independent variable was age, which was divided into two categories: 60-74 years and 75 years. Female and male were the two genders. There were two types of family background: have a history and no history. Smoking, which was classified as smoking if the elderly smoked within the previous year and did not smoke.
Obesity was classified as yes if the BMI is 25 kg/m2 or no if the Body Mass Index (BMI) is less than 25 kg/m2. Physical activity was classified as light if the respondent undertakes less than 30 minutes of light physical activity per day for three days per week. Severe stress and light stress were two types of stress. Excess salt consumption was divided into two categories: yes and no. Alcohol consumption was divided into two categories: yes and no. Low fibber consumption was divided into two categories: yes and no.
Data were analyzed using univariate analysis, followed by bivariate analysis using the chi-square test with a significance value of 0.05. The researchers next ran a multivariate logistic regression analysis to discover the most important factors linked to the occurrence of hypertension.
Findings
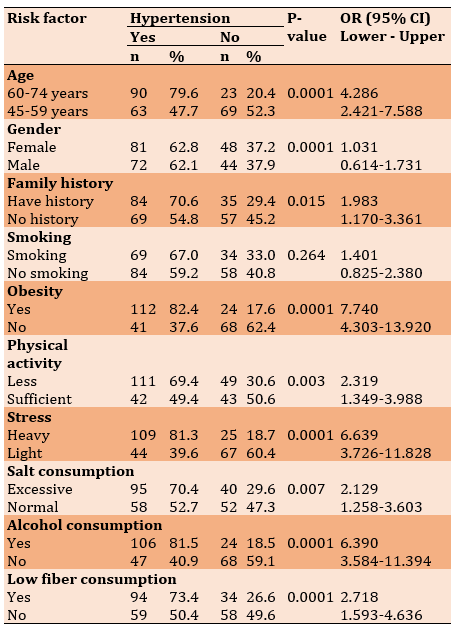
A total of 245 patients attended the Neglasari Health Centre. More than half of respondents were 45-59 years old (53.9%) and female (52.7%) and had a family history of hypertension (51.4%). The frequency distribution of other patient characteristics is presented in Table 1.
Table 1) Frequency distribution of risk factor for hypertension in the elderly (n=245)

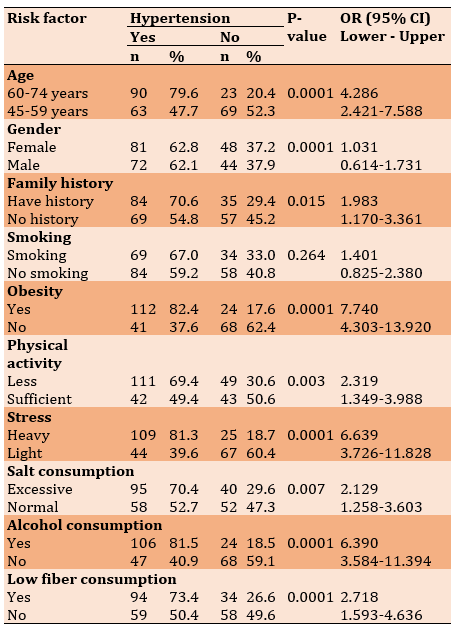
Age (p=0.0001), family history (p=0.015), obesity (p=0.0001), physical activity (p=0.003), stress
(p=0.0001), excessive salt consumption (0.007), alcohol consumption (p=0.0001), and poor fibber consumption were all risk factors for hypertension in the elderly (p=0.0001; Table 2).
Table 2) Determination of risk factors for hypertension in the elderly using chi-square test
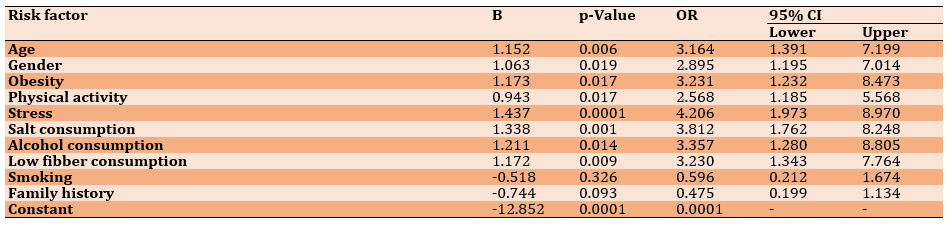
Based on the results of multiple logistic regression, age, gender, obesity, physical activity, stress, salt consumption, alcohol consumption, and high fiber consumption were determined to be risk factors for hypertension. In the meantime, smoking and family history played a role in the development of hypertension in the elderly (Table 3).
Hypertension is a global health issue that affects practically everyone. Hypertension affects 1.28 percent of persons aged 30-79 years globally [1, 2], with two-thirds of those affected living in low and middle-income nations [3]. According to WHO data, hypertension affects 22 percent of the global population, with Africa having the highest prevalence of hypertension at 27 percent, the Eastern Mediterranean at 26 percent, and Southeast Asia at 25 percent [4].
The prevalence of hypertension in Indonesia's population aged 18 years is 34.11 percent, up 8.31 percent from 2013 [5]. The age groups with the highest prevalence of hypertension were 75 and up (69.5) and 65-74 years (63.2). This is because, physically, the older a person becomes, the higher their risk of developing hypertension, which is caused by a decrease in organ function in the body [6]. Hypertension, or high blood pressure, is a common condition among the elderly [7]. The current study also found that the prevalence of all four chronic diseases increased with age, likewise found in other studies [8, 9]. Therefore, young adults and middle age should be made known of the alarming trend and statistic in order for them to consider healthier lifestyles to achieve healthy aging [10].
Hypertension is frequently referred to as a "silent disease". Hypertension risk factors are split into two categories: those that cannot be modified and those that can be changed. Age, gender, race, and heredity are all factors that cannot be changed. Smoking, obesity, a sedentary lifestyle, physical activity, sodium intake, low potassium levels, stress, low fiber intake, and alcohol consumption are all modifiable factors [11].
A previous study has shown that persons who have an unhealthy lifestyle, such as lack of physical activity, smoking, excessive salt consumption, and alcohol consumption, are more likely to develop hypertension [12]. Other factors include genetics, obesity, stress, and the use of frying oil [13]. According to another study, hypertension is more likely to occur in those who are obese/overweight and those who are under pressure/stress. The majority of hypertension patients are more common in those who have a family history of hypertension, and lifestyles such as smoking are considered a lifestyle, all of which are harmful to one's health [14].
Ciamis Regency, with a prevalence of 49.6%, and Bandung City, with a prevalence of 36.79%, have the greatest rate of hypertension in West Java [6]. According to preliminary findings from the Neglasari Health Centre in Bandung, hypertension is the second most common condition after ARI. Hypertension affects 6,031 people, with the elderly accounting for 57% of the total. The rise in cases is likely because many people are still unaware that they have hypertension, and those who have been diagnosed with hypertension do not have regular health checks. This is exacerbated by several other factors, including poor people's lifestyles, such as lack of physical activity, stress, the diet that includes foods that cause hypertension in excess, and smoking habits that are difficult to quit [15].
To combat the rising number of cases, efforts have been made to provide health education, home visits, and community engagement. The number of risk factors for hypertension is so high that health personnel face difficulties in prioritizing preventive measures [16]. As a result, all study that can verify the most dominating risk factor for rising cases of hypertension is required. This study aimed to investigate the non-modifiable and modifiable risk variables, as well as the dominating risk factors, that are linked to the development of hypertension in the elderly.
Instrument and Methods
Quantitative research with a cross-sectional research approach was used. This design was used to look at the association between non-modifiable and modifiable risk variables, as well as the most common risk factors linked to hypertension in the elderly. This study took place in the Neglasari Health Centre in Bandung City from January to April 2022.
All patients who visited and received treatment at the general polyclinic and were registered in the Neglasari Health Centre’s report registration were included in this study. The sample size was calculated using "Sample Size for One-Sample Test of Proportion" (Level of Significance 5%, Power 90%). There were 245 respondents in this survey. A basic random strategy was used to collect samples. The instruments used were questionnaires and observation sheets.
The incidence of hypertension was the dependent variable. If the systolic blood pressure is 140 mmHg and diastolic blood pressure is 90 mmHg that is considered hypertension. The information was derived from the patient's medical records. The independent variable was age, which was divided into two categories: 60-74 years and 75 years. Female and male were the two genders. There were two types of family background: have a history and no history. Smoking, which was classified as smoking if the elderly smoked within the previous year and did not smoke.
Obesity was classified as yes if the BMI is 25 kg/m2 or no if the Body Mass Index (BMI) is less than 25 kg/m2. Physical activity was classified as light if the respondent undertakes less than 30 minutes of light physical activity per day for three days per week. Severe stress and light stress were two types of stress. Excess salt consumption was divided into two categories: yes and no. Alcohol consumption was divided into two categories: yes and no. Low fibber consumption was divided into two categories: yes and no.
Data were analyzed using univariate analysis, followed by bivariate analysis using the chi-square test with a significance value of 0.05. The researchers next ran a multivariate logistic regression analysis to discover the most important factors linked to the occurrence of hypertension.
Findings
A total of 245 patients attended the Neglasari Health Centre. More than half of respondents were 45-59 years old (53.9%) and female (52.7%) and had a family history of hypertension (51.4%). The frequency distribution of other patient characteristics is presented in Table 1.
Table 1) Frequency distribution of risk factor for hypertension in the elderly (n=245)

Age (p=0.0001), family history (p=0.015), obesity (p=0.0001), physical activity (p=0.003), stress
(p=0.0001), excessive salt consumption (0.007), alcohol consumption (p=0.0001), and poor fibber consumption were all risk factors for hypertension in the elderly (p=0.0001; Table 2).
Table 2) Determination of risk factors for hypertension in the elderly using chi-square test
Based on the results of multiple logistic regression, age, gender, obesity, physical activity, stress, salt consumption, alcohol consumption, and high fiber consumption were determined to be risk factors for hypertension. In the meantime, smoking and family history played a role in the development of hypertension in the elderly (Table 3).
Table 3) Multiple logistic regression model of hypertension incidence in the elderly
Discussion
This study aimed to investigate the risk factors for hypertension in the elderly. Hypertension was caused by two basic variables, which could not be changed and factors that could be changed. Age, gender, and family history were the non-modifiable characteristics investigated in this study.
This study established a relationship between age and the occurrence of hypertension, which is consistent with prior research that found a link between age and the occurrence of hypertension [17]. The chance of developing hypertension increases as one gets older. According to research conducted in Padang, the age group above 60 years has the largest number of hypertension victims [18]. It was discovered that respondents above the age of 60 had hypertension. This was because the risk of acquiring hypertension increased with age. The ability of the body's organs, especially the cardiovascular system, which included the heart and blood vessels, decreased as a person ages. Blood vessels became narrower, and blood vessel walls stiffen, causing blood pressure to increase [19].
Gender was observed to be associated with the incidence of hypertension in the logistic regression model. Although the bivariate analysis could not be confirmed, it could be proven that gender was a risk factor for hypertension after controlling for various other variables. This finding supports prior studies that found a link between gender and the prevalence of hypertension. According to a Canadian cohort research, men are more susceptible to hypertension than women [20]. This is because hypertension develops more slowly in women than in men. Men were more prone than women to acquire hypertension in their early adult years [21].
The incidence of hypertension had a strong relationship with family history. According to the findings, people with a history of hypertension were more likely to develop hypertension. This finding supports a prior study that found a link between family history and hypertension [22]. According to another study conducted in Sri Lanka, persons with a family history of hypertension were nearly 1.4 times more likely than those without a family history to acquire hypertension [23].
This study was unable to establish the connection between smoking and the occurrence of hypertension. Hypertension affected both smokers and non-smokers, according to this study. Smoking caused blood pressure to rise because nicotine in cigarettes promoted the adrenaline hormone, which causes blood pressure to rise [24]. Nicotine is absorbed by the blood arteries in the lungs and circulates throughout the body, causing blood vessels to constrict. As a result, the heart labor to pump blood throughout the body through restricted blood arteries increases. Furthermore, smoking can raise the heart rate, and the buildup of cholesterol in blood vessels can cause damage to blood vessels, causing the heart to pump quicker [25].
Obesity and the incidence of hypertension in the elderly were linked. These findings support prior research that suggested being overweight could increase the risk of hypertension [26]. Obese older people are more prone to develop hypertension, according to research findings. The study of obesity is based on BMI. Obesity can directly lead to increased cardiac output [26]. It is because the bigger the body mass, the more blood circulates, and the cardiac output rises as a result [27].
Hypertension is one of the most common diseases of adulthood for various reasons. This study already proved that physical activity is linked to a lower risk of hypertension. Hypertension is 5.7 times more likely in people who did not engage in physical activity. The findings in the field demonstrated that senior people who performed less physical activity had higher blood pressure. According to some respondents, they did not exercise because they were lazy or because they were too busy at work. Some respondents said they only exercised when they had free time, and the majority said they only exercised once a week, on weekends. Regular and isotonic exercise can reduce peripheral resistance, lowering blood pressure (for hypertension) and training the heart muscle so that it becomes acclimated to when the heart has to do more effort owing to particular situations [28].
In addition, this study also examined physical activity, which was categorized into insufficient and sufficient. People who are inactive tend to have a faster heart rate, and their heart muscle has to work harder with each contraction. The harder the heart contracts, the more force it exerts on the arteries. Therefore, to avoid the occurrence of hypertension, one must perform sufficient physical activity by exercising for 30 minutes or more continuously and doing it 3 times a week [29].
The finding revealed that stress contribute to the occurrence of hypertension. This finding supports prior research that indicated that stress can influence the occurrence of hypertension [30]. The majority of the elderly who suffered significant stress had hypertension, according to this study. Humans' physiological and psychological responses to internal and external stress. Long-term stress can induce physical changes that are harmful to the body. The Perceived Stress Scale (PSS) questionnaire was used to calculate stress levels in this study. This questionnaire has been widely utilized in stress investigations, particularly among adults. Blood pressure can rise at any time due to stress. When we are stressed, the hormone adrenaline surges, which causes the heart to pump blood quicker, raising blood pressure. When stress levels drop, blood pressure drops as well [31].
This study proved that excessive salt consumption is significantly associated with the incidence of hypertension. This result is consistent with previous studies, which state that the incidence of hypertension can be caused by excessive salt consumption [32]. This is also in line with other studies conducted in productive age, which state that salt consumption is significantly associated with the incidence of hypertension in productive age [33].
The findings in the field also showed that hypertension affect the majority of the elderly who ingested too much salt. Several respondents stated that they are accustomed to using salt in cooking since food that is not salty enough is less appetizing. Excess sodium consumption produces an increase in sodium content in the extracellular fluid. The intracellular fluid is drained to restore normalcy, causing the extracellular fluid volume to rise. An increase in blood volume is caused by an increase in extracellular fluid volume, which influences the start of hypertension [19]. Because salt pulls fluid outside the cells and prevents it from being expelled, it promotes an accumulation of fluid in the body, increasing blood volume and pressure [34].
Based on the result of this study, alcohol consumption was significantly associated with the incidence of hypertension. A person who consumed alcohol had 2 times the chance of suffering from hypertension. This result is in line with previous research, which stated that alcohol consumption is a risk factor for hypertension [11, 35]. Moreover, the elderly who drank alcohol were more prone to develop hypertension. According to field observations, several respondents said that they did not use alcohol every day but that they did so within two weeks. Alcohol contains a lot of ethanol, and the more ethanol there is, the harder the drink becomes. Alcohol can cause the hormone epinephrine (adrenaline) to be released, which can cause blood vessels to constrict [36].
Low fiber consumption was connected to the development of hypertension. The result of this study supports previous research, which found a link between fiber intake and systolic and diastolic blood pressure. Meanwhile, according to a study conducted in Bengkulu, the lesser the fiber intake, the greater the systolic blood pressure. Low fiber ingestion has an impact on rising blood pressure when blood is circulated throughout the body by the heart [37]. According to our findings, the majority of respondents ate veggies 3-4 times per week. Subjects ate little amounts of vegetables and fruits, particularly soluble fiber sources. Meanwhile, soluble fiber could reduce blood pressure by lowering plasma cholesterol levels. Fiber in the favorable category, such as 25-30 grams, can bind bile acids, reducing fat and blood cholesterol absorption and thereby lowering the risk of high blood pressure. Fiber can help you feel full, prevent constipation, and lower your risk of heart disease by keeping your cholesterol levels within normal ranges [38].
This study needs to be continued using a cohort study and examine more deeply especially stress events, to complete this research.
Conclusion
Both non-modifiable (age and family history) and modifiable (obesity, physical activity, stress, excessive salt consumption, alcohol consumption, and low fiber consumption) factors can influence the occurrence of hypertension. Stress is the most significant factor linked to hypertension. When compared to persons who have mild stress, people who have severe stress have a fourfold increased risk of acquiring hypertension.
Acknowledgments: The authors would like to thank the Center for Research and Community Service of Bhakti Kencana University (LPPM-UB) for supporting this research.
Ethical Permissions: This study was approved by the Immanuel School of Health Sciences Bandung (No.130/KEPK/STIKI/VII/2022).
Conflicts of Interests: The authors declare no conflict of interests.
Authors’ Contribution: Sutriyawan A (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer (35%); Fardhoni F (Second Author), Introduction Writer/ Methodologist/Main Researcher/Discussion Writer (20%); Yusuff AA (Third Author), Assistant Researcher/Statistical Analyst (15%); Akbar H (Forth Author), Assistant Researcher/Discussion Writer (15%); Sangaji M (Fifth Author), Assistant Researcher/Discussion Writer (15%)
Funding/Support: The authors received no financial support for the research, authorship, and publication of this article.
This study aimed to investigate the risk factors for hypertension in the elderly. Hypertension was caused by two basic variables, which could not be changed and factors that could be changed. Age, gender, and family history were the non-modifiable characteristics investigated in this study.
This study established a relationship between age and the occurrence of hypertension, which is consistent with prior research that found a link between age and the occurrence of hypertension [17]. The chance of developing hypertension increases as one gets older. According to research conducted in Padang, the age group above 60 years has the largest number of hypertension victims [18]. It was discovered that respondents above the age of 60 had hypertension. This was because the risk of acquiring hypertension increased with age. The ability of the body's organs, especially the cardiovascular system, which included the heart and blood vessels, decreased as a person ages. Blood vessels became narrower, and blood vessel walls stiffen, causing blood pressure to increase [19].
Gender was observed to be associated with the incidence of hypertension in the logistic regression model. Although the bivariate analysis could not be confirmed, it could be proven that gender was a risk factor for hypertension after controlling for various other variables. This finding supports prior studies that found a link between gender and the prevalence of hypertension. According to a Canadian cohort research, men are more susceptible to hypertension than women [20]. This is because hypertension develops more slowly in women than in men. Men were more prone than women to acquire hypertension in their early adult years [21].
The incidence of hypertension had a strong relationship with family history. According to the findings, people with a history of hypertension were more likely to develop hypertension. This finding supports a prior study that found a link between family history and hypertension [22]. According to another study conducted in Sri Lanka, persons with a family history of hypertension were nearly 1.4 times more likely than those without a family history to acquire hypertension [23].
This study was unable to establish the connection between smoking and the occurrence of hypertension. Hypertension affected both smokers and non-smokers, according to this study. Smoking caused blood pressure to rise because nicotine in cigarettes promoted the adrenaline hormone, which causes blood pressure to rise [24]. Nicotine is absorbed by the blood arteries in the lungs and circulates throughout the body, causing blood vessels to constrict. As a result, the heart labor to pump blood throughout the body through restricted blood arteries increases. Furthermore, smoking can raise the heart rate, and the buildup of cholesterol in blood vessels can cause damage to blood vessels, causing the heart to pump quicker [25].
Obesity and the incidence of hypertension in the elderly were linked. These findings support prior research that suggested being overweight could increase the risk of hypertension [26]. Obese older people are more prone to develop hypertension, according to research findings. The study of obesity is based on BMI. Obesity can directly lead to increased cardiac output [26]. It is because the bigger the body mass, the more blood circulates, and the cardiac output rises as a result [27].
Hypertension is one of the most common diseases of adulthood for various reasons. This study already proved that physical activity is linked to a lower risk of hypertension. Hypertension is 5.7 times more likely in people who did not engage in physical activity. The findings in the field demonstrated that senior people who performed less physical activity had higher blood pressure. According to some respondents, they did not exercise because they were lazy or because they were too busy at work. Some respondents said they only exercised when they had free time, and the majority said they only exercised once a week, on weekends. Regular and isotonic exercise can reduce peripheral resistance, lowering blood pressure (for hypertension) and training the heart muscle so that it becomes acclimated to when the heart has to do more effort owing to particular situations [28].
In addition, this study also examined physical activity, which was categorized into insufficient and sufficient. People who are inactive tend to have a faster heart rate, and their heart muscle has to work harder with each contraction. The harder the heart contracts, the more force it exerts on the arteries. Therefore, to avoid the occurrence of hypertension, one must perform sufficient physical activity by exercising for 30 minutes or more continuously and doing it 3 times a week [29].
The finding revealed that stress contribute to the occurrence of hypertension. This finding supports prior research that indicated that stress can influence the occurrence of hypertension [30]. The majority of the elderly who suffered significant stress had hypertension, according to this study. Humans' physiological and psychological responses to internal and external stress. Long-term stress can induce physical changes that are harmful to the body. The Perceived Stress Scale (PSS) questionnaire was used to calculate stress levels in this study. This questionnaire has been widely utilized in stress investigations, particularly among adults. Blood pressure can rise at any time due to stress. When we are stressed, the hormone adrenaline surges, which causes the heart to pump blood quicker, raising blood pressure. When stress levels drop, blood pressure drops as well [31].
This study proved that excessive salt consumption is significantly associated with the incidence of hypertension. This result is consistent with previous studies, which state that the incidence of hypertension can be caused by excessive salt consumption [32]. This is also in line with other studies conducted in productive age, which state that salt consumption is significantly associated with the incidence of hypertension in productive age [33].
The findings in the field also showed that hypertension affect the majority of the elderly who ingested too much salt. Several respondents stated that they are accustomed to using salt in cooking since food that is not salty enough is less appetizing. Excess sodium consumption produces an increase in sodium content in the extracellular fluid. The intracellular fluid is drained to restore normalcy, causing the extracellular fluid volume to rise. An increase in blood volume is caused by an increase in extracellular fluid volume, which influences the start of hypertension [19]. Because salt pulls fluid outside the cells and prevents it from being expelled, it promotes an accumulation of fluid in the body, increasing blood volume and pressure [34].
Based on the result of this study, alcohol consumption was significantly associated with the incidence of hypertension. A person who consumed alcohol had 2 times the chance of suffering from hypertension. This result is in line with previous research, which stated that alcohol consumption is a risk factor for hypertension [11, 35]. Moreover, the elderly who drank alcohol were more prone to develop hypertension. According to field observations, several respondents said that they did not use alcohol every day but that they did so within two weeks. Alcohol contains a lot of ethanol, and the more ethanol there is, the harder the drink becomes. Alcohol can cause the hormone epinephrine (adrenaline) to be released, which can cause blood vessels to constrict [36].
Low fiber consumption was connected to the development of hypertension. The result of this study supports previous research, which found a link between fiber intake and systolic and diastolic blood pressure. Meanwhile, according to a study conducted in Bengkulu, the lesser the fiber intake, the greater the systolic blood pressure. Low fiber ingestion has an impact on rising blood pressure when blood is circulated throughout the body by the heart [37]. According to our findings, the majority of respondents ate veggies 3-4 times per week. Subjects ate little amounts of vegetables and fruits, particularly soluble fiber sources. Meanwhile, soluble fiber could reduce blood pressure by lowering plasma cholesterol levels. Fiber in the favorable category, such as 25-30 grams, can bind bile acids, reducing fat and blood cholesterol absorption and thereby lowering the risk of high blood pressure. Fiber can help you feel full, prevent constipation, and lower your risk of heart disease by keeping your cholesterol levels within normal ranges [38].
This study needs to be continued using a cohort study and examine more deeply especially stress events, to complete this research.
Conclusion
Both non-modifiable (age and family history) and modifiable (obesity, physical activity, stress, excessive salt consumption, alcohol consumption, and low fiber consumption) factors can influence the occurrence of hypertension. Stress is the most significant factor linked to hypertension. When compared to persons who have mild stress, people who have severe stress have a fourfold increased risk of acquiring hypertension.
Acknowledgments: The authors would like to thank the Center for Research and Community Service of Bhakti Kencana University (LPPM-UB) for supporting this research.
Ethical Permissions: This study was approved by the Immanuel School of Health Sciences Bandung (No.130/KEPK/STIKI/VII/2022).
Conflicts of Interests: The authors declare no conflict of interests.
Authors’ Contribution: Sutriyawan A (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer (35%); Fardhoni F (Second Author), Introduction Writer/ Methodologist/Main Researcher/Discussion Writer (20%); Yusuff AA (Third Author), Assistant Researcher/Statistical Analyst (15%); Akbar H (Forth Author), Assistant Researcher/Discussion Writer (15%); Sangaji M (Fifth Author), Assistant Researcher/Discussion Writer (15%)
Funding/Support: The authors received no financial support for the research, authorship, and publication of this article.
Keywords:
References
1. Alves AM, Rodrigues A, Sa-Couto P, Simões JL. Effect of an educational nursing intervention on the mental adjustment of patients with chronic arterial hypertension: An interventional study. Int J Environ Res Public Health. 2021;19(1):170. [Link] [DOI:10.3390/ijerph19010170]
2. Mercado-Asis LB, Ona DID, Bonzon D, Vilela GA, Diaz AF, Balmores BA, et al. Socioeconomic impact and burden of hypertension in the Philippines projected in 2050. Hypertens Res. 2022;1-9. [Link] [DOI:10.1097/01.hjh.0000835612.76426.8d]
3. World Health Organization. Hypertension [Internet]. Geneva: World Health Organization; 2021 [cited 2022 Mar 11]. Available from: https://www.who.int/news-room/fact-sheets/detail/hypertension. [Link]
4. Ministry of Health of the Republic of Indonesia. Hypertension is a silent killer [Internet]. Jakarta: 2019 [cited 2022 Mar 11]. Available from: https://pusdatin.kemkes.go.id/resources/download/pusdatin/infodatin/infodatin-hipertensi-si-pembunuh-senyap.pdf. [Link]
5. Noviasari NA. Analysis of risk factors Hl. Blum in hypertension patients. Int J Health Educ Soc. 2021;4(2):1-15. [Link]
6. Ministry of Health of the Republic of Indonesia. Main Results of Basic Health Research (RISKESDAS). J Phys A Math Theor. 2018;44(8):1-200. [Indonesian] [Link]
7. Siregar EIS. Systematic review of the relationship between diet and hypertension incidence in the elderly. J Ilmiah PANNMED (Pharmacist, Analyst, Nurse, Nutrition, Midwivery, Environment, Dentist) 2022;17(1):202-9. [Indonesian] [Link] [DOI:10.36911/pannmed.v17i1.1296]
8. Kraja F, Kraja B, Mone I, Harizi I, Babameto A, Burazeri G. Self-reported prevalence and risk factors of non-communicable diseases in the Albanian adult population. Med Arch. 2016;70(3):208-12. [Link] [DOI:10.5455/medarh.2016.70.208-212]
9. Schiøtz ML, Stockmarr A, Høst D, Glümer C, Frølich A. Social disparities in the prevalence of multimorbidity-A register-based population study. BMC Public Health. 2017;17(1):422. [Link] [DOI:10.1186/s12889-017-4314-8]
10. Zhao C, Wong L, Zhu Q, Yang H. Prevalence and correlates of chronic diseases in an elderly population: A community-based survey in Haikou. PLoS One. 2018;13(6):e0199006. [Link] [DOI:10.1371/journal.pone.0199006]
11. Memah M, Kandou GD, Nelwan JE. The relationship between smoking and alcohol consumption with the incidence of hypertension in the Kombi Health Center, Kombi District, Minahasa Regency. KESMAS. 2019;8(1):68-74. [Indonesian] [Link]
12. Rajkumar E, Romate J. Behavioural risk factors, hypertension knowledge, and hypertension in rural India. Int J Hypertens. 2020;2020:8108202. [Link] [DOI:10.1155/2020/8108202]
13. Sutriyawan A, Endah Y, Miranda TG. Relationship between physical activity and routine health checks with incidence of hypertension. Int J Health Sci Med Res. 2021;1(1):1-5. [Link]
14. Siwi AS, Irawan D, Susanto A. Analysis of factors affecting the incidence of hypertension. J Bionurs. 2020;2(3):164-6. [Indonesian] [Link] [DOI:10.20884/1.bion.2020.2.3.70]
15. Utami AR, Irawati HR, Djupri DR. The effect of giving green Cincau leaf juice on lowering blood pressure in hypertensive patients. J Nurs Health Sci. 2022;1(3):98-102. [Indonesian] [Link]
16. Wardana IE, Sriatmi A, Kusumastuti W. Analysis of hypertension management process (Case study at Purwoyoso Health Center Semarang City). Journal of Public Health (Undip). 2020;8(1):76-86. [Indonesian] [Link]
17. Taiso SN, Sudayasa IP, Paddo J. Analysis of sociodemographic relationship with the incidence of hypertension in the work area of the Lasalepa Health Center, Muna Regency. Nurs Care Health Technol J. 2021;1(2):102-9. [Link] [DOI:10.56742/nchat.v1i2.10]
18. Sedayu B, Azmi S, Rahmatini R. Characteristics of hypertensive patients in the inpatient ward of SMF internal medicine RSUP DR. M. Djamil Padang in 2013. J Kesehatan Andalas. 2015;4(1). [Indonesian] [Link] [DOI:10.25077/jka.v4i1.192]
19. Adam L. Determinants of hypertension in the elderly. Jambura Health Sport J. 2019;1(2):82-9. [Indonesian] [Link] [DOI:10.37311/jhsj.v1i2.2558]
20. Trudel X, Brisson C, Gilbert-Ouimet M, Duchaine CS, Dalens V, Talbot D, et al. Masked hypertension incidence and risk factors in a prospective cohort study. Eur J Prev Cardiol. 2019;26(3):231-7. [Link] [DOI:10.1177/2047487318802692]
21. Tumanduk WM, Nelwan JE, Asrifuddin A. Risk factors for hypertension at play at Robert Wolter Mongisidi Hospital. e-CliniC. 2019;7(2):119-125. [Indonesian] [Link] [DOI:10.35790/ecl.v7i2.26569]
22. Sari YH, Majid M. Factors affecting the incidence of hypertension in the elderly in the working area of the Maiwa Health Center, Enrekang Regency. J Ilmiah Manusia Dan Kesehatan. 2019;2(1):68-79. [Indonesian] [Link] [DOI:10.31850/makes.v2i1.125]
23. Ranasinghe P, Cooray DN, Jayawardena R, Katulanda P. The influence of family history of hypertension on disease prevalence and associated metabolic risk factors among Sri Lankan adults. BMC Public Health. 2015;15(1):1-9. [Link] [DOI:10.1186/s12889-015-1927-7]
24. Sangka A, Basri M, Hanis M. Relationship of lifestyle with the incidence of hypertension in the Makassar City General Hospital. JIMPK: J Ilmiah Mahasiswa & Penelitian Keperawatan. 2021;1(2):182-8. [Indonesian] [Link]
25. Oktaviani E, Prastia TN, Dwimawati E. Factors related to the incidence of hypertension in the pre-elderly at the Bojonggede Health Center in 2021. PROMOTOR. 2022;5(2):135-47. [Indonesian] [Link] [DOI:10.32832/pro.v5i2.6148]
26. Herdiani N, Ibad M, Wikurendra EA. The effect of physical activity and obesity with the incidence of hypertension in the elderly at the Klampis Ngasem Health Center, Surabaya City. An-Nadaa: J Kesehatan Masyarakat. 2021;8(2):114-20. [Indonesian] [Link] [DOI:10.31602/ann.v8i2.5561]
27. Mouton AJ, Li X, Hall ME, Hall JE. Obesity, hypertension, and cardiac dysfunction: novel roles of immunometabolism in macrophage activation and inflammation. Circ Res. 2020;126(6):789-806. [Link] [DOI:10.1161/CIRCRESAHA.119.312321]
28. Ladyani F, Febriyani A, Prasetia T, Berliana I. Relationship between exercise and stress with hypertension levels in the elderly. J Ilmiah Kesehatan Sandi Husada. 2021;10(1):82-7. [Indonesian] [Link] [DOI:10.35816/jiskh.v10i1.514]
29. Sutriyawan A, Apriyani R, Miranda TG. The relationship between lifestyle and hypertension cases at UPT Cibiru Public Health Center Bandung City. Dis Prev Public Health J. 2021;15(1):50-6. [Link] [DOI:10.12928/dpphj.v15i1.2456]
30. Mayasari M, Waluyo A, Jumaiyah W, Azzam R. Factors associated with the incidence of hypertension. J Telenurs. 2019;1(2):344-53. [Indonesian] [Link] [DOI:10.31539/joting.v1i2.849]
31. Arikah T, Rahardjo TBW, Widodo S. Incidence of hypertension in pregnant women. J Penelitian dan Pengembangan Kesehatan Masyarakat Indonesia. 2020;1(2):115-24. [Indonesian] [Link] [DOI:10.15294/jppkmi.v1i2.40329]
32. Purwono J, Sari R, Ratnasari A, Budianto A. Salt consumption patterns with the incidence of hypertension in the elderly. J Wacana Kesehatan. 2020;5(1):531-42. [Indonesian] [Link] [DOI:10.52822/jwk.v5i1.120]
33. Agustina R, Raharjo BB. Risk factors related to the incidence of hypertension of productive age (25-54 years). Unnes Journal of Public Health. 2015;4(4):146-158. [Indonesian] [Link] [DOI:10.15294/ujph.v4i4.9690]
34. Yulistina F, Deliana SM, Rustiana ER. Correlation of food intake, stress, and physical activity with hypertension in menopausal age. Unnes J Public Health. 2017;6(1):35-42. [Indonesian] [Link] [DOI:10.15294/ujph.v6i1.13695]
35. Jayanti IGAN, Wiradnyani NK, Ariyasa IG. The relationship between the pattern of alcoholic beverage consumption and the incidence of hypertension in the tourism workforce in Legian Village. Indones J Nutr. 2017;6(1):65-70. [Link] [DOI:10.14710/jgi.6.1.65-70]
36. Rita S. Factors affecting hypertension at Dr. Rm. Djoelham Hospital, Binjai City. J Publikasi Kesehatan Masyarakat Indonesia. 2017;4(3):6. [Indonesian] [Link] [DOI:10.20527/jpkmi.v4i3.4323]
37. Putri SM. Dominant factors in blood pressure of people with hypertension. J Media Kesehatan. 2017;10(1):31-40. [Indonesian] [Link]
38. Yuriah A, Astuti AT, Inayah I. The relationship between fat intake, fiber and the ratio of hip waist circumference to blood pressure of hypertensive patients at the Gondokusuman I Health Center in Yogyakarta. Ilmu Gizi Indonesia. 2019;2(2):115-24. [Indonesian] [Link] [DOI:10.35842/ilgi.v2i2.103]