Volume 13, Issue 4 (2021)
Iran J War Public Health 2021, 13(4): 261-265 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2021/09/4 | Accepted: 2021/10/4 | Published: 2022/01/24
Received: 2021/09/4 | Accepted: 2021/10/4 | Published: 2022/01/24
How to cite this article
Al-Alosi B, Mohsin Hussein A, Jabber S. Improving the Level of Amputation of the Lower Extremity after Therapeutic Endovascular Intervention for Patients with Critical Limb Ischemia. Iran J War Public Health 2021; 13 (4) :261-265
URL: http://ijwph.ir/article-1-1031-en.html
URL: http://ijwph.ir/article-1-1031-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
1- College of Medicine, University of Anbar, Ramadi, Iraq
2- College of Medicine, University of Baghdad, Baghdad, Iraq
3- Department of Vascular Surgery, Ghazi Al-Harery Hospital for Medical Specialties, Baghdad, Iraq
2- College of Medicine, University of Baghdad, Baghdad, Iraq
3- Department of Vascular Surgery, Ghazi Al-Harery Hospital for Medical Specialties, Baghdad, Iraq
Full-Text (HTML) (469 Views)
Introduction
Amputation is a surgical procedure that aims at the total or partial removal of an extremity that, for some reason, could not be recovered, and its maintenance is an aggravation to the patient's tribulation. It aims to relieve physical and psychic suffering [1]. Amputations have indications in some situations of trauma, tumors, and certain categories of patients with the peripheral arterial disease where surgical therapy fails with tissue loss and/or infection [1, 2]. Major lower limb amputation is defined as below, though, or above the knee loss of an extremity. Minor lower extremity amputation refers to below the level of the ankle [2]. Approximately 100,000 major leg amputations are performed each year in the United States; about half are attributable to diabetes and peripheral arterial disease [3, 4]. Within the population of patients with peripheral arterial disease with the critical lower limb, the estimated prevalence of diabetes ranges from 27% to 76%. Concomitant diabetes and peripheral arterial disease carry an amputation risk that is four times greater than the recorded average [3].
Studies have shown that between 25% and 90% of amputations among the populations studied are concomitant with diabetes [4]. Attributable to the combination of peripheral neuropathy and infection derived from diabetes and altered arterial flow due to peripheral arterial disease. Diabetic ulcers, associated with motor, sensory, and autonomic neuropathy, resulting in foot deformities and deterioration in wound healing, are also an integral part of the risk of amputation in patients with diabetes. It is estimated that about 50% of patients with diabetic ulcers have a peripheral arterial disease simultaneously [1, 2, 5]. The second cause of major amputations in the lower limbs is trauma (about 20%). It occurs predominantly in males (around 75%) and is related to traffic accidents and gunshot wounds [2]. Diabetes mellitus stands out in Iraq and the world for its importance as a public health problem [4]. Its epidemiological impact is expressed in increased morbidity and mortality rates and inconsequent disability, e.g., blindness, diabetic retinopathy, end-stage renal failure, and lower extremity amputations [6]. The long duration of disease, prolonged hyperglycemia, dyslipidemia, smoking and drinking habits, the presence of neuropathy or peripheral vascular disease, and previous ulcerative lesions are some of the factors risked for Lower Extremity Amputation in people with diabetes mellitus [5, 6]. Diabetic patients may present with microcirculation and/or microcirculation involvement, clinically presenting with motor and sensory neuropathy and even ischemia [4]. In general, diabetes is responsible for an amputation every thirty seconds, and 50% of these patients will have an amputation above or below the knee. In the United States alone, it is estimated that 80,000 amputations occur annually, and in five years, 50% will require a second amputation, and 50% will die. The cause of death is mainly motivated by cardio or cerebrovascular events [7].
Modern surgical treatment methods and peripheral vascular intervention have provided different modalities of solutions for various vascular diseases. However, amputation of the limb is a final solution to cases where the limb is not salvageable. Lower limb amputation is performed to remove ischemic, infected, necrotizing tissue that cannot be removed locally, which is sometimes a life-saving procedure [8]. The Second Transatlantic Community Consensus Working Group (TASC II) documented significant amputations due to peripheral artery disease ranging from 12 to 50 per 100,000 people per year. The aging population is expected to increase by 50 percent over the next 15 years. Factors that predict the need for lower limb amputations in patients with limb disease include tissue loss, end-stage kidney disease, poor functional conditions, and diabetes. Diabetic amputees are likely to be severely disabled, experience their initial amputation at a younger age, progress to high-level amputations, and die at a younger age than patients without diabetes [9]. Critical lower limb ischemia is a condition that poses a threat to limb viability and should be promptly treated to avoid further amputation. The ideal treatment for Critical lower limb ischemia is revascularization. The higher amputations of the lower limbs have a relevant socioeconomic impact such as loss of work capacity, socialization, and quality of life, associated with significant morbidity and mortality rates. As an aggravating factor in traumatic causes, we greatly involve economically active adults and young people, further worsening the social impact. Therefore, with its positive results, peripheral vascular intervention is an excellent solution to reduce the level of amputation [10]. Peripheral endovascular intervention should be deliberate as an alternative to primary amputation, particularly patients with Critical lower limb ischemia who are poor candidates for conventional surgical bypass [11].
This study aimed to evaluate the impact of revascularization of the lower limb with critical ischemia by peripheral angioplasty on improving the outcome in lowering the level of amputation to the stage that helps improve the patient's life and adjusting of the prosthesis.
Materials and Methods
This experimental study considered cases of patients diagnosed with lower limb ischemia who majorly were diabetic submitted to a consultation clinic in Al-Shaheed Ghazzi Al-Hariri Hospital for Surgical Specialties in Baghdad, Iraq, from October 2019 to October 2020. The cases (N=116) in this study were selected after the clinical examination, color Doppler and CT angiography. Through the results of those examinations, patients were selected for the intervention. The case data included patients diagnosed with critical limb ischemia and scheduled to undergo lower limb major amputation after suffering from arterial insufficiency. Controls were patients with lower limb ischemia, which was delayed or not submitted for intervention. The number of cases was determined randomly according to inclusion criteria. Inclusion criteria were patients of any age or sex who suffered lower limb ischemia where amputation of different levels was indicated for them, followed by pre-and post-endovascular intervention. Individuals were excluded when patients were beyond the level of intervention or those with poor compliance and those whose medical records were insufficiently filled out or missed follow-up. Because they are confounding factors, gender, age, and duration of the diagnosis of diabetes were considered for pairing.
The unfair variables were Socio-demographic characteristics (naturalness, schooling, color, occupation) and Lifestyle habits (smoking and drinking, alcoholic beverages in the present or past, quantity and duration). A protocol was drawn up (form for the collection of data) with personal information: name, gender, age, and birth date, factors related to amputation such as vascular reason, amputation level, blood glucose level, and the number of amputations. As for the amputation level, it was divided into proximal (or trans-femoral) and distal (including leg, foot, or toe(s)) to facilitate comparison with data existing in the literature.
The Chi-Square and Fisher's exact tests were used in SPSS 25 software to calculate the OR (odds ratio) and 95% Cis (confidence intervals) to determine the association between level of amputation with peripheral arterial intervention results.
Findings
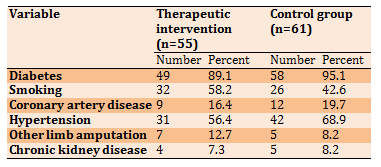
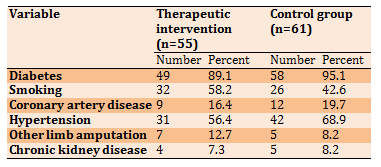
The total number of patients included in this study was 116 who have indications for above-knee amputation, 90 men (77.6%) and 26 women (22.4%). Fifty-five were amputated after performing a peripheral intervention with no restrictions on their age or gender. These patients had decided to amputate them before the therapeutic intervention but at a higher level. Of the 55 patients, 38 were males, and 17 were females, including between 31 and 83 years old. On the other hand, 61 patients were amputated due to arterial insufficiency, and it was not possible to perform a therapeutic intervention for them for various reasons.52 were males, and 9 were females. The mean age was 63.4±9.7 and 61.2±11.7 years in peripheral and without peripheral groups, respectively. Diabetes was the commonest risk factor found in 107 (92.24%) of patients that were followed by smoking (Table 1).
Table 1) Results of demographic and clinical characteristics of the study population
The high levels of amputation were for the control group who did not have a therapeutic intervention (Table 2). Most of them had amputations above the knee (86.9%).
Table 2) The level of amputation in both groups (N=116)

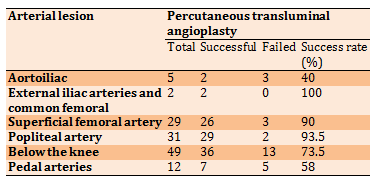
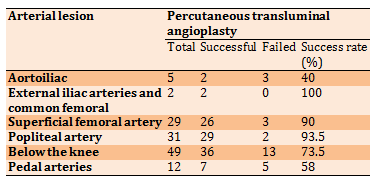
Most of the arterial occlusions of the lower extremities were below the knee; this included tibial arteries, posterior tibial arteries, and peroneal artery stenosis, followed by the popliteal artery in sequence. In contrast, there was a significant number of superficial femoral artery occlusions. The most successful result was obtained from common femoral and external iliac artery intervention (2 out of 2 100%). While below the knee intervention gave the worst result as 36 out of 49 interventions were failed. The superficial femoral artery, popliteal artery, and below-the-knee arterial lesions were the most common among the second group, and above-knee amputations were the most frequent (Table 3).
Table 3) Type of lesion in both groups and the result of the intervention
A case in which a peripheral intervention was performed for a leg that was subject to amputation above the knee due to multiple arterial critical lesions. The figure shows the improvement of the condition after treatment and the change of the amputation level to a level lower than scheduled (Figure 1).

Figure 1) How the lower limbs looked after the peripheral therapeutic intervention and the minor amputation of the foot
Discussion
Several variables are involved in the rise of arterial insufficiency in the lower extremities, and diabetes may be considered the most important. Not forgetting the role of other factors such as smoking and dyslipidemia, but to a lesser extent [12]. The prevalence of major amputation in patients with diabetes mellitus is also higher than in nondiabetics, with rates ranging from 5 to 15 times greater in some studies [13, 14]. In a Medicare population relative to nondiabetic patients, the relative risk for lower extremity amputation was 12.7 in diabetic patients [15]. The amputation of the lower limbs is largely reflected in patients' health, social, and economic status [16]. The post lower extremity amputation survivors have a significantly reduced quality of life and higher risk of depression related to impaired psychosocial functioning [17].
Lower extremity amputation is associated with huge morbidity and mortality [16]. Low and middle-income countries are currently at the greatest risk of diabetes-related complications and deaths [18]. Therefore, in this study, we sought to know the role of the peripheral intervention as a way of revascularization in improving the level of amputation for patients for whom amputation was decided before the peripheral intervention from the main level to a minor level. Most of those included in this study were middle-aged men. This is consistent with the fact that arterial insufficiency is more common in men than in women and that increasing age is a risk factor for its occurrence. The comorbidities associated with peripheral arterial insufficiency were not different from what was mentioned in many previous studies, where it was topped by diabetes and then followed by smoking and hypertension, and others [19-21].
Amputation above the knee was scheduled for all patients in this study. However, after the peripheral intervention and its success in the first group, the results changed and the amputation transformed from major to minor lower limb amputation, where most of the amputation in the first group was trans-metatarsal and in the second group was above the knee. The result was significant for all amputation levels when compared between the two groups. This is due to the improvement in blood flow to the lower extremities after the peripheral intervention. The superficial femoral and popliteal arteries are most frequently affected by atherosclerosis; the pain of intermittent claudication is most commonly localized to the calf [22]. While most of the therapeutic intervention in our study was for the arteries below the knee, followed by superficial femoral and popliteal arteries. Although the total number of the latter two exceeds the first, the high number of the first can be explained by its association with the high proportion of diabetics in the study, as they suffer from symptoms of diabetic foot, a syndrome associated with neuropathy and immunopathy in addition to vasculopathy [23, 24].
The results were not the best of the vascular intervention compared to that of other arteries, but they remained satisfactory. It is impossible to establish a relationship (without bias) between the level of amputation and the anatomical region of the diseased arteries submitted for intervention. This is because most patients suffer from arteriosclerosis in more than one artery, which makes judging the level of amputation or successful intervention illogical in linking the two variables. However, the lesions of the superficial femoral artery, popliteal arteries, and BTK arteries led to the largest amputations above the knee. The therapeutic intervention led to a change in the amputation level to a minor and better level. These results reflect the importance of these arteries in determining the amputation level. Arterial lesions with relatively low PTA success rates require strict pre-operative preparation and intensive post-operative care; these measures might improve the success rate. We support what some previous studies mentioned about the need to consider the peripheral endovascular intervention for any patient predisposed to amputation of his lower limbs after reviewing his condition.
Conclusion
The peripheral therapeutic intervention is not only useful in saving the lower limbs of patients with arterial insufficiency from inevitable amputation, but it is very important in improving the level of amputation in patients who are candidates for high levels of amputation by improving blood flow to the target organ, and this is reflected in the patient's health and social condition.
Acknowledgments: -
Ethical Permissions: This study does not have ethical code.
Conflicts of Interests: -
Authors’ Contribution: Al-Alosi B.M. (First Author), Introduction Writer/Discussion Writer (34%); Mohsin Hussein A. (Second Author), Assistant Researcher (33%); Jabber S.N. (Third Author), Assistant Researcher (33%).
Funding/Support: -
Amputation is a surgical procedure that aims at the total or partial removal of an extremity that, for some reason, could not be recovered, and its maintenance is an aggravation to the patient's tribulation. It aims to relieve physical and psychic suffering [1]. Amputations have indications in some situations of trauma, tumors, and certain categories of patients with the peripheral arterial disease where surgical therapy fails with tissue loss and/or infection [1, 2]. Major lower limb amputation is defined as below, though, or above the knee loss of an extremity. Minor lower extremity amputation refers to below the level of the ankle [2]. Approximately 100,000 major leg amputations are performed each year in the United States; about half are attributable to diabetes and peripheral arterial disease [3, 4]. Within the population of patients with peripheral arterial disease with the critical lower limb, the estimated prevalence of diabetes ranges from 27% to 76%. Concomitant diabetes and peripheral arterial disease carry an amputation risk that is four times greater than the recorded average [3].
Studies have shown that between 25% and 90% of amputations among the populations studied are concomitant with diabetes [4]. Attributable to the combination of peripheral neuropathy and infection derived from diabetes and altered arterial flow due to peripheral arterial disease. Diabetic ulcers, associated with motor, sensory, and autonomic neuropathy, resulting in foot deformities and deterioration in wound healing, are also an integral part of the risk of amputation in patients with diabetes. It is estimated that about 50% of patients with diabetic ulcers have a peripheral arterial disease simultaneously [1, 2, 5]. The second cause of major amputations in the lower limbs is trauma (about 20%). It occurs predominantly in males (around 75%) and is related to traffic accidents and gunshot wounds [2]. Diabetes mellitus stands out in Iraq and the world for its importance as a public health problem [4]. Its epidemiological impact is expressed in increased morbidity and mortality rates and inconsequent disability, e.g., blindness, diabetic retinopathy, end-stage renal failure, and lower extremity amputations [6]. The long duration of disease, prolonged hyperglycemia, dyslipidemia, smoking and drinking habits, the presence of neuropathy or peripheral vascular disease, and previous ulcerative lesions are some of the factors risked for Lower Extremity Amputation in people with diabetes mellitus [5, 6]. Diabetic patients may present with microcirculation and/or microcirculation involvement, clinically presenting with motor and sensory neuropathy and even ischemia [4]. In general, diabetes is responsible for an amputation every thirty seconds, and 50% of these patients will have an amputation above or below the knee. In the United States alone, it is estimated that 80,000 amputations occur annually, and in five years, 50% will require a second amputation, and 50% will die. The cause of death is mainly motivated by cardio or cerebrovascular events [7].
Modern surgical treatment methods and peripheral vascular intervention have provided different modalities of solutions for various vascular diseases. However, amputation of the limb is a final solution to cases where the limb is not salvageable. Lower limb amputation is performed to remove ischemic, infected, necrotizing tissue that cannot be removed locally, which is sometimes a life-saving procedure [8]. The Second Transatlantic Community Consensus Working Group (TASC II) documented significant amputations due to peripheral artery disease ranging from 12 to 50 per 100,000 people per year. The aging population is expected to increase by 50 percent over the next 15 years. Factors that predict the need for lower limb amputations in patients with limb disease include tissue loss, end-stage kidney disease, poor functional conditions, and diabetes. Diabetic amputees are likely to be severely disabled, experience their initial amputation at a younger age, progress to high-level amputations, and die at a younger age than patients without diabetes [9]. Critical lower limb ischemia is a condition that poses a threat to limb viability and should be promptly treated to avoid further amputation. The ideal treatment for Critical lower limb ischemia is revascularization. The higher amputations of the lower limbs have a relevant socioeconomic impact such as loss of work capacity, socialization, and quality of life, associated with significant morbidity and mortality rates. As an aggravating factor in traumatic causes, we greatly involve economically active adults and young people, further worsening the social impact. Therefore, with its positive results, peripheral vascular intervention is an excellent solution to reduce the level of amputation [10]. Peripheral endovascular intervention should be deliberate as an alternative to primary amputation, particularly patients with Critical lower limb ischemia who are poor candidates for conventional surgical bypass [11].
This study aimed to evaluate the impact of revascularization of the lower limb with critical ischemia by peripheral angioplasty on improving the outcome in lowering the level of amputation to the stage that helps improve the patient's life and adjusting of the prosthesis.
Materials and Methods
This experimental study considered cases of patients diagnosed with lower limb ischemia who majorly were diabetic submitted to a consultation clinic in Al-Shaheed Ghazzi Al-Hariri Hospital for Surgical Specialties in Baghdad, Iraq, from October 2019 to October 2020. The cases (N=116) in this study were selected after the clinical examination, color Doppler and CT angiography. Through the results of those examinations, patients were selected for the intervention. The case data included patients diagnosed with critical limb ischemia and scheduled to undergo lower limb major amputation after suffering from arterial insufficiency. Controls were patients with lower limb ischemia, which was delayed or not submitted for intervention. The number of cases was determined randomly according to inclusion criteria. Inclusion criteria were patients of any age or sex who suffered lower limb ischemia where amputation of different levels was indicated for them, followed by pre-and post-endovascular intervention. Individuals were excluded when patients were beyond the level of intervention or those with poor compliance and those whose medical records were insufficiently filled out or missed follow-up. Because they are confounding factors, gender, age, and duration of the diagnosis of diabetes were considered for pairing.
The unfair variables were Socio-demographic characteristics (naturalness, schooling, color, occupation) and Lifestyle habits (smoking and drinking, alcoholic beverages in the present or past, quantity and duration). A protocol was drawn up (form for the collection of data) with personal information: name, gender, age, and birth date, factors related to amputation such as vascular reason, amputation level, blood glucose level, and the number of amputations. As for the amputation level, it was divided into proximal (or trans-femoral) and distal (including leg, foot, or toe(s)) to facilitate comparison with data existing in the literature.
The Chi-Square and Fisher's exact tests were used in SPSS 25 software to calculate the OR (odds ratio) and 95% Cis (confidence intervals) to determine the association between level of amputation with peripheral arterial intervention results.
Findings
The total number of patients included in this study was 116 who have indications for above-knee amputation, 90 men (77.6%) and 26 women (22.4%). Fifty-five were amputated after performing a peripheral intervention with no restrictions on their age or gender. These patients had decided to amputate them before the therapeutic intervention but at a higher level. Of the 55 patients, 38 were males, and 17 were females, including between 31 and 83 years old. On the other hand, 61 patients were amputated due to arterial insufficiency, and it was not possible to perform a therapeutic intervention for them for various reasons.52 were males, and 9 were females. The mean age was 63.4±9.7 and 61.2±11.7 years in peripheral and without peripheral groups, respectively. Diabetes was the commonest risk factor found in 107 (92.24%) of patients that were followed by smoking (Table 1).
Table 1) Results of demographic and clinical characteristics of the study population
The high levels of amputation were for the control group who did not have a therapeutic intervention (Table 2). Most of them had amputations above the knee (86.9%).
Table 2) The level of amputation in both groups (N=116)

Most of the arterial occlusions of the lower extremities were below the knee; this included tibial arteries, posterior tibial arteries, and peroneal artery stenosis, followed by the popliteal artery in sequence. In contrast, there was a significant number of superficial femoral artery occlusions. The most successful result was obtained from common femoral and external iliac artery intervention (2 out of 2 100%). While below the knee intervention gave the worst result as 36 out of 49 interventions were failed. The superficial femoral artery, popliteal artery, and below-the-knee arterial lesions were the most common among the second group, and above-knee amputations were the most frequent (Table 3).
Table 3) Type of lesion in both groups and the result of the intervention
A case in which a peripheral intervention was performed for a leg that was subject to amputation above the knee due to multiple arterial critical lesions. The figure shows the improvement of the condition after treatment and the change of the amputation level to a level lower than scheduled (Figure 1).

Figure 1) How the lower limbs looked after the peripheral therapeutic intervention and the minor amputation of the foot
Discussion
Several variables are involved in the rise of arterial insufficiency in the lower extremities, and diabetes may be considered the most important. Not forgetting the role of other factors such as smoking and dyslipidemia, but to a lesser extent [12]. The prevalence of major amputation in patients with diabetes mellitus is also higher than in nondiabetics, with rates ranging from 5 to 15 times greater in some studies [13, 14]. In a Medicare population relative to nondiabetic patients, the relative risk for lower extremity amputation was 12.7 in diabetic patients [15]. The amputation of the lower limbs is largely reflected in patients' health, social, and economic status [16]. The post lower extremity amputation survivors have a significantly reduced quality of life and higher risk of depression related to impaired psychosocial functioning [17].
Lower extremity amputation is associated with huge morbidity and mortality [16]. Low and middle-income countries are currently at the greatest risk of diabetes-related complications and deaths [18]. Therefore, in this study, we sought to know the role of the peripheral intervention as a way of revascularization in improving the level of amputation for patients for whom amputation was decided before the peripheral intervention from the main level to a minor level. Most of those included in this study were middle-aged men. This is consistent with the fact that arterial insufficiency is more common in men than in women and that increasing age is a risk factor for its occurrence. The comorbidities associated with peripheral arterial insufficiency were not different from what was mentioned in many previous studies, where it was topped by diabetes and then followed by smoking and hypertension, and others [19-21].
Amputation above the knee was scheduled for all patients in this study. However, after the peripheral intervention and its success in the first group, the results changed and the amputation transformed from major to minor lower limb amputation, where most of the amputation in the first group was trans-metatarsal and in the second group was above the knee. The result was significant for all amputation levels when compared between the two groups. This is due to the improvement in blood flow to the lower extremities after the peripheral intervention. The superficial femoral and popliteal arteries are most frequently affected by atherosclerosis; the pain of intermittent claudication is most commonly localized to the calf [22]. While most of the therapeutic intervention in our study was for the arteries below the knee, followed by superficial femoral and popliteal arteries. Although the total number of the latter two exceeds the first, the high number of the first can be explained by its association with the high proportion of diabetics in the study, as they suffer from symptoms of diabetic foot, a syndrome associated with neuropathy and immunopathy in addition to vasculopathy [23, 24].
The results were not the best of the vascular intervention compared to that of other arteries, but they remained satisfactory. It is impossible to establish a relationship (without bias) between the level of amputation and the anatomical region of the diseased arteries submitted for intervention. This is because most patients suffer from arteriosclerosis in more than one artery, which makes judging the level of amputation or successful intervention illogical in linking the two variables. However, the lesions of the superficial femoral artery, popliteal arteries, and BTK arteries led to the largest amputations above the knee. The therapeutic intervention led to a change in the amputation level to a minor and better level. These results reflect the importance of these arteries in determining the amputation level. Arterial lesions with relatively low PTA success rates require strict pre-operative preparation and intensive post-operative care; these measures might improve the success rate. We support what some previous studies mentioned about the need to consider the peripheral endovascular intervention for any patient predisposed to amputation of his lower limbs after reviewing his condition.
Conclusion
The peripheral therapeutic intervention is not only useful in saving the lower limbs of patients with arterial insufficiency from inevitable amputation, but it is very important in improving the level of amputation in patients who are candidates for high levels of amputation by improving blood flow to the target organ, and this is reflected in the patient's health and social condition.
Acknowledgments: -
Ethical Permissions: This study does not have ethical code.
Conflicts of Interests: -
Authors’ Contribution: Al-Alosi B.M. (First Author), Introduction Writer/Discussion Writer (34%); Mohsin Hussein A. (Second Author), Assistant Researcher (33%); Jabber S.N. (Third Author), Assistant Researcher (33%).
Funding/Support: -
Keywords:
References
1. Alothman S, Alenazi A, Waitman LR, LeMaster J, Kluding P. Neuropathy and other risk factors for lower extremity amputation in people with diabetes using a clinical data repository system. J Allied Health. 2018;47(3):217-21. [Link]
2. Moxey PW, Gogalniceanu P, Hinchliffe RJ, Loftus IM, Jones KJ, Thompson MM, et al. Lower extremity amputations--a review of global variability in incidence. Diabet Med. 2011;28(10):1144-53. [Link] [DOI:10.1111/j.1464-5491.2011.03279.x] [PMID]
3. Potier L, Roussel R, Marre M, Bjornstad P, Cherney DZ, El Boustany R, et al. Plasma Copeptin and risk of lower-extremity amputation in type 1 and type 2 diabetes. Diabetes Care. 2019;42(12):2290-7. [Link] [DOI:10.2337/dc19-1062] [PMID] [PMCID]
4. Gamba MA, Gotlieb SLD, Pimentel Bergamaschi D, Vianna LAC. Lower extremity amputations in diabetic patients: A case-control study. Revista de Saude Publica. 2004;38:399-404. [Portuguese] [Link] [DOI:10.1590/S0034-89102004000300010] [PMID]
5. Swedish Council on Health Technology Assessment. Peripheral Arterial Disease - Diagnosis and Treatment: A Systematic Review [Internet]. Stockholm: Swedish Council on Health Technology Assessment (SBU); 2008 Nov. SBU Yellow Report No. 187. [Link]
6. Abusaib M, Ahmed M, Nwayyir HA, Alidrisi HA, Al-Abbood M, Al-Bayati A, et al. Iraqi experts consensus on the management of type 2 diabetes/prediabetes in adults. Clin Med Insights Endocrinol Diabetes. 2020;13. [Link] [DOI:10.1177/1179551420942232] [PMID] [PMCID]
7. Barnes JA, Eid MA, Creager MA, Goodney PP. Epidemiology and risk of amputation in patients with diabetes mellitus and peripheral artery disease. Arterioscler Thromb Vasc Biol. 2020;40(8):1808-17. [Link] [DOI:10.1161/ATVBAHA.120.314595] [PMID] [PMCID]
8. Newhall K, Spangler E, Dzebisashvili N, Goodman DC, Goodney P. Amputation rates for patients with diabetes and peripheral arterial disease: the effects of race and region. Ann Vasc Surg. 2016;30:292-8.e1. [Link] [DOI:10.1016/j.avsg.2015.07.040] [PMID] [PMCID]
9. Sidawy AN, Perler BA. Rutherford's vascular surgery and endovascular therapy. Philadelphia: Elsevier; 2019. [Link]
10. Swaminathan A, Vemulapalli S, Patel MR, Jones WS. Lower extremity amputation in peripheral artery disease: improving patient outcomes. Vasc Health Risk Manag. 2014;10:417-24. [Link] [DOI:10.2147/VHRM.S50588] [PMID] [PMCID]
11. Tefera G, Hoch J, Turnipseed WD. Limb-salvage angioplasty in vascular surgery practice. J Vasc Surg. 2005;41(6):988-93. [Link] [DOI:10.1016/j.jvs.2005.03.018] [PMID]
12. Allie DE, Hebert CJ, Lirtzman MD, Wyatt CH, Keller VA, Khan MH, et al. Critical limb ischemia: a global epidemic.A critical analysis of current treatment unmasks the clinical and economic costs of CLI. EuroIntervention. 2005;1(1):75-84. [Link]
13. American Diabetes Association. Peripheral arterial disease in people with diabetes. Diabetes Care. 2003;26(12):3333-41. [Link] [DOI:10.2337/diacare.26.12.3333] [PMID]
14. Jude EB, Oyibo SO, Chalmers N, Boulton AJ. Peripheral arterial disease in diabetic and nondiabetic patients: a comparison of severity and outcome. Diabetes Care. 2001;24(8):1433-7. [Link] [DOI:10.2337/diacare.24.8.1433] [PMID]
15. Beckman JA, Creager MA, Libby P. Diabetes and atherosclerosis: epidemiology, pathophysiology, and management. JAMA. 2002;287(19):2570-81. [Link] [DOI:10.1001/jama.287.19.2570] [PMID]
16. Ugwu E, Adeleye O, Gezawa I, Okpe I, Enamino M, Ezeani I. Predictors of lower extremity amputation in patients with diabetic foot ulcer: findings from MEDFUN, a multi-center observational study. J Foot Ankle Res. 2019;12:34. [Link] [DOI:10.1186/s13047-019-0345-y] [PMID] [PMCID]
17. Preedy VR. Handbook of disease burdens and quality of life measures. New York: Springer; 2012. pp. 3785-96. [Link]
18. Uloko AE, Musa BM, Ramalan MA, Gezawa ID, Puepet FH, Uloko AT, et al. Prevalence and risk factors for diabetes mellitus in Nigeria: a systematic review and meta-analysis. Diabetes Ther. 2018;9(3):1307-16. [Link] [DOI:10.1007/s13300-018-0441-1] [PMID] [PMCID]
19. American Diabetes Association. Standards of medical care in diabetes--2013. Diabetes Care. 2013;36 (Suppl 1):S11-66. [Link] [DOI:10.2337/dc13-S011] [PMID] [PMCID]
20. Barn R, Waaijman R, Nollet F, Woodburn J, Bus SA. Predictors of barefoot plantar pressure during walking in patients with diabetes, peripheral neuropathy and a history of ulceration. PLoS One. 2015;10(2):e0117443. [Link] [DOI:10.1371/journal.pone.0117443] [PMID] [PMCID]
21. Tessier D, Avila-Funes JA, Aguilar-Navarro S. Diabetes and changes in functional status of the elderly: A reality?. Revista de investigacion clinica; organo del Hospital de Enfermedades de la Nutricion. 2010;62(4):318-22. [Spanish] [Link]
22. Aronow WS. Peripheral arterial disease of the lower extremities. Arch Med Sci. 2012;8(2):375-88. [Link] [DOI:10.5114/aoms.2012.28568] [PMID] [PMCID]
23. Thiruvoipati T, Kielhorn CE, Armstrong EJ. Peripheral artery disease in patients with diabetes: Epidemiology, mechanisms, and outcomes. World J Diabetes. 2015;6(7):961-9. [Link] [DOI:10.4239/wjd.v6.i7.961] [PMID] [PMCID]
24. Kim PJ, Steinberg JS. Complications of the diabetic foot. Endocrinol Metab Clin North Am. 2013;42(4):833-47. [Link] [DOI:10.1016/j.ecl.2013.08.002] [PMID]