Volume 15, Issue 1 (2023)
Iran J War Public Health 2023, 15(1): 17-26 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2022/09/4 | Accepted: 2023/01/10 | Published: 2023/01/30
Received: 2022/09/4 | Accepted: 2023/01/10 | Published: 2023/01/30
How to cite this article
Seddighmokhtari N, Gheitasi M, Miri H, Bayattork M. Effect of an 8-Weeks of Comprehensive Corrective Protocol on Postural control, low Back Pain, Gait Speed and Quality of Life on Unilateral Transtibial Amputees. Iran J War Public Health 2023; 15 (1) :17-26
URL: http://ijwph.ir/article-1-1231-en.html
URL: http://ijwph.ir/article-1-1231-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
1- Department of Sports Injury, Faculty of Physical Education and Sport Sciences, Raja University, Qazvin, Iran
2- Department of Health and Rehabilitation in Sport, Faculty of Sport Science and Health, University of Shahid Beheshti, Tehran, Iran
3- Department of Physical Education and Sports Sciences, Amirkabir University of Technology, Tehran, Iran
4- Sport Sciences and Physical Education Department, Faculty of Humanities Science, University of Hormozgan, Bandar Abbas, Iran
2- Department of Health and Rehabilitation in Sport, Faculty of Sport Science and Health, University of Shahid Beheshti, Tehran, Iran
3- Department of Physical Education and Sports Sciences, Amirkabir University of Technology, Tehran, Iran
4- Sport Sciences and Physical Education Department, Faculty of Humanities Science, University of Hormozgan, Bandar Abbas, Iran
Full-Text (HTML) (294 Views)
Introduction
Movement disabilities are the most prevalent disabilities, and amputation is one of the most common cases [1]. Amputation makes the person susceptible to postural deviation and compensatory movements, and it causes a decrease in function and abnormal adaptation in areas such as the spine and lower limbs. Asymmetric movements in the trunk, lumbar-pelvic joints, and thigh following amputation lead to muscle fatigue and stress on the skeletal-articular structures and ultimately lead to a change in the alignment of the spine and pelvis [2]. Also, the problems of balance, flexibility and peripheral neuropathy are other complications of amputation [3], and disturbance in balance control is one of the most common movement challenges [4, 5]. In an inappropriate physical condition due to amputation, body parts are far from the reference line, and many complications are created, such as pain, increase or decrease in the motion range of the joints, reduced flexibility in muscles and soft tissues, adhesion, and imbalance in muscles, biomechanical change of joints, reduction of physiological capacities, ligament laxity, change in surface sensations and proprioception, a disorder in the sequence of the pattern of using muscles to perform normal daily movements, and functional limitations by inducing movement and pattern position [6, 7]. Therefore, it is very important to pay attention to the movement pattern and perform corrective movements to reduce body deviation, and improve back pain and the quality of life of amputee people.
In examining and treating muscle imbalance syndromes, the more important cause of deviation position and hypertonicity of certain muscle groups is the reducing the threshold of irritability and hyperactivity, which causes stiffness and shortening of these muscles. Whereas hypotonicity and weakness of antagonist muscle groups, with a high excitability threshold which is often weak and inhibited, have a delay in activation [8]. The main aims of correctional exercises for amputated people are restoring the length of shortened contractile and non-contractile tissues, recovery of strength in weak and inhibited muscles, development of endurance and functional power in the muscles, and development of functional and motor power. In this regard, based on the extensive studies on sports and physical activity of amputees for 10 years in America, physical activities improve the condition of these people [6]. Physical activities often include flexibility exercises, muscle strengthening, cardiovascular exercises, balance, and gait [3, 9]. On the other hand, atrophy of the trunk muscles, postural deformities of the spine, and biomechanical changes of the joints cause decreased activity, muscle stiffness, fatigue, and pain, so low back pain is seen in 71% of lower limb amputees [10]. Godlwana et al. [11], Shin et al. [10], Wasser et al. [12], and Faraji et al. [8] showed that strengthening exercises in amputees with back pain reduce pain and increase the strength of back extensors. Godlwana et al. investigated the effect of 3 months of home exercise on lower limb amputees compared to the control group and reported the improvement in performance, mobility, and quality of life in these people [11]. Wasser et al. prescribed exercise interventions for unilateral amputees with low back pain and concluded that regular performance of these exercises reduced the intensity of chronic pain and improved the quality of life in transtibial amputees [12].
Walking speed has been studied in healthy subjects and subjects with transtibial amputation. A normal walking velocity has been reported to be 83m/min. In contrast, walking speed has been estimated at 45m/min for persons who had undergone transtibial amputation for vascular reasons and 36m/min for persons who had undergone transfemoral amputation for vascular reasons, at least 6 months after wearing a prosthesis [13].
Considering the significant population of amputees and the physical complications caused by amputation and musculoskeletal problems, body malalignment, and compensatory movements, as well as the limitations of recent studies background in investigating the role of a comprehensive correction protocol in the symmetry of spine and hip muscles, reducing low back pain, improving the postural control indicators of this group of people, and expanding the hypothesis of movement patterns and frontal plane deviations, this study aimed to investigate the effect of an 8-weeks of comprehensive corrective protocol on postural control, low back pain, gait speed and quality of life on unilateral transtibial amputees.
Materials and Methods
This is a Quasi-experimental study with a pre and post-test design through two training and control groups and is a randomized controlled clinical trial (RCT) due to the use of the intervention variable, the existence of the control group, and the random grouping of the subjects.
The statistical population included unilateral transtibial amputees, who were referred to the comprehensive rehabilitation center of Red Crescent in Tehran between 2019 and 2021. Sampling was conducted based on the inclusion and exclusion criteria. The sample size was determined to be at least 20 using G power software concerning the statistical test, the number of variables, test power, and effect size. The subjects were 23 patients were included if they were at least 18 years of age and transtibial amputees who were homogenized based on the cause of amputation, activity level, gender, pain level, and ability or inability to participate in training sessions and randomly assigned into two training and control groups. The subjects were selected by convincing and purposive sampling and classified into two groups of training (n=13; 8 men and 5 women) and control (n=10; 4 men and 6 women) by the random. The participants signed an informed consent form before the study.
Inclusion and exclusion criteria
Inclusion criteria were age over 18 years, back pain [12] within 30 days before starting the study, non-participation in treatment and correction programs parallel to this study, and no open wounds and infections in the amputated limb within the past few months, continuous use of prosthesis, having a functional level at k2 [14] or higher, and no other musculoskeletal diseases or disabilities in the upper limbs. The prosthetic walking potential of people with lower limb amputation was originally described by the Medicare Functional Classification Level. This classification system consists of five levels referred to as "K-levels". K-levels range from 0 to 4, where K0 refers to a person who does not have the ability or potential to use a prosthesis for transfers or walking, and K4 refers to a person with the ability or potential to exceed basic ambulation skills, exhibiting high impact, stress or energy levels. In summary, the median (IQR) gait speed for each K-level was as follows: K1=0.17 (0.15– 0.19) m/s, K2=0.38 (0.25–0.54) m/s, K3=0.63 (0.50– 0.71) m/s, and K4=1.06 (0.95–1.18) m/s [14].
Exclusion criteria were the subject's lack of cooperation with the researcher, suffering from mental problems and taking sedative drugs, the occurrence of any mental and physical disorder during corrective interventions, not participating in 2 consecutive sessions or 3 non-consecutive sessions, and not participating in the post-test [15].
Assessment of postural control indicators
Computerized Dynamic Posturography (CDP) was used to evaluate the effect of exercises on postural control indicators of amputee people and to measure balance error. The machine evaluated the balance state in six positions, including: 1) senses of vision, hearing, and proprioception, 2) removal of vision sense, 3) change of hearing sense, 4) proprioceptive change, 5) removal of visual sense and change of proprioception, and 6) change of hearing sense and proprioception (ICC=0.35-0.79) [16]. In the 3 first positions, the power plates were fixed, and in the last 3 modes, the power plates moved in anterior and posterior directions. In the first position, a person was placed in the system so that all sensory information involved in postural control was available. In the second position, the subject was tested with a blindfold (removal of visual system information). In the third position, the person's eyes were open, but the visual environment was dynamic, leading to the presentation of incorrect vision arrays. In the fourth position, the force planes were dynamic, and the information of proprioception was removed. In the fifth position, the eyes were closed with a blindfold, and proprioceptive information was removed by moving the force plate. The information on the vestibular system in the postural was controlled in this situation. In the sixth position, the visual sense, hearing available proprioception information were removed. The duration of each test mode was 20 seconds. Each mode was repeated 3 times. The rest time between each mode was 10 seconds. During the rest period, the next situation was following aimed to the subjects. No feedback should be provided to the subjects at all stages. Finally, all the subjects were tested 3 times in each situation. The average stability variables and center of gravity shift were used 3 times in the test. In each of the 6 positions, a range score of 0 to 100 was presented as an index of the individual's balance control (Figure 1) [16].

Figure 1) Computerized dynamic posturography
Assessment of back pain intensity
Back pain intensity was measured using a numerical pain rating scale and a visual analog scale. The visual analog scale is a 10 cm horizontal strip, in which one end is zero meaning no pain, and another is 10 meaning maximum pain. This scale is the most reliable pain grading system for comparison between different courses, and it is widely used in research related to pain, whose reliability (ICC=0.93-0.98) and validity were confirmed [17].
Assessment of quality of life
The comprehensive lower limb amputee socket survey (CLASS) (validity and reliability ranged from 0.73 to 0.97) [18] and Trinity Amputation and Prosthesis Experience Scales (TAPES; available in the attachments) (validity and reliability lower than 0.70) [19], were used to check the quality of life. CLASS questionnaire to check the satisfaction level with prosthetic socket fit included 4 positions of prosthesis stability, suspension, comfort, and appearance in sitting, standing, walking, and going up and down the stairs, which scored using a 5-point scale including totally disagree with score 1, disagree with score 2, agree with score 3, totally agree with score 4 and have no opinion with score 0. The total number of points divided by 60 was expressed as a percentage. The TAPES questionnaire also included scoring the items based on marking each of the 5 positions.
Assessment of gait speed
The 2-minute walk test (ICC=0.86–0.98) was used to determine the walking distance of amputees. By this, the subject covered a distance marked by the researcher for 2 minutes in a round trip mode. After the end of the time, the whole distance was obtained by multiplying the number of round trips and the route taken by the subjects [14, 20].
Comprehensive corrective protocol
The comprehensive corrective protocol included corrective exercises, optimal posture retraining patterns, mirror therapy, training optimal use of prosthesis along with adopting optimal posture, improving the balance of the physical structure, increasing efficiency, preventing and eliminating skeletal-muscular disorders and deviations, and correcting postural abnormalities. According to the specific problems and receiving a history of the physical condition of each subject, an individualized comprehensive correction program through a guidebook was used, including 8 weeks of exercises and training, ranging from easy levels with fewer exercises to advanced combined levels with more exercises and activities.
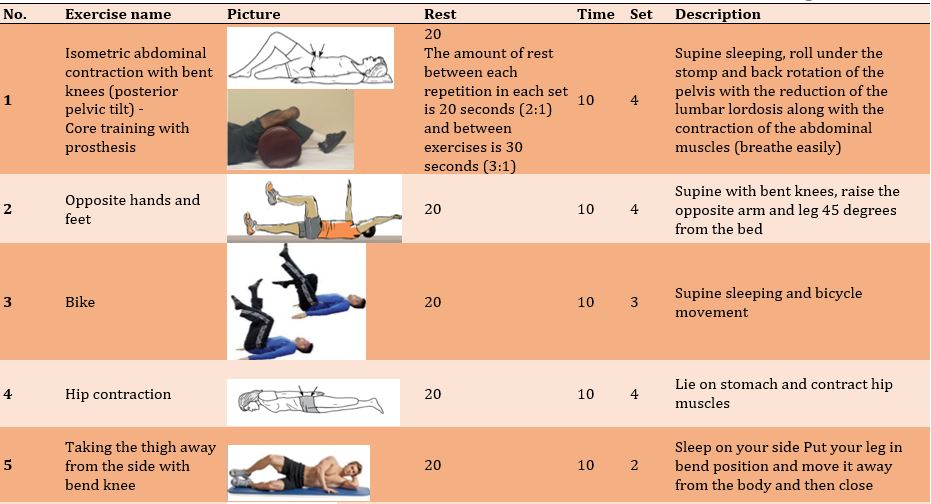
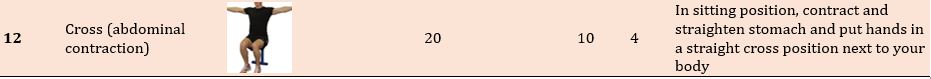
The exercises aimed to restore the length of shortened contractile and non-contractile tissues, recover strength in weak and inhibited muscles, development of endurance and functional power in the muscles and the central portion of the body, development of functional and motor power, improve balance and postural control, teaching optimal body positions, and correcting postural malalignments in the subjects. In addition to the individualization of the comprehensive protocol of exercises and training programs, principles of program development in each subject were accorded to the overload principle, the gradual progress of training intensity, the progress of the subject based on gender, amputation period, medical and sports records and self-report of the subject. At the beginning of the protocol, the subjects' exercise program was designed and implemented with a focus on the center body portion. Appropriate techniques and methods of training were used to release, stretch and restore the natural length of short and tight tissues and to improve the strength and endurance power of the pelvic-thigh muscles. The training program included 3 one-hour training sessions per week at home for eight weeks according to the program of the corrective exercises booklet after ensuring the correct training of the patient in the clinic. The researcher followed up the exercise process and completed the exercise session checklist for each subject. All the exercises were done slowly and without rushing and causing pain. There were 3 main stages of warming up, the main training protocol, and finally cooling down. Middle-body exercises were used for 5-10 minutes of warming up. In the main protocol, there are (1) release of the iliotibial band, tensorfasciata, and iliopsoas muscles, (2) stretching of short and tight tissues, (3) strengthening of weak and inhibited muscles, (4) balance and range of motion exercises and (5) coordination movements. And walking was done for a total of 30-45 minutes. At the end of the protocol, simple breathing and stretching exercises are used to cool down (Figure 2) [8, 15].
Statistical analysis
The information obtained from the measuring variables was analyzed using SPSS 23 software through descriptive and inferential statistics. Data normality was checked using the Shapiro-Wilk test. One-way Analysis of Covariance (ANCOVA) was used to examine the differences between studied groups in the post-test and pre-test. Also, paired t-test was used to check intra-group differences. Partial η2 was used to check the effect size of exercises.
Findings
Demographic information and duration of amputation and using the prosthesis in control and training groups are presented in Table 1.
There was no significant effect of the 8-week comprehensive corrective protocol on postural control in the first (p=0.810), second (p=0.092), and third modes (p=0.133) on unilateral lower limb amputees. However, there was a significant effect of an 8-week comprehensive corrective protocol on postural control in the fourth (p=0.042), fifth (p=0.003), sixth (p=0.021), and the total score of the balance of the subjects (p=0.004; Table 2).
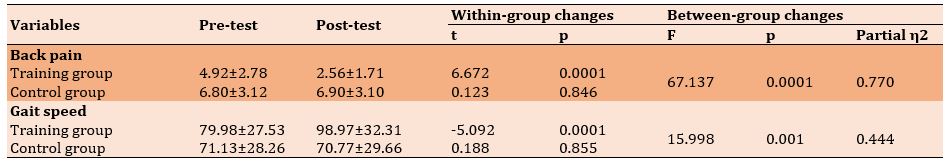
There was a significant difference between the training and control groups regarding back pain intensity in the post-test (p=0.0001). Also, a significant decrease in back pain intensity was observed in the training group at the post-test compared to the pre-test (p=0.0001). However, there was no significant difference in the control group in the post-test (p=0.846; Table 3).
A significant increase in gait speed was observed in the training group than in the control group at the post-test (p=0.001). Also, the gait speed in the training group increased significantly in the post-test than in the pre-test (p=0.0001). However, the result of the control group showed no significant difference in the post-test compared to the pre-test (p=0.885; Table 3).

Movement disabilities are the most prevalent disabilities, and amputation is one of the most common cases [1]. Amputation makes the person susceptible to postural deviation and compensatory movements, and it causes a decrease in function and abnormal adaptation in areas such as the spine and lower limbs. Asymmetric movements in the trunk, lumbar-pelvic joints, and thigh following amputation lead to muscle fatigue and stress on the skeletal-articular structures and ultimately lead to a change in the alignment of the spine and pelvis [2]. Also, the problems of balance, flexibility and peripheral neuropathy are other complications of amputation [3], and disturbance in balance control is one of the most common movement challenges [4, 5]. In an inappropriate physical condition due to amputation, body parts are far from the reference line, and many complications are created, such as pain, increase or decrease in the motion range of the joints, reduced flexibility in muscles and soft tissues, adhesion, and imbalance in muscles, biomechanical change of joints, reduction of physiological capacities, ligament laxity, change in surface sensations and proprioception, a disorder in the sequence of the pattern of using muscles to perform normal daily movements, and functional limitations by inducing movement and pattern position [6, 7]. Therefore, it is very important to pay attention to the movement pattern and perform corrective movements to reduce body deviation, and improve back pain and the quality of life of amputee people.
In examining and treating muscle imbalance syndromes, the more important cause of deviation position and hypertonicity of certain muscle groups is the reducing the threshold of irritability and hyperactivity, which causes stiffness and shortening of these muscles. Whereas hypotonicity and weakness of antagonist muscle groups, with a high excitability threshold which is often weak and inhibited, have a delay in activation [8]. The main aims of correctional exercises for amputated people are restoring the length of shortened contractile and non-contractile tissues, recovery of strength in weak and inhibited muscles, development of endurance and functional power in the muscles, and development of functional and motor power. In this regard, based on the extensive studies on sports and physical activity of amputees for 10 years in America, physical activities improve the condition of these people [6]. Physical activities often include flexibility exercises, muscle strengthening, cardiovascular exercises, balance, and gait [3, 9]. On the other hand, atrophy of the trunk muscles, postural deformities of the spine, and biomechanical changes of the joints cause decreased activity, muscle stiffness, fatigue, and pain, so low back pain is seen in 71% of lower limb amputees [10]. Godlwana et al. [11], Shin et al. [10], Wasser et al. [12], and Faraji et al. [8] showed that strengthening exercises in amputees with back pain reduce pain and increase the strength of back extensors. Godlwana et al. investigated the effect of 3 months of home exercise on lower limb amputees compared to the control group and reported the improvement in performance, mobility, and quality of life in these people [11]. Wasser et al. prescribed exercise interventions for unilateral amputees with low back pain and concluded that regular performance of these exercises reduced the intensity of chronic pain and improved the quality of life in transtibial amputees [12].
Walking speed has been studied in healthy subjects and subjects with transtibial amputation. A normal walking velocity has been reported to be 83m/min. In contrast, walking speed has been estimated at 45m/min for persons who had undergone transtibial amputation for vascular reasons and 36m/min for persons who had undergone transfemoral amputation for vascular reasons, at least 6 months after wearing a prosthesis [13].
Considering the significant population of amputees and the physical complications caused by amputation and musculoskeletal problems, body malalignment, and compensatory movements, as well as the limitations of recent studies background in investigating the role of a comprehensive correction protocol in the symmetry of spine and hip muscles, reducing low back pain, improving the postural control indicators of this group of people, and expanding the hypothesis of movement patterns and frontal plane deviations, this study aimed to investigate the effect of an 8-weeks of comprehensive corrective protocol on postural control, low back pain, gait speed and quality of life on unilateral transtibial amputees.
Materials and Methods
This is a Quasi-experimental study with a pre and post-test design through two training and control groups and is a randomized controlled clinical trial (RCT) due to the use of the intervention variable, the existence of the control group, and the random grouping of the subjects.
The statistical population included unilateral transtibial amputees, who were referred to the comprehensive rehabilitation center of Red Crescent in Tehran between 2019 and 2021. Sampling was conducted based on the inclusion and exclusion criteria. The sample size was determined to be at least 20 using G power software concerning the statistical test, the number of variables, test power, and effect size. The subjects were 23 patients were included if they were at least 18 years of age and transtibial amputees who were homogenized based on the cause of amputation, activity level, gender, pain level, and ability or inability to participate in training sessions and randomly assigned into two training and control groups. The subjects were selected by convincing and purposive sampling and classified into two groups of training (n=13; 8 men and 5 women) and control (n=10; 4 men and 6 women) by the random. The participants signed an informed consent form before the study.
Inclusion and exclusion criteria
Inclusion criteria were age over 18 years, back pain [12] within 30 days before starting the study, non-participation in treatment and correction programs parallel to this study, and no open wounds and infections in the amputated limb within the past few months, continuous use of prosthesis, having a functional level at k2 [14] or higher, and no other musculoskeletal diseases or disabilities in the upper limbs. The prosthetic walking potential of people with lower limb amputation was originally described by the Medicare Functional Classification Level. This classification system consists of five levels referred to as "K-levels". K-levels range from 0 to 4, where K0 refers to a person who does not have the ability or potential to use a prosthesis for transfers or walking, and K4 refers to a person with the ability or potential to exceed basic ambulation skills, exhibiting high impact, stress or energy levels. In summary, the median (IQR) gait speed for each K-level was as follows: K1=0.17 (0.15– 0.19) m/s, K2=0.38 (0.25–0.54) m/s, K3=0.63 (0.50– 0.71) m/s, and K4=1.06 (0.95–1.18) m/s [14].
Exclusion criteria were the subject's lack of cooperation with the researcher, suffering from mental problems and taking sedative drugs, the occurrence of any mental and physical disorder during corrective interventions, not participating in 2 consecutive sessions or 3 non-consecutive sessions, and not participating in the post-test [15].
Assessment of postural control indicators
Computerized Dynamic Posturography (CDP) was used to evaluate the effect of exercises on postural control indicators of amputee people and to measure balance error. The machine evaluated the balance state in six positions, including: 1) senses of vision, hearing, and proprioception, 2) removal of vision sense, 3) change of hearing sense, 4) proprioceptive change, 5) removal of visual sense and change of proprioception, and 6) change of hearing sense and proprioception (ICC=0.35-0.79) [16]. In the 3 first positions, the power plates were fixed, and in the last 3 modes, the power plates moved in anterior and posterior directions. In the first position, a person was placed in the system so that all sensory information involved in postural control was available. In the second position, the subject was tested with a blindfold (removal of visual system information). In the third position, the person's eyes were open, but the visual environment was dynamic, leading to the presentation of incorrect vision arrays. In the fourth position, the force planes were dynamic, and the information of proprioception was removed. In the fifth position, the eyes were closed with a blindfold, and proprioceptive information was removed by moving the force plate. The information on the vestibular system in the postural was controlled in this situation. In the sixth position, the visual sense, hearing available proprioception information were removed. The duration of each test mode was 20 seconds. Each mode was repeated 3 times. The rest time between each mode was 10 seconds. During the rest period, the next situation was following aimed to the subjects. No feedback should be provided to the subjects at all stages. Finally, all the subjects were tested 3 times in each situation. The average stability variables and center of gravity shift were used 3 times in the test. In each of the 6 positions, a range score of 0 to 100 was presented as an index of the individual's balance control (Figure 1) [16].

Figure 1) Computerized dynamic posturography
Assessment of back pain intensity
Back pain intensity was measured using a numerical pain rating scale and a visual analog scale. The visual analog scale is a 10 cm horizontal strip, in which one end is zero meaning no pain, and another is 10 meaning maximum pain. This scale is the most reliable pain grading system for comparison between different courses, and it is widely used in research related to pain, whose reliability (ICC=0.93-0.98) and validity were confirmed [17].
Assessment of quality of life
The comprehensive lower limb amputee socket survey (CLASS) (validity and reliability ranged from 0.73 to 0.97) [18] and Trinity Amputation and Prosthesis Experience Scales (TAPES; available in the attachments) (validity and reliability lower than 0.70) [19], were used to check the quality of life. CLASS questionnaire to check the satisfaction level with prosthetic socket fit included 4 positions of prosthesis stability, suspension, comfort, and appearance in sitting, standing, walking, and going up and down the stairs, which scored using a 5-point scale including totally disagree with score 1, disagree with score 2, agree with score 3, totally agree with score 4 and have no opinion with score 0. The total number of points divided by 60 was expressed as a percentage. The TAPES questionnaire also included scoring the items based on marking each of the 5 positions.
Assessment of gait speed
The 2-minute walk test (ICC=0.86–0.98) was used to determine the walking distance of amputees. By this, the subject covered a distance marked by the researcher for 2 minutes in a round trip mode. After the end of the time, the whole distance was obtained by multiplying the number of round trips and the route taken by the subjects [14, 20].
Comprehensive corrective protocol
The comprehensive corrective protocol included corrective exercises, optimal posture retraining patterns, mirror therapy, training optimal use of prosthesis along with adopting optimal posture, improving the balance of the physical structure, increasing efficiency, preventing and eliminating skeletal-muscular disorders and deviations, and correcting postural abnormalities. According to the specific problems and receiving a history of the physical condition of each subject, an individualized comprehensive correction program through a guidebook was used, including 8 weeks of exercises and training, ranging from easy levels with fewer exercises to advanced combined levels with more exercises and activities.
The exercises aimed to restore the length of shortened contractile and non-contractile tissues, recover strength in weak and inhibited muscles, development of endurance and functional power in the muscles and the central portion of the body, development of functional and motor power, improve balance and postural control, teaching optimal body positions, and correcting postural malalignments in the subjects. In addition to the individualization of the comprehensive protocol of exercises and training programs, principles of program development in each subject were accorded to the overload principle, the gradual progress of training intensity, the progress of the subject based on gender, amputation period, medical and sports records and self-report of the subject. At the beginning of the protocol, the subjects' exercise program was designed and implemented with a focus on the center body portion. Appropriate techniques and methods of training were used to release, stretch and restore the natural length of short and tight tissues and to improve the strength and endurance power of the pelvic-thigh muscles. The training program included 3 one-hour training sessions per week at home for eight weeks according to the program of the corrective exercises booklet after ensuring the correct training of the patient in the clinic. The researcher followed up the exercise process and completed the exercise session checklist for each subject. All the exercises were done slowly and without rushing and causing pain. There were 3 main stages of warming up, the main training protocol, and finally cooling down. Middle-body exercises were used for 5-10 minutes of warming up. In the main protocol, there are (1) release of the iliotibial band, tensorfasciata, and iliopsoas muscles, (2) stretching of short and tight tissues, (3) strengthening of weak and inhibited muscles, (4) balance and range of motion exercises and (5) coordination movements. And walking was done for a total of 30-45 minutes. At the end of the protocol, simple breathing and stretching exercises are used to cool down (Figure 2) [8, 15].
Statistical analysis
The information obtained from the measuring variables was analyzed using SPSS 23 software through descriptive and inferential statistics. Data normality was checked using the Shapiro-Wilk test. One-way Analysis of Covariance (ANCOVA) was used to examine the differences between studied groups in the post-test and pre-test. Also, paired t-test was used to check intra-group differences. Partial η2 was used to check the effect size of exercises.
Findings
Demographic information and duration of amputation and using the prosthesis in control and training groups are presented in Table 1.
There was no significant effect of the 8-week comprehensive corrective protocol on postural control in the first (p=0.810), second (p=0.092), and third modes (p=0.133) on unilateral lower limb amputees. However, there was a significant effect of an 8-week comprehensive corrective protocol on postural control in the fourth (p=0.042), fifth (p=0.003), sixth (p=0.021), and the total score of the balance of the subjects (p=0.004; Table 2).
There was a significant difference between the training and control groups regarding back pain intensity in the post-test (p=0.0001). Also, a significant decrease in back pain intensity was observed in the training group at the post-test compared to the pre-test (p=0.0001). However, there was no significant difference in the control group in the post-test (p=0.846; Table 3).
A significant increase in gait speed was observed in the training group than in the control group at the post-test (p=0.001). Also, the gait speed in the training group increased significantly in the post-test than in the pre-test (p=0.0001). However, the result of the control group showed no significant difference in the post-test compared to the pre-test (p=0.885; Table 3).
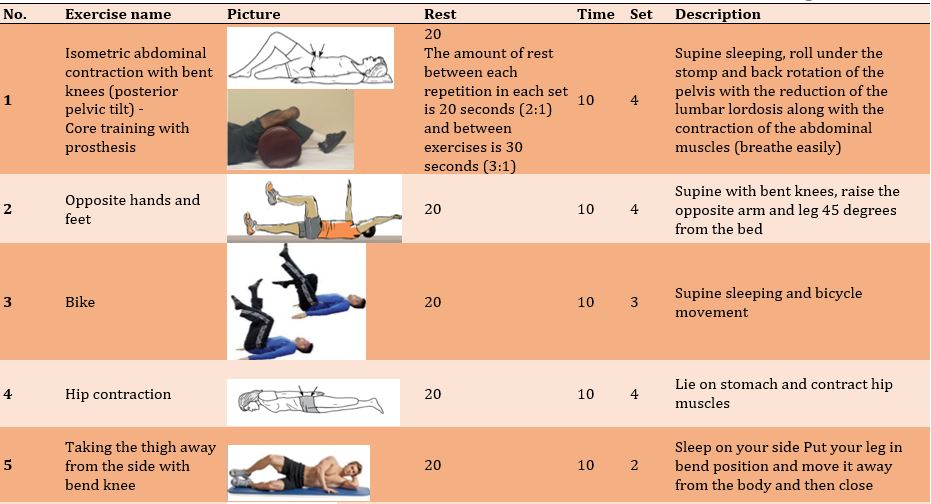

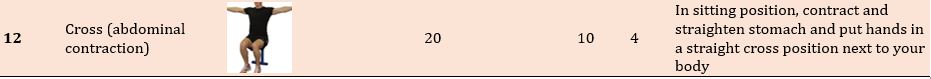
Figure 2) Exercise protocol
Table 1) Demographic information and duration of amputation and using the prosthesis in control (n=10) and training (n=13) groups

Table 2) Comparision of the mean scores of postural control in the pre-and post-test stages in the studied groups


Table 2) Comparision of the mean scores of postural control in the pre-and post-test stages in the studied groups

Table 3) Comparision of the mean scores of back pain and gait speed in the pre-and post-test stages in the studied groups
Considering the quality of life, including 10 items of quality of life and satisfaction with prosthesis function, the results showed the effect of 8 weeks of a comprehensive corrective protocol on the quality of life of unilateral lower limb amputees, and a significant difference was observed between the training and control groups in the post-test stage (p=0.0001; Table 4).
Table 4) Comparision of the mean scores of quality of life and satisfaction level with prosthetic socket fit in the pre-and post-test stages in the studied groups

Discussion
This study aimed to investigate the effect of an 8-week comprehensive rehabilitation protocol, including corrective exercises, correct posture training, mirror therapy, daily activities training, and use of prosthesis on indicators of postural control, back pain, quality of life, and gait speed in adults with unilateral lower limb amputation.
In this research, the postural control index was assessed in six positions separately. There was no significant difference between the existence of three senses of vision, vestibular and proprioceptive, removing vision, and vestibular sense change in the training group than the control group. Also no significant difference was observed in the training group after the post-test. The position 3 to 6 included proprioception change, vision removal and proprioception change, and vestibular and proprioception change. The results of investigating the 3-last positions showed a significant difference between the training and control groups; also, the post-test results showed a significant difference in the training group. The findings of this research on the effective role of corrective exercises in improving postural control and balance in lower limb amputees are accordant with the findings of Schafer et al. [9, 21], Mohamadtaghi et al. [22, 23], Damayanti Sethy et al. [24], Miller et al. [25], Devan et al. [2], and Moradi et al. [1]. Schafer et al., in a randomized controlled trial, looked for the role of a 12-week personal exercise program on the balance of lower limb amputees after home exercise sessions of the exercise group, including balance, endurance, strength, and flexibility exercises on balance scores. The exercise group significantly increased muscle symmetry and weight bearing while standing on an unstable surface without visual input and sensory feedback [21]. Mohamadtaghi et al., in another research entitled "effect of the selected balance program on postural control of amputees under the manipulation of visual, vestibular, and proprioceptive systems with 14 subjects in training and control groups", found that following a therapeutic exercise program was effective in improving balance and increasing stability. Probably, the reasons for effectiveness in the functional conditions of amputees were performing balance exercises, improving the muscle strength in the central portion of the body, improving the proprioceptive function of amputees, and increasing the control of posture in subjects. Postural control indicators in unilateral lower limb amputees changed because of muscle imbalance caused by excessive use of certain groups of muscles and inactivity and proper use of another group, and it inclines the patients towards performing compensatory movements and adopting compensatory postures such as bending to the prosthetic side and creating an unfavorable alignment in the person's posture as a compensatory strategy [22, 23]. One of the prevention and compensation strategies in the design and implementation of corrective protocols for improving postural control by affecting weight distribution between two organs is the proper use of the central muscles of the body and optimal use of the prosthesis during functional activities, which has an important and effective role in maintaining balance and postural control, especially during movement activities [24, 25]. Selective correction exercises, emphasizing the strength of the central portion of the body, improving power and endurance of pelvic-thigh muscles, improving balance and postural control in different situations during 8 weeks, aimed to improve the functional ability of people while using a prosthesis, gait and improving their quality of life [2, 26].
The reduction of back pain in the training group was another result of this research. Back pain is one of the secondary and undeniable conditions after amputation [12]. In this research, we tried to decrease back pain intensity in the subjects using emphasizing exercises in the center portion of the body especially pelvic and thigh muscles, increasing motor control, improving neuromuscular coordination, and improving the alignment of the pelvic and lumbar areas in the frontal and sagittal planes. Also, the findings of Shin et al. [10], Fatone et al. [26], and Faraji et al. [8] showed a decrease in the long-term risk of back pain using a change in the movement strategy of amputees [27]. Consistent with our findings, Shin et al. [10] in a study entitled "effects of lumbar strengthening exercise in lower-limb amputees with chronic back pain", emphasized strengthening exercises to reduce pain and increase the strength of back extensors by strengthening exercises and declared that following exercises prevents atrophy of trunk muscles and compression of joints and have an effect of 71% in reducing the back pain of amputees. It’s because of strengthening the muscles of the central portion of the body, strengthening atrophied muscles, and stretching weak muscles [7, 15]. Similar to our results, Faraji et al. [8], in a study entitled "the effect of 12-week corrective training on lumbar multifidus muscle asymmetry and pain intensity in veterans with one-sided below-knee amputation suffering from chronic back pain", mentioned the positive effect of 12 weeks corrective training on the decrease of back pain intensity whereas there was no effect on the multifidus muscle asymmetry in a maximum contraction of the muscle and muscular endurance. Therefore, this research aimed to design and implement a comprehensive corrective protocol to restore muscle balance, improve the levels of neuromuscular coordination and motor control, especially in the subject who used the prosthesis during daily life activities such as gait, and improve motor patterns and postural strategies in order to reduce back pain intensity in the subject.
There was a significant increase in the quality of life in the training group than in the control group after the post-test. The use of prostheses on amputees has a positive effect on their quality of life since the amputee does not enjoy the same conditions as healthy people, such as the use of stairs, vehicles, and the lack of urban furniture. Selected corrective exercises focus on strengthening weak and stretched muscles, restoring the length of muscles and shortened soft tissues, creating functional organ coordination, and acquiring the ability to perform efficient movements and improve the quality of life of amputees [28, 29].
Our results are consistent with the findings of Bouzas et al. [30], Wasser et al. [12], Miller et al. [25], Parker et al. [31], and MacKenzie et al. [32]. Bouzas et al. reviewed the effect of exercise on the physical performance of amputees and pointed out the role of combined positive, endurance, and functional exercises on respiratory stress, muscle fitness, and better performance in adults with unilateral lower limb amputation [30]. Wasser et al. investigated the exercise intervention for unilateral amputees with low back pain and concluded that stability exercises have a significant role in central body stability, lumbar strength, and dynamic stability, changing the musculoskeletal system, reducing pain, improving quality of life, and reducing injuries caused by the physical problems of amputees [12]. Miller et al., in a study entitled "the effect of a supervised community–based exercise program on balance, balance confidence, and gait in individuals with lower limb amputation", mentioned the positive effect of exercise and rehabilitation programs to maintain the ability and functional activities of amputees on improving their quality of life [25]. In the research by Parker et al., who examined the relationship between the motor ability of amputees, quality of life, and level of performance, the increase in social activity and presence of amputees in society is related to the increase of the quality of life and the induction of a useful social role [31]. Consistent with our findings, MacKenzie et al., in a study entitled "functional outcomes following trauma-related lower-extremity amputation", found the effect of amputation and appropriate surgery to cover the stump with suitable and sufficient soft tissue, patient's personality, health status, prosthetic technology skills and patient's activity level in improving the quality of life of amputees [32]. The present research investigated the quality of life of amputees and the effect of comprehensive corrective protocol on the activity and presence of amputees in society to improve their quality of life. In general, the research background and the present research point to the effective role of corrective exercises in the quality of life and the useful role of amputees in society.
The quality of life of amputees created lower quality due to the lack of limbs, the resulting physical and mental problems, and society's view of this group [3, 32]. According to the results, we can declare that carrying out organized physical activities in the form of suitable correction protocols improved the physical conditions of amputees, such as improving the motor range of joints, improving muscle strength and endurance, and also helping to gain optimal flexibility. In addition, informing people about unfavorable physical conditions, teaching optimal body postures, correcting wrong posture and motor habits, and improving methods of optimal use of prostheses during various activities can lead to the return of this group of people to society and improve their quality of life. The possible reasons for improving the quality of life in amputees are improving their functional levels, individual independence, self-esteem, and a sense of efficiency in life, work, and sports activities.
Another result of the present research was the effectiveness of the corrective protocol in improving the gait speed of lower limb amputations. Amputees suffer from gait and stepping disorders and adopt body positions and compensatory movements to facilitate walking and reduce speed [15, 24]. Therefore, by designing and implementing appropriate and efficient comprehensive corrective protocols in this research under the supervision of a corrective exercise specialist, we observed the improvement of daily activities, individual independence, and functional abilities of amputees. The results of this research are consistent with the findings of Abou et al. [33] and Wong et al. [15] concerning gait speed. Abou et al., in a review study, showed that specific sports activities have a positive effect on the balance and walking speed of amputees compared to traditional prosthetic exercises [33]. Wong et al., in a study entitled "exercise programs to improve gait performance in people with lower limb amputation", emphasized the effect of rehabilitation and use of prosthesis after amputation on wound healing and individual performance, as well as the effect of following exercises such as gait, biofeedback, and balance exercises on improving gait speed and quality of life [15]. It seems that due to amputation, muscle weakness and neuromuscular limitations occur, and a training program focusing on strengthening exercises, balance, flexibility, and correction of gait patterns can increase the speed and quality of gait by increasing the production of muscle power considering the age, level of amputation, and physical conditions of people [24].
In total, this research showed the effectiveness of comprehensive corrective protocol on indicators of postural control, back pain, quality of life, and gait speed of unilateral lower limb amputees. Following comprehensive corrective protocols is suggested considering various educational dimensions, correction of behavioral, postural, and motor habits, and recovery of optimal muscle balance aiming to restore the length of muscles, stiff and shortened tissues, fixing existing contractures, strengthening weak and inhibited muscles, development of endurance, functional, and motor power, restoring the correct motor patterns and optimal use of the prosthesis according to the special conditions of each subject. Also, awareness of physical-movement conditions and self-conscious improvement of body structure and alignment improves balance and postural control indicators, reduces back pain intensity, and improves the quality of life and gait speed index in unilateral lower limb amputees. Due to the side effects of amputation on the physical and mental dimensions, postural and motor patterns, functional abilities, social dimensions, and other quality aspects of life in disabled people with one-sided amputee of the lower limb, it is suggested to use the comprehensive corrective protocols for different recover areas of rehabilitation, reducing negative effects, and improving abilities. In addition, following the corrective exercises protocol as a standard approach in daily programs causes a decrease in the development of physical, mental, and social disabilities and the secondary effects of the disability in this group of people.
In the present study, due to the long distance of the patients from Tehran, first, the exercises were performed in person at the Tehran Red Crescent Movement Center, and then they were performed remotely at home with the researcher closely monitoring the correct implementation of the exercises. But it will be much better if future researchers can do face-to-face exercises with patients.
It is suggested to conduct a study similar to the present study on above-knee amputees and use other exercise protocols to improve muscle balance, prevent falls and improve the walking speed of amputees. In addition, it is suggested to use other tests and methods to check variables such as posture control, walking speed, and low back pain.
Conclusion
The comprehensive corrective protocol affects indicators of postural control, back pain, quality of life, and gait speed of unilateral lower limb amputees. Also, awareness of physical-movement conditions and self-conscious improvement of body structure and alignment improves balance and postural control indicators, reduces back pain intensity, and improves the quality of life and gait speed index in unilateral lower limb amputees.
Acknowledgments: We are grateful to all the amputees of Red Crescent Rehabilitation Center who participated in this study.
Ethical permissions: Before conducting the research, the necessary arrangements were made with the officials of Red Crescent Rehabilitation Center and Raja University. Also, after initial evaluations and proposal writing, the said plan was approved by the Research Commission of the Red Crescent Rehabilitation Center in compliance with ethical principles (Code: IR.SSRC.REC.1398.120). In addition, before conducting the research, the subjects were satisfied Ensure that the information collected will be kept confidential.
Conflict of Interest: No conflict of interest was reported.
Contribution of authors: Seddighmokhtari N (First Author), Introduction Writer/Main Researcher (45%); Gheitasi M (Second Author), Assistant Researcher/Discussion Writer (30%); Miri H (Third Author), Assistant Researcher (2%); Bayattork M (Fourth Author), Methodologist/Statistical Analyst (23%)
Funding: The present research has not received financial support from any institution or organization

Discussion
This study aimed to investigate the effect of an 8-week comprehensive rehabilitation protocol, including corrective exercises, correct posture training, mirror therapy, daily activities training, and use of prosthesis on indicators of postural control, back pain, quality of life, and gait speed in adults with unilateral lower limb amputation.
In this research, the postural control index was assessed in six positions separately. There was no significant difference between the existence of three senses of vision, vestibular and proprioceptive, removing vision, and vestibular sense change in the training group than the control group. Also no significant difference was observed in the training group after the post-test. The position 3 to 6 included proprioception change, vision removal and proprioception change, and vestibular and proprioception change. The results of investigating the 3-last positions showed a significant difference between the training and control groups; also, the post-test results showed a significant difference in the training group. The findings of this research on the effective role of corrective exercises in improving postural control and balance in lower limb amputees are accordant with the findings of Schafer et al. [9, 21], Mohamadtaghi et al. [22, 23], Damayanti Sethy et al. [24], Miller et al. [25], Devan et al. [2], and Moradi et al. [1]. Schafer et al., in a randomized controlled trial, looked for the role of a 12-week personal exercise program on the balance of lower limb amputees after home exercise sessions of the exercise group, including balance, endurance, strength, and flexibility exercises on balance scores. The exercise group significantly increased muscle symmetry and weight bearing while standing on an unstable surface without visual input and sensory feedback [21]. Mohamadtaghi et al., in another research entitled "effect of the selected balance program on postural control of amputees under the manipulation of visual, vestibular, and proprioceptive systems with 14 subjects in training and control groups", found that following a therapeutic exercise program was effective in improving balance and increasing stability. Probably, the reasons for effectiveness in the functional conditions of amputees were performing balance exercises, improving the muscle strength in the central portion of the body, improving the proprioceptive function of amputees, and increasing the control of posture in subjects. Postural control indicators in unilateral lower limb amputees changed because of muscle imbalance caused by excessive use of certain groups of muscles and inactivity and proper use of another group, and it inclines the patients towards performing compensatory movements and adopting compensatory postures such as bending to the prosthetic side and creating an unfavorable alignment in the person's posture as a compensatory strategy [22, 23]. One of the prevention and compensation strategies in the design and implementation of corrective protocols for improving postural control by affecting weight distribution between two organs is the proper use of the central muscles of the body and optimal use of the prosthesis during functional activities, which has an important and effective role in maintaining balance and postural control, especially during movement activities [24, 25]. Selective correction exercises, emphasizing the strength of the central portion of the body, improving power and endurance of pelvic-thigh muscles, improving balance and postural control in different situations during 8 weeks, aimed to improve the functional ability of people while using a prosthesis, gait and improving their quality of life [2, 26].
The reduction of back pain in the training group was another result of this research. Back pain is one of the secondary and undeniable conditions after amputation [12]. In this research, we tried to decrease back pain intensity in the subjects using emphasizing exercises in the center portion of the body especially pelvic and thigh muscles, increasing motor control, improving neuromuscular coordination, and improving the alignment of the pelvic and lumbar areas in the frontal and sagittal planes. Also, the findings of Shin et al. [10], Fatone et al. [26], and Faraji et al. [8] showed a decrease in the long-term risk of back pain using a change in the movement strategy of amputees [27]. Consistent with our findings, Shin et al. [10] in a study entitled "effects of lumbar strengthening exercise in lower-limb amputees with chronic back pain", emphasized strengthening exercises to reduce pain and increase the strength of back extensors by strengthening exercises and declared that following exercises prevents atrophy of trunk muscles and compression of joints and have an effect of 71% in reducing the back pain of amputees. It’s because of strengthening the muscles of the central portion of the body, strengthening atrophied muscles, and stretching weak muscles [7, 15]. Similar to our results, Faraji et al. [8], in a study entitled "the effect of 12-week corrective training on lumbar multifidus muscle asymmetry and pain intensity in veterans with one-sided below-knee amputation suffering from chronic back pain", mentioned the positive effect of 12 weeks corrective training on the decrease of back pain intensity whereas there was no effect on the multifidus muscle asymmetry in a maximum contraction of the muscle and muscular endurance. Therefore, this research aimed to design and implement a comprehensive corrective protocol to restore muscle balance, improve the levels of neuromuscular coordination and motor control, especially in the subject who used the prosthesis during daily life activities such as gait, and improve motor patterns and postural strategies in order to reduce back pain intensity in the subject.
There was a significant increase in the quality of life in the training group than in the control group after the post-test. The use of prostheses on amputees has a positive effect on their quality of life since the amputee does not enjoy the same conditions as healthy people, such as the use of stairs, vehicles, and the lack of urban furniture. Selected corrective exercises focus on strengthening weak and stretched muscles, restoring the length of muscles and shortened soft tissues, creating functional organ coordination, and acquiring the ability to perform efficient movements and improve the quality of life of amputees [28, 29].
Our results are consistent with the findings of Bouzas et al. [30], Wasser et al. [12], Miller et al. [25], Parker et al. [31], and MacKenzie et al. [32]. Bouzas et al. reviewed the effect of exercise on the physical performance of amputees and pointed out the role of combined positive, endurance, and functional exercises on respiratory stress, muscle fitness, and better performance in adults with unilateral lower limb amputation [30]. Wasser et al. investigated the exercise intervention for unilateral amputees with low back pain and concluded that stability exercises have a significant role in central body stability, lumbar strength, and dynamic stability, changing the musculoskeletal system, reducing pain, improving quality of life, and reducing injuries caused by the physical problems of amputees [12]. Miller et al., in a study entitled "the effect of a supervised community–based exercise program on balance, balance confidence, and gait in individuals with lower limb amputation", mentioned the positive effect of exercise and rehabilitation programs to maintain the ability and functional activities of amputees on improving their quality of life [25]. In the research by Parker et al., who examined the relationship between the motor ability of amputees, quality of life, and level of performance, the increase in social activity and presence of amputees in society is related to the increase of the quality of life and the induction of a useful social role [31]. Consistent with our findings, MacKenzie et al., in a study entitled "functional outcomes following trauma-related lower-extremity amputation", found the effect of amputation and appropriate surgery to cover the stump with suitable and sufficient soft tissue, patient's personality, health status, prosthetic technology skills and patient's activity level in improving the quality of life of amputees [32]. The present research investigated the quality of life of amputees and the effect of comprehensive corrective protocol on the activity and presence of amputees in society to improve their quality of life. In general, the research background and the present research point to the effective role of corrective exercises in the quality of life and the useful role of amputees in society.
The quality of life of amputees created lower quality due to the lack of limbs, the resulting physical and mental problems, and society's view of this group [3, 32]. According to the results, we can declare that carrying out organized physical activities in the form of suitable correction protocols improved the physical conditions of amputees, such as improving the motor range of joints, improving muscle strength and endurance, and also helping to gain optimal flexibility. In addition, informing people about unfavorable physical conditions, teaching optimal body postures, correcting wrong posture and motor habits, and improving methods of optimal use of prostheses during various activities can lead to the return of this group of people to society and improve their quality of life. The possible reasons for improving the quality of life in amputees are improving their functional levels, individual independence, self-esteem, and a sense of efficiency in life, work, and sports activities.
Another result of the present research was the effectiveness of the corrective protocol in improving the gait speed of lower limb amputations. Amputees suffer from gait and stepping disorders and adopt body positions and compensatory movements to facilitate walking and reduce speed [15, 24]. Therefore, by designing and implementing appropriate and efficient comprehensive corrective protocols in this research under the supervision of a corrective exercise specialist, we observed the improvement of daily activities, individual independence, and functional abilities of amputees. The results of this research are consistent with the findings of Abou et al. [33] and Wong et al. [15] concerning gait speed. Abou et al., in a review study, showed that specific sports activities have a positive effect on the balance and walking speed of amputees compared to traditional prosthetic exercises [33]. Wong et al., in a study entitled "exercise programs to improve gait performance in people with lower limb amputation", emphasized the effect of rehabilitation and use of prosthesis after amputation on wound healing and individual performance, as well as the effect of following exercises such as gait, biofeedback, and balance exercises on improving gait speed and quality of life [15]. It seems that due to amputation, muscle weakness and neuromuscular limitations occur, and a training program focusing on strengthening exercises, balance, flexibility, and correction of gait patterns can increase the speed and quality of gait by increasing the production of muscle power considering the age, level of amputation, and physical conditions of people [24].
In total, this research showed the effectiveness of comprehensive corrective protocol on indicators of postural control, back pain, quality of life, and gait speed of unilateral lower limb amputees. Following comprehensive corrective protocols is suggested considering various educational dimensions, correction of behavioral, postural, and motor habits, and recovery of optimal muscle balance aiming to restore the length of muscles, stiff and shortened tissues, fixing existing contractures, strengthening weak and inhibited muscles, development of endurance, functional, and motor power, restoring the correct motor patterns and optimal use of the prosthesis according to the special conditions of each subject. Also, awareness of physical-movement conditions and self-conscious improvement of body structure and alignment improves balance and postural control indicators, reduces back pain intensity, and improves the quality of life and gait speed index in unilateral lower limb amputees. Due to the side effects of amputation on the physical and mental dimensions, postural and motor patterns, functional abilities, social dimensions, and other quality aspects of life in disabled people with one-sided amputee of the lower limb, it is suggested to use the comprehensive corrective protocols for different recover areas of rehabilitation, reducing negative effects, and improving abilities. In addition, following the corrective exercises protocol as a standard approach in daily programs causes a decrease in the development of physical, mental, and social disabilities and the secondary effects of the disability in this group of people.
In the present study, due to the long distance of the patients from Tehran, first, the exercises were performed in person at the Tehran Red Crescent Movement Center, and then they were performed remotely at home with the researcher closely monitoring the correct implementation of the exercises. But it will be much better if future researchers can do face-to-face exercises with patients.
It is suggested to conduct a study similar to the present study on above-knee amputees and use other exercise protocols to improve muscle balance, prevent falls and improve the walking speed of amputees. In addition, it is suggested to use other tests and methods to check variables such as posture control, walking speed, and low back pain.
Conclusion
The comprehensive corrective protocol affects indicators of postural control, back pain, quality of life, and gait speed of unilateral lower limb amputees. Also, awareness of physical-movement conditions and self-conscious improvement of body structure and alignment improves balance and postural control indicators, reduces back pain intensity, and improves the quality of life and gait speed index in unilateral lower limb amputees.
Acknowledgments: We are grateful to all the amputees of Red Crescent Rehabilitation Center who participated in this study.
Ethical permissions: Before conducting the research, the necessary arrangements were made with the officials of Red Crescent Rehabilitation Center and Raja University. Also, after initial evaluations and proposal writing, the said plan was approved by the Research Commission of the Red Crescent Rehabilitation Center in compliance with ethical principles (Code: IR.SSRC.REC.1398.120). In addition, before conducting the research, the subjects were satisfied Ensure that the information collected will be kept confidential.
Conflict of Interest: No conflict of interest was reported.
Contribution of authors: Seddighmokhtari N (First Author), Introduction Writer/Main Researcher (45%); Gheitasi M (Second Author), Assistant Researcher/Discussion Writer (30%); Miri H (Third Author), Assistant Researcher (2%); Bayattork M (Fourth Author), Methodologist/Statistical Analyst (23%)
Funding: The present research has not received financial support from any institution or organization
Keywords:
References
1. Moradi Y, Behpoor N, Ghaeeni S, Shamsakohan P. Effects of 8 weeks aquatic exercise on static balance in veterans with unilateral lower limb amputation. Iran J War Public Health. 2014;6(2) :27-34. [Link]
2. Devan H, Carman A, Hendrick P, Hale L, Ribeiro DC. Spinal, pelvic, and hip movement asymmetries in people with lower-limb amputation: Systematic review. J Rehabil Res Dev. 2015;52(1):1-19. [Link] [DOI:10.1682/JRRD.2014.05.0135]
3. Esquenazi A, DiGiacomo R. Rehabilitation after amputation. J Am Podiatr Med Assoc. 2001;91(1):13-22. [Link] [DOI:10.7547/87507315-91-1-13]
4. Mohamadtaghi M, Shamsipour P, Hejazi P. Effects of manipulating visual, auditory and proprioceptive sensory in formations on the balance in healthy subjects and lower limb amputees. J Shahrekord Uuniv Med Sci. 2016;18(5):115-27. [Persian] [Link]
5. Sahay P, Prasad SK, Anwer S, Lenka PK, Kumar R. Efficacy of proprioceptive neuromuscular facilitation techniques versus traditional prosthetic training for improving ambulatory function in transtibial amputees. Hong Kong Physiother J. 2014;32(1):28-34. [Link] [DOI:10.1016/j.hkpj.2013.02.002]
6. França FR, Burke TN, Hanada ES, Marques AP. Segmental stabilization and muscular strengthening in chronic low back pain: a comparative study. Clinics. 2010;65(10):1013-7. [Link] [DOI:10.1590/S1807-59322010001000015]
7. Butowicz CM, Yoder AJ, Farrokhi S, Mazzone B. Low back pain influences trunk-lower limb joint coordination and balance control during standing in persons with lower limb loss. Clin Biomech. 2022;92:105580. [Link] [DOI:10.1016/j.clinbiomech.2022.105580]
8. Faraji A, Barati A, Sadeghi H, Fateh H, Allami M, Soroush M. Effect of 12 weeks of corrective movement exercises on lumbar multifidus muscle asymmetry and pain intensity in unilateral amputees with chronic low back pain. Iran J War Public Health. 2018;10(1):47-52. [Link] [DOI:10.29252/ijwph.10.1.47]
9. Schafer ZA, Perry JL, Vanicek N. A personalised exercise programme for individuals with lower limb amputation reduces falls and improves gait biomechanics: A block randomised controlled trial. Gait Posture. 2018;63:282-9. [Link] [DOI:10.1016/j.gaitpost.2018.04.030]
10. Shin MK, Yang HS, Yang HE, Kim DH, Ahn BR, Kwon H, et al. Effects of lumbar strengthening exercise in lower-limb amputees with chronic low back pain. Ann Rehabil Med. 2018;42(1):59-66. [Link] [DOI:10.5535/arm.2018.42.1.59]
11. Godlwana L, Stewart A, Musenge E. The effect of a home exercise intervention on persons with lower limb amputations: a randomized controlled trial. Clin Rehabil. 2020;34(1):99-110. [Link] [DOI:10.1177/0269215519880295]
12. Wasser JG, Herman DC, Horodyski M, Zaremski JL, Tripp B, Page P, et al. Exercise intervention for unilateral amputees with low back pain: study protocol for a randomised, controlled trial. Trials. 2017;18(1):630. [Link] [DOI:10.1186/s13063-017-2362-0]
13. Brooks D Parsons J, Hunter JP, Devlin M, Walker J. The 2-minute walk test as a measure of functional improvement in persons with lower limb amputation. Arch Phys Med Rehabil. 2001;82(10):1478-83. [Link] [DOI:10.1053/apmr.2001.25153]
14. Batten HR, McPhail SM, Mandrusiak AM, Varghese PN, Kuys SS. Gait speed as an indicator of prosthetic walking potential following lower limb amputation. Prosthet Orthot Int. 2019;43(2):196-203. [Link] [DOI:10.1177/0309364618792723]
15. Wong CK, Ehrlich JE, Ersing JC, Maroldi NJ, Stevenson CE, VarcaMJ. Exercise programs to improve gait performance in people with lower limb amputation: A systematic review. Prosthet Orthot Int. 2016;40(1):8-17. [Link] [DOI:10.1177/0309364614546926]
16. Barnett CT, Vanicek N, Polman R. Postural responses during volitional and perturbed dynamic balance tasks in new lower limb amputees: A longitudinal study. Gait Posture. 2013;37(3):319-25. [Link] [DOI:10.1016/j.gaitpost.2012.07.023]
17. Alghadir AH, Anwer S, Iqbal A, Iqbal ZA. Test-retest reliability, validity, and minimum detectable change of visual analog, numerical rating, and verbal rating scales for measurement of osteoarthritic knee pain. J Pain Res. 2018;11:851-56. [Link] [DOI:10.2147/JPR.S158847]
18. Rouhani N, Esfandiari E, Babaee T, Khosravi M, Moradi V. The comprehensive lower limb amputee socket survey: reliability and validity of the Persian version. Prosthet Orthot Int. 2021;45(2):131-7. [Link] [DOI:10.1177/0309364620958526]
19. Mazaheri M, Fardipour S, Salavati M, Hadadi M, Negahban H, Bahramizadeh M, et al. The Persian version of Trinity Amputation and Prosthetics Experience Scale: translation, factor structure, reliability and validity. Disabil Rehabil. 2011;33(19-20):1737-45. [Link] [DOI:10.3109/09638288.2010.544838]
20. Stahlhut M, Downs J, Leonard H, Bisgaard AM, Nordmark E. Building the repertoire of measures of walking in Rett syndrome. Disabil Rehabil. 2017;39(19): 1926-31. [Link] [DOI:10.1080/09638288.2016.1212280]
21. Schafer ZA, Vanicek N. A block randomised controlled trial investigating changes in postural control following a personalised 12-week exercise programme for individuals with lower limb amputation. Gait Posture. 2021;84:198-204. [Link] [DOI:10.1016/j.gaitpost.2020.12.001]
22. Mohammadtaghi B, Hejazi Dinan P, Shamsipour Dehkordi P. The effects of 12 sessions of mirror therapy on postural control kinetic variables of amputation below the knee in terms of the manipulation of afferent information. Armaghan-e-Danesh. 2016;21(2):160-73. [Persian] [Link]
23. Mohamadtaghi B, Hejazi Dinan P, Shamsipour Dehkordi P. Effect of the selected balance program on postural control of amputees under manipulation of visual, vestibular and proprioceptive systems. Iran J War Public Health. 2016;8(1):1-8. [Link] [DOI:10.18869/acadpub/IJWPH.2016.01]
24. Damayanti Sethy M, Kujur ES, Sau K. Effect of balance exercise on balance control in unilateral lower limb amputees. Indian J Occup Ther. 2009;41(3):63-8. [Link]
25. Miller CA, Williams JE, Durham KL, Hom SC, Smith JL. The effect of a supervised community-based exercise program on balance, balance confidence, and gait in individuals with lower limb amputation. Prosthet Orthot Int. 2017;41(5):446-54. [Link] [DOI:10.1177/0309364616683818]
26. Fatone S, Stine R, Gottipati P, Dillon M. Pelvic and spinal motion during walking in persons with transfemoral amputation with and without low back pain. Am J Phys Med Rehabil. 2016;95(6):438-47. [Link] [DOI:10.1097/PHM.0000000000000405]
27. Actis JA, Nolasco LA, Gates DH, Silverman AK. Lumbar loads and trunk kinematics in people with a transtibial amputation during sit-to-stand. J Biomech. 2018;69:1-9. [Link] [DOI:10.1016/j.jbiomech.2017.12.030]
28. Seay JF, Van Emmerik REA, Hamill J. Influence of low back pain status on pelvis-trunk coordination during walking and running. Spine. 2011;36(16):E1070-9. [Link] [DOI:10.1097/BRS.0b013e3182015f7c]
29. Morgenroth DC, Orendurff MS, Shakir A, Segal A, Shofer J, Czerniecki JM. The relationship between lumbar spine kinematics during gait and low-back pain in transfemoral amputees. Am J Phys Med Rehabil. 2010;89(8):635-43. [Link] [DOI:10.1097/PHM.0b013e3181e71d90]
30. Bouzas S, Molina AJ, Fernández-Villa T, Miller K, Sanchez-Lastra MA, Ayán C. Effects of exercise on the physical fitness and functionality of people with amputations: systematic review and meta-analysis. Disabil Health J. 2021;14(1):100976. [Link] [DOI:10.1016/j.dhjo.2020.100976]
31. Parker K, Kirby RL, Adderson J, Thompson K. Ambulation of people with lower-limb amputations: relationship between capacity and performance measures. Arch Phys Med Rehabil. 2010;91(4):543-9. [Link] [DOI:10.1016/j.apmr.2009.12.009]
32. MacKenzie EJ, Bosse MJ, Castillo RC, Smith DG, Webb LX, Kellam JF, et al. Functional outcomes following trauma-related lower-extremity amputation. J Bone Joint Surg Am. 2004;86(8):1636-45. [Link] [DOI:10.2106/00004623-200408000-00006]
33. Abou L, Fliflet A, Zhao L, Du Y, Rice L. The effectiveness of exercise interventions to improve gait and balance in individuals with lower limb amputations: a systematic review and meta-analysis. Clin Rehabil. 2022;36(7):857-72. [Link] [DOI:10.1177/02692155221086204]










