Volume 13, Issue 4 (2021)
Iran J War Public Health 2021, 13(4): 313-317 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2021/11/21 | Accepted: 2021/12/27 | Published: 2022/02/12
Received: 2021/11/21 | Accepted: 2021/12/27 | Published: 2022/02/12
How to cite this article
Khairi Hussein K, Razzaq Hayyawy M, Mohammud Habash M. Seton in Managing High Anal Fistula. Iran J War Public Health 2021; 13 (4) :313-317
URL: http://ijwph.ir/article-1-1069-en.html
URL: http://ijwph.ir/article-1-1069-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
1- College of Medicine, Tikrit University, Tikrit, Iraq
2- Council of Arabic Board for Medical Specialities, Baghdad, Iraq
3- Department of Surgery, College of Medicine, Diyala University, Baqubah, Iraq
2- Council of Arabic Board for Medical Specialities, Baghdad, Iraq
3- Department of Surgery, College of Medicine, Diyala University, Baqubah, Iraq
Full-Text (HTML) (2494 Views)
Introduction
A fistula is an aberrant passage connecting one internal cavity to another or outside world. It may or may not be lined by mucous membrane or epithelium. An infection of the anal glands that spread down the intersphincteric plane to develop a leaking perianal abscess causes nearly all anal fistulas. These abscesses can leak in any path and plane, resulting in various fistulae. [1]. The incidence rate is 8.6 cases per 100,000 people. Men had a ratio of 12.3 cases per 100,000 people. In women, there are 5.6 instances per 100,000 people. A male-to-female ratio of 1.8:1 exists. Patients are 38.3 years old on average [2]. According to the cryptoglandular concept, an infection begins to develop in the anal gland and spreadsto the muscle layers of the anal sphincters, causing an anorectal abscess. A granular, lined channel may be left behind after surgical or voluntary drainage in the perianal region, causing repeated problems. According to several studies, anorectal abscess leads to creating a fistula pathway in 7-40% of cases [3, 4]. Almost nothing has changed in understanding the illness process since this early phase. Parks improved the classification method that is still widely used today in 1976. Over the last 30 years, several researchers have reported innovative techniques and case studies to reduce the incidence rate and leakage consequences. Fistula-in-ano remains a challenging surgical illness over 2500 decades of practice [2]. Generally, Fistula-in-ano is caused in various cases such as previous anorectal abscess, trauma, Crohn’s disease, anal fissure, carcinoma, radiation therapy, actinomycosis, tuberculosis and chlamydial infections, etc. [5]. Seton serves two goals and identifies the amount of sphincter muscle involved visually. These are used to evacuate the fluid, encourage fibrosis, and cut through the fissure. Large silk sutures, silicone-based vascular markers, or rubber bands inserted through the fistula passage can all be used to make seton. In the surgery, sometimes, early and delayed postoperative complications can occur. The early postoperative complications can be bleeding, urinary retention, fecal impaction, Thrombosed hemorrhoids, etc. The delayed postoperative complications can be Incontinence (stool), anal stenosis, delayed wound healing and recurrence. With this background, the study aimed to evaluate the efficacy of loose seton use in managing high anal fistula. '
Materials and Methods
A prospective cohort study (n=68) for low and high anal fistula management was designed. Seton placement's high anal fistula management (n=26) was carried out in a Baghdad teaching hospital's surgical unit. Initially, around 68 patients were screened (ages range between 17-63 years, both gender). A questionnaire containing the history of pain, swelling, and spontaneous or planned surgical drainage of an anorectal abscess with duration was taken. A review of symptoms of abdominal pain, weight loss and change in bowel habits were noted. Past medical history of inflammatory bowel disease, diverticulitis, previous radiation therapy for prostate or rectal cancer, tuberculosis, steroid therapy, HIV infection and past surgical history for fistula in one was also recorded.
Diagnosis
The diagnosis was made in three ways, i.e., physical examination, use of proctoscopy and radiological examination. The details of each are given below.
Physical examination
The patient in the left lateral position examined the whole perineum for an external opening that looks like an open sinus or granular tissue rise. On digital rectal examination, uncontrolled secretion via the external orifice may be visible or easily interpretable. The anus and a digital rectal examination (DRE) by inserting a lubricated, gloved finger into the rectum are done. Underneath the skin, a fibrous tract or cord may be seen. It also aided us in identifying any remaining acute inflammation that had not been drained.
Proctoscopy
In some patients, an interior opening wasn't identified by palpation or bypassing the probe through it. And to determine whether the opening was in the anal canal or above the anorectal ring in the rectum. Besides this, Proctoscopy showed us the state of the rectal mucosa and helped decide if any other underlying factors like proctocolitis were present.
Radiological examination
When in doubt or if a track was expected to proceed to more than one orifice, i.e., if the path was considered bifurcate, radiological evaluation of the fistulous track following injection of Conery Dye proved beneficial. High anorectal fistulas or fistulas with one or more pathways and openings benefited from this. Full radiological investigation and Sigmoidoscopy undertook in a patient with a previous history of recurrence to exclude any rectal tumor or inflammatory bowel disease involving the rectum.
Classification of patients
From clinical and radiological examinations, patients were divided into two groups:
1) Group A (n=42): Patients with low fistula type were treated by fistulotomy.
2) Group B (n=26): Patient with high fistula, 23 patients with a single opening, and three patients with multiple opening high fistulae.
Only group B was considered for the operations—Seton treated all the patients with high fistula type.
Preoperative preparation and operative procedure
An enema should be used to empty the lower bowel about an hour before the operation. As a preventive precaution, bowel sterilization is not required.
The Seton was usually inserted at the procedures were performed in the operating room with brief general anesthesia. The patient was examined in the left lateral position. The pre-rectal examination would reveal the diagnosis, and the fistula tract was identified by probing with the metallic malleable probe. Incision of skin from external opening of the fistula to the anal verge, subcutaneous tissue, internal sphincter and superficial part of the external sphincter. Insertion of loose Seton. A non-absorbable suture (2 silk). A Seton was left loosely and kept in situ for three months.
Follow‐up parameters
In follow-up care, twice daily, Sits baths, analgesics, and stool bulking agents (e.g., bran, psyllium products) were used. Repeated examinations were carried out every four weeks interval. At each visit position of the Seton was assessed. Wound healing detection of any recurrence were also recorded.
Statistical analysis
The data were represented as the mean (percentage) of the patients. The data were subjected to statistical analysis using Graph Pad Instat (Version 3, GraphPad Software Inc., San Diego, CA, USA). Dunnett Multiple Comparison Test and one-way Analysis of Variance (ANOVA) were performed.
Findings
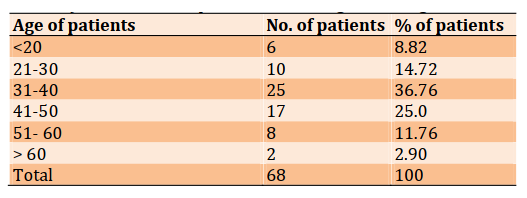
Out of 68 patients, 42 (61.8%) had a low fistula, and 26 (38.2) had a high fistula in this study. About 23 (33.8) with a single opening in the high fistula group, and 3 (4.4 %) patients had a high fistula with multiple openings. All patients with low types fistula (N=42) were treated by primary fistulotomy. All patients (n = 26) with high fistula treated by Seton. Sixty-eight patients were admitted with perianal fistula. Of these 68 patients, 51 were males, and 17 were females; the male to female ratio was 3:1. The incidence was low in both sexes below 20 years and after 50 years. Peak occurrence was noted between 20 to 50 years. Incidence according to age is shown in Table 1. The median age was 41 (range: 17-63).
Table 1) Distribution of patients, according to their age
Of these 68 patients, 51 were males, and 17 were females; the male to female ratio was 3:1. Out of these 26 patients, 23 were males, and 03 were
females; the male to female ratio was 7.7:1. The study parameters variables are depicted in Table 2.
Table 2) Study parameters variation

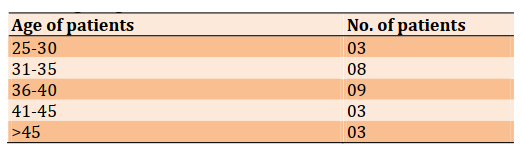
Twenty-six patients with a high type of fistula in ano treated with Seton. 34.6% of patients reported surgery history in the Seton treated group. The
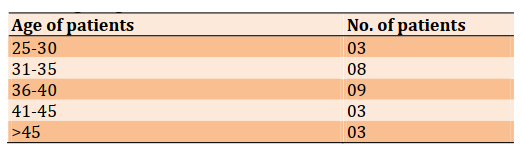
distribution of patients treated with Seton (n=26) according to age is represented in Table 3.
Table 3) Distribution of patients treated with Seton (n=26) according to age
Minor incontinence was noted in two patients (7.7%). These patients lost control of flatus which persisted for four months. No fecal incontinence was noticed in any patient. In around 21 patients, high fistula-in-ano were successfully eliminated by Seton treatment alone (Successful rate=81%). Around 05 patients, high fistula-in-ano were failed to be treated by a Seton method (Failure rate=19%). Two-stage Seton (draining/fibrosing) methods.
Discussion
Fistula-in-ano is one of the commonly encountered surgical problems. It is believed to originate from an infection of the anal glands. The main management principle is drainage of infection aerated these patients and eradicating fistulous tract with preservation of sphincter function [6]. In high perianal fistulas, the typical laying-open approach may need the loss of part or all of the sphincter muscle, affecting continence. It is self-evident that the larger the degree of anal muscle division, the greater the degree of incontinence [7]. High complicated fistulas can be successfully treated using several seton techniques with just a small loss of continence [8-12]. Conventionally, the Seton is used to manage high or complicated anal fistula [12]. The function of the Seton is to provide drainage, induce chronic fibrosis, and cut the fistulous tract with preservation of the sphincter mechanism. Cutting Seton and two-staged fistulotomy are two common techniques that have been used [13]. The Seton is tightly knotted around the fistulous tract in the cutting Seton procedure. Pressure necrosis will progressively traverse the muscle, and fibrosis will fix and protect sphincter removal. The Seton is loosely knotted, and the fistulotomy is conducted as a following step in the two-staged fistulotomy. The Seton is a drainage system that also causes fibrosis. In our study, the silk suture was used as Seton. Hippocrates first described this method [14]. Stenos can be made of various materials, but the most frequent are suture, rubber, wire, and medicated thread (Kshaarasootra) [15]. The results of this study demonstrated FIA is affecting many age groups and the data showed the 31-40 years age groups and 41-50 years were higher than other age groups with (p <0.01), with male predominance (75%) seen in this series are similar to the Seow-Choen et al. [16] and, Mc-Courtney and Finlay [15] studies.
Out of 68 patients with anal fistulae, 42 (61.8%) had a low fistula, and all of these patients were successfully treated by a simple laying-open technique. Twenty-six (38.2%) patients had high fistulae. Our findings are in accordance with the previously published studies [17-20]. They reported that "Most perineum fistulae are of the lower variation, meaning that they open underneath the anorectal ring. They are treated successfully using a laying-open procedure that does not require division of the anal sphincter muscles and so does not provide a risk of severe incontinence" [17-20]. According to Marks and Ritchie [21], high and intricate fistulae are uncommon. Only phased surgeries can treat them, which enter into the anal canal at or above the anorectal ring. The most likely explanation of this high prevalence of high fistula-in-ano is insufficient care at peripheral hospitals. High anal fistulae are harder to diagnose as well as a treat. To treat these fistulae, various surgical
procedures have been documented [22-25]. Our study suggests that most anal fistula can be treated successfully with loose Seton (success rate 81%) alone without a second surgery. Most of our patients tolerated the procedure well and were satisfied with the treatment. McCourtney and Finlay [15] described in the study, which supports the 2-stage approach with a 0-nylon Seton. The study reported that the stone is removed once wound healing is complete without division of the remaining encircled deep external sphincter muscle. The researchers reported eradicating the fistula tract in 60-78% of cases.
In our study, recurrence rates (19%) was low, and the disruption is minor and short-lived. The outcomes are equivalent to those reported using more complicated procedures to treat these complex fistulas. Abbas et al. [5] found that the long-term outcome of endorectal advancement flap for complex anorectal fistulae, Accordance with standard fistulotomy, the observed rate of incidence is 0-18% and the rate of any stool incontinence is 3-7% while following seton use, the identified rate of incidence is 0-17%, and the rate of any stool incontinence is 0-17%, and just after mucous progression flap, the reported rate of incidence is 1-17%, and the rate of any stool incontinence is 6-8% [5].
Incontinence can make fistula surgery more difficult. Nobody in this trial suffered severe incontinence. In the present study, two patients (7.7%) developed flatus incontinence, and both of them with a previous history of Perineum fistula require many procedures. The damage was just temporary and did not last in any patients. Others have also reported some lack of continence and management of flatus following surgery [26, 27].
Patients who have had previous fistula surgery have a higher risk of developing postoperative incontinence [28]. There has been a link between the rising frequency of this issue and the increasing number of previous fistula procedures. Lower resting and squeeze pressures are more likely to trigger incontinence after surgery than normal pressures [29].
Conclusion
In all cases, proper preoperative evaluation, light general anesthesia, gentle probing, and staining the track with a dye are key to success. Our method provides an alternative to the conventional operative treatment for high anal fistulae. The results from loose Seton are safe and effective regardless of the type of anal fistula. This treatment for fistula-in-ano also has the advantage of being considerably cheaper than inpatient operative methods and may allow the patient to continue employment. In the future, comparative studies with conventional surgery are required to confirm its role in managing all anal fistulae.
Acknowledgments: None declared by the authors.
Ethical Permissions: The ethical permission was taken from the Baghdad Teaching Hospital.
Conflicts of Interests: None.
Authors’ Contribution: Khairi Hussein Kh (First Author), Main Researcher (40%); Hayyawy MR (Second Author), Methodologist (30%); Mohammud Habash M (Third Author), Assistant Researcher (30%)
Funding/Support: None declared by the authors.
A fistula is an aberrant passage connecting one internal cavity to another or outside world. It may or may not be lined by mucous membrane or epithelium. An infection of the anal glands that spread down the intersphincteric plane to develop a leaking perianal abscess causes nearly all anal fistulas. These abscesses can leak in any path and plane, resulting in various fistulae. [1]. The incidence rate is 8.6 cases per 100,000 people. Men had a ratio of 12.3 cases per 100,000 people. In women, there are 5.6 instances per 100,000 people. A male-to-female ratio of 1.8:1 exists. Patients are 38.3 years old on average [2]. According to the cryptoglandular concept, an infection begins to develop in the anal gland and spreadsto the muscle layers of the anal sphincters, causing an anorectal abscess. A granular, lined channel may be left behind after surgical or voluntary drainage in the perianal region, causing repeated problems. According to several studies, anorectal abscess leads to creating a fistula pathway in 7-40% of cases [3, 4]. Almost nothing has changed in understanding the illness process since this early phase. Parks improved the classification method that is still widely used today in 1976. Over the last 30 years, several researchers have reported innovative techniques and case studies to reduce the incidence rate and leakage consequences. Fistula-in-ano remains a challenging surgical illness over 2500 decades of practice [2]. Generally, Fistula-in-ano is caused in various cases such as previous anorectal abscess, trauma, Crohn’s disease, anal fissure, carcinoma, radiation therapy, actinomycosis, tuberculosis and chlamydial infections, etc. [5]. Seton serves two goals and identifies the amount of sphincter muscle involved visually. These are used to evacuate the fluid, encourage fibrosis, and cut through the fissure. Large silk sutures, silicone-based vascular markers, or rubber bands inserted through the fistula passage can all be used to make seton. In the surgery, sometimes, early and delayed postoperative complications can occur. The early postoperative complications can be bleeding, urinary retention, fecal impaction, Thrombosed hemorrhoids, etc. The delayed postoperative complications can be Incontinence (stool), anal stenosis, delayed wound healing and recurrence. With this background, the study aimed to evaluate the efficacy of loose seton use in managing high anal fistula. '
Materials and Methods
A prospective cohort study (n=68) for low and high anal fistula management was designed. Seton placement's high anal fistula management (n=26) was carried out in a Baghdad teaching hospital's surgical unit. Initially, around 68 patients were screened (ages range between 17-63 years, both gender). A questionnaire containing the history of pain, swelling, and spontaneous or planned surgical drainage of an anorectal abscess with duration was taken. A review of symptoms of abdominal pain, weight loss and change in bowel habits were noted. Past medical history of inflammatory bowel disease, diverticulitis, previous radiation therapy for prostate or rectal cancer, tuberculosis, steroid therapy, HIV infection and past surgical history for fistula in one was also recorded.
Diagnosis
The diagnosis was made in three ways, i.e., physical examination, use of proctoscopy and radiological examination. The details of each are given below.
Physical examination
The patient in the left lateral position examined the whole perineum for an external opening that looks like an open sinus or granular tissue rise. On digital rectal examination, uncontrolled secretion via the external orifice may be visible or easily interpretable. The anus and a digital rectal examination (DRE) by inserting a lubricated, gloved finger into the rectum are done. Underneath the skin, a fibrous tract or cord may be seen. It also aided us in identifying any remaining acute inflammation that had not been drained.
Proctoscopy
In some patients, an interior opening wasn't identified by palpation or bypassing the probe through it. And to determine whether the opening was in the anal canal or above the anorectal ring in the rectum. Besides this, Proctoscopy showed us the state of the rectal mucosa and helped decide if any other underlying factors like proctocolitis were present.
Radiological examination
When in doubt or if a track was expected to proceed to more than one orifice, i.e., if the path was considered bifurcate, radiological evaluation of the fistulous track following injection of Conery Dye proved beneficial. High anorectal fistulas or fistulas with one or more pathways and openings benefited from this. Full radiological investigation and Sigmoidoscopy undertook in a patient with a previous history of recurrence to exclude any rectal tumor or inflammatory bowel disease involving the rectum.
Classification of patients
From clinical and radiological examinations, patients were divided into two groups:
1) Group A (n=42): Patients with low fistula type were treated by fistulotomy.
2) Group B (n=26): Patient with high fistula, 23 patients with a single opening, and three patients with multiple opening high fistulae.
Only group B was considered for the operations—Seton treated all the patients with high fistula type.
Preoperative preparation and operative procedure
An enema should be used to empty the lower bowel about an hour before the operation. As a preventive precaution, bowel sterilization is not required.
The Seton was usually inserted at the procedures were performed in the operating room with brief general anesthesia. The patient was examined in the left lateral position. The pre-rectal examination would reveal the diagnosis, and the fistula tract was identified by probing with the metallic malleable probe. Incision of skin from external opening of the fistula to the anal verge, subcutaneous tissue, internal sphincter and superficial part of the external sphincter. Insertion of loose Seton. A non-absorbable suture (2 silk). A Seton was left loosely and kept in situ for three months.
Follow‐up parameters
In follow-up care, twice daily, Sits baths, analgesics, and stool bulking agents (e.g., bran, psyllium products) were used. Repeated examinations were carried out every four weeks interval. At each visit position of the Seton was assessed. Wound healing detection of any recurrence were also recorded.
Statistical analysis
The data were represented as the mean (percentage) of the patients. The data were subjected to statistical analysis using Graph Pad Instat (Version 3, GraphPad Software Inc., San Diego, CA, USA). Dunnett Multiple Comparison Test and one-way Analysis of Variance (ANOVA) were performed.
Findings
Out of 68 patients, 42 (61.8%) had a low fistula, and 26 (38.2) had a high fistula in this study. About 23 (33.8) with a single opening in the high fistula group, and 3 (4.4 %) patients had a high fistula with multiple openings. All patients with low types fistula (N=42) were treated by primary fistulotomy. All patients (n = 26) with high fistula treated by Seton. Sixty-eight patients were admitted with perianal fistula. Of these 68 patients, 51 were males, and 17 were females; the male to female ratio was 3:1. The incidence was low in both sexes below 20 years and after 50 years. Peak occurrence was noted between 20 to 50 years. Incidence according to age is shown in Table 1. The median age was 41 (range: 17-63).
Table 1) Distribution of patients, according to their age
Of these 68 patients, 51 were males, and 17 were females; the male to female ratio was 3:1. Out of these 26 patients, 23 were males, and 03 were
females; the male to female ratio was 7.7:1. The study parameters variables are depicted in Table 2.
Table 2) Study parameters variation

Twenty-six patients with a high type of fistula in ano treated with Seton. 34.6% of patients reported surgery history in the Seton treated group. The
distribution of patients treated with Seton (n=26) according to age is represented in Table 3.
Table 3) Distribution of patients treated with Seton (n=26) according to age
Minor incontinence was noted in two patients (7.7%). These patients lost control of flatus which persisted for four months. No fecal incontinence was noticed in any patient. In around 21 patients, high fistula-in-ano were successfully eliminated by Seton treatment alone (Successful rate=81%). Around 05 patients, high fistula-in-ano were failed to be treated by a Seton method (Failure rate=19%). Two-stage Seton (draining/fibrosing) methods.
Discussion
Fistula-in-ano is one of the commonly encountered surgical problems. It is believed to originate from an infection of the anal glands. The main management principle is drainage of infection aerated these patients and eradicating fistulous tract with preservation of sphincter function [6]. In high perianal fistulas, the typical laying-open approach may need the loss of part or all of the sphincter muscle, affecting continence. It is self-evident that the larger the degree of anal muscle division, the greater the degree of incontinence [7]. High complicated fistulas can be successfully treated using several seton techniques with just a small loss of continence [8-12]. Conventionally, the Seton is used to manage high or complicated anal fistula [12]. The function of the Seton is to provide drainage, induce chronic fibrosis, and cut the fistulous tract with preservation of the sphincter mechanism. Cutting Seton and two-staged fistulotomy are two common techniques that have been used [13]. The Seton is tightly knotted around the fistulous tract in the cutting Seton procedure. Pressure necrosis will progressively traverse the muscle, and fibrosis will fix and protect sphincter removal. The Seton is loosely knotted, and the fistulotomy is conducted as a following step in the two-staged fistulotomy. The Seton is a drainage system that also causes fibrosis. In our study, the silk suture was used as Seton. Hippocrates first described this method [14]. Stenos can be made of various materials, but the most frequent are suture, rubber, wire, and medicated thread (Kshaarasootra) [15]. The results of this study demonstrated FIA is affecting many age groups and the data showed the 31-40 years age groups and 41-50 years were higher than other age groups with (p <0.01), with male predominance (75%) seen in this series are similar to the Seow-Choen et al. [16] and, Mc-Courtney and Finlay [15] studies.
Out of 68 patients with anal fistulae, 42 (61.8%) had a low fistula, and all of these patients were successfully treated by a simple laying-open technique. Twenty-six (38.2%) patients had high fistulae. Our findings are in accordance with the previously published studies [17-20]. They reported that "Most perineum fistulae are of the lower variation, meaning that they open underneath the anorectal ring. They are treated successfully using a laying-open procedure that does not require division of the anal sphincter muscles and so does not provide a risk of severe incontinence" [17-20]. According to Marks and Ritchie [21], high and intricate fistulae are uncommon. Only phased surgeries can treat them, which enter into the anal canal at or above the anorectal ring. The most likely explanation of this high prevalence of high fistula-in-ano is insufficient care at peripheral hospitals. High anal fistulae are harder to diagnose as well as a treat. To treat these fistulae, various surgical
procedures have been documented [22-25]. Our study suggests that most anal fistula can be treated successfully with loose Seton (success rate 81%) alone without a second surgery. Most of our patients tolerated the procedure well and were satisfied with the treatment. McCourtney and Finlay [15] described in the study, which supports the 2-stage approach with a 0-nylon Seton. The study reported that the stone is removed once wound healing is complete without division of the remaining encircled deep external sphincter muscle. The researchers reported eradicating the fistula tract in 60-78% of cases.
In our study, recurrence rates (19%) was low, and the disruption is minor and short-lived. The outcomes are equivalent to those reported using more complicated procedures to treat these complex fistulas. Abbas et al. [5] found that the long-term outcome of endorectal advancement flap for complex anorectal fistulae, Accordance with standard fistulotomy, the observed rate of incidence is 0-18% and the rate of any stool incontinence is 3-7% while following seton use, the identified rate of incidence is 0-17%, and the rate of any stool incontinence is 0-17%, and just after mucous progression flap, the reported rate of incidence is 1-17%, and the rate of any stool incontinence is 6-8% [5].
Incontinence can make fistula surgery more difficult. Nobody in this trial suffered severe incontinence. In the present study, two patients (7.7%) developed flatus incontinence, and both of them with a previous history of Perineum fistula require many procedures. The damage was just temporary and did not last in any patients. Others have also reported some lack of continence and management of flatus following surgery [26, 27].
Patients who have had previous fistula surgery have a higher risk of developing postoperative incontinence [28]. There has been a link between the rising frequency of this issue and the increasing number of previous fistula procedures. Lower resting and squeeze pressures are more likely to trigger incontinence after surgery than normal pressures [29].
Conclusion
In all cases, proper preoperative evaluation, light general anesthesia, gentle probing, and staining the track with a dye are key to success. Our method provides an alternative to the conventional operative treatment for high anal fistulae. The results from loose Seton are safe and effective regardless of the type of anal fistula. This treatment for fistula-in-ano also has the advantage of being considerably cheaper than inpatient operative methods and may allow the patient to continue employment. In the future, comparative studies with conventional surgery are required to confirm its role in managing all anal fistulae.
Acknowledgments: None declared by the authors.
Ethical Permissions: The ethical permission was taken from the Baghdad Teaching Hospital.
Conflicts of Interests: None.
Authors’ Contribution: Khairi Hussein Kh (First Author), Main Researcher (40%); Hayyawy MR (Second Author), Methodologist (30%); Mohammud Habash M (Third Author), Assistant Researcher (30%)
Funding/Support: None declared by the authors.
Keywords:
References
1. Dutta, G, Bain J, Ray A, Dey S, Das N, Das B. Comparing Ksharasutra (Ayurvedic Seton) and open fistulotomy in the management of fistula-in-ano. J Natur Sci Biol Med. 2015;6:406-10. [Link] [DOI:10.4103/0976-9668.160022] [PMID] [PMCID]
2. Sainio P. Fistula-in-ano in a defined population. Incidence and epidemiological aspects. Ann Chir Gynaecol. 1984;73(4):219-24. [Link]
3. Hancock BD. ABC of colorectal diseases. Anal fissures and fistulas. BMJ. 1992;304(6831):904-7. [Link] [DOI:10.1136/bmj.304.6831.904] [PMID] [PMCID]
4. Mark H, Kilkenny J, Hyman N. Practice Parameters for treatment of Perianal abscess and fistula in ano. Dis Colon Rectum. 2006;49:371-6. [Link]
5. Abbas MA, Lemus-Rangel R, Hamadani A. Long-term outcome of endorectal advancement flap for complex anorectal fistulae. Am Surg. 2008;74(10):921-4. [Link] [DOI:10.1177/000313480807401008]
6. Carr S, Velasco AL. Fistula In Ano. Treasure Island (FL): Stat Pearls Publishing; 2021. [Link]
7. Vogel JD, Johnson EK, Morris AM, Paquette IM, Saclarides TJ, Feingold DL, et al. Clinical Practice Guideline for the Management of Anorectal Abscess, Fistula-in-Ano, and Rectovaginal Fistula. Dis Colon Rectum. 2016;59(12):1117-33. [Link] [DOI:10.1097/DCR.0000000000000733] [PMID]
8. Buchanan GN, Bartram CI, Phillips RK, Gould SW, Halligan S, Rockall TA, et al. Efficacy of fibrin sealant in the management of complex anal fistula: a prospective trial. Dis Colon Rectum. 2003;46(9):1167-74. [Link] [DOI:10.1007/s10350-004-6708-9] [PMID]
9. Kelly ME, Heneghan HM, McDermott FD, Nason GJ, Freeman C, Martin ST, et al. The role of loose seton in the management of anal fistula: a multicenter study of 200 patients. Tech Coloproctol. 2014;18(10):915-9. [Link] [DOI:10.1007/s10151-014-1186-0] [PMID]
10. Wang D, Yang G, Qiu J, Song Y, Wang L, Gao J, et al. Risk factors for anal fistula: a case-control study. Tech Coloproctol. 2014;18(7):635-9. [Link] [DOI:10.1007/s10151-013-1111-y] [PMID]
11. Stamos MJ, Snyder M, Robb BW, Ky A, Singer M, Stewart DB, et al. Prospective multicenter study of a synthetic bioabsorbable anal fistula plug to treat cryptoglandular transsphincteric anal fistulas. Dis Colon Rectum. 2015;58(3):344-51. [Link] [DOI:10.1097/DCR.0000000000000288] [PMID]
12. Akiba RT, Rodrigues FG, da Silva G. Management of Complex Perineal Fistula Disease. Clin Colon Rectal Surg. 2016;29(2):92-100. [Link] [DOI:10.1055/s-0036-1580631] [PMID] [PMCID]
13. Rosen L. Anorectal abscess-fistulae. Surg Clin North Am. 1994;74(6):1293-308. [Link] [DOI:10.1016/S0039-6109(16)46481-9]
14. Weisman RI, Orsay CP, Pearl RK, Abcarian H. The role of fistulography in fistula-in-ano. Report of five cases. Dis Colon Rectum. 1991;34(2):181-4. [Link] [DOI:10.1007/BF02049995] [PMID]
15. Mc-Courtney J.S and Finlay IG. Review seton in the surgical management of fistula in ano. Br J Surg. 1995;82:448-52. [Link] [DOI:10.1002/bjs.1800820406] [PMID]
16. Seow-Choen F, Nicholls RJ. Anal fistula. Br J Surg. 1992;79:197-205. [Link] [DOI:10.1002/bjs.1800790304] [PMID]
17. Vainlevsky CA, Gordon PH. Results of treatment of fistula-in-ano. Dis Colon Rectum. 1985;28:225-31. [Link] [DOI:10.1007/BF02554037] [PMID]
18. Shoulder PJ, Crimley RP, Keighley MRB, Alexander WJ. Fistula-in-ano is usually simple to treat surgically. Int J Colon Dis. 1986;1:113-5. [Link] [DOI:10.1007/BF01648418] [PMID]
19. Eu KW. Fistulotomy and marsupialization for simple fistula-in-ano. Singapore Med J. 1992;33(5):532. [Link]
20. Cintron JR, Park JJ, Orsy CP, Pearl RK, Nelson RL, Sone JH, et al. Repair of fistula-in-ano using fibrin adhesive glue; long-term follow-up. Dis Colon Rectum. 2000;43(7):944-50. [Link] [DOI:10.1007/BF02237355] [PMID]
21. Marks CG, Ritchie JK. Anal fistula at St. Marks's Hospital. Br J Surg. 1977:64:84-91. [Link] [DOI:10.1002/bjs.1800640203] [PMID]
22. Sahu M. A Manual on fistula in ano and ksharasutra therapy. Varanasi:National Resource Center on Ksharasutra Therapy; 2015. [Link]
23. Mashhour AN, Omar HS, Marzouk AS, Raslan MM, Farag A. Evaluation of the role of endoanal ultrasonography in preoperative assessment of perianal fistula. Egypt J Surg. 2015;34:122-6. [Link] [DOI:10.4103/1110-1121.155723]
24. Ramachandra ML, Garg M. A comparative study in the management of fistula in ano using various modalities. Int Surg J. 2018:5(6):2223-7. [Link] [DOI:10.18203/2349-2902.isj20182226]
25. Tripathi N, Chavan S, Bendre M, Sharma V. Comparative study of MRI fistulogram and X-ray fistulography with operative findings in fistula in ano. Int Surg J. 2019;6(5):1704-9. [Link] [DOI:10.18203/2349-2902.isj20191894]
26. Owen G, Keshava A, Stewart P, Patterson J, Chapuis P, Bokey E, et al. Plugs unplugged. Anal fistula plug: the Concord experience. ANZ J Surg. 2010;80:341-3. [Link] [DOI:10.1111/j.1445-2197.2010.05278.x] [PMID]
27. Abou-Zeid AA. Anal fistula: intraoperative difficulties and unexpected findings. World J Gastroenterol. 2011;17(28):3272-6. [Link] [DOI:10.3748/wjg.v17.i28.3272] [PMID] [PMCID]
28. Emile SH. Recurrent anal fistulas: When, why, and how to manage?. World J Clin Cases. 2020;8(9):1586-91. [Link] [DOI:10.12998/wjcc.v8.i9.1586] [PMID] [PMCID]
29. Bjørsum-Meyer T, Christensen P, Jakobsen MS, Baatrup G, Qvist N. Correlation of anorectal manometry measures to severity of fecal incontinence in patients with anorectal malformations - a cross-sectional study. Sci Rep;2020;10:601-6. [Link] [DOI:10.1038/s41598-020-62908-w] [PMID] [PMCID]