Volume 14, Issue 4 (2022)
Iran J War Public Health 2022, 14(4): 455-464 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2022/08/24 | Accepted: 2022/12/10 | Published: 2022/12/19
Received: 2022/08/24 | Accepted: 2022/12/10 | Published: 2022/12/19
How to cite this article
Gharibi F, Imani A, Haghi M, Dalal K. Relationship between Political-Economic Sanctions and Catastrophic Health Costs in Multiple Sclerosis Patients in Iran. Iran J War Public Health 2022; 14 (4) :455-464
URL: http://ijwph.ir/article-1-1223-en.html
URL: http://ijwph.ir/article-1-1223-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
1- “Social Determinants of Health Research Center” and “Department of Community Medicine, Faculty of Medicine”, Semnan University of Medical Sciences, Semnan, Iran
2- Department of Health Economics, School of Management and Medical Informatics, Tabriz University of Medical Sciences, Tabriz, Iran
3- “Social Determinants of Health Research Center” and “Department of Public Health, Faculty of Health and Nutrition”, Lorestan University of Medical Sciences, Khorramabad, Iran
4- Department of Public Health Science, School of Health Sciences, Mid Sweden University, Sundsvall, Sweden
2- Department of Health Economics, School of Management and Medical Informatics, Tabriz University of Medical Sciences, Tabriz, Iran
3- “Social Determinants of Health Research Center” and “Department of Public Health, Faculty of Health and Nutrition”, Lorestan University of Medical Sciences, Khorramabad, Iran
4- Department of Public Health Science, School of Health Sciences, Mid Sweden University, Sundsvall, Sweden
Full-Text (HTML) (621 Views)
Introduction
One of the health systems' leading roles is to protect their citizens against health costs and prevent them from incurring health-related financial problems by creating a fair financing system. In such a system, all citizens receive the health services they need but pay for them according to their economic affordability. Special attention is paid to more vulnerable people in such a system due to having a non-communicable and incurable disease with low financial affordability [1, 2].
Studies have shown that most low- and middle-income countries have failed to create a fair financing system [3, 4]. Due to the lack of development of pre-payment insurance systems in these countries, out-of-pocket payments are higher than 15-20%, recommended by World Health Organization (WHO) [5, 6]. WHO also estimates that 150 million people face grave financial problems each year due to unfair health payments, and 100 million fall into poverty annually [2]. To cover their health expenses, these poor people borrow and sell their assets or refuse to receive the necessary health care, and Catastrophic Health Expenditure (CHE) occurs [7].
The CHE is defined as "spending health care over household payment capacity" [8]. The CHE rate varies from 1 to 15 per cent in different countries, and people with chronic, debilitating and incurable diseases will be more likely to face it [9, 10].
Multiple Sclerosis (MS) is a complex inflammatory disease that affects the central nervous system, resulting in muscle stiffness, diplopia, sensory loss, limb weakness, gait ataxia, loss of bladder control, epilepsy, functional impairment and disability and several [11]. The chronic and debilitating nature of MS has a significant and devastating effect on patients' economic, social, and healthcare issues. The catastrophic effects of MS are not limited to patients but to the family of patients, the health system, insurance and third-party payers and, in general, the community [11].
Considering that one of the primary responsibilities of the health systems is to safeguard patients against healthcare costs and that MS patients face difficulty making a living due to progressive physical and mental disabilities, it is evident that the financial protection of MS patients is of paramount importance [7, 11]. However, the Iranian health system cannot provide adequate support to patients with many diseases, such as MS. One of these reasons is the imposition of political, financial, and health sanctions against this country [12]. The leading cause of CHE and impoverishment due to health costs is the lack of financial protection of the health system (main lack of proper health insurance) for vulnerable patients and their households [13, 14]. Other causes of enhancing health costs are overuse because of occurring induction demands and non-compliance with treatment protocol in prescribing [15], and informal payment to health providers from caregivers [16, 17]. The higher rate of Out-of-pocket Payments (OOPs), CHE and poverty result in more economic pressure on patients and families through disease costs and problems in receiving required healthcare services. These events can lead to a notable decrease in health outcomes of MS patients and remarkable diminish in living standards in households with MS patients [7, 18].
The modern world uses economic sanctions as an alternative way to the former army-initiated territory-occupying strategy [19]. Countries and sanctions enforcement agencies claim that sanctions are cost-effective, low-aggressive, feasible, and peaceful to exert pressure [20]. However, studies indicate that sanctions have widespread vicious effects on various sectors of the sanctioned societies, people's lives, and well-being, especially health and healthcare [21, 22]. Iran has faced several sanctions resulting from low national revenues, non-realization of revenues, a dramatic increase in the inflation rate, and a high unemployment rate [23]. These problems, together, diminish people's well-being and their inability to access living standards such as nutrition and healthcare; but the sanction enforcement countries and agencies claim that the health sector, especially medicine and medical equipment, is exempted and safe from sanctions [23]. Nevertheless, the truth of these claims has never been checked objectively and with reliable indicators.
In May 2018, Iran faced a recent nuclear sanction. Following the return of sanctions, the health status of the Iranian people was threatened in many ways [12]. These sanctions have had a devastating impact on the public's health and access to medicines, equipment, and healthcare. The sanction, in particular, affects more than 6 million patients with non-communicable diseases [24].
To the best of the authors' knowledge, no previous study has examined the impact of political-economic sanctions on the OOPs and Catastrophic Health Expenditures (CHE) incurred by patients with MS or other diseases worldwide [25, 26]. It is crucial to assess the probable negative impacts of sanctions, especially on non-communicable and disabling diseases [27]. However, the effects of sanctions are not well explored [28].
MS is one of the important non-communicable diseases, which CHE rate in patients affected by it was investigated before the return of sanctions, so the applied changes in this indicator could indicate the effects of sanctions return [7, 13]. The present study aimed to investigate the association of political-economic sanctions with the CHE of MS patients in Iran.
Instruments and Methods
Design
This is a before-after study that was conducted on 300 MS patients residing in the East Azerbaijan province of Iran. We have asked those 300 MS patients questions at the pre-sanctions (April-May 2018) and post-sanctions (April-May 2019) phases. Given that the incurred sanctions affected all patients with MS and their families simultaneously countrywide, we could not assign any control group. In May 2018, a survey was conducted to estimate the OOPs and CHE of MS patients and their families. Immediately after the data collection, the current sanctions were imposed on Iran. One year later, in May 2019, the research team conducted another survey with the same group of MS patients. We used pre- and post-survey to compare sanctions results, estimating both OOPs and CHE of the MS patients.
Participants
The study population included all MS patients registered in the MS Association (MSA) of the East Azerbaijan province, Iran. There were two inclusion criteria in the initial study phase (May 2018): having a medical record in the MSA of East Azerbaijan province and being treated for at least one year. The MSA registry has a total of 1200 MS patients. Using Morgan's table, the final sample size included 300 patients [29]. Therefore, in the first phase of the study, 300 patients were randomly selected and evaluated. In the final phase (post-survey), the same number of participants were included. However, 12 patients were removed from the second phase of the study due to different problems: two patients died, two patients migrated or were out of reach, three patients did not answer the calls, and five patients refused to participate. Finally, the second survey was conducted with 288 participants. At the data collection phase, the healthcare expenditures of the MS patients and their families in the past year were assessed and calculated through a combination of methods, including assessing the health records, analyzing the bills, and conducting patient interviews.
Instruments
The health condition of patients was assessed as the quality of life based on The Expanded Disability Status Scale (EDSS) scale. The EDSS assess the health status/condition of patients with MS by measuring their physical function/mobility and independency in implementing the daily activity. The EDSS score for each patient with MS varies from 1 to 10 (scores of 1 and 10 refer to the worst and best health condition, respectively). The EDSS score of the patients in the before and after phase of levied nuclear sanctions was 3.14 and 3.08, respectively, and their difference was not significant statistically (p=0.794). It means that the probable rising of OOPs and CHE will not be related to the deterioration of the health status of assessed patients.
A pre-tested questionnaire was used to collect the data on OOPs, other living expenses of patients and their families, and many demographic and background variables. The collaboration of 10 experts evaluated the questionnaire's content validity and face validity in relevance, transparency, simplicity, necessity, and measurability. First, the average Content Validity Ratio (CVR) for the necessity index was evaluated. After validating this index's questions, the mean Content Validity Index (CVI) of four other indexes was confirmed [7]. Accordingly, the acceptance score of 70% was chosen as the criterion for decision-making due to the ten experts' participation. In this study, the scores for CVR and CVI were 88.5% and 92%, respectively. The questionnaire contained demographic/ background variables regarding MS patients, the various imposed costs on them to get required healthcare, their household income and costs, and their perspective regarding financial pressure by health costs on them.
Controlling for confounding variables
The main potential confounding variables in similar studies are the occurring change in background/demographic variables, which in this study, they were controlled by selecting the same participants before and after phases, and shortening the time between two study phases. Another probable confounding variable was the change in patients' quality of life, which was assessed using the EDSS score, and the statistical differences were not seen between the before and after phases of imposing sanctions. Also, the insurance covering rate was not changed before and after sanctions because all of the MS patients had basic health insurance, and the percentage of patients with supplemental insurance was not changed too. In addition, the specific health care program was not conducted for MS patients in this period, and the Iran health reform plan as the leading health program was conducted is such time completely. The last item is the template of treatment, which was not able to change because the treatment process and pattern of MS patients in Iran are standardized and implemented based on approved treatment protocols and guidelines. The sanction was not the confounding variable because it is the main primary effect of sanctions, which led to items such as unemployment, scarcity of medicine, and finally occurring CHE, as the last effect of sanctions.
Statistical calculations
The occurring diseases, especially the non-communicable and disabling diseases, incur several costs on patients and their households. These costs are dividing direct medical costs (for investigation, treatment, and rehabilitation), direct non-medical costs (for transportation, nutrition, and settlement of caregiving period; physical space adjustments, aiding in personal works, etc.), and indirect costs (the opportunity cost). The CHE is calculated based on OOPs, therefore it is related to direct medical costs. Direct medical costs are the costs that are incurred by the patients or the community for healthcare-related issues. The direct medical costs refer to all the costs associated with diagnosis, treatment, and rehabilitation of the patients (including physician visits, diagnostic services, medicine, surgery, hospitalization, supplemental and alternative care, home care, physiotherapy services, occupational therapy, etc.), which are the basis for calculating OOPs, and consequently, the CHE and the resulting poverty in this study [30, 31].
The descriptive part reported survey results by frequency (percentage), mean, and standard deviation. All costs of the MS disease were calculated and summed as the total annual cost imposed on patients. An exchange rate (1 USD= 42,000 IRR), announced by the Central Bank of Iran, was used. Spending at least 40% of the family income (non-food costs) on health care issues is regarded as CHE [32]. Also, if health costs exceed 50% of non-food costs, the existing poverty is regarded as a consequence of severe health costs [33]. The reason for choosing these methods and their related thresholds in this study is that the calculation methods of assessing CHE were proposed by WHO and widely used methods by researchers [27, 34].
The following formula was used to calculate catastrophic costs:
Catastrophic HCEh= Health E>40%CTP
The household's ability to pay was calculated as follows:
Ctph = exph – seh if seh <= foodh
Student's t-test (for two-state variables including gender), analysis of variance /ANOVA (for multi-state variables such as educational level), and linear regression (for quantitative variables including the age of disease onset) were used to assess the statistical relationship between "out-of-pocket payments" with demographical and background variables. The chi-square test was used to assess the statistical relationship between occurring "catastrophic health expenditure" and "poverty resulting from costs" with qualitative variables (two
and multi-state variables). In addition, the paired t-test and chi-square tests were used for two-state (such as occurring catastrophic expenditure) and multi-state (such as the source of funding) outcomes to assess the significance of occurred changes in outcomes before and after sanction, respectively. All analyses were performed using SPSS 18 software, and a p-value less than 0.05 was considered significant.
Findings
Characteristics of the participants
The average age of patients was 37.15±9.68 years, and 68% of them were female. The mean age of disease onset was 27.18±7.64 years. On average, 9.95±7.06 years have passed since the diagnosis of MS. Almost two-thirds (63%) of the patients were married. Half of the respondents (50.7%) were household women. 855% of patients were natives of Tabriz. Among the respondents, 42.7% had an academic education. Although 100% of patients had basic health insurance, only 36.4% had supplemental insurance.
Out-of-pocket payments (OOPs)
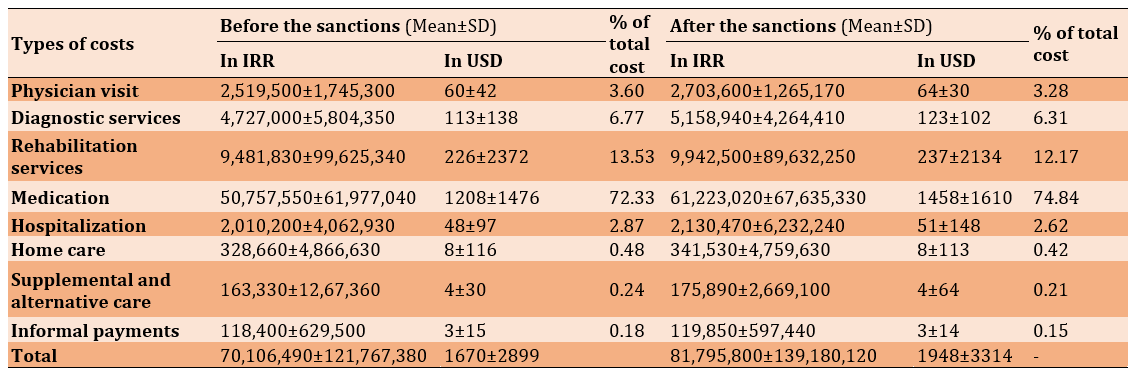
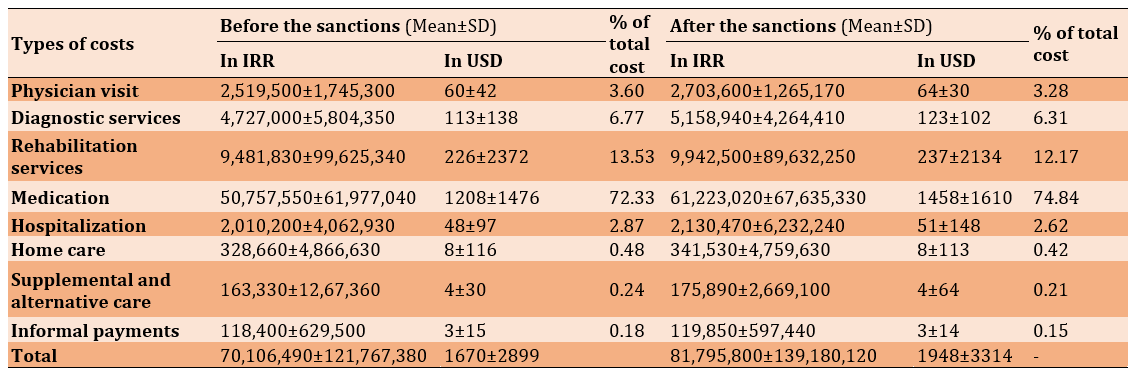
The average OOPs by patients for receiving health care, such as physician visits, diagnostic services, rehabilitation services, medications, hospitalization, home care, complementary and alternative therapies, and informal payments to individuals or centers in the pre-sanctions phase, was about 70 million IRR. This amount had increased by14.3% and reached about 82 million IRR in the post-sanctions phase. Most of the OOPs were spent on medication, rehabilitation care, and diagnostic services, respectively (Table 1). The most significant increase in the OOPs was related to the rising prices of medicines, particularly the Betaferon ampoule. This ampoule price had increased by more than 17.5% (from 8,000,000 IRR/190.47 USD to 9,400,000 IRR/223.91 USD).
Studies have shown that most low- and middle-income countries have failed to create a fair financing system [3, 4]. Due to the lack of development of pre-payment insurance systems in these countries, out-of-pocket payments are higher than 15-20%, recommended by World Health Organization (WHO) [5, 6]. WHO also estimates that 150 million people face grave financial problems each year due to unfair health payments, and 100 million fall into poverty annually [2]. To cover their health expenses, these poor people borrow and sell their assets or refuse to receive the necessary health care, and Catastrophic Health Expenditure (CHE) occurs [7].
The CHE is defined as "spending health care over household payment capacity" [8]. The CHE rate varies from 1 to 15 per cent in different countries, and people with chronic, debilitating and incurable diseases will be more likely to face it [9, 10].
Multiple Sclerosis (MS) is a complex inflammatory disease that affects the central nervous system, resulting in muscle stiffness, diplopia, sensory loss, limb weakness, gait ataxia, loss of bladder control, epilepsy, functional impairment and disability and several [11]. The chronic and debilitating nature of MS has a significant and devastating effect on patients' economic, social, and healthcare issues. The catastrophic effects of MS are not limited to patients but to the family of patients, the health system, insurance and third-party payers and, in general, the community [11].
Considering that one of the primary responsibilities of the health systems is to safeguard patients against healthcare costs and that MS patients face difficulty making a living due to progressive physical and mental disabilities, it is evident that the financial protection of MS patients is of paramount importance [7, 11]. However, the Iranian health system cannot provide adequate support to patients with many diseases, such as MS. One of these reasons is the imposition of political, financial, and health sanctions against this country [12]. The leading cause of CHE and impoverishment due to health costs is the lack of financial protection of the health system (main lack of proper health insurance) for vulnerable patients and their households [13, 14]. Other causes of enhancing health costs are overuse because of occurring induction demands and non-compliance with treatment protocol in prescribing [15], and informal payment to health providers from caregivers [16, 17]. The higher rate of Out-of-pocket Payments (OOPs), CHE and poverty result in more economic pressure on patients and families through disease costs and problems in receiving required healthcare services. These events can lead to a notable decrease in health outcomes of MS patients and remarkable diminish in living standards in households with MS patients [7, 18].
The modern world uses economic sanctions as an alternative way to the former army-initiated territory-occupying strategy [19]. Countries and sanctions enforcement agencies claim that sanctions are cost-effective, low-aggressive, feasible, and peaceful to exert pressure [20]. However, studies indicate that sanctions have widespread vicious effects on various sectors of the sanctioned societies, people's lives, and well-being, especially health and healthcare [21, 22]. Iran has faced several sanctions resulting from low national revenues, non-realization of revenues, a dramatic increase in the inflation rate, and a high unemployment rate [23]. These problems, together, diminish people's well-being and their inability to access living standards such as nutrition and healthcare; but the sanction enforcement countries and agencies claim that the health sector, especially medicine and medical equipment, is exempted and safe from sanctions [23]. Nevertheless, the truth of these claims has never been checked objectively and with reliable indicators.
In May 2018, Iran faced a recent nuclear sanction. Following the return of sanctions, the health status of the Iranian people was threatened in many ways [12]. These sanctions have had a devastating impact on the public's health and access to medicines, equipment, and healthcare. The sanction, in particular, affects more than 6 million patients with non-communicable diseases [24].
To the best of the authors' knowledge, no previous study has examined the impact of political-economic sanctions on the OOPs and Catastrophic Health Expenditures (CHE) incurred by patients with MS or other diseases worldwide [25, 26]. It is crucial to assess the probable negative impacts of sanctions, especially on non-communicable and disabling diseases [27]. However, the effects of sanctions are not well explored [28].
MS is one of the important non-communicable diseases, which CHE rate in patients affected by it was investigated before the return of sanctions, so the applied changes in this indicator could indicate the effects of sanctions return [7, 13]. The present study aimed to investigate the association of political-economic sanctions with the CHE of MS patients in Iran.
Instruments and Methods
Design
This is a before-after study that was conducted on 300 MS patients residing in the East Azerbaijan province of Iran. We have asked those 300 MS patients questions at the pre-sanctions (April-May 2018) and post-sanctions (April-May 2019) phases. Given that the incurred sanctions affected all patients with MS and their families simultaneously countrywide, we could not assign any control group. In May 2018, a survey was conducted to estimate the OOPs and CHE of MS patients and their families. Immediately after the data collection, the current sanctions were imposed on Iran. One year later, in May 2019, the research team conducted another survey with the same group of MS patients. We used pre- and post-survey to compare sanctions results, estimating both OOPs and CHE of the MS patients.
Participants
The study population included all MS patients registered in the MS Association (MSA) of the East Azerbaijan province, Iran. There were two inclusion criteria in the initial study phase (May 2018): having a medical record in the MSA of East Azerbaijan province and being treated for at least one year. The MSA registry has a total of 1200 MS patients. Using Morgan's table, the final sample size included 300 patients [29]. Therefore, in the first phase of the study, 300 patients were randomly selected and evaluated. In the final phase (post-survey), the same number of participants were included. However, 12 patients were removed from the second phase of the study due to different problems: two patients died, two patients migrated or were out of reach, three patients did not answer the calls, and five patients refused to participate. Finally, the second survey was conducted with 288 participants. At the data collection phase, the healthcare expenditures of the MS patients and their families in the past year were assessed and calculated through a combination of methods, including assessing the health records, analyzing the bills, and conducting patient interviews.
Instruments
The health condition of patients was assessed as the quality of life based on The Expanded Disability Status Scale (EDSS) scale. The EDSS assess the health status/condition of patients with MS by measuring their physical function/mobility and independency in implementing the daily activity. The EDSS score for each patient with MS varies from 1 to 10 (scores of 1 and 10 refer to the worst and best health condition, respectively). The EDSS score of the patients in the before and after phase of levied nuclear sanctions was 3.14 and 3.08, respectively, and their difference was not significant statistically (p=0.794). It means that the probable rising of OOPs and CHE will not be related to the deterioration of the health status of assessed patients.
A pre-tested questionnaire was used to collect the data on OOPs, other living expenses of patients and their families, and many demographic and background variables. The collaboration of 10 experts evaluated the questionnaire's content validity and face validity in relevance, transparency, simplicity, necessity, and measurability. First, the average Content Validity Ratio (CVR) for the necessity index was evaluated. After validating this index's questions, the mean Content Validity Index (CVI) of four other indexes was confirmed [7]. Accordingly, the acceptance score of 70% was chosen as the criterion for decision-making due to the ten experts' participation. In this study, the scores for CVR and CVI were 88.5% and 92%, respectively. The questionnaire contained demographic/ background variables regarding MS patients, the various imposed costs on them to get required healthcare, their household income and costs, and their perspective regarding financial pressure by health costs on them.
Controlling for confounding variables
The main potential confounding variables in similar studies are the occurring change in background/demographic variables, which in this study, they were controlled by selecting the same participants before and after phases, and shortening the time between two study phases. Another probable confounding variable was the change in patients' quality of life, which was assessed using the EDSS score, and the statistical differences were not seen between the before and after phases of imposing sanctions. Also, the insurance covering rate was not changed before and after sanctions because all of the MS patients had basic health insurance, and the percentage of patients with supplemental insurance was not changed too. In addition, the specific health care program was not conducted for MS patients in this period, and the Iran health reform plan as the leading health program was conducted is such time completely. The last item is the template of treatment, which was not able to change because the treatment process and pattern of MS patients in Iran are standardized and implemented based on approved treatment protocols and guidelines. The sanction was not the confounding variable because it is the main primary effect of sanctions, which led to items such as unemployment, scarcity of medicine, and finally occurring CHE, as the last effect of sanctions.
Statistical calculations
The occurring diseases, especially the non-communicable and disabling diseases, incur several costs on patients and their households. These costs are dividing direct medical costs (for investigation, treatment, and rehabilitation), direct non-medical costs (for transportation, nutrition, and settlement of caregiving period; physical space adjustments, aiding in personal works, etc.), and indirect costs (the opportunity cost). The CHE is calculated based on OOPs, therefore it is related to direct medical costs. Direct medical costs are the costs that are incurred by the patients or the community for healthcare-related issues. The direct medical costs refer to all the costs associated with diagnosis, treatment, and rehabilitation of the patients (including physician visits, diagnostic services, medicine, surgery, hospitalization, supplemental and alternative care, home care, physiotherapy services, occupational therapy, etc.), which are the basis for calculating OOPs, and consequently, the CHE and the resulting poverty in this study [30, 31].
The descriptive part reported survey results by frequency (percentage), mean, and standard deviation. All costs of the MS disease were calculated and summed as the total annual cost imposed on patients. An exchange rate (1 USD= 42,000 IRR), announced by the Central Bank of Iran, was used. Spending at least 40% of the family income (non-food costs) on health care issues is regarded as CHE [32]. Also, if health costs exceed 50% of non-food costs, the existing poverty is regarded as a consequence of severe health costs [33]. The reason for choosing these methods and their related thresholds in this study is that the calculation methods of assessing CHE were proposed by WHO and widely used methods by researchers [27, 34].
The following formula was used to calculate catastrophic costs:
Catastrophic HCEh= Health E>40%CTP
The household's ability to pay was calculated as follows:
Ctph = exph – seh if seh <= foodh
Student's t-test (for two-state variables including gender), analysis of variance /ANOVA (for multi-state variables such as educational level), and linear regression (for quantitative variables including the age of disease onset) were used to assess the statistical relationship between "out-of-pocket payments" with demographical and background variables. The chi-square test was used to assess the statistical relationship between occurring "catastrophic health expenditure" and "poverty resulting from costs" with qualitative variables (two
and multi-state variables). In addition, the paired t-test and chi-square tests were used for two-state (such as occurring catastrophic expenditure) and multi-state (such as the source of funding) outcomes to assess the significance of occurred changes in outcomes before and after sanction, respectively. All analyses were performed using SPSS 18 software, and a p-value less than 0.05 was considered significant.
Findings
Characteristics of the participants
The average age of patients was 37.15±9.68 years, and 68% of them were female. The mean age of disease onset was 27.18±7.64 years. On average, 9.95±7.06 years have passed since the diagnosis of MS. Almost two-thirds (63%) of the patients were married. Half of the respondents (50.7%) were household women. 855% of patients were natives of Tabriz. Among the respondents, 42.7% had an academic education. Although 100% of patients had basic health insurance, only 36.4% had supplemental insurance.
Out-of-pocket payments (OOPs)
The average OOPs by patients for receiving health care, such as physician visits, diagnostic services, rehabilitation services, medications, hospitalization, home care, complementary and alternative therapies, and informal payments to individuals or centers in the pre-sanctions phase, was about 70 million IRR. This amount had increased by14.3% and reached about 82 million IRR in the post-sanctions phase. Most of the OOPs were spent on medication, rehabilitation care, and diagnostic services, respectively (Table 1). The most significant increase in the OOPs was related to the rising prices of medicines, particularly the Betaferon ampoule. This ampoule price had increased by more than 17.5% (from 8,000,000 IRR/190.47 USD to 9,400,000 IRR/223.91 USD).
Table 1) Status of out-of-pocket payments in patients under study (before and after sanction phases)
Income status of patients and how to spend it
An examination of MS patients and their families income status showed that families' average annual income increased by 8.74% (from 217,679,590 IRR to 236,704,780 IRR), mainly due to a 10% increase in the salaries of the employed individuals. In the pre-sanctions phase, households spent an average of 32% (69,745,360 IRR) of their annual income on food costs and 68% (150,662,410 IRR) on non-food expenditures. However, after sanctions, there was an explosive increase in the costs due to the dramatic decline of the Iranian Rial and the increase in the US Dollar price (1USD=40,000 IRR Vs.1USD=130,000 IRR even 1USD=210,000 IRR in a short period). As a result (Table 2), while the share of food costs increased by approximately 55% (131,818,730 IRR), the share of non-food costs decreased by about 45% (102,842,160 IRR).
Negative consequences of costs
The sanctions resulted in a 15% increase in the CHE (from 54% to 69%) and a 14% increase in disease-related poverty (from 44% to 58%). Moreover, variables such as "delay in receiving health services or not receiving care due to high costs," "preferring low-quality services over expensive high-quality services," and "receiving loans or grants from individuals or organizations for treatment" increased after sanctions by 5%, 6%, and 14%, respectively. The pressure on the patients and families to cover the disease costs increased significantly. In the absence of adequate support from governmental or non-governmental organizations, the patients or their families had to sell their assets or borrow from individuals and banks to cover the disease costs. The levied sanctions led to a significant increase in the majority of outcome measures, including catastrophic health expenditures, poverty resulting from health care costs, delay in receiving services or not receiving care due to high costs, receiving low-quality services due to high costs of high quality services, obtaining loans or grants from individuals or organizations for MS treatment and the amount of pressure on patients and families to cover the costs of the disease (p<0.05; Table 3).
Income status of patients and how to spend it
An examination of MS patients and their families income status showed that families' average annual income increased by 8.74% (from 217,679,590 IRR to 236,704,780 IRR), mainly due to a 10% increase in the salaries of the employed individuals. In the pre-sanctions phase, households spent an average of 32% (69,745,360 IRR) of their annual income on food costs and 68% (150,662,410 IRR) on non-food expenditures. However, after sanctions, there was an explosive increase in the costs due to the dramatic decline of the Iranian Rial and the increase in the US Dollar price (1USD=40,000 IRR Vs.1USD=130,000 IRR even 1USD=210,000 IRR in a short period). As a result (Table 2), while the share of food costs increased by approximately 55% (131,818,730 IRR), the share of non-food costs decreased by about 45% (102,842,160 IRR).
Negative consequences of costs
The sanctions resulted in a 15% increase in the CHE (from 54% to 69%) and a 14% increase in disease-related poverty (from 44% to 58%). Moreover, variables such as "delay in receiving health services or not receiving care due to high costs," "preferring low-quality services over expensive high-quality services," and "receiving loans or grants from individuals or organizations for treatment" increased after sanctions by 5%, 6%, and 14%, respectively. The pressure on the patients and families to cover the disease costs increased significantly. In the absence of adequate support from governmental or non-governmental organizations, the patients or their families had to sell their assets or borrow from individuals and banks to cover the disease costs. The levied sanctions led to a significant increase in the majority of outcome measures, including catastrophic health expenditures, poverty resulting from health care costs, delay in receiving services or not receiving care due to high costs, receiving low-quality services due to high costs of high quality services, obtaining loans or grants from individuals or organizations for MS treatment and the amount of pressure on patients and families to cover the costs of the disease (p<0.05; Table 3).
Table 2) Annual income status and how it is spent by MS patients and their families


Table 3) Negative effects of costs incurred by patients and their families

The relationship between demographic/contextual variables with the costs and their destructive impacts
In both pre-sanctions and post-sanctions phases, among the variables under study, only occupational status, having supplemental insurance, and being native had a significant impact on the amount of OOPs, CHE, or poverty resulting from the disease costs (Table 4).
The rate of CHE was low for public-sector employees, the average for pensioners and homemakers, and very high for unemployed and university students (p<0.05). Also, there was a significant relationship between having supplemental insurance and CHE and the poverty resulting from MS disease costs, so those with supplemental insurance were significantly less affected than those without supplemental insurance (p<0.05). Also, native patients had fewer OOPs compared to non-native patients. (Tables 5
and 6).

The relationship between demographic/contextual variables with the costs and their destructive impacts
In both pre-sanctions and post-sanctions phases, among the variables under study, only occupational status, having supplemental insurance, and being native had a significant impact on the amount of OOPs, CHE, or poverty resulting from the disease costs (Table 4).
The rate of CHE was low for public-sector employees, the average for pensioners and homemakers, and very high for unemployed and university students (p<0.05). Also, there was a significant relationship between having supplemental insurance and CHE and the poverty resulting from MS disease costs, so those with supplemental insurance were significantly less affected than those without supplemental insurance (p<0.05). Also, native patients had fewer OOPs compared to non-native patients. (Tables 5
and 6).
Table 4) Relationship between demographic and contextual variables and disease costs and their impacts
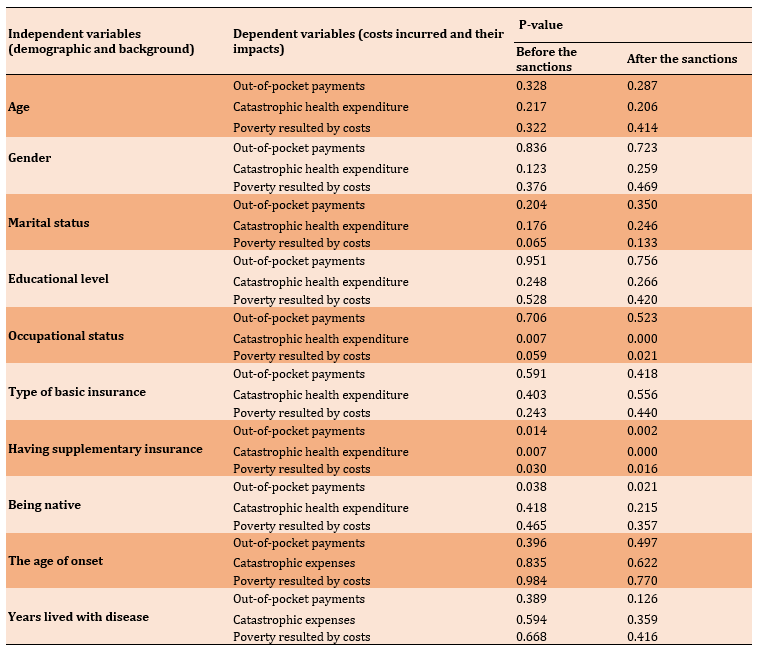
Table 5) Relationship of demographic/background variable with CHE and poverty resulting from health care costs

Table 6) Relationship of demographic/background variables with OOPs

Discussion
The present study was conducted to investigate the association of Iran sanctions with the health costs of MS patients in Iran. The average OOPs by patients for receiving health care in the pre-sanctions phase was about 70 million IRR, but this amount had increased by 14.3% and reached about 82 million IRR in the post-sanctions phase. Meanwhile, food costs increased by 23% with the return of sanctions, but the share of non-food costs decreased by 25% for MS patients. It could be a severe increase in living costs due to a massive decline in the value of the Iranian Rial. The IRR value of one US dollar ranged from 42,000 IRR (before sanctions) to about 140,000 IRR, and even 210,000 IRR at specific points (after sanctions), resulting in a more than 300% drop in the purchasing power of the IRR, Iranian national currency. As a result, all living costs increased, and MS patients and their families had to spend their income mainly on essential needs such as food, housing, and healthcare. Meanwhile, some other problems emerged, such as a higher unemployment rate, a significant decline in production, and a sharp inflation rate. However, this was not a new phenomenon for Iranians. For example, the sanctions imposed on Iran in 2012 resulted in an 11.8% decline in Gross Domestic Product (GDP), a 40% increase in the inflation rate and a 200% drop in Rial price compared to 2011. All of this led to an increase in the cost of living and unemployment [35]. Conversely, in the first year after the agreement was signed in 2015, GDP in Iran increased by 14.1% [35]. It is important to note that numerous rounds of sanctions over the past four decades have had a devastating effect on the Iranian economy and subsequently, Iranian citizens, so that the dollar price has risen from 69 IRR in 1979 to about 160,000 IRR in early 2020.
After the imposition of sanctions, its short and long-term destructive consequences appear. Immediately after imposing sanctions on a country, many essential medications become inaccessible, and even local medication production is grossly hampered by a lack of necessary raw materials and manufacturing equipment. In such circumstances, medicine prices rise sharply so that people with average and low incomes fail to afford healthcare costs [36], leading to the expansion of black markets and even the production of counterfeit medicines. The consequent black market also includes all non-pharmaceutical equipment and materials [19]. The widespread destructive effects of economic sanctions on population health are particularly critical in malnutrition and lack of access to essential healthcare services [37]. In such a situation, vulnerable groups such as the poor, patients, women, the elderly, and especially children suffer the most [23]. Sanctions also harm social determinants of health, which lead to a decline in the overall health level of the sanctioned societies, causing inequality and widening the gap in healthcare utilization among the citizens [35]. As a result, many people may die silently from various diseases, and war crimes occur [19].
Since the current sanctions (May 2018), OOPs have risen by 14.3%, leading to an increase in medication prices, especially for Betaferon. Medication prices increase due to a shortage in raw materials and a drop in the Iranian currency value. Surveys show that 73 types of pharmaceutical products are in short supply due to sanctions, 44% of which have been identified as essential according to a list published by WHO [38]. The following examples are some of the damaging effects of sanctions: in asthmatic patients, 19% and 42% reduction in imported and internally manufactured medications, respectively [39], and a fourteen-fold increase in the price of the dietary formula for allergic infants [12]. The return of sanctions resulted in a 15% CHE increase (54% to 69%) and a 14% increase in disease-driven poverty (44% to 58%). We get some crucial concerns such as "delay in receiving services or not receiving care due to high costs," "preferring low-quality services over high-quality ones," and "receiving loans or grants from individuals or organizations for the treatment of disease".
Generally, some demographic and background variables may lead to the protection of patients against CHE or accelerate its occurrence. Assessing the statistical relationship between demographic and background variables and the amount of OOPs, and the impact of CHE on patients and their families showed that in both pre-sanctions and post-sanctions phases, among the variables under study, only occupational status, having supplemental insurance, and being native had a significant impact on the amount of OOPs, CHE, or the poverty resulted by the disease costs. Undoubtedly, the leading cause of this situation is the severe drop in the Iranian Rial and the refusal of pharmaceutical companies and international banks to cooperate and deal with Iran for fear of US sanctions on them [38]. CHE and poverty due to high OOPs in Iran are mainly related to the imposed international political and financial sanctions. Undoubtedly, the sanctions were the leading cause of this situation for many direct and indirect adverse health and economic effects. The sanction affects the government's ability, and consequently, health systems to have proper support from patients and their households.
Although the Iranian health system has always provided patients with the necessary subsidies and medicines, these measures were insufficient. Also, access to essential care became more difficult for patients because of the widespread sanctions, especially financially. One of the main reasons for this problem is the lack of an efficient basic health insurance system and government support to expand supplemental insurance effectively [12, 40, 41]. The unilateral US sanctions on Iran have even caused severe problems for the Iranian Red Crescent, so this non-governmental humanitarian organization failed to timely access equipment, medications, and food sent by international organizations during times of crisis [38]. For example, during the nationwide 2019 floods that hit many cities in Iran, the following problems emerged as the result of the current sanctions: a shortage in the number of helicopters and relief boats, severe restrictions on receiving relief supplies and purchasing health kits from countries, inability to get financial aids from other countries, and the delayed entry of non-monetary relief items into Iran [12, 42].
The devastating effects of international sanctions have evident several detrimental effects on Iran and other countries. The following health issues are the results of war, and sanctions levied on Iraq in ten years: the mortality rate of less than one-year-old infants increased from 47 to 108 per 1000 live births; the mortality rate of less than 5-year-old children increased from 56 to 131 per 1000 live births; the acute malnutrition rate increased from 3% to 11%; the number of infants born with Low Birth Weight (LBW; <2.5 kg) increased from 4% to 25% due to malnutrition of 70% of the mothers; the access to safe drinking water reduced from 90% and 70% in cities and villages to 50% and 33%, respectively [43]. Interestingly, immediately after lifting some sanctions and introducing the oil-for-food program, these indicators, particularly infant mortality, began to decline significantly [43]. The devastating effects of the sanctions on patients with such diseases as HIV, diabetes, kidney failure, and cancer, along with the severe weakening of children's vaccination program due to the lack of access to equipment and medications in Venezuela, resulted in the death of more than 40,000 Venezuelan citizens between the years 2017 and 2018 [44]. Some other examples of the devastating effects of the sanctions on countries' public health include a 15% increase in the death rate of older people over a year in Cuba and a 15% and 30% increase in overall mortality and hospital deaths, respectively, in Yugoslavia [22]. Similar health disasters are occurring again in Syria, Yemen, and Gaza due to wars and sanctions [37, 45, 46]. Despite the claim that economic sanctions are a peaceful alternative to war, the examples presented in this study showed that this claim does not seem to be true [20], and the sanctions can also have similar and even wider destructive health consequences due to their broad scope and long active period. Imposing sanctions on countries violates people's right to access healthcare services easily [23].
One of the main strengths of the present study is its novelty, as it is the first article in the world to explicitly examine the economic and health impacts of sanctions on patients with a disease and their families. The primary study limitations in all CHE studies are the recall period and the number of cost elements used in the study instrument [47]. Due to the lack of comprehensive and illustrative health records (as clinical/managerial information systems) for patients with MS in Iran, we used a combination of possible approaches to access the patients' financial and clinical information, especially their health services utilization and costs, including assessing health records, analyzing the bills, conducting patient interviews, and comparing obtained results from this approaches. To cope with the existing limitation of assessing costing items, we developed a comprehensive questionnaire and standardized them on the expert's opinion and advice. The last limitation of this study is the impossibility to have a control group due to imposing sanctions on all country populations and its wide negative consequences on various parts of community.
Based on the current results, the study recommends that well-reputed international organizations such as the United Nations, WHO, UNICEF, and the International Monetary Fund (IMF) carefully examine the impact of sanctions on countries in priority areas such as public health and vulnerable groups of societies, and predict the potential problems and provide effective solutions. Meanwhile, sanctioned countries should do their best to protect the health of all, especially vulnerable people and groups, especially by promoting an efficient insurance system and moving towards self-sufficiency in producing health supplies. The current study can also suggest other research on different diseases in different sanctioned countries. Those results can clearly show the harmful health effects of sanctions on international organizations and provide a rational solution.
Conclusion
Nuclear-related political-economic sanctions have devastating effects on the public health of sanctioned countries because they can seriously impede access to appropriate healthcare services through a shortage of medicines and a lack of equipment/technology and raw materials. Therefore they lead to an increase in out-of-pocket payments and a decreased ability to pay for patients with multiple sclerosis and their households. In such circumstances, international organizations must protect the citizens' rights of the sanctioned countries by protecting health issues. In addition, the government of the sanctioned country, mainly the health system and third-party payment mechanism, must protect the patients with multiple sclerosis, especially the vulnerable patients who have lost their job, do have not enough income, or have no complementary health insurance.
Acknowledgements: The researchers would like to thank all patients for their active participation in the study. Also, the research team would like to thank all the experts for their sincere collaboration in the development of the questionnaire.
Ethical Permission: The researchers observed all ethical principles. All patients were free to accept or reject participation in the study, and written informed consent was obtained from all patients. We followed the privacy codes of the patients and assured them that the study results should only be used for the defined research purposes. Furthermore, the Ethics Committee of Tabriz University of Medical Sciences approved this study (IR.TBZMED.REC.1396.101).
Conflict of Interests: The authors declare no conflict of interest.
Authors’ Contribution: Gharibi F (First Author), Introduction Writer/Methodologist/Main Researcher/Statistical Analyst/Discussion Writer (40%); Imani A (Second Author), Methodologist/Main Researcher/Statistical Analyst (20%); Haghi M (Third Author), Introduction Writer/Main Researcher/Discussion Writer (10%); Dalal K (Fourth Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer (30%)
Funding: The study was conducted by financial support of Tabriz Health Services Management Research Center.
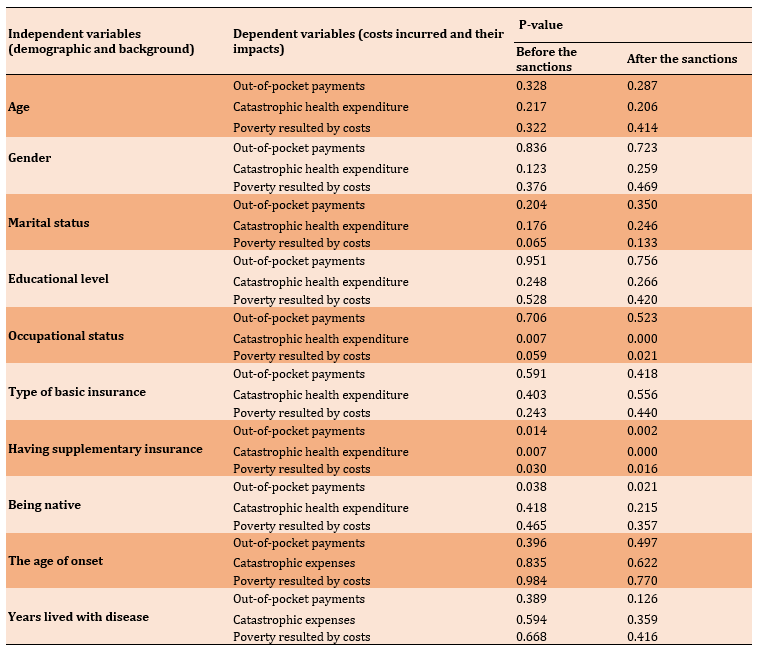
Table 5) Relationship of demographic/background variable with CHE and poverty resulting from health care costs

Table 6) Relationship of demographic/background variables with OOPs

Discussion
The present study was conducted to investigate the association of Iran sanctions with the health costs of MS patients in Iran. The average OOPs by patients for receiving health care in the pre-sanctions phase was about 70 million IRR, but this amount had increased by 14.3% and reached about 82 million IRR in the post-sanctions phase. Meanwhile, food costs increased by 23% with the return of sanctions, but the share of non-food costs decreased by 25% for MS patients. It could be a severe increase in living costs due to a massive decline in the value of the Iranian Rial. The IRR value of one US dollar ranged from 42,000 IRR (before sanctions) to about 140,000 IRR, and even 210,000 IRR at specific points (after sanctions), resulting in a more than 300% drop in the purchasing power of the IRR, Iranian national currency. As a result, all living costs increased, and MS patients and their families had to spend their income mainly on essential needs such as food, housing, and healthcare. Meanwhile, some other problems emerged, such as a higher unemployment rate, a significant decline in production, and a sharp inflation rate. However, this was not a new phenomenon for Iranians. For example, the sanctions imposed on Iran in 2012 resulted in an 11.8% decline in Gross Domestic Product (GDP), a 40% increase in the inflation rate and a 200% drop in Rial price compared to 2011. All of this led to an increase in the cost of living and unemployment [35]. Conversely, in the first year after the agreement was signed in 2015, GDP in Iran increased by 14.1% [35]. It is important to note that numerous rounds of sanctions over the past four decades have had a devastating effect on the Iranian economy and subsequently, Iranian citizens, so that the dollar price has risen from 69 IRR in 1979 to about 160,000 IRR in early 2020.
After the imposition of sanctions, its short and long-term destructive consequences appear. Immediately after imposing sanctions on a country, many essential medications become inaccessible, and even local medication production is grossly hampered by a lack of necessary raw materials and manufacturing equipment. In such circumstances, medicine prices rise sharply so that people with average and low incomes fail to afford healthcare costs [36], leading to the expansion of black markets and even the production of counterfeit medicines. The consequent black market also includes all non-pharmaceutical equipment and materials [19]. The widespread destructive effects of economic sanctions on population health are particularly critical in malnutrition and lack of access to essential healthcare services [37]. In such a situation, vulnerable groups such as the poor, patients, women, the elderly, and especially children suffer the most [23]. Sanctions also harm social determinants of health, which lead to a decline in the overall health level of the sanctioned societies, causing inequality and widening the gap in healthcare utilization among the citizens [35]. As a result, many people may die silently from various diseases, and war crimes occur [19].
Since the current sanctions (May 2018), OOPs have risen by 14.3%, leading to an increase in medication prices, especially for Betaferon. Medication prices increase due to a shortage in raw materials and a drop in the Iranian currency value. Surveys show that 73 types of pharmaceutical products are in short supply due to sanctions, 44% of which have been identified as essential according to a list published by WHO [38]. The following examples are some of the damaging effects of sanctions: in asthmatic patients, 19% and 42% reduction in imported and internally manufactured medications, respectively [39], and a fourteen-fold increase in the price of the dietary formula for allergic infants [12]. The return of sanctions resulted in a 15% CHE increase (54% to 69%) and a 14% increase in disease-driven poverty (44% to 58%). We get some crucial concerns such as "delay in receiving services or not receiving care due to high costs," "preferring low-quality services over high-quality ones," and "receiving loans or grants from individuals or organizations for the treatment of disease".
Generally, some demographic and background variables may lead to the protection of patients against CHE or accelerate its occurrence. Assessing the statistical relationship between demographic and background variables and the amount of OOPs, and the impact of CHE on patients and their families showed that in both pre-sanctions and post-sanctions phases, among the variables under study, only occupational status, having supplemental insurance, and being native had a significant impact on the amount of OOPs, CHE, or the poverty resulted by the disease costs. Undoubtedly, the leading cause of this situation is the severe drop in the Iranian Rial and the refusal of pharmaceutical companies and international banks to cooperate and deal with Iran for fear of US sanctions on them [38]. CHE and poverty due to high OOPs in Iran are mainly related to the imposed international political and financial sanctions. Undoubtedly, the sanctions were the leading cause of this situation for many direct and indirect adverse health and economic effects. The sanction affects the government's ability, and consequently, health systems to have proper support from patients and their households.
Although the Iranian health system has always provided patients with the necessary subsidies and medicines, these measures were insufficient. Also, access to essential care became more difficult for patients because of the widespread sanctions, especially financially. One of the main reasons for this problem is the lack of an efficient basic health insurance system and government support to expand supplemental insurance effectively [12, 40, 41]. The unilateral US sanctions on Iran have even caused severe problems for the Iranian Red Crescent, so this non-governmental humanitarian organization failed to timely access equipment, medications, and food sent by international organizations during times of crisis [38]. For example, during the nationwide 2019 floods that hit many cities in Iran, the following problems emerged as the result of the current sanctions: a shortage in the number of helicopters and relief boats, severe restrictions on receiving relief supplies and purchasing health kits from countries, inability to get financial aids from other countries, and the delayed entry of non-monetary relief items into Iran [12, 42].
The devastating effects of international sanctions have evident several detrimental effects on Iran and other countries. The following health issues are the results of war, and sanctions levied on Iraq in ten years: the mortality rate of less than one-year-old infants increased from 47 to 108 per 1000 live births; the mortality rate of less than 5-year-old children increased from 56 to 131 per 1000 live births; the acute malnutrition rate increased from 3% to 11%; the number of infants born with Low Birth Weight (LBW; <2.5 kg) increased from 4% to 25% due to malnutrition of 70% of the mothers; the access to safe drinking water reduced from 90% and 70% in cities and villages to 50% and 33%, respectively [43]. Interestingly, immediately after lifting some sanctions and introducing the oil-for-food program, these indicators, particularly infant mortality, began to decline significantly [43]. The devastating effects of the sanctions on patients with such diseases as HIV, diabetes, kidney failure, and cancer, along with the severe weakening of children's vaccination program due to the lack of access to equipment and medications in Venezuela, resulted in the death of more than 40,000 Venezuelan citizens between the years 2017 and 2018 [44]. Some other examples of the devastating effects of the sanctions on countries' public health include a 15% increase in the death rate of older people over a year in Cuba and a 15% and 30% increase in overall mortality and hospital deaths, respectively, in Yugoslavia [22]. Similar health disasters are occurring again in Syria, Yemen, and Gaza due to wars and sanctions [37, 45, 46]. Despite the claim that economic sanctions are a peaceful alternative to war, the examples presented in this study showed that this claim does not seem to be true [20], and the sanctions can also have similar and even wider destructive health consequences due to their broad scope and long active period. Imposing sanctions on countries violates people's right to access healthcare services easily [23].
One of the main strengths of the present study is its novelty, as it is the first article in the world to explicitly examine the economic and health impacts of sanctions on patients with a disease and their families. The primary study limitations in all CHE studies are the recall period and the number of cost elements used in the study instrument [47]. Due to the lack of comprehensive and illustrative health records (as clinical/managerial information systems) for patients with MS in Iran, we used a combination of possible approaches to access the patients' financial and clinical information, especially their health services utilization and costs, including assessing health records, analyzing the bills, conducting patient interviews, and comparing obtained results from this approaches. To cope with the existing limitation of assessing costing items, we developed a comprehensive questionnaire and standardized them on the expert's opinion and advice. The last limitation of this study is the impossibility to have a control group due to imposing sanctions on all country populations and its wide negative consequences on various parts of community.
Based on the current results, the study recommends that well-reputed international organizations such as the United Nations, WHO, UNICEF, and the International Monetary Fund (IMF) carefully examine the impact of sanctions on countries in priority areas such as public health and vulnerable groups of societies, and predict the potential problems and provide effective solutions. Meanwhile, sanctioned countries should do their best to protect the health of all, especially vulnerable people and groups, especially by promoting an efficient insurance system and moving towards self-sufficiency in producing health supplies. The current study can also suggest other research on different diseases in different sanctioned countries. Those results can clearly show the harmful health effects of sanctions on international organizations and provide a rational solution.
Conclusion
Nuclear-related political-economic sanctions have devastating effects on the public health of sanctioned countries because they can seriously impede access to appropriate healthcare services through a shortage of medicines and a lack of equipment/technology and raw materials. Therefore they lead to an increase in out-of-pocket payments and a decreased ability to pay for patients with multiple sclerosis and their households. In such circumstances, international organizations must protect the citizens' rights of the sanctioned countries by protecting health issues. In addition, the government of the sanctioned country, mainly the health system and third-party payment mechanism, must protect the patients with multiple sclerosis, especially the vulnerable patients who have lost their job, do have not enough income, or have no complementary health insurance.
Acknowledgements: The researchers would like to thank all patients for their active participation in the study. Also, the research team would like to thank all the experts for their sincere collaboration in the development of the questionnaire.
Ethical Permission: The researchers observed all ethical principles. All patients were free to accept or reject participation in the study, and written informed consent was obtained from all patients. We followed the privacy codes of the patients and assured them that the study results should only be used for the defined research purposes. Furthermore, the Ethics Committee of Tabriz University of Medical Sciences approved this study (IR.TBZMED.REC.1396.101).
Conflict of Interests: The authors declare no conflict of interest.
Authors’ Contribution: Gharibi F (First Author), Introduction Writer/Methodologist/Main Researcher/Statistical Analyst/Discussion Writer (40%); Imani A (Second Author), Methodologist/Main Researcher/Statistical Analyst (20%); Haghi M (Third Author), Introduction Writer/Main Researcher/Discussion Writer (10%); Dalal K (Fourth Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer (30%)
Funding: The study was conducted by financial support of Tabriz Health Services Management Research Center.
Keywords:
References
1. The World Health Organization. The world health report 2000: health systems; improving performance [Internet]. Geneva: The World Health Organization; 2000 [cited 2020 May 15]. Available from: https://apps.who.int/iris/handle/10665/79020. [Link]
2. The World Health Organization. The world health report 2010: health systems financing; the path to universal coverage [Internet]. Geneva: The World Health Organization; 2010 [cited 2020 May 15]. Available from: https://apps.who.int/iris/handle/10665/44371. [Link]
3. Azzani M, Roslani AC, Su TT. Determinants of household catastrophic health expenditure: a systematic review. Malays J Med Sci. 2019;26(1):15-43. [Link] [DOI:10.21315/mjms2019.26.1.3]
4. Russell S. The economic burden of illness for households in developing countries: a review of studies focusing on malaria, tuberculosis, and human immunodeficiency virus/acquired immunodeficiency syndrome. Am J of Trop Med and Hyg. 2004;71(2):147-55. [Link] [DOI:10.4269/ajtmh.2004.71.147]
5. Okoroh J, Essoun S, Seddoh A, Harris H, Weissman JS, Dsane-Selby L, et al. Evaluating the impact of the national health insurance scheme of Ghana on out of pocket expenditures: a systematic review. BMC Health Ser Res. 2018;18(426):1-14. [Link] [DOI:10.1186/s12913-018-3249-9]
6. Jan S, Lee SW, Sawhney JP, Ong TK, Chin CT, Kim HS. Catastrophic health expenditure on acute coronary events in Asia: a prospective study. Bull World Health Organ. 2016;94(3):193-200. [Link] [DOI:10.2471/BLT.15.158303]
7. Gharibi F, Imani A, Koustuv D. The catastrophic out-of-pocket health expenditure of multiple sclerosis patients in Iran. BMC Health Ser Res. 2021;21(1):1-8. [Link] [DOI:10.1186/s12913-021-06251-4]
8. Wagstaff A, Doorslaer EV. Catastrophe and impoverishment in paying for health care: With applications to Vietnam 1993-1998. Health Econ. 2003;12(11):921-33. [Link] [DOI:10.1002/hec.776]
9. Ariankhesal A, Etemadi M, Mohseni M, Azami-Aghdash S, Nakhaei M. Catastrophic health expenditure in Iran: a review article. Iran J Public Health. 2018;47(2):166-77. [Link]
10. Moradi G, Safari H, Piroozi B, Qanbari L, Farshadi S, Qasri H, et al. Catastrophic health expenditure among households with members with special diseases: A case study in Kurdistan. Med J Islam Repub Iran. 2017;31(43):1-7. [Link] [DOI:10.14196/mjiri.31.43]
11. Kobelt G, Lindgren P, Smala A, Joˆnsson B. Costs and quality of life in multiple sclerosis. A cross-sectional observational study in Germany. Eur J Health Econ. 2001;2:60-8. [Link] [DOI:10.1007/s101980100057]
12. Danaei G, Harirchi I, Sajadi HS, Yahyaei F, Majdzadeh R. The harsh effects of sanctions on Iranian health. Lancet. 2019;394(10197):468-9. [Link] [DOI:10.1016/S0140-6736(19)31763-5]
13. Imani A, Gharibi F, Khezri A, Joudyian N, Dalal K. Economic costs incurred by the patients with multiple sclerosis at different levels of the disease: a cross-sectional study in Northwest Iran. BMC Neurol. 2020;20(205):1-10. [Link] [DOI:10.1186/s12883-020-01790-5]
14. Hsu J, Flores G, Evans D, Mills A, Hanson K. Measuring financial protection against catastrophic health expenditures: methodological challenges for global monitoring. Int J Equit Health. 2018;17(69):1-13. [Link] [DOI:10.1186/s12939-018-0749-5]
15. Meskarpour-Amiri M, Dopeykar N, Mehdizadeh P, Ayoubian A, Motaghed Z. Study on the factors affecting the prescription of injection medicines in Iran: a policy making approach. Glob J Health Sci. 2015;7(3):291-7. [Link] [DOI:10.5539/gjhs.v7n3p291]
16. Meskarpour Amiri M, Teymourzadeh E, Ravangard R, Bahadori M. Health informal payments and their main determinants: the case of Iran. Proceed Singapore Healthcare. 2019:1-10. [Link] [DOI:10.1177/2010105818822594]
17. Meskarpour-Amiri M, Assari-Arani A, Sadeghi H, Agheli L. The reality behind informal health payments in Iran: "under the table payments" or "on the table payments"? Iran J Public Health. 2017;46(2):278. [Link]
18. Xin XX, Guan XD, Shi LX. Catastrophic expenditure and impoverishment of patients affected by 7 rare diseases in China. Orphanet J Rare Dis. 2016;11(74):1-8. [Link] [DOI:10.1186/s13023-016-0454-7]
19. Habibzadeh F. Economic sanction: a weapon of mass destruction. Lancet. 2018;392(10150):816-7. [Link] [DOI:10.1016/S0140-6736(18)31944-5]
20. Arya N. Economic sanctions: the kinder, gentler alternative? Med Confl Surv. 2008;24(1):25-41. [Link] [DOI:10.1080/13623690701775205]
21. Albright MK. Economic sanctions and public health: A view from the department of state. Ann Intern Med. 2000;132(2):155-7. [Link] [DOI:10.7326/0003-4819-132-2-200001180-00012]
22. Gorji A. Sanctions against Iran: The impact on health services. Iranian J Publ Health. 2014;43(3):381-2. [Link]
23. Kokabisaghi F. Assessment of the effects of economic sanctions on Iranians' right to health by using human rights impact assessment tool: A systematic review. Int J Health Policy Manag. 2018;7(5):374-93. [Link] [DOI:10.15171/ijhpm.2017.147]
24. Shahabi S, Fazlalizadeh H, Stedman J, Chuang L, Ram R. The impact of international economic sanctions on Iranian cancer healthcare. Health Policy. 2015;119:1309-18. [Link] [DOI:10.1016/j.healthpol.2015.08.012]
25. Kobelt G, Teich V, Cavalcanti M, Canzonieri AM. Burden and cost of multiple sclerosis in Brazil. PLoS ONE. 2019;14(1):e0208837. [Link] [DOI:10.1371/journal.pone.0208837]
26. Kobelt G, Thompson A, Berg J. New insights into the burden and costs of multiple sclerosis in Europe. Mult Scler J. 2017;23(8):1123-36. [Link] [DOI:10.1177/1352458517694432]
27. Piroozi B, Moradi G, Nouri B, Mohamadi Bolbanabad A, Safari H. Catastrophic health expenditure after the implementation of health sector evolution plan: a case study in the west of Iran. Int J Health Policy Manag. 2016;5(7):417-23. [Link] [DOI:10.15171/ijhpm.2016.31]
28. Barfar E, Pourreza A, Sharifi V, Sobhanian SMH, Sari AA. Catastrophic health expenditure in households with severe mental disorders patients: Evidence after Iran's health transformation plan. Health Scope. 2019;8(2):1-6. [Link] [DOI:10.5812/jhealthscope.79700]
29. Krejcie V, Morgan DW. Determining sample size for research activities. Educ Psychol Measur. 1970;30(3):670-10. [Link] [DOI:10.1177/001316447003000308]
30. Dunn J. Impact of mobility impairment on the burden of care giving in individuals with multiple sclerosis. Expert Rev Pharmacoecon Outcomes Res. 2010;10(4):433-40. [Link] [DOI:10.1586/erp.10.34]
31. Grima DT, Torrance GW, Francis G, Rice G, Rosner AJ, Lafortune L. Cost and health related quality of life consequences of multiple sclerosis. Mult Scler. 2000;6(2):91-8. [Link] [DOI:10.1177/135245850000600207]
32. Ekman BJ. Catastrophic health payments and health insurance: Some counterintuitive evidence from one low income country. J Health Policy. 2007;83(2-3):304 - 13. [Link] [DOI:10.1016/j.healthpol.2007.02.004]
33. Daneshkohan A, Karami M, Najafi F, Karami Matin B. Household catastrophic health expenditure. Iran J Public Health. 2011;40(1):94-9. [Link]
34. Xu K, Evans DB, Kawabata K. Household catastrophic health expenditure: a multicountry analysis. Lancet. 2003;362(9378):111-7. [Link] [DOI:10.1016/S0140-6736(03)13861-5]
35. Aloosh M, Salavati A, Aloosh A. Economic sanctions threaten population health: the case of Iran. Public Health. 2019;169:10-3. [Link] [DOI:10.1016/j.puhe.2019.01.006]
36. Mohammadi S, Carlbom A, Taheripanah R, Essén B. Experiences of inequitable care among Afghan mothers surviving near-miss morbidity in Tehran, Iran: a qualitative interview study. Int J Equity Health. 2017;16(121):1-8. [Link] [DOI:10.1186/s12939-017-0617-8]
37. Choonara I. Economic sanctions and child health. Med Confl Surv. 2013;29(2):93-8. [Link] [DOI:10.1080/13623699.2012.739048]
38. Setayesh S, Mackey TK. Addressing the impact of economic sanctions on Iranian drug shortages in the joint comprehensive plan of action: promoting access to medicines and health diplomacy. Glob Health. 2016;12(31):1-14. [Link] [DOI:10.1186/s12992-016-0168-6]
39. Ghiasi G, Rashidian A, Kebriaeezadeh A, Salamzadeh J. The impact of the sanctions made against Iran on availability to asthma medicines in Tehran. Iran J Pharm Res. 2016;15(3):567-71. [Link]
40. Gharibi F, Dadgar E. Pay-for-performance challenges in family physician program. Malay Fam Physician. 2020;15(2):19-29. [Link]
41. Xu K, Evans DB, Carrin G. Protecting households from catastrophic health spending. Health Affairs. 2007;26(4):972-83. [Link] [DOI:10.1377/hlthaff.26.4.972]
42. Peyravi M, Ahmadi Marzaleh M. The effect of the US sanctions on humanitarian aids during the great flood of Iran in 2019. Prehosp Disaster Med. 2020;35(2):233-4. [Link] [DOI:10.1017/S1049023X20000242]
43. Ali MM, Shah IH. Sanctions and childhood mortality in Iraq. Lancet. 2000;355:1851-7. [Link] [DOI:10.1016/S0140-6736(00)02289-3]
44. Zakrison TL, Muntaner C. US sanctions in Venezuela: help, hindrance, or violation of human rights? Lancet. 2019;393(10191):2586-7. [Link] [DOI:10.1016/S0140-6736(19)31397-2]
45. Moret ES. Humanitarian impacts of economic sanctions on Iran and Syria. Eur Secur. 2015;24(12):120-40. [Link] [DOI:10.1080/09662839.2014.893427]
46. Devi S. Devastation in Yemen ongoing. Lancet. 2018;392(10142):110-1. [Link] [DOI:10.1016/S0140-6736(18)31607-6]
47. Lu C, Chin B, Li G, Murray CJL. Limitations of methods for measuring out-of-pocket and catastrophic private health expenditures. Bull World Health Organ. 2009;87(3):238-44. [Link] [DOI:10.2471/BLT.08.054379]