Volume 13, Issue 4 (2021)
Iran J War Public Health 2021, 13(4): 235-238 |
Back to browse issues page
Article Type:
Subject:
History
Received: 2021/09/4 | Accepted: 2021/10/4 | Published: 2022/01/24
Received: 2021/09/4 | Accepted: 2021/10/4 | Published: 2022/01/24
How to cite this article
Bdaiwi S, Abdul - Saheb R. Variation in the Outcome following Intralesional 5-FU in the Treatment of Various Forms of Cutaneous Warts in Iraqi Patients based on Clinical Presentation. Iran J War Public Health 2021; 13 (4) :235-238
URL: http://ijwph.ir/article-1-1032-en.html
URL: http://ijwph.ir/article-1-1032-en.html
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



Rights and permissions
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Authors
S.A. Bdaiwi *1, R.H. Abdul - Saheb2
1- Lecturer/ dermatology specialist/ Department of Medicine, College of Medicine, University of Al- Qadisiyah, Iraq
2- Diwaniyah Teaching Hospital, Al-Qadisiyah, Iraq
2- Diwaniyah Teaching Hospital, Al-Qadisiyah, Iraq
Full-Text (HTML) (537 Views)
Introduction
One common skin problem seen in routine dermatological practice is cutaneous warts [1]. Their warty lesions are named according to their site in the body so that lesions of the face, dorsum of the hand, and shins are called "verruca plana", lesions seen on the sole of the feet are named "verruca plantaris", common warts are named "verruca vulgaris", and those lesions surrounding the nails are called "periungual verruca" [2]. These lesions are caused by infection of cells of the skin by the human papillomavirus (HPV). HPV is a small DNA virus that belongs to the family papovavirus [3]. The types of HPV are more than 150. Verruca vulgaris lesions are due to types 1, 2, 4, 27, or 57 and verruca plana lesions by HPV types 10 or 3 [3]. The most frequent types of HPV are 2, 27, 57, and 1 [4]. Warty lesions are mostly asymptomatic; however, they may cause psychological upset or physical disfigurement [4]. Cutaneous warts are common in children, and their prevalence in that age group is in the range of 3.3% up to 33% [5, 6]. In young adults, the prevalence rate is less than that in children, and roughly speaking, it is around 3.5%, and the prevalence rate becomes even less in individuals more than 35 years of age [4]. Cutaneous warts may undergo spontaneous resolution, and it has been shown that half of the children with warty lesions will get cured spontaneously within one year [7]. In general, spontaneous resolution is influenced by HPV type, host immune response, and infection location. People often seek medical advice because of the long time needed for spontaneous resolution, and some reports have shown that spontaneous resolution is seen in 40% only within a period of 2 years of follow-up [8]. The most cited study on the natural course of cutaneous warts reported that 113 of 168 children (67%) were free of warts after two years [9-11].
Antiviral agents can treat these lesions; however, the natural immune response can control the spread of these viral lesions and their sequelae. Some authors have suggested identifying the specific HPV type associated with a skin lesion before treating the lesion [12]. If initial treatment fails to control the skin lesion, it will be known as "recalcitrant"; therefore, an alternative form of treatment is required [13]. It has been stated that various topical agents used in everyday dermatological practice are often unsuccessful, and therefore patients may suffer adverse effects of these topical agents with no added benefit [13]. One meta-analysis showed that liquid nitrogen cryotherapy is not significantly different from placebo and that there was no significant difference between salicylic acid and cryotherapy when all areas of the body are considered [8]. In recent literature, the issue of using immune-manipulation methods is frequently raised including, dinitrochlorobenzene, 5-fluorouracil, intralesional interferon, intralesional bleomycin, intralesional antigen, and photodynamic therapy [8]. Although the exact mechanism of these immune modulators is not fully understood, most of these agents have been associated with promising results [13].
One of the well-known anti-tumor agents used in clinical practice is Five-Fluorouracil (FU), and it acts by inhibiting DNA synthesis through the blocking of thymidine and pyrimidine [14]. Prevention of DNA synthesis will stop cellular replication and proliferation, and this is the basis for using 5-FU in treating warts with some reports that favored acceptable efficacy and safety [15, 16].
The current study was planned and conducted to see the safety and efficacy of intralesional 5-FU in treating cutaneous warty lesions in a sample of Iraqi patients.
Materials and Methods
This experimental study included patients with various types of warty skin lesions. A total of 60 patients visited the dermatology unit at Aldiwaniyah teaching hospital, Aldiwaniyah province, Iraq, from August 2020 to August 2021. Sixty patients with various warty skin lesions, without any history of previous treatment, whose ages ranged from 20 to 55 years, were included in the present study. Pregnant women, children, and patients with a history of any other systemic illness were also excluded from the study. The diagnosis was made based on history and typical clinical features.
A questionnaire form was prepared and included information about age, gender, severity, and duration of disease, the character of the lesion, site of lesion, diagnosis, and treatment.
The study was approved ethically by the ethical approval committee of the college of medicine, the University of Al-Qadisiyah, and verbal consent was obtained from all participants. A solution was created containing 4mL of 50mg/mL 5-fluorouracil. Each wart and the adjacent skin were cleaned with isopropyl alcohol. The new solution was injected strictly intralesionally till blanching of the lesion occurred. After two weeks of 5-fluorouracil injection, a black ecchymosed eschar developed, which was pared, and residual warts, if present, were injected a second time. After each injection, antibiotics and anti-inflammatory agents were prescribed for five days to prevent secondary infection and post-injection pain. The patients were followed up to 3 months and then quarterly up to 1 year. Results were evaluated based on clinical improvement. Persistence of wart after three months of the last injection was taken as a failure of treatment the statistical analysis was done with the statistical package for social sciences (SPSS) version 16 (IBM, Chicago, USA) and Microsoft Office Excel 2007. Quantitative data were expressed as a range, standard deviation, and mean; while, qualitative data were expressed as percentages and numbers. Independent samples t-test was used to evaluate the difference in mean of quantitative variables; the Chi-square test was used to compare variation in proportions of qualitative variables. The cutoff value labeling significance was chosen at p≤0.05, and the cutoff level labeling high significance was chosen at p≤0.01.
Findings
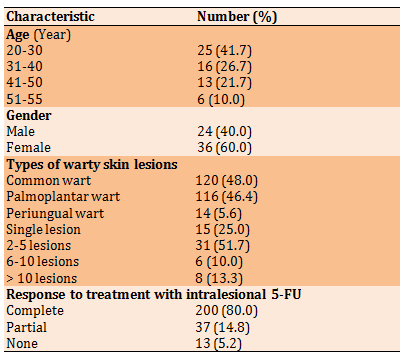
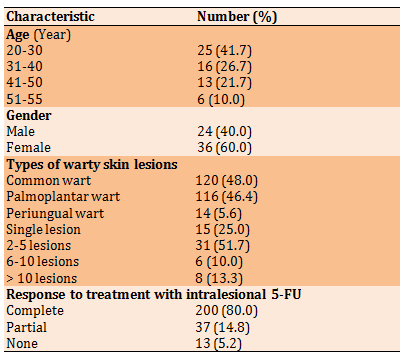
The current study included 60 patients with skin warts (Table 1). The mean age of patients was 35.81±7.06 years with a range of 20 to 55 years. Collectively, the total number of all warty lesions in all enrolled patients was 250.
Table 1) Demographic characteristics of study sample (n=60)
There was no significant association between size of warty lesion and response to intralesional 5-FU (p>0.05), but there was a significant association between type of warty lesion and response to intralesional 5-FU (p<0.05); in such a way that complete response was most commonly associated with palmoplantar lesions, whereas, no response was mostly associated with periungual lesions (Table 2).
Table 2) The association between size and type of warty lesion and response to intralesional 5-FU by the Chi-square test

Discussion
Cutaneous warts still represent a treatment challenge despite the wide array of various treatment options offered. Some of these lesions undergo spontaneous resolution; however, resistance to treatment or recurrence of lesions may stand as sources of autoinoculation [17]. 5-Fluorouracil is an antimetabolite known to be an effective and safe approach for treating common warts [18]. Topical 5-fluorouracil (5-FU) has been used to treat dermatological conditions for nearly half a century [19]. As a treatment for warts, topical 5-fluorouracil is primarily of historical interest, with most trials carried out in the 1970s and 1980s [20]. Based on previous reports on the successful response to intralesional 5-FU when treating cutaneous warts [16, 21], we planned and conducted this study because little is known about its efficacy and safety in Iraqi patients. The rationale for using 5-FU in treating warty lesions is that it inhibits DNA synthesis and limits cellular proliferation [14, 16]. The literature has shown that conventional treatments used in everyday practice are uniformly unsuccessful and carry concerns regarding safety [22, 23]. It has been stated that intralesional delivery of 5-FU is associated with pain that is intolerable by patients [16, 21]; however, in the current study, the pain was not intolerable to the degree of refusing treatment by patients all participants were cooperative, and the only undesirable outcome is the failure of therapy in 5.2% of patients. Therefore, we believe that intralesional administration of 5-FU in cases resistant to conventional modes of treatment or characterized by a high rate of recurrence is justified. Complete response was seen in 80% of patients, and this response rate is highly promising. In one previous study, complete response was seen in 76.7% of patients receiving intralesional 5-FU [16], and this rate is nearly similar to that obtained in the current study. In another study, complete response was seen in 70% of cases treated with intralesional 5 –FU [14], and this figure is somewhat less than that reported in our study. Unfortunately, the placebo group in the current study was not involved because of the refusal of most of the patients to receive such mode of treatment, but, Isçimen et al. in 2004 included a control group (treated with conventional treatment) in whom the response rate was 29% only, and this reflects the advantage of using intralesional 5-FU over conventional modalities of therapy.
On the other hand, a placebo group was enrolled in one previous study in which the success rate of intralesional 5-FU was 64.7% compared to 35.3% in the placebo group [21]. In addition, in another study, the rate of success in the group of 5-FU was 95.4% compared to 13.3% in the placebo group [24]. The most important adverse effects associated with intralesional 5-FU, as reported by previous authors [14, 24], were pain and hemorrhagic eschars; however, in our study, hemorrhagic eschars were not reported. In another comparative study, the success rate in the case of 5-FU was 63.9% compared to 40% in the control group [25]. In our study, response to treatment was not affected by the lesion site;
however, the type of lesion significantly influenced the treatment response.
Conclusion
The intralesional 5-FU appears to be highly effective in treating cutaneous warts; however, the response is influenced by the type of skin lesion, being maximal with palmoplantar wart and least common with the skin lesion periungual lesions.
Acknowledgments: I would like to express my deep thanks to all patients enrolled in the current study for their kind cooperation to complete the present therapeutic trial.
Ethical Permissions: The study was approved by the ethical approval committee of the college of medicine of the University of Al-Qadisiyah.
Conflicts of Interests: -
Authors’ Contribution: Bdaiwi SA. (First Author), Introduction Writer/Discussion Writer (50%); Abdul - Saheb RH. (Second Author), Assistant Researcher (50%).
Funding/Support: -
One common skin problem seen in routine dermatological practice is cutaneous warts [1]. Their warty lesions are named according to their site in the body so that lesions of the face, dorsum of the hand, and shins are called "verruca plana", lesions seen on the sole of the feet are named "verruca plantaris", common warts are named "verruca vulgaris", and those lesions surrounding the nails are called "periungual verruca" [2]. These lesions are caused by infection of cells of the skin by the human papillomavirus (HPV). HPV is a small DNA virus that belongs to the family papovavirus [3]. The types of HPV are more than 150. Verruca vulgaris lesions are due to types 1, 2, 4, 27, or 57 and verruca plana lesions by HPV types 10 or 3 [3]. The most frequent types of HPV are 2, 27, 57, and 1 [4]. Warty lesions are mostly asymptomatic; however, they may cause psychological upset or physical disfigurement [4]. Cutaneous warts are common in children, and their prevalence in that age group is in the range of 3.3% up to 33% [5, 6]. In young adults, the prevalence rate is less than that in children, and roughly speaking, it is around 3.5%, and the prevalence rate becomes even less in individuals more than 35 years of age [4]. Cutaneous warts may undergo spontaneous resolution, and it has been shown that half of the children with warty lesions will get cured spontaneously within one year [7]. In general, spontaneous resolution is influenced by HPV type, host immune response, and infection location. People often seek medical advice because of the long time needed for spontaneous resolution, and some reports have shown that spontaneous resolution is seen in 40% only within a period of 2 years of follow-up [8]. The most cited study on the natural course of cutaneous warts reported that 113 of 168 children (67%) were free of warts after two years [9-11].
Antiviral agents can treat these lesions; however, the natural immune response can control the spread of these viral lesions and their sequelae. Some authors have suggested identifying the specific HPV type associated with a skin lesion before treating the lesion [12]. If initial treatment fails to control the skin lesion, it will be known as "recalcitrant"; therefore, an alternative form of treatment is required [13]. It has been stated that various topical agents used in everyday dermatological practice are often unsuccessful, and therefore patients may suffer adverse effects of these topical agents with no added benefit [13]. One meta-analysis showed that liquid nitrogen cryotherapy is not significantly different from placebo and that there was no significant difference between salicylic acid and cryotherapy when all areas of the body are considered [8]. In recent literature, the issue of using immune-manipulation methods is frequently raised including, dinitrochlorobenzene, 5-fluorouracil, intralesional interferon, intralesional bleomycin, intralesional antigen, and photodynamic therapy [8]. Although the exact mechanism of these immune modulators is not fully understood, most of these agents have been associated with promising results [13].
One of the well-known anti-tumor agents used in clinical practice is Five-Fluorouracil (FU), and it acts by inhibiting DNA synthesis through the blocking of thymidine and pyrimidine [14]. Prevention of DNA synthesis will stop cellular replication and proliferation, and this is the basis for using 5-FU in treating warts with some reports that favored acceptable efficacy and safety [15, 16].
The current study was planned and conducted to see the safety and efficacy of intralesional 5-FU in treating cutaneous warty lesions in a sample of Iraqi patients.
Materials and Methods
This experimental study included patients with various types of warty skin lesions. A total of 60 patients visited the dermatology unit at Aldiwaniyah teaching hospital, Aldiwaniyah province, Iraq, from August 2020 to August 2021. Sixty patients with various warty skin lesions, without any history of previous treatment, whose ages ranged from 20 to 55 years, were included in the present study. Pregnant women, children, and patients with a history of any other systemic illness were also excluded from the study. The diagnosis was made based on history and typical clinical features.
A questionnaire form was prepared and included information about age, gender, severity, and duration of disease, the character of the lesion, site of lesion, diagnosis, and treatment.
The study was approved ethically by the ethical approval committee of the college of medicine, the University of Al-Qadisiyah, and verbal consent was obtained from all participants. A solution was created containing 4mL of 50mg/mL 5-fluorouracil. Each wart and the adjacent skin were cleaned with isopropyl alcohol. The new solution was injected strictly intralesionally till blanching of the lesion occurred. After two weeks of 5-fluorouracil injection, a black ecchymosed eschar developed, which was pared, and residual warts, if present, were injected a second time. After each injection, antibiotics and anti-inflammatory agents were prescribed for five days to prevent secondary infection and post-injection pain. The patients were followed up to 3 months and then quarterly up to 1 year. Results were evaluated based on clinical improvement. Persistence of wart after three months of the last injection was taken as a failure of treatment the statistical analysis was done with the statistical package for social sciences (SPSS) version 16 (IBM, Chicago, USA) and Microsoft Office Excel 2007. Quantitative data were expressed as a range, standard deviation, and mean; while, qualitative data were expressed as percentages and numbers. Independent samples t-test was used to evaluate the difference in mean of quantitative variables; the Chi-square test was used to compare variation in proportions of qualitative variables. The cutoff value labeling significance was chosen at p≤0.05, and the cutoff level labeling high significance was chosen at p≤0.01.
Findings
The current study included 60 patients with skin warts (Table 1). The mean age of patients was 35.81±7.06 years with a range of 20 to 55 years. Collectively, the total number of all warty lesions in all enrolled patients was 250.
Table 1) Demographic characteristics of study sample (n=60)
There was no significant association between size of warty lesion and response to intralesional 5-FU (p>0.05), but there was a significant association between type of warty lesion and response to intralesional 5-FU (p<0.05); in such a way that complete response was most commonly associated with palmoplantar lesions, whereas, no response was mostly associated with periungual lesions (Table 2).
Table 2) The association between size and type of warty lesion and response to intralesional 5-FU by the Chi-square test

Discussion
Cutaneous warts still represent a treatment challenge despite the wide array of various treatment options offered. Some of these lesions undergo spontaneous resolution; however, resistance to treatment or recurrence of lesions may stand as sources of autoinoculation [17]. 5-Fluorouracil is an antimetabolite known to be an effective and safe approach for treating common warts [18]. Topical 5-fluorouracil (5-FU) has been used to treat dermatological conditions for nearly half a century [19]. As a treatment for warts, topical 5-fluorouracil is primarily of historical interest, with most trials carried out in the 1970s and 1980s [20]. Based on previous reports on the successful response to intralesional 5-FU when treating cutaneous warts [16, 21], we planned and conducted this study because little is known about its efficacy and safety in Iraqi patients. The rationale for using 5-FU in treating warty lesions is that it inhibits DNA synthesis and limits cellular proliferation [14, 16]. The literature has shown that conventional treatments used in everyday practice are uniformly unsuccessful and carry concerns regarding safety [22, 23]. It has been stated that intralesional delivery of 5-FU is associated with pain that is intolerable by patients [16, 21]; however, in the current study, the pain was not intolerable to the degree of refusing treatment by patients all participants were cooperative, and the only undesirable outcome is the failure of therapy in 5.2% of patients. Therefore, we believe that intralesional administration of 5-FU in cases resistant to conventional modes of treatment or characterized by a high rate of recurrence is justified. Complete response was seen in 80% of patients, and this response rate is highly promising. In one previous study, complete response was seen in 76.7% of patients receiving intralesional 5-FU [16], and this rate is nearly similar to that obtained in the current study. In another study, complete response was seen in 70% of cases treated with intralesional 5 –FU [14], and this figure is somewhat less than that reported in our study. Unfortunately, the placebo group in the current study was not involved because of the refusal of most of the patients to receive such mode of treatment, but, Isçimen et al. in 2004 included a control group (treated with conventional treatment) in whom the response rate was 29% only, and this reflects the advantage of using intralesional 5-FU over conventional modalities of therapy.
On the other hand, a placebo group was enrolled in one previous study in which the success rate of intralesional 5-FU was 64.7% compared to 35.3% in the placebo group [21]. In addition, in another study, the rate of success in the group of 5-FU was 95.4% compared to 13.3% in the placebo group [24]. The most important adverse effects associated with intralesional 5-FU, as reported by previous authors [14, 24], were pain and hemorrhagic eschars; however, in our study, hemorrhagic eschars were not reported. In another comparative study, the success rate in the case of 5-FU was 63.9% compared to 40% in the control group [25]. In our study, response to treatment was not affected by the lesion site;
however, the type of lesion significantly influenced the treatment response.
Conclusion
The intralesional 5-FU appears to be highly effective in treating cutaneous warts; however, the response is influenced by the type of skin lesion, being maximal with palmoplantar wart and least common with the skin lesion periungual lesions.
Acknowledgments: I would like to express my deep thanks to all patients enrolled in the current study for their kind cooperation to complete the present therapeutic trial.
Ethical Permissions: The study was approved by the ethical approval committee of the college of medicine of the University of Al-Qadisiyah.
Conflicts of Interests: -
Authors’ Contribution: Bdaiwi SA. (First Author), Introduction Writer/Discussion Writer (50%); Abdul - Saheb RH. (Second Author), Assistant Researcher (50%).
Funding/Support: -
Keywords:
References
1. Dall'oglio F, D'Amico V, Nasca MR, Micali G. Treatment of cutaneous warts: an evidence-based review. Am J Clin Dermatol. 2012;13(2):73-96. [Link] [DOI:10.2165/11594610-000000000-00000] [PMID]
2. Ringin SA. The effectiveness of cutaneous wart resolution with current treatment modalities. J Cutan Aesthet Surg. 2020;13(1):24-30. [Link]
3. Sterling JC, Gibbs S, Haque Hussain SS, Mohd Mustapa MF, Handfield-Jones SE. British association of dermatologists' guidelines for the management of cutaneous warts 2014. Br J Dermatol. 2014;171(4):696-712. [Link] [DOI:10.1111/bjd.13310] [PMID]
4. Liu J, Li H, Yang F, Ren Y, Xia T, Zhao Z, et al. Epidemiology and clinical profile of cutaneous warts in Chinese college students: a cross-sectional and follow-up study. Sci Rep. 2018;8(1):15450. [Link] [DOI:10.1038/s41598-018-33511-x] [PMID] [PMCID]
5. Yamamah GA, Emam HM, Abdelhamid MF, Elsaie ML, Shehata H, Farid T, et al. Epidemiologic study of dermatologic disorders among children in South Sinai, Egypt. Int J Dermatol. 2012;51(10):1180-5. [Link] [DOI:10.1111/j.1365-4632.2012.05475.x] [PMID]
6. Silverberg JI, Silverberg NB. The US prevalence of common warts in childhood: a population-based study. J Invest Dermatol. 2013;133(12):2788-90. [Link] [DOI:10.1038/jid.2013.226] [PMID]
7. Bruggink SC, Eekhof JAH, Egberts PF, van Blijswijk SCE, Assendelft WJJ, Gussekloo J. Natural course of cutaneous warts among primary schoolchildren: a prospective cohort study. Ann Fam Med. 2013;11(5):437-41. [Link] [DOI:10.1370/afm.1508] [PMID] [PMCID]
8. Kwok CS, Gibbs S, Bennett C, Holland R, Abbott R. Topical treatments for cutaneous warts. Cochrane Database Syst Rev. 2012;2012(9):CD001781. [Link] [DOI:10.1002/14651858.CD001781.pub3] [PMID] [PMCID]
9. Massing AM, Epstein WL. Natural history of warts: a two-year study. Arch Dermatol. 1963;87:306-10 [Link] [DOI:10.1001/archderm.1963.01590150022004] [PMID]
10. van der Werf E. Studies on the incidence and course of warts in school children. Ned Tijdschr Geneeskd. 1959;103(23):1204-8. [Dutch] [Link]
11. Williams HC, Pottier A, Strachan D. The descriptive epidemiology of warts in British schoolchildren. Br J Dermatol. 1993;128(5):504-11 [Link] [DOI:10.1111/j.1365-2133.1993.tb00226.x] [PMID]
12. Bruggink SC, Gussekloo J, de Koning MN, Feltkamp MC, Bavinck JN, Quint WG, et al. HPV type in plantar warts influences natural course and treatment response: secondary analysis of a randomised controlled trial. J Clin Virol. 2013;57(3):227-32. [Link] [DOI:10.1016/j.jcv.2013.02.021] [PMID]
13. Abd-Elazeim FM, Mohammed GF, Fathy A, Mohamed RW. Evaluation of IL-12 serum level in patients with recalcitrant multiple common warts, treated by intralesional tuberculin antigen. J Dermatolog Treat. 2014;25(3):264-7. [Link] [DOI:10.3109/09546634.2013.768760] [PMID]
14. Isçimen A, Aydemir EH, Göksügür N, Engin B. Intralesional 5-fluorouracil, lidocaine and epinephrine mixture for the treatment of verrucae: a prospective placebo-controlled, single-blind randomized study. J Eur Acad Dermatol Venereol. 2004;18(4):455-8. [Link] [DOI:10.1111/j.1468-3083.2004.00984.x] [PMID]
15. Kannambal K, Kaviarasan PK, Prasad PVS, Poorana B, Balajiganesh J. Efficacy of intralesional 5-fluorouracil in recalcitrant warts a study at tertiary care centre. J Med Sci Clin Res. 2019;7:556-60. [Link] [DOI:10.18535/jmscr/v7i6.94]
16. Ghonemy S, Ibrahim Ali M, Ebrahim HM. The efficacy of microneedling alone vs its combination with 5-fluorouracil solution vs 5-fluorouracil intralesional injection in the treatment of plantar warts. Dermatol Ther. 2020;33(6):e14179. [Link] [DOI:10.1111/dth.14179] [PMID]
17. Konicke K, Olasz E. Successful treatment of recalcitrant plantar warts with bleomycin and microneedling. Dermatol Surg. 2016;42(8):1007-8. [Link] [DOI:10.1097/DSS.0000000000000738] [PMID]
18. Mahajan BB, Singla M. Evaluation of intralesional 5% 5-fluorouracil in resistant localized plaque psoriasis. Indian Dermatol Online J. 2014;5(3):287-90. [Link] [DOI:10.4103/2229-5178.137779] [PMID] [PMCID]
19. Moore AY. Clinical applications for topical 5-fluorouracil in the treatment of dermatological disorders. J Dermatolog Treat. 2009;20(6):328-35. [Link] [DOI:10.3109/09546630902789326] [PMID]
20. Bunney MH. The treatment of plantar warts with 5-fluorouracil. Br J Dermatol 1973;89:96-7 [Link] [DOI:10.1111/j.1365-2133.1973.tb01926.x] [PMID]
21. Yazdanfar A, Farshchian M, Fereydoonnejad M, Farshchian M. Treatment of common warts with an intralesional mixture of 5-fluorouracil, lidocaine, and epinephrine: a prospective placebo-controlled, double-blind randomized trial. Dermatol Surg. 2008;34(5):656-9.
https://doi.org/10.1111/j.1524-4725.2007.34123.x [Link] [DOI:10.1097/00042728-200805000-00009] [PMID]
22. Gibbs S. The trials of treating warts. Indian J Dermatol Venereol Leprol. 2014;80:495-6. [Link] [DOI:10.4103/0378-6323.144142] [PMID]
23. Khozeimeh F, Jabbari Azad F, Mahboubi Oskouei Y, Jafari M, Tehranian S, Alizadehsani R, et al. Intralesional immunotherapy compared to cryotherapy in the treatment of warts. Int J Dermatol. 2017;56(4):474-8. [Link] [DOI:10.1111/ijd.13535] [PMID]
24. Srivastava A, Ghiya BC, Soni p, Dave H, Dhanwal A, Mehta RD. Efficacy of intralesional 5-fluorouracil in treatment of Palmo-plantar warts. Int J Med Res. 2016;2(3):60-3. [Link] [DOI:10.21276/ijmrp.2016.2.3.013]
25. Kenawi MZ, Sherine H, EL-Rahman SH, Salam OH. Efficacy of Intralesional 5-fluorouracil versus BCG vaccine in the treatment of warts. Egypt J Dermatol Androl. 2012;32:3-14. [Link]








