Volume 13, Issue 1 (2021)
Iran J War Public Health 2021, 13(1): 57-61 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2021/05/12 | Accepted: 2021/08/25 | Published: 2021/09/11
Received: 2021/05/12 | Accepted: 2021/08/25 | Published: 2021/09/11
How to cite this article
Nazari M, Movahed E, Soltaninejad M. Survey Hospitals Preparedness and Resilience in Crisis COVID-19 in the South of Kerman Province, Iran. Iran J War Public Health 2021; 13 (1) :57-61
URL: http://ijwph.ir/article-1-981-en.html
URL: http://ijwph.ir/article-1-981-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
1- Health in Disasters and Emergencies Research Center, Kerman University of Medical Sciences, Kerman, Iran
2- School of Public Health, Jiroft University of Medical Sciences, Jiroft, Iran
3- Department of Scientometrics, Jiroft University of medical sciences, Jiroft, Iran
2- School of Public Health, Jiroft University of Medical Sciences, Jiroft, Iran
3- Department of Scientometrics, Jiroft University of medical sciences, Jiroft, Iran
Full-Text (HTML) (506 Views)
Introduction
One of the problems that constantly threatens human life is the occurrence of disasters and events. Disasters occur without prior knowledge. Events such as floods, earthquakes, fires, volcanoes, water pollution, and epidemics of diseases are among the most unforeseen circumstances globally [1]. Iran is one of the ten most vulnerable countries globally, and according to statistics, 31 out of 40 natural disasters have been registered in the world, have occurred in Iran, and the probability of it happening in the future is not far from expected [2]. Looking at past statistics, we can see the lack of preparedness to deal with crises and increased disasters. In several studies, it was found that the health system in Iran for effective control of disasters or public health emergencies is at a low level in terms of preparedness and equipment [3].
Some institutions have failed to train their employees, and despite the hospital's crisis management teams, they have not been very efficient, and hospitals are not ready yet. Preparedness can be defined as one of the stages of the events management cycle, and planning, human resources, equipment, practice, and maneuvering are considered its components [4]. The purpose of preparedness is to know what to do, how to do it, and the necessary equipment when disasters occur [5]. In the face of crises, each organization should have a codified program; medical centers are no exception because they are the first centers that deal with event victims [6].
Another critical issue due to the increase in natural disasters and unforeseen events are paying serious attention to the management and resilience of cities and organizations. Strength transforms organizations into constructive elements that can be sufficiently prepared and prepared against events and is the function of three variables: situational awareness, adaptability capacity, and critical vulnerability [4].
In early 2020, an unexpected incident called the new covid-19 epidemic began in Wuhan, China, spread rapidly worldwide, and became a significant pandemic [7]. According to the World Health Organization (WHO), as of April 5, 2020, 1133,046 people were infected in all countries and 55,743 males in Iran [8]. The disease has already caused enormous economic and psychological damages in human societies.
According to a U.S. study, the results showed that if the covid-19 pandemic is similar to the 1957-1968 flu, especially if it is stable, it requires twice as many unique beds and surgery because some patients need rare sources such as out-of-body membrane oxygenation and ventilators. The hospital is prepared for how patients share, allocate resources, and staff departments [9].
The WHO has published guidelines for all countries on how to be prepared for Covid-19. The guide includes monitoring patients, testing samples, treating patients, and controlling infection in health centers [10]. one of the factors that 20% of patients need is ICU, as well as X-ray equipment, is needed for diagnosis of the disease, besides, the hospital should be used to transfer the patient if necessary to move from predetermined routes and to protect personnel. Other patients and visitors of filter masks type 2 and 3 [11].
Although The World Health Organization (WHO) has published guidelines, it seems that there is a significant difference in the level of development of health services in Kerman province, according to results of studies in this field, using the focus index of Vegstaff, Pasi, and Dorsler has shown that the most focus of health services is in Kerman city. This index has been ranked the cities of Kerman province in four levels that Jiroft city in the level between concentration and the towns of Baft, Zarand, Kahnouj, Babak City, Bardsir, Anbarabad, Ravar, Rudbar Jonub, Fahraj, Anar, Rabbar, Reagan, Manujan, Qal'eh Ganj and Koohbanan are at the level of concentration [12].
Considering the importance of people health in society and the fact that having physical and mental health is the universal right of the people, and the use of health care facilities by the people of the society has been emphasized in the Constitution of the Islamic Republic of Iran, in some deprived areas of Iran, including seven cities in the south of Kerman province, health services have been distributed at a lower level. Therefore, this study investigated the preparedness and resilience of hospitals in the South of Kerman Province, Iran.
Instrument and Methods
This descriptive study was designed cross-sectional and conducted by health officials (Crisis Committee) working at Hospitals of Jiroft University of Medical Sciences South Kerman from April 2020 to Mar 2021. Members of the Crisis Committee in 7 hospitals in the south of Kerman province covered by Jiroft University of Medical Sciences were chosen. According to Morgan's table, a sample size of 77 cases was obtained; 11 people (head of the hospital, internal manager, accreditation officer and occupational health officer of the hospital, etc.) from each hospital completed the questionnaire. Inclusion criteria included people who were active in Jiroft University of Medical Sciences and tended to cooperate.
The data collection tool was two preparedness and resilience questionnaires. Preparedness questionnaire derived from the CDC (Centers for Disease Control and Prevention) checklist including ten components: infection prevention and control policies and training for HCP, the process for the rapid identification and isolation of patients with confirmed or suspected Covid-19, patient placement, transmission-based precautions, movement of a confirmed or suspected Covid-19 patient within the facility, hand hygiene, environment cleaning, monitoring, and managing HCP, and visitor access and movement within the facility. It is 76 globes that will be scored in three Likert spectrums (not started, completed, and in progress), which will be achieved with grades (0, 1, and 2), respectively. The score of this section is reported in frequency and percentage, and the closer it gets to 100, the more hospitals are prepared for the COVID-19. The organizational resilience questionnaire was created and translated by Dr. Asgari based on the McManus model [13]. This questionnaire has 67 questions. The scoring method of this questionnaire based on the Likert 5 degree spectrum is very high, high, somewhat low, deficient, which is awarded to low score one and very high score 5. This score will range from 67 to 335; obviously, the higher the score, the higher the organizational resilience, and vice versa. Considering that this questionnaire was researcher-made and translated and there was no information about its validity and reliability, therefore, to determine the apparent and content validity (CVR) of the questionnaire, we first confirmed it to 10 expert professors. Then, to obtain reliability, we used Cronbach's alpha method so that by sending the questionnaire online to 30 participants, the reliability of the questionnaire was calculated higher than 0.7.during the survey.
After obtaining the code of ethics from the Ethics Committee of Jiroft University of Medical Sciences (IR.JMU.REC.1399.008), researchers obtained the list of eligible individuals by referring to the hospitals in the south of Kerman province, Iran. Before sampling, participants were provided with explanations about the study's purpose, and informed consent forms were obtained. Furthermore, they were ensured about confidentially of information. They were free to skip any question or quit the survey if they so desired. No human subject was directly involved or at risk. Questionnaires were distributed twice among the members of the Hospital Crisis Committee. The first stage was distributed in print, and the second stage was via Google Drive and online.
Descriptive statistics (frequency, percentage, mean, and standard deviation) described the study population. The Preparedness and Resilience were evaluated using the Pearson correlation coefficient and the Chi-square using SPSS 25 software for data analysis.
Findings
A total of 77 respondents Crisis Committee, each working in 7 hospitals at total Hospitals, were included in the study.
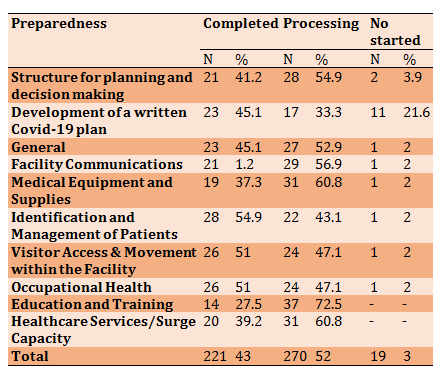
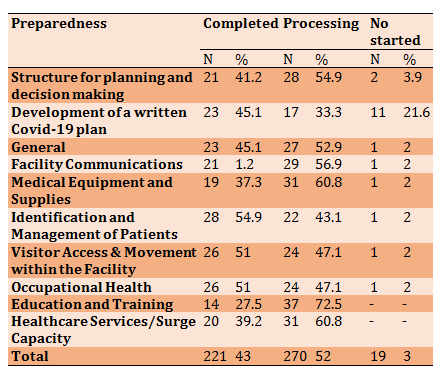
According to Table 1, the most amount frequency of preparedness related to identification and management of patients by 54.%. The lowest rate was facility communications by 1.2%. Overall, 43% of the preparedness was complete, 52% was in progress, and 3% was not yet started.
Table 1) Frequency Preparedness of hospitals in the south of Kerman against covid-19
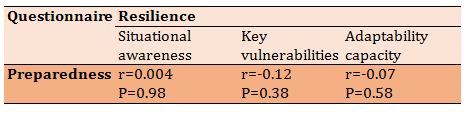
The mean scores of resilience were 194.37±41.40 (Table 2). The rate of the "key vulnerabilities" component in the resilience was higher than the other components.
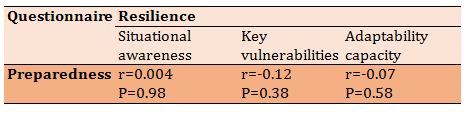
There was no relationship between preparedness and component of resilience in Hospitals (Table 3).
Table 2) Mean and standard deviation of preparedness and resilience

Table 3) Results of the Pearson correlation coefficient
Discussion
This study was conducted to determine the preparedness and resilience of Jiroft University of Medical Sciences Hospitals in South Kerman from April 2020 to Mar 2021. The perceived level of preparedness was low to moderate, and the mean score of resilience was higher than average. Also, in the survey of the relationship between readiness and strength, the result showed no correlation between preparedness and stability, consistent with the study of Andrea Grimes et al. [14]. In this study, the mean level of resilience was 194.37, Which is higher compared to nursing student cohorts in Hong Kong (24.00), India (26.31), Nigeria (27.64), and Northern Queensland Australia [15-17].
Our survey during the covid-19 epidemic provided some information on the lack of preparedness in different components in south Kerman hospitals. Our results showed that less than 50% of hospitals were prepared to deal with the crisis in the covid-19, and the highest rate of preparedness related to "Identification and Management of Patients" by 54.9% and The lowest rate was "Facility Communications" by 1.2% in during covid-19 epidemic. That is consistent with the study by Khorsand Chobdar et al., their survey also showed a low amount by" Facility Communications" and estimated the preparedness of hospitals in Sistan and Baluchestan province as equal to 40.12%, which is assessed as poor [18].
Therefore, the results indicate that hospitals in the south of Kerman and Iran are not suitable, and policymakers must plan to improve the preparedness indicators in hospitals in the south of the country. However, it is possible that due to geographical location, other hospitals in the north of the country and the capital have a more appropriate situation that requires further studies.
This survey found that 27.5 % of medical staff were trained, and 72.5% were training. A study of Pawan Kumar Hama in Nepal about preparedness in Government Hospitals of Physicians' point of view also shown that were only 53.8% trained in central hospitals [19].
This difference in results can be due to different samples in the two studies so that in our research, the head of the hospital, the internal manager, the accreditation officer, and the occupational health officer of the hospitals were investigated. However, in the study, Pawan Kumar Hama was only evaluated by the physicians. However, staff training in our study was not appropriate and required serious support and planning.
And the majority of medical doctors working in government hospitals of Nepal perceive that provision of facemask distribution, airborne isolation rooms, critical care preparedness, and hands-on staff training were not adequate [19]. Also, in the present study amount of medical equipment and supplies is estimated low.
Therefore, due to the rapid transmission of the covid-19 and the high mortality rate of the disease, the use of essential equipment such as isolation room, proper ventilation, preparation of the intensive unit of hospitals, and the use of durable equipment can be considered as a powerful tool for controlling and dealing with the covid-19 in critical situations.
In Survey of Shrestha et al. showed that Preparedness for Covid-19 Disease in Hospitals of Nepal in management of patients with Covid-19 are not well prepared, and to enhance national preparedness for the pandemic suggested Resource allocation and policymaking [20]. But in our study Identification and Management of Ill Patients with amount Frequency, 54.9% estimated moderated.
The finding of Ejercito Mangawa Balay-odao's study showed that Most clinical nurses perceived a high self-assessed Covid-19 hospital preparedness, by the mean score of 49.65±2.30; furthermore, all Covid-19 hospital preparedness subscales were rated as high [21]. Despite our study that subscale preparedness's low and the level of hospital preparedness is low.
Location, age group, and different geographical status can be the reason for differences in results in the two studies. The use of experienced experts and psychologists to train and promote confidence in hospital staff is of particular importance and can increase resilience.
In the present study, the mean resilience score was reported to be higher than the average. In Taylor's analysis, the results were in line with our study [22]. The positive characteristics of the participants like (age, years of experience, and degree of confidence in public health authorities) were lead to enhancement of resilience. As a person ages, their strength increases, especially in problem-solving and handling emotional problems [14]. Since the questionnaires were completed virtually and are self-reported, there were two main limitations in the present study.
Conclusion
This study found that hospitals' preparedness is low, and the mean score of resilience was higher than average. Thus, improving the health system during a crisis requires reviewing existing data and implementing new change ideas. The findings of this study help university administrators and policymakers improve the continuing education program, psychological support, and planning and decision making to control the crisis of the covid-19 epidemic.
Acknowledgments: This study was a research project in JMU. Researchers express their gratitude to the Crisis Committee Jiroft University of Medical Sciences, who participated in the study.
Ethical Permissions: This study was approved by the Ethics Committee of Jiroft University of Medical Sciences (IR.JMU.REC.1399.008).
Conflicts of Interests: Authors have not Conflicted with research interest.
Authors' Contributions: Nazari M. (First Author), Main Researcher (50%); Movahed E. (Second Author), Statistical Analyst (45%); Soltaninejad M. (Third Author), Introduction Writer/Methodologist/Discussion Writer (5%).
Funding/Support: This study was a research project in JMU by code grant (p-450).
One of the problems that constantly threatens human life is the occurrence of disasters and events. Disasters occur without prior knowledge. Events such as floods, earthquakes, fires, volcanoes, water pollution, and epidemics of diseases are among the most unforeseen circumstances globally [1]. Iran is one of the ten most vulnerable countries globally, and according to statistics, 31 out of 40 natural disasters have been registered in the world, have occurred in Iran, and the probability of it happening in the future is not far from expected [2]. Looking at past statistics, we can see the lack of preparedness to deal with crises and increased disasters. In several studies, it was found that the health system in Iran for effective control of disasters or public health emergencies is at a low level in terms of preparedness and equipment [3].
Some institutions have failed to train their employees, and despite the hospital's crisis management teams, they have not been very efficient, and hospitals are not ready yet. Preparedness can be defined as one of the stages of the events management cycle, and planning, human resources, equipment, practice, and maneuvering are considered its components [4]. The purpose of preparedness is to know what to do, how to do it, and the necessary equipment when disasters occur [5]. In the face of crises, each organization should have a codified program; medical centers are no exception because they are the first centers that deal with event victims [6].
Another critical issue due to the increase in natural disasters and unforeseen events are paying serious attention to the management and resilience of cities and organizations. Strength transforms organizations into constructive elements that can be sufficiently prepared and prepared against events and is the function of three variables: situational awareness, adaptability capacity, and critical vulnerability [4].
In early 2020, an unexpected incident called the new covid-19 epidemic began in Wuhan, China, spread rapidly worldwide, and became a significant pandemic [7]. According to the World Health Organization (WHO), as of April 5, 2020, 1133,046 people were infected in all countries and 55,743 males in Iran [8]. The disease has already caused enormous economic and psychological damages in human societies.
According to a U.S. study, the results showed that if the covid-19 pandemic is similar to the 1957-1968 flu, especially if it is stable, it requires twice as many unique beds and surgery because some patients need rare sources such as out-of-body membrane oxygenation and ventilators. The hospital is prepared for how patients share, allocate resources, and staff departments [9].
The WHO has published guidelines for all countries on how to be prepared for Covid-19. The guide includes monitoring patients, testing samples, treating patients, and controlling infection in health centers [10]. one of the factors that 20% of patients need is ICU, as well as X-ray equipment, is needed for diagnosis of the disease, besides, the hospital should be used to transfer the patient if necessary to move from predetermined routes and to protect personnel. Other patients and visitors of filter masks type 2 and 3 [11].
Although The World Health Organization (WHO) has published guidelines, it seems that there is a significant difference in the level of development of health services in Kerman province, according to results of studies in this field, using the focus index of Vegstaff, Pasi, and Dorsler has shown that the most focus of health services is in Kerman city. This index has been ranked the cities of Kerman province in four levels that Jiroft city in the level between concentration and the towns of Baft, Zarand, Kahnouj, Babak City, Bardsir, Anbarabad, Ravar, Rudbar Jonub, Fahraj, Anar, Rabbar, Reagan, Manujan, Qal'eh Ganj and Koohbanan are at the level of concentration [12].
Considering the importance of people health in society and the fact that having physical and mental health is the universal right of the people, and the use of health care facilities by the people of the society has been emphasized in the Constitution of the Islamic Republic of Iran, in some deprived areas of Iran, including seven cities in the south of Kerman province, health services have been distributed at a lower level. Therefore, this study investigated the preparedness and resilience of hospitals in the South of Kerman Province, Iran.
Instrument and Methods
This descriptive study was designed cross-sectional and conducted by health officials (Crisis Committee) working at Hospitals of Jiroft University of Medical Sciences South Kerman from April 2020 to Mar 2021. Members of the Crisis Committee in 7 hospitals in the south of Kerman province covered by Jiroft University of Medical Sciences were chosen. According to Morgan's table, a sample size of 77 cases was obtained; 11 people (head of the hospital, internal manager, accreditation officer and occupational health officer of the hospital, etc.) from each hospital completed the questionnaire. Inclusion criteria included people who were active in Jiroft University of Medical Sciences and tended to cooperate.
The data collection tool was two preparedness and resilience questionnaires. Preparedness questionnaire derived from the CDC (Centers for Disease Control and Prevention) checklist including ten components: infection prevention and control policies and training for HCP, the process for the rapid identification and isolation of patients with confirmed or suspected Covid-19, patient placement, transmission-based precautions, movement of a confirmed or suspected Covid-19 patient within the facility, hand hygiene, environment cleaning, monitoring, and managing HCP, and visitor access and movement within the facility. It is 76 globes that will be scored in three Likert spectrums (not started, completed, and in progress), which will be achieved with grades (0, 1, and 2), respectively. The score of this section is reported in frequency and percentage, and the closer it gets to 100, the more hospitals are prepared for the COVID-19. The organizational resilience questionnaire was created and translated by Dr. Asgari based on the McManus model [13]. This questionnaire has 67 questions. The scoring method of this questionnaire based on the Likert 5 degree spectrum is very high, high, somewhat low, deficient, which is awarded to low score one and very high score 5. This score will range from 67 to 335; obviously, the higher the score, the higher the organizational resilience, and vice versa. Considering that this questionnaire was researcher-made and translated and there was no information about its validity and reliability, therefore, to determine the apparent and content validity (CVR) of the questionnaire, we first confirmed it to 10 expert professors. Then, to obtain reliability, we used Cronbach's alpha method so that by sending the questionnaire online to 30 participants, the reliability of the questionnaire was calculated higher than 0.7.during the survey.
After obtaining the code of ethics from the Ethics Committee of Jiroft University of Medical Sciences (IR.JMU.REC.1399.008), researchers obtained the list of eligible individuals by referring to the hospitals in the south of Kerman province, Iran. Before sampling, participants were provided with explanations about the study's purpose, and informed consent forms were obtained. Furthermore, they were ensured about confidentially of information. They were free to skip any question or quit the survey if they so desired. No human subject was directly involved or at risk. Questionnaires were distributed twice among the members of the Hospital Crisis Committee. The first stage was distributed in print, and the second stage was via Google Drive and online.
Descriptive statistics (frequency, percentage, mean, and standard deviation) described the study population. The Preparedness and Resilience were evaluated using the Pearson correlation coefficient and the Chi-square using SPSS 25 software for data analysis.
Findings
A total of 77 respondents Crisis Committee, each working in 7 hospitals at total Hospitals, were included in the study.
According to Table 1, the most amount frequency of preparedness related to identification and management of patients by 54.%. The lowest rate was facility communications by 1.2%. Overall, 43% of the preparedness was complete, 52% was in progress, and 3% was not yet started.
Table 1) Frequency Preparedness of hospitals in the south of Kerman against covid-19
The mean scores of resilience were 194.37±41.40 (Table 2). The rate of the "key vulnerabilities" component in the resilience was higher than the other components.
There was no relationship between preparedness and component of resilience in Hospitals (Table 3).
Table 2) Mean and standard deviation of preparedness and resilience

Table 3) Results of the Pearson correlation coefficient
Discussion
This study was conducted to determine the preparedness and resilience of Jiroft University of Medical Sciences Hospitals in South Kerman from April 2020 to Mar 2021. The perceived level of preparedness was low to moderate, and the mean score of resilience was higher than average. Also, in the survey of the relationship between readiness and strength, the result showed no correlation between preparedness and stability, consistent with the study of Andrea Grimes et al. [14]. In this study, the mean level of resilience was 194.37, Which is higher compared to nursing student cohorts in Hong Kong (24.00), India (26.31), Nigeria (27.64), and Northern Queensland Australia [15-17].
Our survey during the covid-19 epidemic provided some information on the lack of preparedness in different components in south Kerman hospitals. Our results showed that less than 50% of hospitals were prepared to deal with the crisis in the covid-19, and the highest rate of preparedness related to "Identification and Management of Patients" by 54.9% and The lowest rate was "Facility Communications" by 1.2% in during covid-19 epidemic. That is consistent with the study by Khorsand Chobdar et al., their survey also showed a low amount by" Facility Communications" and estimated the preparedness of hospitals in Sistan and Baluchestan province as equal to 40.12%, which is assessed as poor [18].
Therefore, the results indicate that hospitals in the south of Kerman and Iran are not suitable, and policymakers must plan to improve the preparedness indicators in hospitals in the south of the country. However, it is possible that due to geographical location, other hospitals in the north of the country and the capital have a more appropriate situation that requires further studies.
This survey found that 27.5 % of medical staff were trained, and 72.5% were training. A study of Pawan Kumar Hama in Nepal about preparedness in Government Hospitals of Physicians' point of view also shown that were only 53.8% trained in central hospitals [19].
This difference in results can be due to different samples in the two studies so that in our research, the head of the hospital, the internal manager, the accreditation officer, and the occupational health officer of the hospitals were investigated. However, in the study, Pawan Kumar Hama was only evaluated by the physicians. However, staff training in our study was not appropriate and required serious support and planning.
And the majority of medical doctors working in government hospitals of Nepal perceive that provision of facemask distribution, airborne isolation rooms, critical care preparedness, and hands-on staff training were not adequate [19]. Also, in the present study amount of medical equipment and supplies is estimated low.
Therefore, due to the rapid transmission of the covid-19 and the high mortality rate of the disease, the use of essential equipment such as isolation room, proper ventilation, preparation of the intensive unit of hospitals, and the use of durable equipment can be considered as a powerful tool for controlling and dealing with the covid-19 in critical situations.
In Survey of Shrestha et al. showed that Preparedness for Covid-19 Disease in Hospitals of Nepal in management of patients with Covid-19 are not well prepared, and to enhance national preparedness for the pandemic suggested Resource allocation and policymaking [20]. But in our study Identification and Management of Ill Patients with amount Frequency, 54.9% estimated moderated.
The finding of Ejercito Mangawa Balay-odao's study showed that Most clinical nurses perceived a high self-assessed Covid-19 hospital preparedness, by the mean score of 49.65±2.30; furthermore, all Covid-19 hospital preparedness subscales were rated as high [21]. Despite our study that subscale preparedness's low and the level of hospital preparedness is low.
Location, age group, and different geographical status can be the reason for differences in results in the two studies. The use of experienced experts and psychologists to train and promote confidence in hospital staff is of particular importance and can increase resilience.
In the present study, the mean resilience score was reported to be higher than the average. In Taylor's analysis, the results were in line with our study [22]. The positive characteristics of the participants like (age, years of experience, and degree of confidence in public health authorities) were lead to enhancement of resilience. As a person ages, their strength increases, especially in problem-solving and handling emotional problems [14]. Since the questionnaires were completed virtually and are self-reported, there were two main limitations in the present study.
Conclusion
This study found that hospitals' preparedness is low, and the mean score of resilience was higher than average. Thus, improving the health system during a crisis requires reviewing existing data and implementing new change ideas. The findings of this study help university administrators and policymakers improve the continuing education program, psychological support, and planning and decision making to control the crisis of the covid-19 epidemic.
Acknowledgments: This study was a research project in JMU. Researchers express their gratitude to the Crisis Committee Jiroft University of Medical Sciences, who participated in the study.
Ethical Permissions: This study was approved by the Ethics Committee of Jiroft University of Medical Sciences (IR.JMU.REC.1399.008).
Conflicts of Interests: Authors have not Conflicted with research interest.
Authors' Contributions: Nazari M. (First Author), Main Researcher (50%); Movahed E. (Second Author), Statistical Analyst (45%); Soltaninejad M. (Third Author), Introduction Writer/Methodologist/Discussion Writer (5%).
Funding/Support: This study was a research project in JMU by code grant (p-450).
Keywords:
References
1. Khankeh HR, Mohammadi R, Ahmadi F. Health care delivery in the event of a natural disaster: A qualitative study. Iran J Nurs. 2007;20(51):85-96. [Persian] [Link]
2. Ghorbani M, Mahmood Zadeh A. Crisis management and crisis. Isfahan: GOLHAYE MOHAMMADI; 2005. [Persian] [Link]
3. Veenema TG. Disaster nursing and emergency preparedness: for chemical, biological, and radiological terrorism and other hazards. New York: Springer Publishing; 2012. [Link] [DOI:10.1891/9780826108654]
4. Rezaei Z, Ebrahiminejad M, Sadeghi Z. Investigation of the relationship between preparedness and organizational resilience when facing earthquake (case study: Medical sciences university hospitals in Kerman). Disaster Prev Manag Knowl. 2017;6(4):358-67. [Persian] [Link]
5. Coppola DP. Introduction to international disaster management. Amsterdam: Elsevier; 2010. [Link] [DOI:10.1016/B978-0-12-382174-4.00018-5]
6. Mirzaee F, Kakaei H, Farasati F, Zamani N. Investigation on the safety status and preparedness of Ilam's hospitals against disasters in 2012. J Ilam Univ Med Sci. 2015;22(7):14-23. [Persian] [Link]
7. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel covid-19 in Wuhan, China. Lancet. 2020;395(10223):497-506. [Link] [DOI:10.1016/S0140-6736(20)30183-5]
8. World health organization. Coronavirus disease (COVID-19) pandemic [Internet]. Geneva: World health Organization; 2020 [cited 2020 Mar 24]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019. [Link]
9. Chopra V, Toner E, Waldhorn R, Washer L. How should U.S. hospitals prepare for coronavirus disease 2019 (COVID-19). Ann Intern Med. 2020;172(9):621-2. [Link] [DOI:10.7326/M20-0907]
10. World health organization. Infection prevention and control during health care when novel COVID-19 (nCoV) infection is suspected [Internet]. Geneva: World health Organization; 2020 [cited 2020 Mar 24]. Available from: https://www.who.int/publications/i/item/10665-331495. [Link]
11. Jansson M, Liao X, Rello J. Strengthening ICU health security for a coronavirus epidemic. Intensive Crit care Nurs. 2020;57:102812. [Link] [DOI:10.1016/j.iccn.2020.102812]
12. Ghazanfarpour H. Stratification and development ratio of medical service in Kerman province cities by concentration index. J Spat Plan. 2014;3(4):1-17. [Persian] [Link]
13. McManus S. Resilience management: A framework for assessing and improving the resilience of organization. Thousand Oaks: BPR Publishers; 2007. [Link]
14. Grimes A, Sparke V, Rouen C, West C. Preparedness and resilience of student nurses in northern Queensland Australia for disasters. Int J Disaster Risk Reduct. 2020;48:101585. [Link] [DOI:10.1016/j.ijdrr.2020.101585]
15. Chow KM, Tang WKF, Chan WHC, Sit WHJ, Choi KC, Chan S. Resilience and well-being of university nursing students in Hong Kong: A cross-sectional study. BMC Med Educ. 2018;18(1):13. [Link] [DOI:10.1186/s12909-018-1119-0]
16. Mathad MD, Pradhan B, Rajesh SK. Correlates and predictors of resilience among baccalaureate nursing students. J Clin Diagn Res. 2017;11(2):5-8. [Link] [DOI:10.7860/JCDR/2017/24442.9352]
17. Aloba O, Olabisi O, Aloba T. The 10-item Connor-Davidson resilience scale: Factorial structure, reliability, validity, and correlates among student nurses in southwestern Nigeria. J Am Psychiatr Nurs Assoc. 2016;22(1):43-51. [Link] [DOI:10.1177/1078390316629971]
18. Khorsand Chobdar M, Rahdar MA. Investigating the readiness of hospitals in Sistan and Baluchestan province in crisis of COVID-19. J Mil Med. 2020;22(6):553-61. [Persian] [Link]
19. Hamal PK, Pokhrel N, Pandey D, Malla P, Lamsal R. Perspective of doctors for COVID-19 pandemic readiness in government hospitals of Nepal. J Nepal Health Res Counc. 2020;18(2):166-71. [Link] [DOI:10.33314/jnhrc.v18i2.2811]
20. Shrestha GS, Paneru HR, Acharya SP, Shrestha SK, Sigdel MR, Tiwari S, et al. Preparedness for COVID-19 disease in hospitals of Nepal: A nationwide survey. J Nepal Med Assoc. 2020;58(224):248-51. [Link] [DOI:10.31729/jnma.4941]
21. Balay-Odao EM, Alquwez N, Inocian EP, Alotaibi RS. Hospital preparedness, resilience, and psychological burden among clinical nurses in addressing the COVID-19 crisis in Riyadh, Saudi Arabia. Front Public Health. 2021;8:573932. [Link] [DOI:10.3389/fpubh.2020.573932]
22. Taylor MG, Carr D. Psychological resilience and health among older adults: A comparison of personal resources. J Gerontol. 2020;76(6):1241-50. [Link] [DOI:10.1093/geronb/gbaa116]