Volume 14, Issue 3 (2022)
Iran J War Public Health 2022, 14(3): 303-309 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2022/05/4 | Accepted: 2022/07/20 | Published: 2022/08/13
Received: 2022/05/4 | Accepted: 2022/07/20 | Published: 2022/08/13
How to cite this article
Wang Y, Liu L, Geng Y, Wang C, Li S. Formation of a Costs Model for Patient Rehabilitation. Iran J War Public Health 2022; 14 (3) : 8
URL: http://ijwph.ir/article-1-1202-en.html
URL: http://ijwph.ir/article-1-1202-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
1- Department of the Physical Training, Beijing Sport University, Beijing, China
2- Department of Physical Education, Peking University, Beijing, China
3- Department of the Olympic Sport History and Theory, National University of Ukraine on Physical Education and Sport, Kyiv, Ukraine
4- Department of the High-Performance Sport, Beijing Sport University, Beijing, China
5- PE Teaching Group, Beijing Foreign Languages School, Beijing, China
2- Department of Physical Education, Peking University, Beijing, China
3- Department of the Olympic Sport History and Theory, National University of Ukraine on Physical Education and Sport, Kyiv, Ukraine
4- Department of the High-Performance Sport, Beijing Sport University, Beijing, China
5- PE Teaching Group, Beijing Foreign Languages School, Beijing, China
Full-Text (HTML) (461 Views)
Introduction
An indicator framework is an essential part of monitoring, the composition of which largely determines its content and structure [1]. The indicator framework for monitoring the process of cost for a patient should be an adequate information model of the pricing process [2]. The set of indicators for monitoring the process of generating costs for a patient is a combination of primary and secondary indicators that can provide a holistic assessment of the state of the process, and qualitative and quantitative changes in it [3]. Creation of an indication framework in the process of high-quality rehabilitation of a patient in terms of interaction with a medical institution. The correct rehabilitation process largely depends on compliance with all factors, and monitoring is an important part of it. Indicators should be structured; therefore, it is necessary to choose approaches to such structuring and classify indicators according to those signs that will ensure the processability of the system [4].
The task of constructing an indicator framework for integrated process monitoring of costs for a patient by medical rehabilitation institutions is complicated by the lack of general recommendations on its filling with specific indicators [5]. Therefore, the basis for the development of an indicator framework is directly the process of price formation and its components [6].
In the course of scientific research and development of optimal ways of interaction between systems, several key approaches to the issue of costing monitoring have been identified. They were divided into models, each of which operates with one or another set of indicators to compile the most accurate summary.
The standard model provides for the definition of such concepts as “state of nature” and “internal strategy” [7]:
An indicator framework is an essential part of monitoring, the composition of which largely determines its content and structure [1]. The indicator framework for monitoring the process of cost for a patient should be an adequate information model of the pricing process [2]. The set of indicators for monitoring the process of generating costs for a patient is a combination of primary and secondary indicators that can provide a holistic assessment of the state of the process, and qualitative and quantitative changes in it [3]. Creation of an indication framework in the process of high-quality rehabilitation of a patient in terms of interaction with a medical institution. The correct rehabilitation process largely depends on compliance with all factors, and monitoring is an important part of it. Indicators should be structured; therefore, it is necessary to choose approaches to such structuring and classify indicators according to those signs that will ensure the processability of the system [4].
The task of constructing an indicator framework for integrated process monitoring of costs for a patient by medical rehabilitation institutions is complicated by the lack of general recommendations on its filling with specific indicators [5]. Therefore, the basis for the development of an indicator framework is directly the process of price formation and its components [6].
In the course of scientific research and development of optimal ways of interaction between systems, several key approaches to the issue of costing monitoring have been identified. They were divided into models, each of which operates with one or another set of indicators to compile the most accurate summary.
The standard model provides for the definition of such concepts as “state of nature” and “internal strategy” [7]:
• “state of nature” is a combination of environmental factors that determine the estimated cost of patient rehabilitation;
• “internal strategy” is a combination of internal capabilities and factors that determine the behavior of an individual healthcare institution in forming the composition of the production equipment for the rehabilitation process, determining the capacity (number of rehabilitated), and forming the rehabilitation structure that affects, on the one hand, the totality of variables and fixed costs, and on the other, they influence the determination of the average estimated price for the rehabilitation of each patient.
The final decision regarding the formation of the actual application for the number of rehabilitated and the price application by medical rehabilitation institutions is made after a statistical experiment that gives it the most probable information about the choice [8]. This model of the process of generating costs for a patient by medical rehabilitation institutions with a unit for assessing uncertainty and risk is easily integrated with the modeling of statistical games [9]. Statistical games (models) are a game of two persons – man and nature – with the use of additional statistical information about the state of nature by man [10].
The key goal of the presented article is to define the concept of the costing model in the process of medical rehabilitation, as well as to analyze the main trends and signs of its formation in terms of both pricing policy and framework management. Proper costing monitoring is an integral part of correct rehabilitation. Its study in the presented article will be extremely useful for medical practice and further research in the field of medical rehabilitation.
Materials and Methods
The conditions of the statistical game in the process of generating costs for the patient by the medical rehabilitation institutions are set in the form of a matrix, whereA = a ij Q = q ij
The key goal of the presented article is to define the concept of the costing model in the process of medical rehabilitation, as well as to analyze the main trends and signs of its formation in terms of both pricing policy and framework management. Proper costing monitoring is an integral part of correct rehabilitation. Its study in the presented article will be extremely useful for medical practice and further research in the field of medical rehabilitation.
Materials and Methods
The conditions of the statistical game in the process of generating costs for the patient by the medical rehabilitation institutions are set in the form of a matrix, where
Therefore, the development of an indicator framework proceeds from the formation of a library of indicators to the selection and determination of key indicators that can assess the state and dynamics of monitoring objects and contribute to the selection of optimal pricing strategies [12]. According to the frequency of data collection, it is necessary to distinguish between information that is collected annually – for stable and slowly changing data used in strategic planning and control of price decisions, and monthly (weekly, daily) reporting – for dynamic indicators used in operational control and management of the pricing process [13]. Therefore, it is advisable to divide all indicators into two groups [14]:
1- dynamic – those that can assess the impact of relevant factors on the pricing process in the short term [15];
2- strategic – those that can affect the process of pricing in the medium and long term [16].
Of course, in the model of integrated monitoring of the process of cost for a patient by medical rehabilitation institutions, the main focus is on the indicators of the first group, however, to prevent spasmodic changes in price dynamics, it is necessary to monitor and record changes in the indicators of the second group, which can also positively or negatively affect pricing strategies, own pricing decisions or change the vector of regulatory policy in the field of pricing [17].
This study aimed to develop of an indicator framework for integrated monitoring of the costing process for a patient by rehabilitation medical institutions.
Findings
The strategic change factors system, as an object of integrated monitoring of the process of cost for a patient by medical rehabilitation institutions, is presented in the form of their distribution to internal and external (Table 1). Internal factors in the strategic changes factors system are presented in the context of determining the technical condition and the possibility of accepting patients in the medium and long term, and other internal factors that should be taken into account, but have an indirect effect on the process of cost for the patient, and accordingly on decision-making regarding the formation of a price application and an application for the number of patients received. This group of factors differs from the internal ones presented in the dynamic indicator framework in that the frequency of their observation and assessment can be significantly wider in time.
External factors in the system of factors of strategic changes are presented in the context of the institutional component and factors associated with changes in supply and demand in the rehabilitation market. The first group of factors is associated with changes in the functioning of the public health infrastructure itself. The manifestation of changes in certain of these factors can fundamentally change the goals and objectives of monitoring the process of cost formation for patients of healthcare institutions, so tracking these indicators with a given frequency is important for modeling conditions of nature. The second group of factors – supply and demand, also affect the qualitative changes in the process of costs for a patient in healthcare institutions but are not able to change it in the short term. Because of this, they also form a system of factors of strategic change and change the external environment.
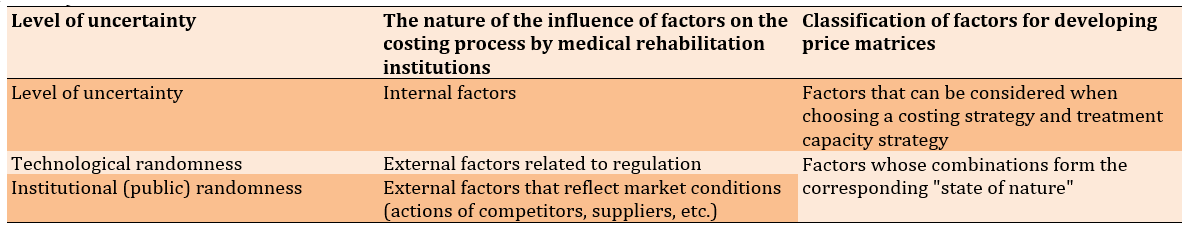
The development of a dynamic indicator framework of integrated monitoring and indicators of relevant monitoring factors for the formation of costing strategies and modeling of the state of the external environment requires the classification of all factors:
This study aimed to develop of an indicator framework for integrated monitoring of the costing process for a patient by rehabilitation medical institutions.
Findings
The strategic change factors system, as an object of integrated monitoring of the process of cost for a patient by medical rehabilitation institutions, is presented in the form of their distribution to internal and external (Table 1). Internal factors in the strategic changes factors system are presented in the context of determining the technical condition and the possibility of accepting patients in the medium and long term, and other internal factors that should be taken into account, but have an indirect effect on the process of cost for the patient, and accordingly on decision-making regarding the formation of a price application and an application for the number of patients received. This group of factors differs from the internal ones presented in the dynamic indicator framework in that the frequency of their observation and assessment can be significantly wider in time.
External factors in the system of factors of strategic changes are presented in the context of the institutional component and factors associated with changes in supply and demand in the rehabilitation market. The first group of factors is associated with changes in the functioning of the public health infrastructure itself. The manifestation of changes in certain of these factors can fundamentally change the goals and objectives of monitoring the process of cost formation for patients of healthcare institutions, so tracking these indicators with a given frequency is important for modeling conditions of nature. The second group of factors – supply and demand, also affect the qualitative changes in the process of costs for a patient in healthcare institutions but are not able to change it in the short term. Because of this, they also form a system of factors of strategic change and change the external environment.
The development of a dynamic indicator framework of integrated monitoring and indicators of relevant monitoring factors for the formation of costing strategies and modeling of the state of the external environment requires the classification of all factors:
•by the level of uncertainty: technological randomness, social randomness, variety of meanings, and unreliability;
•by the nature of the influence of factors on the costing process for a patient by medical rehabilitation institutions: internal factors, external factors related to regulation, and external factors that reflect market conditions (Table 2).
Table 1) System of factors of strategic changes in integrated monitoring of the costing process by medical rehabilitation institutions

Table 2) Classification of indicators of an indicator framework according to the level and nature of uncertainty
Therefore, the system of dynamic indicators of integrated monitoring of the costing process for a patient by medical rehabilitation institutions consists of 10 groups of factors presented in the context of preliminary (ex-ante-monitoring), intermediate (ex-mid-monitoring), and final (ex- post-monitoring) types of monitoring. Each group also has its own appropriate monitoring method (toolkit). To form a pricing strategy, medical rehabilitation institutions of the enterprise based on monitoring results developed a set of indicators that affect the choice of internal strategy and form the state of the environment (state of nature).
The strategy of medical rehabilitation institutions to develop a cost request and patient capacity develops under the influence of internal (controlled, measured) factors (Equation 1):

Accordingly, states of nature are formed on the basis of various combinations of external (uncontrolled, difficult to measure, or immeasurable) factors (Equation 2):

As a result, a matrix of five states of nature and five variants of the internal strategy for a separate dispatch interval during the stated period (18-00 hours) was obtained (Table 3).
Table 3) Price matrix

To assess the risk and adopt an optimal internal strategy for the development of capacity and price bids, the following criteria will be used:
1- Wald’s maximin criterion or criterion of extreme pessimism;
2- Savage’s minimax criterion (also a criterion of extreme pessimism);
3- the criterion of extreme optimism;
4- Hurwitz’s generalized maximin criterion (the criterion of pessimism – optimism);
5- Laplace’s criterion of insufficient substantiation.
According to Wald’s criterion, if a medical institution’s price (profit) matrix is considered, then the best solution would be for which the gain will be the highest of all the minimum under various conditions. This principle is called the maximin criterion. The formal expression of maximin looks like Equation 3-5:

wherea i H w
Wald’s maximin criterion makes it possible to obtain a lower price, and according to this, a management strategy for medical rehabilitation institutions is chosen, which guarantees under any conditions a profit at a price not less thanma x i mi n j a ij
Table 4) Price matrix for determining the internal pricing strategy by medical rehabilitation institutions, USD/person

Table 5) Risk assessment criteria for determining the internal pricing strategy by medical rehabilitation institutions, USD/person

The formalized expression of the criterion of extreme optimism has the form (Equation 6-8):

wherea i H o
The Savage minimax criterion is used in those cases when it is necessary to avoid a big risk. In contrast to Wald’s criterion, when calculating the Savage criterion for making a decision, it is not the price (profit) matrix that is considered, but the risk matrix or the profit loss matrix. Loss of profit Pij was defined as the difference between the maximum gain and the gain of a particular decision in a given situation (Table 6; Equation 9):

Table 6) Profit loss matrix, USD/person

According to the Savage criterion, preference should be given to a solution for which the maximum losses under various conditions are minimal (Table 5 line 11, Table 5 line 6). The Savage formalized criterion has the form Equation 11-13:

wherep ij
The Hurwitz criterion of generalized maximin, in contrast to the criteria of Wald and Savage, takes into account both a pessimistic and optimistic approach to the situation. It can be used if it is necessary to focus on the decision between the line of conduct for the worst and the line for the best, so it is called the criterion of pessimism-optimism. When applying the Hurwitz criterion for the price (profit) matrix, then preference should be given to the solution option for which the maximum indicator G, determined from the expression (Equation 14-16):

Where aij – winnings correspond to the i-th solution, with the j-th version of the situation.
At the same time, the Hurwitz criterion separately takes into account the risk probability, the so-called optimism indicator x(0≤x≤1), where x=0 best line of conduct, x=1 worst-case line of conduct. If x=1, the Hurwitz criterion is equated to the Wald criterion, that is, an orientation toward cautious behavior in determining the price bid and the capacity request of a rehabilitation medical institution. If x=0 focus on marginal risk, corresponding to the criterion of extreme optimism. Value X between 0 and 1 was intermediate between risk and caution, depending on the specific situation and the risk aptitude of decision-makers. In current calculations, the value of 0.8 was taken as 0.8, which characterizes the minimum risk aptitude (Table 5). The principle of Laplace’s insufficient substantiation is one of the classical criteria used in decision-making under conditions of uncertainty. This criterion can be used if it can be assumed that any of the variants of the states of nature is no more probable than the other. Then the probabilities of the states of nature can be considered equal and the choice of a solution can be made in the same way as in risk conditions – at the minimum of the average risk indicator. In these calculations, the Laplace criterion was calculated as the average value of the estimated price for each internal strategy under the adopted equal environmental conditions (Table 5).
The experiment for the period from 18-00 to 19-00 hours based on monitoring, assessment, and modeling options for urgent rehabilitation requests, price requests, and environmental conditions allows us to conclude that it is advisable to apply the internal strategy of the medical institution, since:

where
Wald’s maximin criterion makes it possible to obtain a lower price, and according to this, a management strategy for medical rehabilitation institutions is chosen, which guarantees under any conditions a profit at a price not less than
Table 4) Price matrix for determining the internal pricing strategy by medical rehabilitation institutions, USD/person

Table 5) Risk assessment criteria for determining the internal pricing strategy by medical rehabilitation institutions, USD/person

The formalized expression of the criterion of extreme optimism has the form (Equation 6-8):

where
The Savage minimax criterion is used in those cases when it is necessary to avoid a big risk. In contrast to Wald’s criterion, when calculating the Savage criterion for making a decision, it is not the price (profit) matrix that is considered, but the risk matrix or the profit loss matrix. Loss of profit Pij was defined as the difference between the maximum gain and the gain of a particular decision in a given situation (Table 6; Equation 9):

Table 6) Profit loss matrix, USD/person

According to the Savage criterion, preference should be given to a solution for which the maximum losses under various conditions are minimal (Table 5 line 11, Table 5 line 6). The Savage formalized criterion has the form Equation 11-13:

where
The Hurwitz criterion of generalized maximin, in contrast to the criteria of Wald and Savage, takes into account both a pessimistic and optimistic approach to the situation. It can be used if it is necessary to focus on the decision between the line of conduct for the worst and the line for the best, so it is called the criterion of pessimism-optimism. When applying the Hurwitz criterion for the price (profit) matrix, then preference should be given to the solution option for which the maximum indicator G, determined from the expression (Equation 14-16):

Where aij – winnings correspond to the i-th solution, with the j-th version of the situation.
At the same time, the Hurwitz criterion separately takes into account the risk probability, the so-called optimism indicator x(0≤x≤1), where x=0 best line of conduct, x=1 worst-case line of conduct. If x=1, the Hurwitz criterion is equated to the Wald criterion, that is, an orientation toward cautious behavior in determining the price bid and the capacity request of a rehabilitation medical institution. If x=0 focus on marginal risk, corresponding to the criterion of extreme optimism. Value X between 0 and 1 was intermediate between risk and caution, depending on the specific situation and the risk aptitude of decision-makers. In current calculations, the value of 0.8 was taken as 0.8, which characterizes the minimum risk aptitude (Table 5). The principle of Laplace’s insufficient substantiation is one of the classical criteria used in decision-making under conditions of uncertainty. This criterion can be used if it can be assumed that any of the variants of the states of nature is no more probable than the other. Then the probabilities of the states of nature can be considered equal and the choice of a solution can be made in the same way as in risk conditions – at the minimum of the average risk indicator. In these calculations, the Laplace criterion was calculated as the average value of the estimated price for each internal strategy under the adopted equal environmental conditions (Table 5).
The experiment for the period from 18-00 to 19-00 hours based on monitoring, assessment, and modeling options for urgent rehabilitation requests, price requests, and environmental conditions allows us to conclude that it is advisable to apply the internal strategy of the medical institution, since:
•with a cautious approach, no matter what is the situation of external factors, the average estimated price for patient rehabilitation for a medical rehabilitation institution will be at least 519.58 USD/person, but it can be even more, as evidenced by a small amount of risk, the Hurwitz criterion (according to the A3 strategy, it can be 540.02 USD per person);
•with a risky approach, it is possible to use the A1 strategy with an average estimated price of 653.22 USD/person. However, the Laplace criterion, which reinforces the decision on the A1 strategy, gives less accurate results than the Hurwitz criterion. The Laplace criterion nevertheless determines the average price among all the declared internal strategies.
The development of price matrices, risk assessment according to the specified criteria, and decision-making on choosing an internal strategy depending on the influence of environmental factors is performed for each hour of the rehabilitation interval and can be adapted by any medical rehabilitation institution working on the rehabilitation process according to price requests.
Discussion
Analyzing the results obtained, one can come to a series of key conclusions that form the main points for a qualitative discussion of the presented topic. In the process of analyzing the main shaping factors, the fundamental aspects of the framework and monitoring of cost for rehabilitation were identified.
The study showed that consideration of the actual problem is quite broad and some specialists are interested in the peculiarities of the formation of costs for rehabilitation. In particular, taking into account modernity, A. Beivers notes that the corona crisis increased the problems of the question of the role of rehabilitation and its financing, but at the same time, such a course of events prompted the emergence of new conceptual solutions [18]. The author claims that rehabilitation clinics make a significant contribution to solving the relevant issue and creating new digital concepts of care. But at the same time, rehabilitation service providers themselves are increasingly acting as regional gatekeepers, that is, as mediators in the contact between two different organizations. In this case, capitalization models or complex fixed rates can be useful.
High-ranking stakeholders, i.e. parliament, play an important role in the formation of a financing model for patient rehabilitation, as they can have a significant influence directly on other subjects of the relevant issue. Researcers note that the implementation of the organization of political dialogue with high-ranking legislators, as well as other persons who exert influence on politics, can be a rational way of discussing this issue [19]. Which, in turn, will lead to the development and application of options for effective strategies for patient rehabilitation models.
The process of generating costs for a patient by medical rehabilitation institutions should be different from the current one [20]. A characteristic feature of the new approach to pricing a patient’s rehabilitation is the presence of a component for assessing the level of uncertainty and risk and making informed decisions based on the results of such an assessment on the formation of actual bids for labor capacity and price bids [21]. The specified component, as a component of the cost-formation process, acquires a special role in conditions of uncertainty in establishing the estimated cost of patient rehabilitation [22].
It is worth noting that the formed indicators framework for integrated monitoring of the costing process for a patient by medical rehabilitation institutions allows us to determine the behavior of an individual healthcare institution regarding the composition of technological equipment, determine the capacity of a medical institution, form a structure of rehabilitation measures that affect recovery rates and determine the average estimated prices for the rehabilitation of each patient, which together determine the "internal strategy" of the rehabilitation medical institution. Moreover, the development of internal strategies occurs following the simulated "state of nature", which is formed under the influence of those environmental factors that determine the likely price for the rehabilitation of an individual patient [23-25]. An important aspect of this study is also the importance of understanding the differences in the process of rehabilitation of ordinary citizens and military patients (combatants) who were injured in the course of hostilities. Rehabilitation of this category of the population is notable for its difficulties, and cost monitoring in the aspect of the indicator framework is much more relevant. The specifics of the rehabilitation of combatants are largely related to the professional deformation of the military, the psychological consequences of participating in hostilities, as well as the effects of possible shell shock, injuries, and other aspects that can affect the rehabilitation process and require a unique approach [26, 27].
Conclusions
Thus, as a result of the development of an indicator framework for integrated monitoring of the costing process for a patient by rehabilitation medical institutions:
Discussion
Analyzing the results obtained, one can come to a series of key conclusions that form the main points for a qualitative discussion of the presented topic. In the process of analyzing the main shaping factors, the fundamental aspects of the framework and monitoring of cost for rehabilitation were identified.
The study showed that consideration of the actual problem is quite broad and some specialists are interested in the peculiarities of the formation of costs for rehabilitation. In particular, taking into account modernity, A. Beivers notes that the corona crisis increased the problems of the question of the role of rehabilitation and its financing, but at the same time, such a course of events prompted the emergence of new conceptual solutions [18]. The author claims that rehabilitation clinics make a significant contribution to solving the relevant issue and creating new digital concepts of care. But at the same time, rehabilitation service providers themselves are increasingly acting as regional gatekeepers, that is, as mediators in the contact between two different organizations. In this case, capitalization models or complex fixed rates can be useful.
High-ranking stakeholders, i.e. parliament, play an important role in the formation of a financing model for patient rehabilitation, as they can have a significant influence directly on other subjects of the relevant issue. Researcers note that the implementation of the organization of political dialogue with high-ranking legislators, as well as other persons who exert influence on politics, can be a rational way of discussing this issue [19]. Which, in turn, will lead to the development and application of options for effective strategies for patient rehabilitation models.
The process of generating costs for a patient by medical rehabilitation institutions should be different from the current one [20]. A characteristic feature of the new approach to pricing a patient’s rehabilitation is the presence of a component for assessing the level of uncertainty and risk and making informed decisions based on the results of such an assessment on the formation of actual bids for labor capacity and price bids [21]. The specified component, as a component of the cost-formation process, acquires a special role in conditions of uncertainty in establishing the estimated cost of patient rehabilitation [22].
It is worth noting that the formed indicators framework for integrated monitoring of the costing process for a patient by medical rehabilitation institutions allows us to determine the behavior of an individual healthcare institution regarding the composition of technological equipment, determine the capacity of a medical institution, form a structure of rehabilitation measures that affect recovery rates and determine the average estimated prices for the rehabilitation of each patient, which together determine the "internal strategy" of the rehabilitation medical institution. Moreover, the development of internal strategies occurs following the simulated "state of nature", which is formed under the influence of those environmental factors that determine the likely price for the rehabilitation of an individual patient [23-25]. An important aspect of this study is also the importance of understanding the differences in the process of rehabilitation of ordinary citizens and military patients (combatants) who were injured in the course of hostilities. Rehabilitation of this category of the population is notable for its difficulties, and cost monitoring in the aspect of the indicator framework is much more relevant. The specifics of the rehabilitation of combatants are largely related to the professional deformation of the military, the psychological consequences of participating in hostilities, as well as the effects of possible shell shock, injuries, and other aspects that can affect the rehabilitation process and require a unique approach [26, 27].
Conclusions
Thus, as a result of the development of an indicator framework for integrated monitoring of the costing process for a patient by rehabilitation medical institutions:
•results of the research can be used in the process of making informed decisions on the formation of the actual request for the capacity of the institution and price request;
•it was proposed that all indicators of integrated monitoring of the costing process for a patient be divided into two groups: dynamic, which can assess the impact of relevant factors on the pricing process in the short term, and strategic, which can affect the pricing process in the medium and long term;
•a model of the process of cost formation for a patient by rehabilitation medical institutions, presented in the research, allows the use of monitoring results for modeling statistical games;
•a dynamic indicator framework of 10 groups of factors presented in the context of preliminary, intermediate, and final types of monitoring. Classification based on the influence of factors on the process of generating costs for a patient allows for identifying indicators that reflect external factors. Internal – allows us to create an internal pricing strategy, and external – to predict the state of the external environment for the formation of prices, which is used in the modeling of statistical games;
•according to the results of the experiment, whatever the situation of external factors, the choice of pricing strategy allows us to get a minimum, but guaranteed price. With a risky approach, it is possible to use a strategy with a price whose profit will be high, but the risk of it will also increase.
Acknowledgments: None declared.
Ethical Permissions: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. A study was approved by National Ethics Commission of the Ministry of Health of Ukraine, November 28, 2021, No 1013-5.
Conflicts of Interests: The authors declare no conflicts of interests.
Authors’ Contributions: Wang Y (First Author), Introduction Writer/Main Researcher (20%); Liu L (Second Author), Methodologist/Statistical Analyst (20%); Geng Y (Third Author), Discussion Writer/Data Analyst (20%); Wang C (Fourth Author), Assistant Researcher/Discussion Writer (20%); Li S (Fifth Author), Introduction Writer/Assistant Researcher (20%)
Funding/Support: None declared.
Keywords:
References
1. Rothstein BE, Gonzalez J, Cunningham K, Saraiya A, Dornelles AC, Nguyen BM. Direct and indirect patient costs of dermatology clinic visits and their impact on access to care and provider preference. Cutis. 2017;100(6):405-10. [Link]
2. Trude S, Grossman JM. Patient cost-sharing innovations: promises and pitfalls. Issue Brief Cent Stud Health Syst Change. 2004;(75):1-4. [Link]
3. Lee J, Dowd B. Effect of health information technology expenditure on patient level cost. Healthc Inform Res. 2013;19(3):215-21. [Link] [DOI:10.4258/hir.2013.19.3.215]
4. Hunt J, Rozenfeld Y, Shenolikar R. Effect of patient medication cost share on adherence and glycemic control. Manag Care. 2009;18(7):47-53. [Link]
5. Vassall A, Seme A, Compernolle P, Meheus F. Patient costs of accessing collaborative tuberculosis and human immunodefi ciency virus interventions in Ethiopia. Int J Tuberc Lung Dis. 2010;14(5):604-10. [Link]
6. Xu Y, Li N, Lu M, Dixon E, Myers RP, Jelley RJ, et al. The effects of patient cost sharing on inpatient utilization, cost, and outcome. PLoS One. 2017;12(10):e0187096. [Link] [DOI:10.1371/journal.pone.0187096]
7. Lostao L, Regidor E, Geyer S, Aïach P. Patient cost sharing and social inequalities in access to health care in three western European countries. Soc Sci Med. 2007;65(2):367-76. [Link] [DOI:10.1016/j.socscimed.2007.05.001]
8. Banyra O, Sheremeta R, Shulyak A. Strangulation of the penis: two case reports. Cent Eur J Urol. 2013;66(2):242-5. [Link] [DOI:10.5173/ceju.2013.04.art2]
9. Williams AR, McDougall JC, Bruggeman SK, Erwin PJ, Kroshus ME, Naessens JM. Estimation of unreimbursed patient education costs at a large group practice. J Contin Educ Health Prof. 2004;24(1):12-9. [Link] [DOI:10.1002/chp.1340240104]
10. Martsolf GR, Auerbach D, Benevent R, Stocks C, Jiang HJ, Pearson ML, et al. Examining the value of inpatient nurse staffing: an assessment of quality and patient care costs. Med Care. 2014;52(11):982-8. [Link] [DOI:10.1097/MLR.0000000000000248]
11. Carreras M, García-Goñi M, Ibern P, Coderch J, Vall-Llosera L, Inoriza JM. Estimates of patient costs related with population morbidity: can indirect costs affect the results?. Eur J Health Econ. 2011;12(4):289-95. [Link] [DOI:10.1007/s10198-010-0227-5]
12. Hockenberry JM, Mutter R, Barrett M, Parlato J, Ross MA. Factors associated with prolonged observation services stays and the impact of long stays on patient cost. Health Serv Res. 2014;49(3):893-909. [Link] [DOI:10.1111/1475-6773.12143]
13. Engström SG, Carlsson L, Östgren CJ, Nilsson GH Borgquist LA. The importance of comorbidity in analysing patient costs in Swedish primary care. BMC Public Health. 2006;6:36. [Link] [DOI:10.1186/1471-2458-6-36]
14. Carey K. A multilevel modelling approach to analysis of patient costs under managed care. Health Econ. 2000;9(5):435-46.
https://doi.org/10.1002/1099-1050(200007)9:5<435::AID-HEC523>3.0.CO;2-Z [Link] [DOI:10.1002/1099-1050(200007)9:53.0.CO;2-Z]
15. Tambor M, Pavlova M, Woch P, Groot W. Diversity and dynamics of patient cost-sharing for physicians' and hospital services in the 27 European :union: countries. Eur J Public Health. 2011;21(5):585-90. [Link] [DOI:10.1093/eurpub/ckq139]
16. Trude S. Patient cost sharing: how much is too much?. Issue Brief Cent Stud Health Syst Change. 2003;(72):1-4. [Link]
17. Kernick DP, Reinhold DM, Netten A. What does it cost the patient to see the doctor?. Br J Gen Pract. 2000;50(454):401-3. [Link]
18. Chekhovska IV, Balynska OM, Blahuta RI, Sereda VV, Mosondz SO. Euthanasia or palliative care: legal principles of the implementation in the context of the realization of human rights to life. Wiad Lek. 2019;72(4):677-81. [Link] [DOI:10.36740/WLek201904133]
19. Shahabi S, Ahmadi Teymourlouy A, Shabaninejad H, Kamali M, Lankarani KB. Financing of physical rehabilitation services in Iran: a stakeholder and social network analysis. BMC Health Serv Res. 2020;20:599. [Link] [DOI:10.1186/s12913-020-05447-4]
20. Cyganska M, Cyganski P, Pyke C. Development of clinical value unit method for calculating patient costs. Health Econ. 2019;28(8):971-83. [Link] [DOI:10.1002/hec.3902]
21. Lostao L, Regidor E, Geyer S, Aïach P. Patient cost sharing and physician visits by socioeconomic position: findings in three Western European countries. J Epidemiol Community Health. 2007;61(5):416-20. [Link] [DOI:10.1136/jech.2006.047126]
22. Dahlin S, Raharjo H. Relationship between patient costs and patient pathways. Int J Health Care Qual Assur. 2019;32(1):246-61. [Link] [DOI:10.1108/IJHCQA-10-2017-0199]
23. Monkerud LC, Tjerbo T. The effects of the Norwegian coordination reform on the use of rehabilitation services: panel data analyses of service use, 2010 to 2013. BMC Health Serv Res. 2016;16(a):353. [Link] [DOI:10.1186/s12913-016-1564-6]
24. Verville RE, Chan L. Legislative issues. The federal financing and regulation of physical medicine and rehabilitation services. Phys Med Rehabil Clin North Am. 2002;13(2):195-211. [Link] [DOI:10.1016/S1047-9651(01)00008-0]
25. Office of Special Education and Rehabilitative Services, Department of Education. Final priority; rehabilitation services administration--assistive technology alternative financing program. Fed Regist. 2014;79(157):47575-9. [Link]
26. Kazemian R, Abolmaali Alhosseini K. Comparison of mature, immature, and neurotic defense mechanisms in veterans and normal people. Iranian J War Public Health. 2018;10(4):221-26. [Link] [DOI:10.29252/ijwph.10.4.221]
27. Ganjparvar Z, Mousavi B, Khateri S, Soroush M, Masoumi M, Shokoohi H. Daily Activity of adolescent victims of landmine and unexploded ordnance. Iranian J War Public Health. 2014;6(42):137-42. [Link]