Volume 14, Issue 1 (2022)
Iran J War Public Health 2022, 14(1): 51-57 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2022/01/1 | Accepted: 2022/02/23 | Published: 2022/03/5
Received: 2022/01/1 | Accepted: 2022/02/23 | Published: 2022/03/5
How to cite this article
Kostetskiy I, Bagin V, Kaliskin A, Shamrikov A, Davydova N. Comparative Evaluation of LMA-Supreme and i-gel Supraglottic Airway Devices with Endotracheal Intubation during Surgical Correction of Traumatic Orbital Injuries. Iran J War Public Health 2022; 14 (1) :51-57
URL: http://ijwph.ir/article-1-1112-en.html
URL: http://ijwph.ir/article-1-1112-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
1- Department of Anesthesiology and Intensive Care No. 1, City Clinical Hospital No. 23, Yekaterinburg, Russian Federation
2- Department of Anesthesiology and Intensive Care No. 5, City Clinical Hospital No. 40, Yekaterinburg, Russian Federation
3- Department of Anesthesiology and Intensive Care, Ural State Medical University, Yekaterinburg, Russian Federation
2- Department of Anesthesiology and Intensive Care No. 5, City Clinical Hospital No. 40, Yekaterinburg, Russian Federation
3- Department of Anesthesiology and Intensive Care, Ural State Medical University, Yekaterinburg, Russian Federation
Full-Text (HTML) (635 Views)
Introduction
Supraglottic airway devices (SADs) are firmly established in modern anesthesiology practice and are often considered as one of the options to ensure airway management in patients with ‘difficult airways’ [1, 2]. These devices are used in prehospital medical care [3-6] and resuscitation [3]. One of the variants of their use is airway control during anesthesia, where they have also demonstrated their safety and efficiency [7-21]. By providing airway control with rather a simple insertion and less invasiveness in many situations, SADs can
compete with the “gold standard” in maintaining airway management, that is, endotracheal intubation [7, 22, 23]. At the same time, a wide variety of supraglottic airway devices available on the markets is an advantage as well as a disadvantage of this technology, as it makes it much more difficult to select the necessary device in each specific situation. The analysis of publications on this topic sometimes gives contradictory data with restrictions. Very often in our clinic, we admit patients with mild traumatic brain injury and fractured midface, who need orbital fractures osteosynthesis. Features of this category of interventions include a low degree of anesthetic risk (ASA I or II, according to the American Society of Anesthesiologists scale), and the average duration of surgery of 30-60 minutes. It requires deep anesthesia, relaxation, and controlled ventilation to make sure the surgeon can operate comfortably. Supraglottic airway devices allow providing all the aforementioned conditions while being less aggressive compared to the standard endotracheal intubation. This fact was the reason for the comparative assessment of SADs and intubation in this type of operation. Having analyzed publications devoted to the comparison of second-generation airway devices in various surgical interventions, we could not conclude the obvious advantage of any device.
The most common parameters for comparing airway devices are time, efficacy, and ease of insertion, the oropharyngeal leak pressure (OLP; peak airway pressure at which leak is recorded), and the number of complications associated with the use of the device. In the work of Das et al. [9] i-gel, ProSeal and Laryngeal Tube Suction D (LTS-D) airway devices were compared during elective surgery using general anesthesia. The devices showed comparable high efficacy (LMA-P – 96%, i-gel – 100%, LTS-D – 94%). The smallest leak pressure was demonstrated in the i-gel group (23.38±2.06cmH2O) compared to LMA-P (28.5±2.8cmH2O) and LTS-D (26.06±2.11cmH2O); p<0.0005. The highest average insertion time was found in the LMA-P group (38.77±3.2sec) compared to LTS-D (21.66±2.31sec) and i-gel (27.9±2.53sec); p<0.0005. van Zundert et al. [8] compared three airway devices in their study, LMA-Supreme (LMA-S) laryngeal mask, LMA-
ProSeal (LMA-P) laryngeal mask, and i-gel during elective surgical interventions with spontaneous breathing. This study concludes that LMA-S is the optimal airway device in terms of speed and ease of insertion compared to other SADs. Leak pressure in this study did not differ between groups. In Somri et al.’s study, our colleagues not only compared the LMA-S and LTS-D in elective small volume operations with standard criteria but also evaluated the leak pressure at different head positions (flexion, extension, rotation) [10]. In these conditions, the laryngeal tube showed the highest leak pressure during rotations, but the clinical significance of this result remains open. Other devices (LTS-D and LMA-S) showed comparable efficacy – first-attempt insertion in 86.2% and 87.5% of cases respectively; p=0.815. The authors also noted a high incidence of sore throat after surgical intervention in the group of patients with LTS-D airway devices.
LMA-S and i-gel airway devices were also compared in the meta-analysis by Chen et al., 10 controlled randomized trials were included in the study [11]. The results of this meta-analysis proved both airway devices to be equally effective in terms of frequency and speed of insertion, but it was found that the LMA-S was more likely to cause sore throat in the postoperative period, with the insertion of a nasogastric tube through the drainage airway device being slower in the i-gel group.
The work of Liew et al. shows higher leak pressure when using i-gel during elective surgery in comparison with LMA-S and LMA-P. At the same time in the group of patients with inserted i-gel, the average leak pressure was 27.31±0.92cmH2O, LMA-S=23.60±0.70cmH2O, and LMA-P=24.44±0.70cmH2O and p<0.003 [12].
To date, a large number of studies have been published demonstrating various advantages of different “second-generation” airway devices (LMA-S, LTS-D, i-gel, and LMA-P) [13-18], however, it is not yet possible to identify a clear favorite in terms of clinical efficacy and/or safety of the application. Therefore, in search of an optimal device registered in the Russian Federation, we conducted a pilot study [24, 25] and selected i-gel and LMA-Supreme airway devices as the most effective SADs.
Later on, we continued the study to increase the number of patients in groups of selected devices until statistically significant results were obtained. The main objective was to decide which device to choose for further use [26]. In addition, we decided to compare the routine technique of endotracheal intubation with supraglottic airway devices, taking into account already available data on the advantage of SADs over intubation demonstrated in other studies [7, 22, 23]. The study aimed to compare endotracheal intubation with i-gel and LMA-Supreme supraglottic airway devices in orbital osteosynthesis surgery.
Materials & Methods
This comparative perspective single-center randomized study was conducted in the Department of Anesthesiology and Intensive Care at the Advanced Training and Professional Retraining Faculty of the Ural State Medical University in Yekaterinburg Clinical Hospital No. 23, Russia, in 2021. Upon selection of patients according to the enrollment and exclusion criteria, randomization into 3 groups was carried out (with the use of https://www.random.org electronic service): 1) LMA-Supreme; 2) i-gel; 3) endotracheal tube (ETT). The size of each airway device was chosen in accord with the manufacturer’s recommendations, based on the patient’s body weight and height. Given that for i-gel airway devices the manufacturer recommends using size No. 3 for patients with a body mass of 30-60 kg and size No. 4 for patients with a body weight of 50-90 kg, the range between 50-60 kg remains a zone of possible disagreement. It appears that according to the recommendations, one can insert either i-gel No. 3 or No. 4. Taking into account data from available literature, we chose the standard option for such cases and modified the manufacturer's recommendations. For patients whose body weight is 30-55 kg i-gel No. 3 was planned to be inserted, and for patients with a body weight of 56-90 kg – No. 4. Intubation tubes were used according to standard recommendations – size 7.5-8.5 for women and size 8.5-9 for men [25]. Finally, a total of 134 patients were enrolled in the study. 42 patients were included in the LMA-S group, 49 in the i-gel group, and 43 in the ETT group. Criteria for enrolment included mild traumatic brain injury and presence of midface fractures, patients 18-70 years old, elective surgical intervention of orbital osteosynthesis with general Anesthesia, duration of the operation more than 30 min. Criteria for exclusion: 1) upper and lower jaw injury, face, neck edema, difficult intubation in past medical history or high risk thereof (Mallampati score 3-4, mouth opening <3 cm, anomalies of the facial skeleton or cervical spine); 2) body mass index (BMI) >35 kg/m², pregnancy, high risk of aspiration of gastric contents; 3) presence of chronic obstructive pulmonary disease (COPD) or other pulmonary and/or laryngopharynx diseases; 4) complications resulting in the need for prolonged artificial lung ventilation (ALV) and endotracheal intubation.
After approval by Ural State Medical University ethical committee, patients were compared by sex, age, body mass index, physical condition according to ASA classification (American Society of Anesthesiologists; ASA I, II, III is an anesthesiologic assessment of the patient's condition before surgery, according to the scale of the American Society of Anesthesiologists) and duration of surgery [2].
The Datex Aespire View machine was used for anesthesia in all cases. A noninvasive technique (oscillometric method) of MPR 6-03 Treaton Electronic Systems monitor was used to monitor central hemodynamic parameters (cardiac index and systemic vascular resistance). Datex-Ohmeda Cardiocap 5 monitor was used to measure standard hemodynamic parameters, gas exchange, and ventilation. Induction into anesthesia was preceded by standard preoxygenation, mask ventilation was used during induction. Propofol at a dose of 1.5-2.5mg/kg and fentanyl at a dose of 1-3mg/kg was used for induction into anesthesia. Anesthesia was maintained by sevoflurane in the concentration of 1-1.5 minimum alveolar concentration (MAC) and fentanyl at the dose of 2-3µg/kg/hr. For relaxation, rocuronium 0.6mg/kg was used during induction into anesthesia; injection of the drug was repeated at the dose of 0.2mg/kg if necessary. Upon reaching the required level of anesthesia and relaxation of maxillofacial muscles, endotracheal intubation or insertion of an appropriate SAD was performed. Insertion of i-gel airway device was carried out according to the ‘classical’ method using the index finger, LMA-S airway device was inserted by the method described in the instructions for use. Intubation was carried out in accord with the standard technique with the use of a laryngoscope. The following parameters were fixed – time of the airway device insertion, need for additional manipulations (jaw thrust maneuver, head extension, rotation of the device, head rotation), how many attempts were made to insert the SAD. Insertion was considered completed when the first wave appeared on the capnographic curve after the beginning of ALV. Insertion was performed by an anesthesiologist with work experience of at least three years, having had experience with each airway device (at least 10 insertions before the beginning of the study). In case of failure to insert the airway device after two attempts, the patient received endotracheal intubation. A manual pressure monitoring cuff device (Portex manometer) was used to set the pressure in the cuff for the LMA-S at 60cmH2O and in the cuff of the intubation tube at 25 cm H2O. The drainage (gastric) canal of SAD was used as an additional criterion for the correct position of the airway device (jugular test) and always remained open. No patient enrolled in the study needed to administer the stomach tube.
Patients were ventilated in the Pressure Control Ventilation – Volume Guaranteed (PCV-VG) mode, tidal volume (TV) was set in the range from 6-8ml/kg of ideal body weight, and the respiratory frequency was initially set at 14 per minute and was further corrected to achieve normocapnia. Before the beginning of and after the operation, a test for measuring OLP was performed. For this purpose, the device was switched to bag ventilation mode, APL valve was set at 30cmH2O with an oxygen inflow of 3L/min. Neck auscultation was performed with a stethoscope in laryngeal projection; as the circuit pressure rose it was fixed on the manometer, at which point the characteristic sound of air leak appeared. Heart rate (HR), mean arterial pressure (MAP), systemic vascular resistance (SVR), cardiac index (CI), arterial oxygen saturation measured by non-invasive method (SpO2) were recorded at the following stages: before surgery; after airway device insertion; 10, 20, 30 minutes after the beginning of the surgery; at end of surgery. After endotracheal intubation and the beginning of the ALV, ventilation parameters were also recorded at the aforementioned stages, except for the before surgery stage. Minute volume (MV), tidal volume (TV), end-tidal carbon dioxide (EtCO2), peak inspiratory pressure (PIP) were recorded. After the end of anesthesia, extubation (SAD removal) was performed, presence or absence of blood in the mouth was recorded. The total time of anesthesia from induction to airway device removal was also noted. In the postoperative period (3 hours after the extubation), the patient was questioned about the presence of problems with swallowing, pain, and discomfort in the oropharynx.
For statistical processing, the EZR program (version 1.37) on R commander (version 3.4.1) was used. The Shapiro-Wilk test was used to evaluate the normal distribution of continuous variables. The Kruskal-Wallis h-criterion was used to analyze continuous data. Pearson’s χ²-test with Yates’ correction in case of need or F-test was used for categorical data analysis. The statistical difference is p<0.05.
Findings
The results of comparing sex, age, BMI, physical condition according to ASA classification, and duration of surgery were shown in Table 1.
No significant differences in ALV parameters were obtained between groups at the study stages. However, it should be noted that the TV differed significantly between the groups at all study stages. At stage 1 minute after the airway device insertion, TV was significantly lower in the LMA-S group than in the i-gel and ETT groups. The same pattern was observed at all subsequent study stages (Table 2).
Nevertheless, account must be taken that, despite the statistical validity of the differences, this indicator is within normal values and no significant differences in the minute volume and peak pressure were obtained in the studied groups. EtCO2 at the specified stages of the operation was within normal values, indicating that there was no clinical difference in respiratory volume. Although at the 30-minute stage and the end of the operation there was a significantly higher value of EtCO2 in the LMA-S group (p>0.05), this parameter was again within normal values, and in our opinion, this statistical difference does not have clinical importance. No significant differences in hemodynamic parameters were obtained at most study stages, but a significantly higher value of mean arterial pressure, heart rate, cardiac index, and systemic vascular resistance in the ETT group at the stage 1 minute after insertion should be noted (Table 2). There was a significant difference in OLP between the groups at the beginning and the end of the surgical intervention (p<0.05). Herewith, 1 minute after the airway device insertion it was significantly higher in the ETT group compared to LMA-S and i-gel (p<0.05). Leak pressure between LMA-S and i-gel did not differ at this stage (p>0.05). At the end of the surgery, OLP also remained significantly higher in the ETT group compared to LMA-S and i-gel, but at this stage, there was also a significant difference between SADs (LMA-S and i-gel). Significant differences in the time of airway device insertion in the studied groups were also obtained. in ETT group. Apart from that, the number of patients who required additional maneuvers for SAD insertion was different.
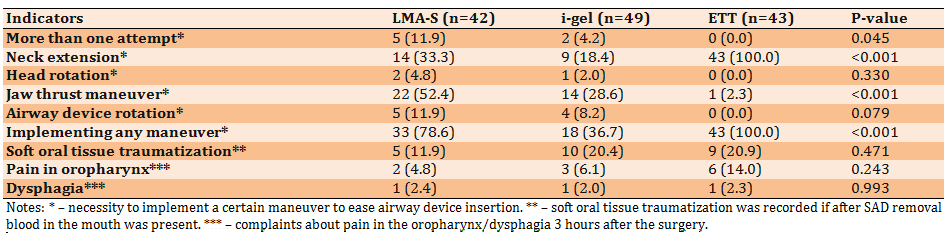
Significant differences were obtained in the frequency of neck extension, jaw thrust maneuver during airway device insertion and the total number of maneuvers (p<0.05). The largest number of neck extensions was registered in the ETT group, which was quite natural considering the standard intubation technique, with no difference between LMA-S and i-gel groups on this parameter. The jaw thrust maneuver was most often used during LMA-S insertion. The total number of maneuvers required for the airway device insertion was the highest in the ETT group and the lowest in the i-gel group. The number of complications (presence of blood in the mouth, sore throat, dysphagia) was minimal and did not differ between the groups (Table 3).
If airway device-assisted ALV proved ineffective, endotracheal intubation was required, and patients were excluded from the study. There were 4 such patients in the LMA-S group (8.7%) and 6 patients in the i-gel group (10.9%).
Supraglottic airway devices (SADs) are firmly established in modern anesthesiology practice and are often considered as one of the options to ensure airway management in patients with ‘difficult airways’ [1, 2]. These devices are used in prehospital medical care [3-6] and resuscitation [3]. One of the variants of their use is airway control during anesthesia, where they have also demonstrated their safety and efficiency [7-21]. By providing airway control with rather a simple insertion and less invasiveness in many situations, SADs can
compete with the “gold standard” in maintaining airway management, that is, endotracheal intubation [7, 22, 23]. At the same time, a wide variety of supraglottic airway devices available on the markets is an advantage as well as a disadvantage of this technology, as it makes it much more difficult to select the necessary device in each specific situation. The analysis of publications on this topic sometimes gives contradictory data with restrictions. Very often in our clinic, we admit patients with mild traumatic brain injury and fractured midface, who need orbital fractures osteosynthesis. Features of this category of interventions include a low degree of anesthetic risk (ASA I or II, according to the American Society of Anesthesiologists scale), and the average duration of surgery of 30-60 minutes. It requires deep anesthesia, relaxation, and controlled ventilation to make sure the surgeon can operate comfortably. Supraglottic airway devices allow providing all the aforementioned conditions while being less aggressive compared to the standard endotracheal intubation. This fact was the reason for the comparative assessment of SADs and intubation in this type of operation. Having analyzed publications devoted to the comparison of second-generation airway devices in various surgical interventions, we could not conclude the obvious advantage of any device.
The most common parameters for comparing airway devices are time, efficacy, and ease of insertion, the oropharyngeal leak pressure (OLP; peak airway pressure at which leak is recorded), and the number of complications associated with the use of the device. In the work of Das et al. [9] i-gel, ProSeal and Laryngeal Tube Suction D (LTS-D) airway devices were compared during elective surgery using general anesthesia. The devices showed comparable high efficacy (LMA-P – 96%, i-gel – 100%, LTS-D – 94%). The smallest leak pressure was demonstrated in the i-gel group (23.38±2.06cmH2O) compared to LMA-P (28.5±2.8cmH2O) and LTS-D (26.06±2.11cmH2O); p<0.0005. The highest average insertion time was found in the LMA-P group (38.77±3.2sec) compared to LTS-D (21.66±2.31sec) and i-gel (27.9±2.53sec); p<0.0005. van Zundert et al. [8] compared three airway devices in their study, LMA-Supreme (LMA-S) laryngeal mask, LMA-
ProSeal (LMA-P) laryngeal mask, and i-gel during elective surgical interventions with spontaneous breathing. This study concludes that LMA-S is the optimal airway device in terms of speed and ease of insertion compared to other SADs. Leak pressure in this study did not differ between groups. In Somri et al.’s study, our colleagues not only compared the LMA-S and LTS-D in elective small volume operations with standard criteria but also evaluated the leak pressure at different head positions (flexion, extension, rotation) [10]. In these conditions, the laryngeal tube showed the highest leak pressure during rotations, but the clinical significance of this result remains open. Other devices (LTS-D and LMA-S) showed comparable efficacy – first-attempt insertion in 86.2% and 87.5% of cases respectively; p=0.815. The authors also noted a high incidence of sore throat after surgical intervention in the group of patients with LTS-D airway devices.
LMA-S and i-gel airway devices were also compared in the meta-analysis by Chen et al., 10 controlled randomized trials were included in the study [11]. The results of this meta-analysis proved both airway devices to be equally effective in terms of frequency and speed of insertion, but it was found that the LMA-S was more likely to cause sore throat in the postoperative period, with the insertion of a nasogastric tube through the drainage airway device being slower in the i-gel group.
The work of Liew et al. shows higher leak pressure when using i-gel during elective surgery in comparison with LMA-S and LMA-P. At the same time in the group of patients with inserted i-gel, the average leak pressure was 27.31±0.92cmH2O, LMA-S=23.60±0.70cmH2O, and LMA-P=24.44±0.70cmH2O and p<0.003 [12].
To date, a large number of studies have been published demonstrating various advantages of different “second-generation” airway devices (LMA-S, LTS-D, i-gel, and LMA-P) [13-18], however, it is not yet possible to identify a clear favorite in terms of clinical efficacy and/or safety of the application. Therefore, in search of an optimal device registered in the Russian Federation, we conducted a pilot study [24, 25] and selected i-gel and LMA-Supreme airway devices as the most effective SADs.
Later on, we continued the study to increase the number of patients in groups of selected devices until statistically significant results were obtained. The main objective was to decide which device to choose for further use [26]. In addition, we decided to compare the routine technique of endotracheal intubation with supraglottic airway devices, taking into account already available data on the advantage of SADs over intubation demonstrated in other studies [7, 22, 23]. The study aimed to compare endotracheal intubation with i-gel and LMA-Supreme supraglottic airway devices in orbital osteosynthesis surgery.
Materials & Methods
This comparative perspective single-center randomized study was conducted in the Department of Anesthesiology and Intensive Care at the Advanced Training and Professional Retraining Faculty of the Ural State Medical University in Yekaterinburg Clinical Hospital No. 23, Russia, in 2021. Upon selection of patients according to the enrollment and exclusion criteria, randomization into 3 groups was carried out (with the use of https://www.random.org electronic service): 1) LMA-Supreme; 2) i-gel; 3) endotracheal tube (ETT). The size of each airway device was chosen in accord with the manufacturer’s recommendations, based on the patient’s body weight and height. Given that for i-gel airway devices the manufacturer recommends using size No. 3 for patients with a body mass of 30-60 kg and size No. 4 for patients with a body weight of 50-90 kg, the range between 50-60 kg remains a zone of possible disagreement. It appears that according to the recommendations, one can insert either i-gel No. 3 or No. 4. Taking into account data from available literature, we chose the standard option for such cases and modified the manufacturer's recommendations. For patients whose body weight is 30-55 kg i-gel No. 3 was planned to be inserted, and for patients with a body weight of 56-90 kg – No. 4. Intubation tubes were used according to standard recommendations – size 7.5-8.5 for women and size 8.5-9 for men [25]. Finally, a total of 134 patients were enrolled in the study. 42 patients were included in the LMA-S group, 49 in the i-gel group, and 43 in the ETT group. Criteria for enrolment included mild traumatic brain injury and presence of midface fractures, patients 18-70 years old, elective surgical intervention of orbital osteosynthesis with general Anesthesia, duration of the operation more than 30 min. Criteria for exclusion: 1) upper and lower jaw injury, face, neck edema, difficult intubation in past medical history or high risk thereof (Mallampati score 3-4, mouth opening <3 cm, anomalies of the facial skeleton or cervical spine); 2) body mass index (BMI) >35 kg/m², pregnancy, high risk of aspiration of gastric contents; 3) presence of chronic obstructive pulmonary disease (COPD) or other pulmonary and/or laryngopharynx diseases; 4) complications resulting in the need for prolonged artificial lung ventilation (ALV) and endotracheal intubation.
After approval by Ural State Medical University ethical committee, patients were compared by sex, age, body mass index, physical condition according to ASA classification (American Society of Anesthesiologists; ASA I, II, III is an anesthesiologic assessment of the patient's condition before surgery, according to the scale of the American Society of Anesthesiologists) and duration of surgery [2].
The Datex Aespire View machine was used for anesthesia in all cases. A noninvasive technique (oscillometric method) of MPR 6-03 Treaton Electronic Systems monitor was used to monitor central hemodynamic parameters (cardiac index and systemic vascular resistance). Datex-Ohmeda Cardiocap 5 monitor was used to measure standard hemodynamic parameters, gas exchange, and ventilation. Induction into anesthesia was preceded by standard preoxygenation, mask ventilation was used during induction. Propofol at a dose of 1.5-2.5mg/kg and fentanyl at a dose of 1-3mg/kg was used for induction into anesthesia. Anesthesia was maintained by sevoflurane in the concentration of 1-1.5 minimum alveolar concentration (MAC) and fentanyl at the dose of 2-3µg/kg/hr. For relaxation, rocuronium 0.6mg/kg was used during induction into anesthesia; injection of the drug was repeated at the dose of 0.2mg/kg if necessary. Upon reaching the required level of anesthesia and relaxation of maxillofacial muscles, endotracheal intubation or insertion of an appropriate SAD was performed. Insertion of i-gel airway device was carried out according to the ‘classical’ method using the index finger, LMA-S airway device was inserted by the method described in the instructions for use. Intubation was carried out in accord with the standard technique with the use of a laryngoscope. The following parameters were fixed – time of the airway device insertion, need for additional manipulations (jaw thrust maneuver, head extension, rotation of the device, head rotation), how many attempts were made to insert the SAD. Insertion was considered completed when the first wave appeared on the capnographic curve after the beginning of ALV. Insertion was performed by an anesthesiologist with work experience of at least three years, having had experience with each airway device (at least 10 insertions before the beginning of the study). In case of failure to insert the airway device after two attempts, the patient received endotracheal intubation. A manual pressure monitoring cuff device (Portex manometer) was used to set the pressure in the cuff for the LMA-S at 60cmH2O and in the cuff of the intubation tube at 25 cm H2O. The drainage (gastric) canal of SAD was used as an additional criterion for the correct position of the airway device (jugular test) and always remained open. No patient enrolled in the study needed to administer the stomach tube.
Patients were ventilated in the Pressure Control Ventilation – Volume Guaranteed (PCV-VG) mode, tidal volume (TV) was set in the range from 6-8ml/kg of ideal body weight, and the respiratory frequency was initially set at 14 per minute and was further corrected to achieve normocapnia. Before the beginning of and after the operation, a test for measuring OLP was performed. For this purpose, the device was switched to bag ventilation mode, APL valve was set at 30cmH2O with an oxygen inflow of 3L/min. Neck auscultation was performed with a stethoscope in laryngeal projection; as the circuit pressure rose it was fixed on the manometer, at which point the characteristic sound of air leak appeared. Heart rate (HR), mean arterial pressure (MAP), systemic vascular resistance (SVR), cardiac index (CI), arterial oxygen saturation measured by non-invasive method (SpO2) were recorded at the following stages: before surgery; after airway device insertion; 10, 20, 30 minutes after the beginning of the surgery; at end of surgery. After endotracheal intubation and the beginning of the ALV, ventilation parameters were also recorded at the aforementioned stages, except for the before surgery stage. Minute volume (MV), tidal volume (TV), end-tidal carbon dioxide (EtCO2), peak inspiratory pressure (PIP) were recorded. After the end of anesthesia, extubation (SAD removal) was performed, presence or absence of blood in the mouth was recorded. The total time of anesthesia from induction to airway device removal was also noted. In the postoperative period (3 hours after the extubation), the patient was questioned about the presence of problems with swallowing, pain, and discomfort in the oropharynx.
For statistical processing, the EZR program (version 1.37) on R commander (version 3.4.1) was used. The Shapiro-Wilk test was used to evaluate the normal distribution of continuous variables. The Kruskal-Wallis h-criterion was used to analyze continuous data. Pearson’s χ²-test with Yates’ correction in case of need or F-test was used for categorical data analysis. The statistical difference is p<0.05.
Findings
The results of comparing sex, age, BMI, physical condition according to ASA classification, and duration of surgery were shown in Table 1.
No significant differences in ALV parameters were obtained between groups at the study stages. However, it should be noted that the TV differed significantly between the groups at all study stages. At stage 1 minute after the airway device insertion, TV was significantly lower in the LMA-S group than in the i-gel and ETT groups. The same pattern was observed at all subsequent study stages (Table 2).
Nevertheless, account must be taken that, despite the statistical validity of the differences, this indicator is within normal values and no significant differences in the minute volume and peak pressure were obtained in the studied groups. EtCO2 at the specified stages of the operation was within normal values, indicating that there was no clinical difference in respiratory volume. Although at the 30-minute stage and the end of the operation there was a significantly higher value of EtCO2 in the LMA-S group (p>0.05), this parameter was again within normal values, and in our opinion, this statistical difference does not have clinical importance. No significant differences in hemodynamic parameters were obtained at most study stages, but a significantly higher value of mean arterial pressure, heart rate, cardiac index, and systemic vascular resistance in the ETT group at the stage 1 minute after insertion should be noted (Table 2). There was a significant difference in OLP between the groups at the beginning and the end of the surgical intervention (p<0.05). Herewith, 1 minute after the airway device insertion it was significantly higher in the ETT group compared to LMA-S and i-gel (p<0.05). Leak pressure between LMA-S and i-gel did not differ at this stage (p>0.05). At the end of the surgery, OLP also remained significantly higher in the ETT group compared to LMA-S and i-gel, but at this stage, there was also a significant difference between SADs (LMA-S and i-gel). Significant differences in the time of airway device insertion in the studied groups were also obtained. in ETT group. Apart from that, the number of patients who required additional maneuvers for SAD insertion was different.
Significant differences were obtained in the frequency of neck extension, jaw thrust maneuver during airway device insertion and the total number of maneuvers (p<0.05). The largest number of neck extensions was registered in the ETT group, which was quite natural considering the standard intubation technique, with no difference between LMA-S and i-gel groups on this parameter. The jaw thrust maneuver was most often used during LMA-S insertion. The total number of maneuvers required for the airway device insertion was the highest in the ETT group and the lowest in the i-gel group. The number of complications (presence of blood in the mouth, sore throat, dysphagia) was minimal and did not differ between the groups (Table 3).
If airway device-assisted ALV proved ineffective, endotracheal intubation was required, and patients were excluded from the study. There were 4 such patients in the LMA-S group (8.7%) and 6 patients in the i-gel group (10.9%).
Table 1) Base characteristics of patient groups of airway device type
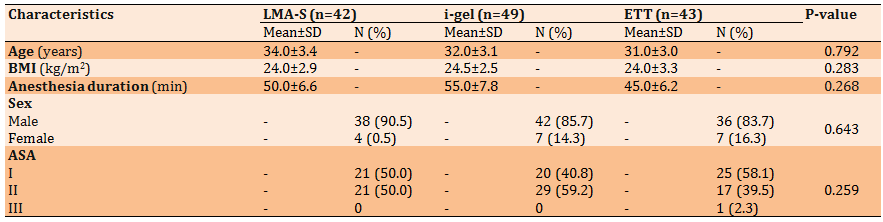
Table 2) The mean (and range) of Hemodynamic, gas exchange and OLP indicators at the study stages

Table 3) Frequency results of basic parameters of airway device insertion (the numbers in parentheses are in percent)
Discussion
We have not found any publications comparing LMA-Supreme, i-gel, and ETT airway devices for orbital osteosynthesis surgery in the literature available to us.
However, we believe it is necessary to describe several studies comparing LMA-ProSeal supraglottic airway device with endotracheal intubation in various interventions, as this airway device does not differ fundamentally from LMA-S that we used [7, 22, 23]. In one of them, Lim et al. applied the abovementioned airway device and compared it with endotracheal intubation in laparoscopic operations in gynecology [7]. The authors concluded that the insertion of a supraglottic airway device takes less time in comparison with intubation and is accompanied by a less hemodynamic stress response. Saraswat et al. made a comparative assessment of LMA-ProSeal with intubation in laparoscopic operations and concluded that the airway device is a worthy alternative to intubation with comparable hemodynamic parameters, gas exchange, and the number of complications [22]. Güleç et al. compared LMA-ProSeal with intubation for planned laparoscopic cholecystectomy and found a higher level of cortisol in the group of endotracheal intubations, and concluded that insertion of a supraglottic airway device is accompanied by less metabolic stress in comparison with intubation [23]. In any case, the data obtained by us are quite consistent with the results described above. The shortest insertion time was obtained in the i-gel airway device group. We also found the state of hemodynamics hyperdynamic response to endotracheal intubation, which is not present in the SAD groups. And it is quite natural and explainable because the trachea and vocal cords are by all means more reflexogenic zones than the laryngopharynx, where the supraglottic airway device is placed. This fact, despite the lack of difference in the number of complications between the groups we studied, allows us to consider the insertion of supraglottic airway devices as a gentler method in comparison with endotracheal intubation. And, of course, it should be taken into account when planning anesthesia in patients with a high risk of cardiovascular complications.
The data we obtained on the value of OLP are comparable with the leak pressure described in publications comparing different combinations of similar airway devices [9, 12, 16, 17]. The leak pressure recorded in our study was within 21-30cmH2O, which is quite enough to perform effective ALV in patients without obstructive and restrictive lung diseases. At the same time, naturally, the measurement of leak pressure in the endotracheal intubation group was a mere formality, because a leak-proof cuff allows ventilation with peak pressure exceeding 30cmH2O. However, we found it unsafe to raise the airway pressure above 30cmH2O, so we inserted an adjustable pressure-limiting valve at this number. And the highest leak pressure was recorded in the ETT group at all stages of registration. A significant difference in leak pressure between LMA-S and i-gel was obtained at the end of the operation. At the same time, the higher leak pressure in the LMA-S group is probably due to the presence of the cuff in this device and better leak-proofness owing to it. Taking into account the smallest number of maneuvers and the shortest time required to insert the i-gel airway device, it can be concluded that this SAD is the easiest to insert and is the airway device of choice in patients with uncompromised breathing apparatus. In situations where high peak pressure ventilation may be required, it is probably better to use an LMA-S airway device or endotracheal intubation.
Our study limitations include, in the first place, the absence of researchers’ “blindness” when recording parameters at the study stages, and secondly, the peculiarities of the patients enrolled in the study, i.e. young patients with low anesthetic risk and without severe comorbidity, which does not allow extrapolating the study data to the entire population of patients requiring SAD insertion. It should be noted that there is no hemodynamics hyperdynamic response to insertion of LMA-S and i-gel airway devices in comparison with endotracheal intubation. At the same time, the i-gel airway device is the easiest to insert but provides smaller leak pressure in comparison with LMA-S and endotracheal intubation. Despite some statistical differences in individual parameters, both SADs (LMA-Supreme and i-gel) can be equally effective airway devices in orbital osteosynthesis surgery and provide ventilation and gas exchange parameters comparable with intubation. Regarding the number of complications, they do not differ from the standard intubation technique. The statistical difference in individual comparison parameters does not indicate the necessity to abandon the clinical use of a particular airway device, in addition, study data are often contradictory. Aiming to make a comparative assessment of LMA-S and i-gel supraglottic airway devices with endotracheal intubation, we were looking to find the optimal airway device for this surgical intervention. But as is often the case in medicine, there is nothing universal and in each specific situation, we need to focus on the patient’s peculiarities.
Conclusion
LMA-S and i-gel supraglottic airway devices allow for normal lung ventilation and gas exchange, are accompanied by equally low levels of complications, and may be used as an alternative to endotracheal intubation during orbital osteosynthesis.
Acknowledgments: The authors did not declare.
Ethical Permissions: The ethical code was UR8023.4ETH.
Conflicts of Interests: The authors did not declare.
Authors’ Contribution: Kostetskiy I (First Author), Introduction Writer/Main Researcher (25%); Bagin V (Second Author), Methodologist/Statistical Analyst (25%); Kaliskin A (Third Author), Discussion Writer/Methodologist (20%); Shamrikov A (Fourth Author), Discussion Writer/Data Analyst (15%); Davydova N (Fifth Author), Introduction Writer/Assistant Researcher (15%)
Funding/Support: The authors did not declare.
Keywords:
References
1. Frerk C, Mitchell VS, McNarry AF, Mendonca C, Bhagrath R, Patel A. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth. 2015;115(6):827-48. [Link] [DOI:10.1093/bja/aev371]
2. Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT, Nickinovich DG, et al. Practice guidelines for the management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesth. 2013;118(2):251-70. [Link] [DOI:10.1097/ALN.0b013e31827773b2]
3. Gahan K, Studnek JR, Vandeventer S. King LT-D use by urban basic life support first responders as the primary airway device for out-of-hospital cardiac arrest. Resuscitation. 2011;82(12):1525-8. [Link] [DOI:10.1016/j.resuscitation.2011.06.036]
4. Hubble MW, Wilfong DA, Brown LH, Hertelendy A, Benner RW. A meta-analysis of prehospital airway control techniques, part II: Alternative airway devices and cricothyrotomy success rates. Prehosp Emerg Care. 2010;14(4):515-30. [Link] [DOI:10.3109/10903127.2010.497903]
5. Andreenko AA, Grachev IN, Faizov II. Comparison of intubating supraglottic airways lma fastrach™ and ilts-d® under normal and simulated difficult airways - Study on the mannequin. Ann Crit Care. 2017;1:12-18. [Russian] [Link] [DOI:10.21320/1818-474X-2017-1-12-19]
6. Schalk R, Byhahn C, Fausel F, Egner A, Oberndörfer D, Walcher F, et al. Out-of-hospital airway management by paramedics and emergency physicians using laryngeal tubes. Resuscitation. 2010;81(3):323-6. [Link] [DOI:10.1016/j.resuscitation.2009.11.007]
7. Lim Y, Goel S, Brimacombe JR. The ProSeal™ laryngeal mask airway is an effective alternative to laryngoscope-guided tracheal intubation for gynaecological laparoscopy. Anaesth Intensive Care. 2007;35(1):52-6. [Link] [DOI:10.1177/0310057X0703500106]
8. Van Zundert TC, Brimacombe JR. Similar oropharyngeal leak pressures during anaesthesia with i-gel, LMA-ProSeal and LMA-Supreme Laryngeal Masks. Acta Anaesth Belg. 2012;63(1):35-41. [Link]
9. Das B, Varshney R, Mitra S. A randomised controlled trial comparing ProSeal laryngeal mask airway, i gel and Laryngeal Tube Suction D under general anaesthesia for elective surgical patients requiring controlled ventilation. Indian J Anaesth. 2017;61(12):32-7. [Link] [DOI:10.4103/ija.IJA_339_17]
10. Somri M, Vaida S, Fornari GG, Mendoza GR, Charco-Mora P, Hawash N, et al. A randomized prospective controlled trial comparing the laryngeal tube suction disposable and the supreme laryngeal mask airway: the influence of head and neck position on oropharyngeal seal pressure. BMC Anesth. 2016;6:87. [Link] [DOI:10.1186/s12871-016-0290-2]
11. Chen X, Jiao J, Cong X, Liu L, Wu X. A comparison of the performance of the I-gelTM vs. the LMA-STM during Anesthesia: A meta-analysis of randomized controlled trials. PLoS One. 2013;8(8):e71910. [Link] [DOI:10.1371/journal.pone.0071910]
12. Liew GHC, Yu ED, Shah SS, Kothandan H. Comparison of the clinical performance of i-gel, LMA Supreme and LMA ProSeal in elective surgery. Singapore Med J. 2016;57(8):432-7. [Link] [DOI:10.11622/smedj.2016133]
13. Maitra S, Khanna P, Baidya DK. Comparison of laryngeal mask airway Supreme and laryngeal mask airway Pro-Seal for controlled ventilation during general anaesthesia in adult patients: systematic review with meta-analysis. Eur J Anaesth. 2014;31(5):266-73. [Link] [DOI:10.1097/01.EJA.0000435015.89651.3d]
14. Arı DE, Ar AY, Karip CŞ, Siyahkoç İ, Arslan AH, Akgün FN. Comparison of I-gel with classic laryngeal mask airway regarding the ease of use and clinical performance. Turk J Anaesth Reanim. 2015;43:299-303. [Link] [DOI:10.5152/TJAR.2015.71542]
15. Kömür E, Bakan N, Tomruk ŞG, Karaören G, Doğan ZT. Comparison of the supraglottic airway devices classic, fastrach and supreme laryngeal mask airway: A prospective randomised clinical trial of efficacy, safety and complications. Turk J Anaesth Reanim. 2015;43(6):406-11. [Link] [DOI:10.5152/TJAR.2015.97830]
16. Mukadder S, Zekine B, Erdogan KG, Ulku O, Muharrem U, Saim Y, et al. Comparison of the Proseal, Supreme, and I-Gel SAD in gynecological laparoscopic surgeries. Sci World J. 2015:634320. [Link] [DOI:10.1155/2015/634320]
17. Park SY, Rim JC, Kim H, Lee JH, Chung CJ. Comparison of i-gel® and LMA Supreme® during laparoscopic cholecystectomy. Korean J Anesth. 2015;68(5):455-61. [Link] [DOI:10.4097/kjae.2015.68.5.455]
18. Russo SG, Cremer S, Galli T, Eich C, Bräuer A, Crozier TA, et al. Randomized comparison of the i-gel™, the LMA Supreme™, and the Laryngeal Tube Suction-D using clinical and fibreoptic assessments in elective patients. BMC Anesthesiol. 2012;12:18. [Link] [DOI:10.1186/1471-2253-12-18]
19. Likhvantsev VV, Bolshedvorov RV. Optimization of initial anesthesia in a one-day surgical hospital. Gen Reanimatol. 2010;6(1):44-8. [Link] [DOI:10.15360/1813-9779-2010-1-44]
20. Mironov PI, Estekhin AM, Mirasov AA. Anaesthetic maintenance with laryngeal mask for a laparoscopic surgery in pediatric patients. Russ J Anaesth Reanimatol. 2013;(1):10-4. [Russian] [Link]
21. Dolbneva EL, Stamov VI, Gavrilov SV, Mizikov VM. Intubating laryngeal mask efficacy in obese and overweight patients. Russ J Anaesth Reanimatol. 2013;2:58-62. [Russian] [Link]
22. Saraswat N, Kumar A, Mishra A, Gupta A, Saurabh G, Srivastava U. The comparison of Proseal laryngeal mask airway and endotracheal tube in patients undergoing laparoscopic surgeries under general anesthesia. Indian J Anaesth. 2011;55(2):129-34. [Link] [DOI:10.4103/0019-5049.79891]
23. Güleç H, Cakan T, Yaman H, Kilinç AŞ, Başar H. Comparison of hemodynamic and metabolic stress responses caused by endotracheal tube and Proseal laryngeal mask airway in laparoscopic cholecystectomy. J Res Med Sci. 2012;17(2):148-53. [Link]
24. Kostetskiy IV, Shamrikov AA, Bagin VA, Kaliskin AA. Comparison of LMA-SUPREME, i-gel and LTS-D during orbital fractures reconstruction. Russ J Anaesth Reanimatol. 2018;4:57-63. [Russian] [Link] [DOI:10.17116/anaesthesiology201804157]
25. Gel'fand BR, Kirienko PA, Grinenko TF, Gur'yanov VA. Anesthesiology and Reanimatology. Moscow: Literra; 2006. [Russian] [Link]
26. Kostetskiy IV, Shamrikov АА, Bagin VА, Kaliskin АА. Results of the randomized comparative study of second-generation supraglottic airways in orbital osteosynthesis. Messenger Anesth Resusc. 2019;16(6):46-53. [Russian] [Link] [DOI:10.21292/2078-5658-2019-16-6-46-53]